Published online Sep 24, 2015. doi: 10.5500/wjt.v5.i3.137
Peer-review started: April 1, 2015
First decision: June 9, 2015
Revised: July 22, 2015
Accepted: August 4, 2015
Article in press: August 7, 2015
Published online: September 24, 2015
Processing time: 176 Days and 21.2 Hours
AIM: To analyze the national trends associated with body mass index (BMI) and living kidney donation.
METHODS: Forty-seven thousand seven hundred and five adult living kidney donors as reported to the Organ Procurement and Transplantation Network from 1999 to 2011 were analyzed using their pre-donation BMI. Predictor variables of interest included age, gender, ethnicity, relationship, education status, and transplant region.
RESULTS: Sixteen thousand nine hundred and seventy-one of the living kidney donors were normal weight (35.6%); 19337 were overweight (40.5%); 9007 were mildly obese (18.9%); 1992 were moderate to morbidly obese (4.2%). Overweight and mildly obese kidney donors have increased through time by 12% and 20% every 5 years, respectively (P < 0.05). Donors 35-49 years of age, hispanic males or females and black females, those with high school diploma or general Education Degree, and biologically related or partner/spouses were more likely to be obese.
CONCLUSION: Over the past 13 years, the majority of living kidney donors have spanned the overweight to obese categories. Paralleling the national rise is an increase in overweight and mildly obese kidney donors. A fair number of moderate to morbidly obese living kidney donors are still allowed to donate.
Core tip: The obesity epidemic is increasing. This study was conducted to analyze the national trends associated with body mass index (BMI) and living kidney donation using the United Network for Organ Sharing/Organ Procurement and Transplantation Network database in the United States. Forty-seven thousand seven hundred and five adult living kidney donors were analyzed according to BMI. Sixty-three point six percent of living kidney donors over the past thirteen years have spanned the overweight to obese categories. The increase in the overweight and mildly obese living kidney donors in our study parallels the national increase in obesity trends. A fair number of moderate to morbidly obese living kidney donors are still allowed to donate. Donors 35-49 years of age, hispanic males or females and black females, those with high school diploma or general Education Degree, and biologically related or partner/spouses were more likely to be obese. Care is advised when allowing donors in this BMI category to donate due to the uncertainty of the long term outcomes. Continued awareness and implementation of programs to limit the obesity crisis are needed.
- Citation: Sachdeva M, Rosen LM, Varghese J, Fishbane S, Molmenti EP. Weight trends in United States living kidney donors: Analysis of the UNOS database. World J Transplant 2015; 5(3): 137-144
- URL: https://www.wjgnet.com/2220-3230/full/v5/i3/137.htm
- DOI: https://dx.doi.org/10.5500/wjt.v5.i3.137
The obesity epidemic has been increasing over the past three decades[1]. Measuring a height, weight, and calculating a body mass index (BMI) has been the recommended standard practice by the Organ Procurement and Transplantation Network (OPTN) as part of the physical evaluation of a potential living kidney donor[2]. According to OPTN guidelines, having a BMI greater than 35 kg/m2 is considered a relative contraindication to be a living kidney donor[3]. Despite this, transplant centers across the United States use different criteria in determining donor exclusion based on BMI. Based on a 2007 United States Transplant Center Survey, twenty percent of the transplant centers that were surveyed excluded those with BMI greater than 40 kg/m2, fifty two percent of United States kidney transplant centers excluded donors with BMI greater than 35 kg/m2, ten percent of programs excluded those with BMI over 30 kg/m2, twelve percent had no policy for exclusion, and six percent excluded based on BMI if they had other cardiovascular risks[4].
There is a shortage of living kidney donors. In 1999, per OPTN data, there were approximately 4728 living kidney donors. Although there has been an increase in the number of living kidney donors in the past 10 years, there is a downward trend since 2010. The number of living kidney donors went from 6278 to 5773 to 5619 to 5734 during 2010, 2011, 2012, and 2013 respectively[5]. These numbers of living kidney donor transplantations are not able to keep up with the increasing potential kidney recipients on the wait list which currently runs at approximately 103627[5].
Due to the shortage of living kidney donors, some transplant centers may be less stringent on the obesity criteria. However, the safety of potential donors must come first. Peri-operative and post-operative outcomes are concerns with obese kidney donors. Having a BMI greater than 35 kg/m2 has been associated with slightly longer operative times and overall more peri-operative complications, such as wound complications[6]. In addition, long term outcomes for obese living kidney donors are still uncertain[7].
