Published online Feb 18, 2023. doi: 10.5500/wjt.v13.i2.28
Peer-review started: September 3, 2022
First decision: October 31, 2022
Revised: January 5, 2023
Accepted: January 8, 2023
Article in press: February 8, 2023
Published online: February 18, 2023
Processing time: 165 Days and 22.1 Hours
Patients with end-stage renal disease in Greece are facing long waiting times to receive a kidney transplant from a deceased donor. Living kidney donation offers a valuable alternative that provides optimal outcomes and significantly expands the donor pool but still remains relatively underutilised. Developments around the world in the field of kidney transplantation mandate a change in current practice to include additional options for living donation through paired exchange, antibody-incompatible transplantation and other strategies, following careful consideration of the cultural and ethical factors involved in these complex clinical decisions. An increase in living donation rates may be achieved in several ways, including targeted campaigning to overcome potential barriers. Educating clinicians on transplantation will prove as equally important as informing patients and prospective donors but requires training and resources. Adoption of established practices and implementation of new strategies must be tailored to the needs of the Greek donor and recipient population. Local beliefs about donation, perception of associated risk and other social characteristics must be considered in the design of future strategies. Facilitating living donation in a safe environment with appropriate donor and recipient education will form the solid foundation of a new era of kidney transplantation in Greece.
Core Tip: Living kidney donation is the driving force behind every successful kidney transplant programme worldwide. In Greece, in particular, it accounts for nearly half of performed transplants annually. Its role is of paramount importance since deceased donor kidney transplant waiting times are currently unacceptably long. Paired exchange and other options will form the basis to expand the donor pool and facilitate future developments in the field.
- Citation: Karydis N, Maroulis I. Changing landscape in living kidney donation in Greece. World J Transplant 2023; 13(2): 28-35
- URL: https://www.wjgnet.com/2220-3230/full/v13/i2/28.htm
- DOI: https://dx.doi.org/10.5500/wjt.v13.i2.28
Living kidney donation remains the optimal source of kidney transplants worldwide, despite advances in deceased donor organ utilisation and preservation. Living donor kidneys offer excellent long-term outcomes in terms of patient and graft survival[1,2]. Apart from this, living donation has gradually served as the basis for expansion and development of novel patient pathways in kidney transplantation. Antibody-incompatible transplant programmes have been largely successful, enabling discontinuation of dialysis and prolongation of survival in highly sensitised recipients[3,4]. Kidney exchange pro
National living donor programmes share many common features but also differ in many ways, even among countries with obvious geographical and cultural similarities. The plausible explanation lies in the complexities of healthcare systems to identify and utilise the maximum number of potential donors, both deceased and living. Furthermore, disparities in training and education may inevitably magnify the differences in donation and transplant rates. Greece is currently entering a new era in kidney transplantation, in particular living donor transplantation, with major new developments that could substantially increase the transplant rates.
Although donation and transplant rates are low in Greece at approximately five deceased donors per million population[7], the actual living donor kidney transplant rate, ranging between 38%-50% of all transplants the last 5 years, is easily comparable to countries with well-established deceased donor and living donor programmes[8]. This simple observation justifies the argument that an appropriate expansion of the living donor pool could, at least to some extent, “generate” many more high-quality kidney grafts. Additionally, it provides important clues regarding the intention of the Greek population to donate organs albeit usually within the limits of close or extended family.
Deceased donor kidney transplantation currently suffers from unacceptably long waiting times due to multifactorial long-standing issues that effectively limit the number of brain-dead donors who proceed to donation. The obvious advantage of living donation over deceased kidney donation is the relative independence from complicated donor pathways, lack of suitable infrastructure, staffing issues, limitations of laboratory workflows and cultural trends towards donation in general. The latter has been studied in a relatively small sample of an urban population but has provided very useful insight into the attitudes towards organ donation in Greece[9]. Although the vast majority (90.0%-98.0%) of participants demonstrated a high level of understanding around brain death, organ donation and transplantation, only 3.8% were formally registered with the national organ donor register. Half of the participants would be willing to donate the organs of a relative, however more than half would feel guilty doing so. Another emerging concern in this survey was the fear about the process of organ removal, which probably reflects a lack of trust in the processes and regulatory framework related to organ donation in general. Interestingly, religious beliefs did not emerge as significant potential obstacles to donation, and willingness to donate was actually higher among Greek Orthodox participants (63.7%) than the study sample average (48.3%).
Other significant advantages of living over deceased donation include shorter workup times for living donor pairs, presumably due to the willingness of donors and recipients alike to proceed with a transplant, improved immunological matching between family members, ability to proceed with incompatible transplants and finally the relative ease to manage logistical issues, from access to the operating theatre to specialist perioperative and postoperative care. Deceased donation rates are expected to grow over the next few years in Greece, owing to changes in legislation and the investment of financial and staffing resources to national and local transplant coordination. Until then, living kidney donors will likely drive the country into the new era of transplantation by offering invaluable organs to their respective recipients and by acting as ambassadors of donation and transplantation in the general population. The latter may be more impactful on the public’s attitude towards issues surrounding transplantation in general but also requires a coordinated approach led by donors and clinicians in equal parts. The United Network for Organ Sharing has developed a volunteer programme with the primary goal of raising awareness and educating prospective donors through real-life experiences of other donors[10]. Becoming an ambassador of living donation involves an initial orientation and education phase, after which living donors share their personal experience through local events, the United Network for Organ Sharing website and social media. Similar programmes are being developed around the world by national transplant organisations, such as the United Kingdom’s National Health Service Blood and Transplant, and are expected to improve communication between transplant professionals and the public.