Due to the national shortage of living kidney donors and the parallel national increase in obesity, the primary aim of our study was to analyze the national temporal trends associated with BMI and living kidney donation over the past 13 years. In addition, we wanted to examine the association between live kidney donor BMIs and age, gender, race/ethnicity, relationship to the kidney transplant recipient, education status, transplant region, and year.
Adult live kidney donors, over the age of 18 years in the United States from January 1st, 1999 to December 31st, 2011 were analyzed based on the United Network for Organ Sharing (UNOS)/OPTN standard transplant analysis and research files database. The study was performed with approval from the North Shore-LIJ Health System institutional review board.
The primary variable of interest was pre-donation BMI category. BMI was divided into five categories using the World Health Organization classification of obesity: Mildly thin was defined as BMI greater than or equal to 17 kg/m2 and less than 18.5 kg/m2. Normal weight was defined as a BMI greater than or equal to 18.5 kg/m2 and less than 25 kg/m2. Overweight was defined as a BMI greater than or equal to 25 kg/m2 and less than 30 kg/m2. Mild obesity was defined as a BMI greater than or equal to 30 kg/m2 and less than 35 kg/m2. Moderate to morbid obesity was defined as a BMI greater than or equal to 35 kg/m2. Multinomial logistic regression was used to model the outcome of donor BMI category: normal, overweight, mild obesity and moderate/morbid obesity. Due to the smaller number of subjects in the mildly thin category, it was excluded from the multinomial logistic regression analysis. Normal weight category was chosen as the reference.
Predictors of BMI included age category (18-34, 35-49, 50-65, ≥ 65 years), gender, race/ethnicity (White, Black, Hispanic, Asian, Other), education (no high school diploma or general education degree (GED), high school diploma or GED (GED refers to testing that assures that the test taker is at high school level academic skills), attended college/technical school, associate/bachelor’s degree, graduate degree), relationship to the organ recipient (non-biological, biological, partner/spouse), transplant region, and year. For demographics, descriptive statistics (mean, standard deviation, median, interquartile range-IQR, frequencies and percents) of demographic factors were used to describe the donors.
BMIs less than 17 kg/m2 or over 45 kg/m2 were considered implausible values and most likely to be erroneous entries, therefore, donors with BMI values outside of the 17 kg/m2 to 45 kg/m2 range were excluded. Donors less than 18 years of age or with a relationship status of paired exchange, deceased donor exchange or domino were excluded.
All analysis was conducted in SAS version 9.3 (SAS Institute, Inc., Cary, NC). Results were considered significant at P < 0.05.
There were a total of 53671 adult living donors who donated a kidney between 1999 and 2011. Five thousand seven hundred and sixty-four (10.7%) were removed due to missing BMI and 202 (0.4%) were removed for implausible values (see methods section). This resulted in 47705 adult live kidney donors who met the inclusion criteria. Characteristics of the live kidney donors are listed in Table 1. The average age was 40.69 ± 11.28 years. Females, whites, and biologically related donors comprised the majority of the live kidney donors. Few live donors were Asian. The average BMI was 26.87 ± 4.38 kg/m2. Sixty-three point six percent of living kidney donors had BMI above 25 kg/m2. 25.3% of donors had either a high school diploma/GED, and 22.1% had attended college/technical school.
| Characteristic | (%) |
| Age | |
| 18-34 | 31.7 |
| 35-49 | 44.5 |
| 50-64 | 22.5 |
| ≥ 65 | 1.3 |
| Gender | |
| Male | 40.2 |
| Female | 59.8 |
| Race/ethnicity | |
| Asian | 3.7 |
| Black | 13.3 |
| Hispanic | 14.1 |
| White | 67.5 |
| Other | 1.4 |
| BMI | |
| Mildly thin | 0.8 |
| Normal | 35.6 |
| Overweight | 40.5 |
| Mildly obese | 18.9 |
| Moderate/morbid obese | 4.2 |
| Living donor relationship | |
| Biological | 61.5 |
| Spouse/life partner | 12.9 |
| Non-biological | 25.6 |
| Education | |
| No HS diploma or GED | 1.8 |
| HS or GED | 25.3 |
| Attended college/technical school | 22.1 |
| Associate/bachelors degree | 19.9 |
| Graduate degree | 8.1 |
| Unknown | 22.7 |
| Region | |
| 1 | 4.4 |
| 2 | 14.3 |
| 3 | 8.8 |
| 4 | 7.7 |
| 5 | 18.2 |
| 6 | 2.6 |
| 7 | 13.8 |
| 8 | 6.1 |
| 9 | 8.1 |
| 10 | 8.5 |
| 11 | 7.4 |
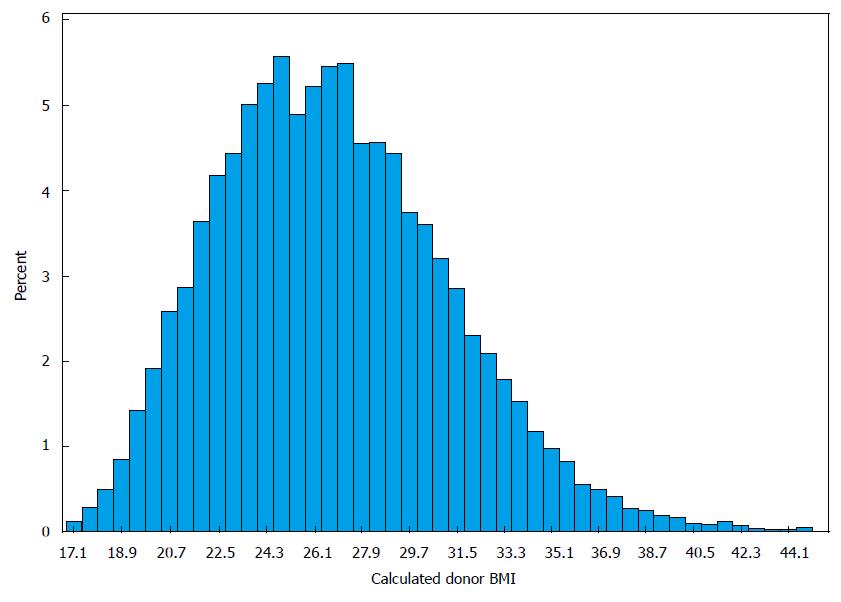
Of the total donors who met the inclusion criteria, 398 were mildly thin (0.8%); 16971 were normal weight (35.6%); 19337 were overweight (40.5%); 9007 were in the mild obesity group (18.9%); 1992 in the moderate/morbidly obese group (4.2%). Figure 1 depicts the distribution of living kidney donors by BMI.
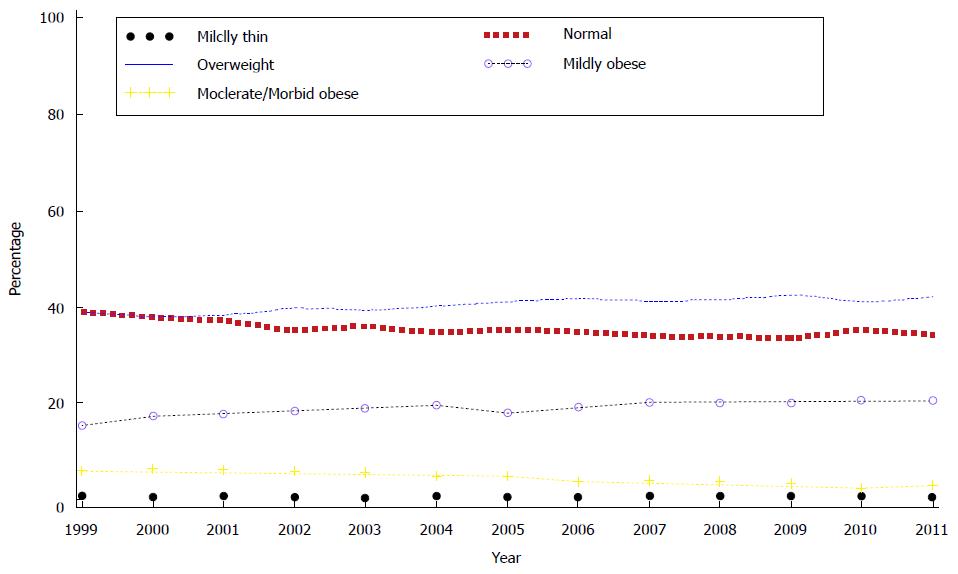
As depicted in Figure 2, over time, donors were less likely to be in the moderate/morbid BMI category as compared to the normal weight BMI category. More specifically, with each 5 year period, the odds of donors being in the moderate/morbid BMI category as compared to the normal weight BMI category decreased by 25% (P < 0.05). However, over time, donors were more likely to be in the mildly obese and overweight BMI categories as compared to the normal weight BMI category. More specifically, with each 5 year period, the odds of donors being in the mildly obese and overweight BMI categories as compared to normal weight BMI categories increased by 20% and 12%, respectively, P < 0.05.
Results from the multinomial logistic regression are summarized in Table 2. Live donor relationship (P < 0.0001), education (P < 0.0001), region (P < 0.0001) and increasing year (P < 0.0001) were significantly associated with donor BMI category. Additionally, significant interactions were noted between donor age and gender (P < 0.0001), and ethnicity (P < 0.0001).
| Weight category | Moderate/morbid | Mild obese | Overweight |
| vs normal weight | obese OR (95%CI) | OR (95%CI) | OR (95%CI) |
| Relationship | |||
| Biological | 1.34 (1.19, 1.51)a | 1.19 (1.11, 1.27)a | 1.08 (1.03, 1.14)a |
| Partner/spouse | 1.64 (1.39, 1.93)a | 1.31 (1.19, 1.43)a | 1.18 (1.09, 1.27)a |
| Non-biological | Ref. | Ref. | Ref. |
| Age x gender | |||
| Males | |||
| 18-34 yr | Ref. | Ref. | Ref. |
| 35-49 yr | 1.65 (1.38, 1.97)a | 1.84 (1.67, 2.02)a | 1.82 (1.69, 1.97)a |
| 50-64 yr | 1.32 (1.04, 1.69)a | 1.76 (1.56, 1.98)a | 1.78 (1.61, 1.96)a |
| ≥ 65 yr | 1.40 (0.66, 2.97) | 1.47 (0.99, 2.16) | 1.40 (1.03, 1.92)a |
| Females | |||
| 18-34 yr | Ref. | Ref. | Ref. |
| 35-49 yr | 1.03 (0.90, 1.17) | 1.30 (1.20, 1.41)a | 1.23 (1.15, 1.32)a |
| 50-64 yr | 0.86 (0.72, 1.02) | 1.21 (1.10, 1.33)a | 1.43 (1.33, 1.55)a |
| ≥ 65 yr | 0.51 (0.25, 1.04) | 0.73 (0.52, 1.04) | 1.27 (1.01, 1.61)a |
| Ethnicity/race x gender | |||
| Males | |||
| Asian | 0.31 (0.18, 0.55)a | 0.22 (0.17, 0.30)a | 0.49 (0.42, 0.58)a |
| Black | 1.18 (0.95, 1.46) | 0.99 (0.87, 1.12) | 0.84 (0.76, 0.93)a |
| Hispanic | 1.46 (1.16, 1.85)a | 1.34 (1.18, 1.52)a | 1.21 (1.09, 1.35)a |
| White | Ref. | Ref. | Ref. |
| Other | 1.60 (0.85, 3.00) | 1.23 (0.84, 1.79) | 1.13 (0.82, 1.54) |
| Females | |||
| Asian | 0.15 (0.07, 0.30)a | 0.33 (0.26, 0.42)a | 0.54 (0.47, 0.63)a |
| Black | 2.75 (2.36, 3.22)a | 2.41 (2.17, 2.66)a | 1.82 (1.66, 1.99)a |
| Hispanic | 1.49 (1.24, 1.78)a | 1.50 (1.35, 1.66)a | 1.49 (1.37, 1.62)a |
| White | Ref. | Ref. | Ref. |
| Other | 2.06 (1.34, 3.17)a | 1.83 (1.40, 2.41)a | 1.57 (1.25, 1.99)a |
| Education | |||
| No HS diploma or GED | Ref. | Ref. | Ref. |
| HS or GED | 2.03 (1.26, 3.28)a | 1.08 (0.88, 1.32) | 0.91 (0.77, 1.07) |
| Attended college/technical school | 1.91 (1.18, 3.10)a | 1.02 (0.83, 1.26) | 0.93 (0.79, 1.10) |
| Associate/bachelors degree | 1.40 (0.86, 2.28) | 0.80 (0.65, 0.99)a | 0.80 (0.67, 0.94)a |
| Graduate degree | 1.04 (0.62, 1.73) | 0.61 (0.49, 0.76)a | 0.67 (0.56, 0.80)a |
| Unknown | 1.84 (1.14, 2.98)a | 1.03 (0.84, 1.27) | 0.92 (0.77, 1.08) |
| Region | |||
| 1 | 1.18 (0.88, 1.57) | 1.26 (1.08, 1.48)a | 1.14 (1.01, 1.29)a |
| 2 | 1.23 (0.99, 1.52) | 1.09 (0.97, 1.23) | 0.99 (0.90, 1.08) |
| 3 | 1.08 (0.85, 1.37) | 1.19 (1.05, 1.36)a | 1.13 (1.02, 1.25)a |
| 4 | 1.51 (1.19, 1.90) | 1.46 (1.28, 1.66)a | 1.15 (1.03, 1.28)a |
| 5 | 0.78 (0.63, 0.97)a | 0.99 (0.88, 1.11) | 0.99 (0.91, 1.09) |
| 6 | 0.85 (0.58, 1.26) | 0.98 (0.81, 1.19) | 1.07 (0.92, 1.24) |
| 7 | 1.49 (1.21, 1.83)a | 1.31 (1.17, 1.47)a | 1.03 (0.94, 1.13) |
| 8 | 0.71 (0.53, 0.95)a | 0.92 (0.79, 1.06) | 1.04 (0.93, 1.16) |
| 9 | Ref. | Ref. | Ref. |
| 10 | 1.30 (1.03, 1.64)a | 1.33 (1.17, 1.52)a | 1.13 (1.02, 1.26)a |
| 11 | 1.06 (0.83, 1.35) | 1.23 (1.08, 1.41)a | 1.11 (0.99, 1.23) |
| Year | 0.75 (0.69, 0.80)a | 1.20 (1.15, 1.25)a | 1.12 (1.08, 1.15)a |
| aP < 0.05 |
Male donors (35-49 years, and 50-64 years) were more likely to be obese and overweight than younger donors. Female donors 35-49 years of age had increased odds as compared to female donors 50-64 years of being moderately or morbidly obese (OR: 1.19, 95%CI: 1.02-1.40).
Male and female Asian donors had decreased odds as compared to all other donors of being obese. Female Blacks and Hispanics were more likely to be in the obese categories. Female Black donors had increased odds as compared to female Hispanic donors of being in higher BMI categories (moderate/morbid OR: 1.85, 95%CI: 1.50-2.29, mild OR: 1.61, 95%CI: 1.41-1.83). Male Hispanics were more likely to be obese as compared to male Black donors.
Biologically related donors and partner/spouse donors had increased odds as compared to non-biological donors of being obese as compared to normal weight donors. Partner/spouse donors had increased odds as compared to biological donors of being moderately or morbidly obese (OR: 1.22, 95%CI: 1.06, 1.40) and mildly obese (OR: 1.10. 95%CI: 1.01, 1.19).
Donors with a High School (HS) diploma or GED had increased odds as compared to donors with an associate/bachelor’s degree and donors with a graduate degree of being moderately or morbidly obese (OR: 1.45, 95%CI: 1.25-1.68 and 1.96, 95%CI: 1.60-2.45, respectively) and mildly obese (OR: 1.35, 95%CI: 1.25-1.46 and 1.77, 95%CI: 1.58-1.97, respectively). Donors who attended college or technical school had increased odds as compared to donors with an associate or bachelor’s degree and donors with a graduate degree of being moderately or morbidly obese (OR: 1.37, 95%CI: 1.17-1.59 and 1.85, 95%CI: 1.47-2.32, respectively) and mildly obese (OR: 1.28, 95%CI: 1.18-1.39 and 1.68, 95%CI: 1.50-1.87, respectively) as compared to normal weight.
To help organ procurement, allocation, and transplantation, the United States is divided into 11 different UNOS regions. These regions correspond to some extent to the United States Census regions. There was a significant association between region and donor BMI. Region 9 had reduced odds as compared to other regions of having donors in higher BMI groups. Region 4 and Region 7 were more likely to have donors in the higher BMI groups.
Obesity is an increasing epidemic in the United States[8,9]. Sixty-three point six percent of living kidney donors in the past thirteen years have spanned the overweight to obese categories. The increase in the overweight and mildly obese living kidney donors in our study parallel the national increase in obesity trends.
Of concern is that obesity can be associated with an increased risk of hypertension, impaired fasting glucose, diabetes mellitus, dyslipidemia, metabolic syndrome, coronary artery disease, sleep apnea, and nonalcoholic fatty liver disease as well as an increased risk for certain cancers and indirectly through co-morbidities such as diabetes and hypertension, can lead to chronic kidney disease[10]. At five year follow up, Kramer et al[11] found that overweight and obese individuals had 20% and 40% risk of developing chronic kidney disease. Having a higher baseline BMI can serve as an independent risk factor for end stage kidney disease[12]. The long term effects of obesity on the solitary kidney of a kidney donor are still uncertain[7]. This risk factor increases the risk of developing other co-morbid conditions such as diabetes mellitus, hypertension, or even proteinuria which can together compromise the function of their solitary kidney. Since more than half of the living kidney donors in the past decade fall in the category of overweight or obese, concerns regarding post donation outcome should be taken into account. Obese donors should be counseled regarding their long term risk of developing the various aforementioned co-morbid conditions and regarding implementation of lifestyle modifications to try to decrease their risk. Due to the different BMI criteria of exclusion at different transplant centers, analysis revealed 1992 donors who were moderately to morbidly obese. Although a low net percentage of 4.2%, special concern and follow up should be dedicated to this subpopulation as they are likely to be of highest risk for subsequent co-morbidities. Short term outcomes of obese living kidney donors have shown increased wound related complications and longer operative times[6,13]. A recent meta-analysis found that operative duration, rise in serum creatinine, and conversion rate from laparoscopic donor nephrectomy to open procedure favored the lower BMI than higher BMI group[14]. Six months to one year follow up did not show any significant differences in renal function, creatinine levels, microalbuminuria, or hypertension when obese kidney donors were compared to their non-obese counterparts[6,15-17]. Still uncertain are the very long term outcomes in obese living kidney donors. At a mean of 11 year follow up, obese donors had an increased risk of developing hypertension and dyslipidemia, two important risk factors for coronary artery disease, however these were not found to be exacerbated by nephrectomy[17].
When a potential kidney donor comes for evaluation, certain donor demographics should be taken into consideration. For the obese kidney donor, especially in the 35-49 years old category cumulative donor health risk, may be increased throughout time. Biologically related and partner/spouses were more likely to be in the obese donor categories. This trend may be a reflection of the donors’ willingness to do good for that close family member or loved one, blunting concern about themselves and their potential risks associated with their BMI.
Black and Hispanic females and Hispanic males were more likely than Whites and Asians to be obese donors. Our findings for males in regard to ethnicity deviated from the national trends. Among those greater than 20 years old, data from NHANES reveals that Non-Hispanic blacks have the highest age-adjusted rates of obesity (49.5%) compared with Mexican Americans (40.4%), Hispanics (39.1%), and non-Hispanic whites (34.3%)[18]. In our study, however, Hispanic males were more likely to be in the obese groups when compared to Blacks. Hispanic females were less likely to be in the obese groups when compared to Black females. This trend in the male Black population could be due to fact that Blacks were being excluded in the predonation period. Many Black obese donors may nevertheless end up being excluded because of obesity-related complications that have already developed prior to donation. In fact, in the pre-donation period, the majority of moderately to morbidly obese potential living kidney donors who were excluded were Black[19]. Of further concern is that Hispanics and Blacks are at highest risk for hypertension and kidney disease. Being of Hispanic ethnicity, increased the risk of end stage renal disease and progression of end stage renal disease, partially explained by higher prevalence of diabetes in this group[20]. Blacks as well have a higher prevalence of ESRD[17,21]. Informed consent and risk stratification of these donors in the predonation evaluation period is imperative.
The UNOS/OPTN database is the only national database for living kidney donors. As with all databases, there are limitations. There can be under reporting and missing donor data as well as inaccurately entered data. Ten point seven percent of the total donors had missing BMI and less than 1% had implausible data entries as discussed in the methods section. A strength is the large number of living kidney donors and the diversity of donors in the database. Another limitation of this study is that the database does not capture how many potential living kidney donors were excluded due to obesity or obesity related complications in the predonation evaluation period, as more than fifty percent of United States transplant centers are excluding those with BMI greater than 35 kg/m2. Prior studies have shown that obesity is serving as a potential barrier to kidney donation[19,22]. Although we do see an upward trend in the overweight and mildly obese paralleling the national trend, knowing this predonation information would allow us to demonstrate an accurate trend of kidney donors in this higher BMI category.
The obesity epidemic is affecting the living kidney donor population. Paralleling the national rise, there is an increase in the overweight and mildly obese kidney donors. In addition, there still remains a small number of moderate to morbidly obese donors who are allowed to donate. Care is advised when allowing donors in this BMI category to donate due to the uncertainty of the long term outcomes. On a national level, continued awareness and implementation of programs to limit the obesity crisis are needed.
We acknowledge the Organ Procurement and Transplantation Network for providing the database for this research. The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy of or interpretation by the OPTN. The authors thank the Janet and John D. Raggio Institute.
The obesity epidemic has been increasing over the past three decades. Transplant centers across the United States use different criteria in determining donor exclusion based on body mass index (BMI). There is a national shortage of living kidney donors. Due to the shortage of living kidney donors, some transplant centers may be less stringent on the obesity criteria. However, the safety of potential donors must come first. Long term outcomes for obese living kidney donors are still uncertain. The primary aim of the study was to analyze the national temporal trends associated with BMI and living kidney donation over the past 13 years. In addition, the authors wanted to examine the association between live kidney donor BMIs and age, gender, race/ethnicity, relationship to the kidney transplant recipient, education status, transplant region, and year.
This study allows us to see the temporal trend of BMI and living kidney donation. It highlights certain donor characteristics which should be taken into account when a potential kidney donor is evaluated. Since most of the living kidney donors fall in the overweight or obese categories, hence contributing to the majority of the living kidney donor encounters, and due to uncertain long term outcomes in the obese living kidney donor, this study highlights the importance of discussing all possible long term co-morbidities and complications associated with obesity during an initial donor evaluation.
By analyzing the temporal trend of BMI and living kidney donation, the authors were able to determine where the authors stand in relationship to the obesity epidemic. The authors found that 63.6% of living kidney donors over the past thirteen years have spanned the overweight to obese categories. The increase in the overweight and mildly obese living kidney donors in the study parallels the national increase in obesity trends. Seeing that more than half of the living kidney donors fall in the overweight to obese categories, something needs to be done to address the obesity epidemic. In addition, there were 1992 in the moderate/morbidly obese group who were allowed to donate. Although a low net percentage of 4.2%, special concern and follow up should be dedicated to this subpopulation as they are likely to be of highest risk for subsequent co-morbidities. In addition, the authors found that donors 35-49 years of age, hispanic males or females and black females, those with high school diploma or general education degree, and biologically related or partner/spouses were more likely to be obese. These certain donor demographics should be taken into account when a potential kidney donor comes in for evaluation.
The authors see that more of the donors are overweight and obese and still there are a minority of kidney donors who are moderate to morbidly obese. Caution should be taken when allowing these donors to donate due to uncertain long term kidney donation outcomes in this subpopulation. The first priority in donor evaluation should be to assess safety and to discuss all potential long term comorbidities and complications with this subpopulation. In addition, a call for national and international programs is needed to stop the obesity epidemic.
This is a well written paper.
P- Reviewer: Nechifor G, Saleem M S- Editor: Ji FF L- Editor: A E- Editor: Jiao XK
| 1. | Barry CL, Gollust SE, Niederdeppe J. Are Americans ready to solve the weight of the nation? N Engl J Med. 2012;367:389-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 2. | OPTN Policies and Bylaws For Living Kidney Donation. 2015. Available from: http://optn.transplant.hrsa.gov/PoliciesandBylaws2/policies/pdfs/policy_172.pdf. |
| 3. | OPTN/UNOS Living Kidney Donor Report. 2015. Available from: http://optn.transplant.hrsa.gov/CommitteeReports/board_main_LivingDonorCommittee_11_14_2012_11_34.pdf. |
| 4. | Mandelbrot DA, Pavlakis M, Danovitch GM, Johnson SR, Karp SJ, Khwaja K, Hanto DW, Rodrigue JR. The medical evaluation of living kidney donors: a survey of US transplant centers. Am J Transplant. 2007;7:2333-2343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 224] [Cited by in RCA: 215] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 5. | Organ Procurement and Transplantation Network Annual Report. 2015. Available from: http: //optn.transplant.hrsa.gov/latestData/rptData.asp. |
| 6. | Heimbach JK, Taler SJ, Prieto M, Cosio FG, Textor SC, Kudva YC, Chow GK, Ishitani MB, Larson TS, Stegall MD. Obesity in living kidney donors: clinical characteristics and outcomes in the era of laparoscopic donor nephrectomy. Am J Transplant. 2005;5:1057-1064. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 114] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 7. | Nogueira JM, Weir MR, Jacobs S, Breault D, Klassen D, Evans DA, Bartlett ST, Cooper M. A study of renal outcomes in obese living kidney donors. Transplantation. 2010;90:993-999. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 57] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 8. | Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999-2000. JAMA. 2002;288:1723-1727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4389] [Cited by in RCA: 4036] [Article Influence: 175.5] [Reference Citation Analysis (0)] |
| 9. | Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA. 2010;303:235-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4734] [Cited by in RCA: 4472] [Article Influence: 298.1] [Reference Citation Analysis (0)] |
| 10. | Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998;101:518-525. [PubMed] |
| 11. | Kramer H, Luke A, Bidani A, Cao G, Cooper R, McGee D. Obesity and prevalent and incident CKD: the Hypertension Detection and Follow-Up Program. Am J Kidney Dis. 2005;46:587-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 260] [Cited by in RCA: 276] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 12. | Hsu CY, McCulloch CE, Iribarren C, Darbinian J, Go AS. Body mass index and risk for end-stage renal disease. Ann Intern Med. 2006;144:21-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 934] [Cited by in RCA: 983] [Article Influence: 51.7] [Reference Citation Analysis (0)] |
| 13. | Pesavento TE, Henry ML, Falkenhain ME, Cosio FG, Bumgardner GL, Elkhammas EA, Pelletier RP, Ferguson RM. Obese living kidney donors: short-term results and possible implications. Transplantation. 1999;68:1491-1496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Lafranca JA, Hagen SM, Dols LF, Arends LR, Weimar W, Ijzermans JN, Dor FJ. Systematic review and meta-analysis of the relation between body mass index and short-term donor outcome of laparoscopic donor nephrectomy. Kidney Int. 2013;83:931-939. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 15. | Reese PP, Feldman HI, Asch DA, Thomasson A, Shults J, Bloom RD. Short-term outcomes for obese live kidney donors and their recipients. Transplantation. 2009;88:662-671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 55] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 16. | Aggarwal N, Porter AC, Tang IY, Becker BN, Akkina SK. Creatinine-based estimations of kidney function are unreliable in obese kidney donors. J Transplant. 2012;2012:872894. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | Tavakol MM, Vincenti FG, Assadi H, Frederick MJ, Tomlanovich SJ, Roberts JP, Posselt AM. Long-term renal function and cardiovascular disease risk in obese kidney donors. Clin J Am Soc Nephrol. 2009;4:1230-1238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 61] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 18. | Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA. 2012;307:491-497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3909] [Cited by in RCA: 3855] [Article Influence: 296.5] [Reference Citation Analysis (0)] |
| 19. | Sachdeva M, Sunday S, Israel E, Varghese J, Rosen L, Bhaskaran M, Molmenti EP, Mattana J. Obesity as a barrier to living kidney donation: a center-based analysis. Clin Transplant. 2013;27:882-887. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 20. | Peralta CA, Shlipak MG, Fan D, Ordoñez J, Lash JP, Chertow GM, Go AS. Risks for end-stage renal disease, cardiovascular events, and death in Hispanic versus non-Hispanic white adults with chronic kidney disease. J Am Soc Nephrol. 2006;17:2892-2899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 120] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 21. | Hsu CY, Lin F, Vittinghoff E, Shlipak MG. Racial differences in the progression from chronic renal insufficiency to end-stage renal disease in the United States. J Am Soc Nephrol. 2003;14:2902-2907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 333] [Article Influence: 15.9] [Reference Citation Analysis (0)] |