Highlighting the successes of living donation as well as the safety of modern techniques[11], i.e., minimally invasive donor nephrectomy, quick recovery time, reduced postoperative pain, short length of hospital stay, minimal postoperative complications and excellent long-term outcomes in terms of general health and donor survival, is central to any communication relating to transplantation to strengthen the public’s trust. Transparency and publication of interval donation and transplant-related statistics on a scheduled basis in an easily accessible public domain will eliminate suspicion and fear around unacceptable practices that have been reported elsewhere in the world from time to time.
In the recent past, the norm in living kidney donation would be a donor who would come forward and donate to a specified, compatible recipient, usually a member of their close or extended family. Alth
The boundaries of living donation have been pushed significantly to make every living donor kidney count for patients in need of an organ, either directly or indirectly[12]. In this context, every suitable living donor should proceed either with a direct or indirect transplant to their intended recipient, which has allowed the development of complex paired exchange networks, mostly but not exclusively geographically confined within their countries. In some instances, these complex networks “interact” with deceased donor pathways to create novel opportunities for highly sensitised or difficult-to-transplant patients who would otherwise not have any chance to receive a kidney transplant. The notion of a “donor-recipient” pair is becoming less clear in this reality, and programmes around the world are being challenged to keep up with developments.
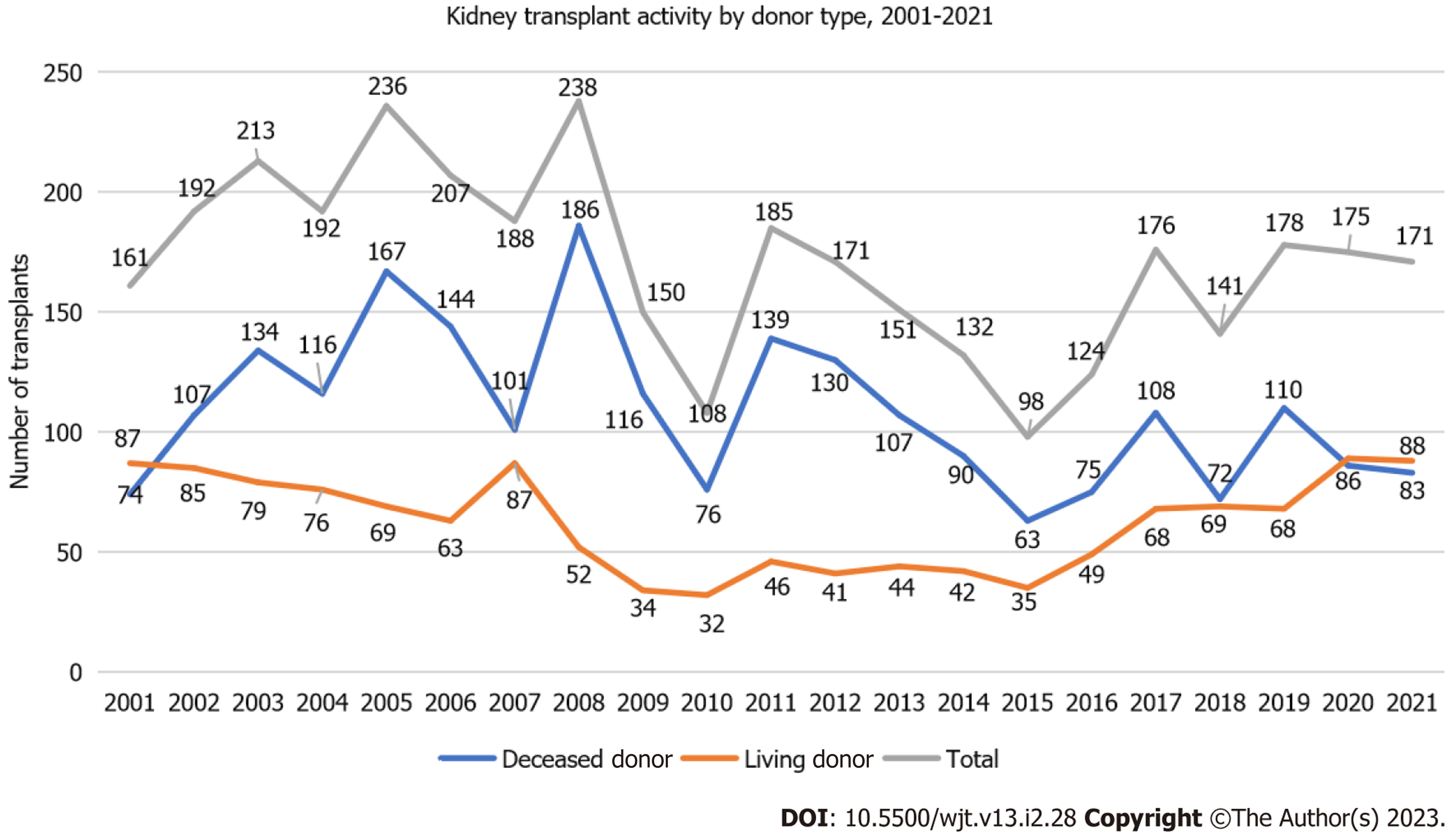
The landscape of living kidney donation has significantly changed in Greece over the last few years, though there is still a long way to cover in certain areas. However, most efforts have concentrated on encouraging living donation, thus the conditions to allow living kidney transplantation to flourish are already in place. Official data from the National Transplant Organisation indicate a rising number of living donor kidney transplants (Figure 1), despite adverse circumstances such as the coronavirus disease 2019 pandemic.
A direct living donor transplant is in many ways the “gold” standard of care. It allows for an immunologically straightforward kidney transplant, in the context of blood group (ABO) and human leukocyte antigen (HLA) compatibility between donor and recipient. Until recently, such transplants were only allowed within extended families, excluding several other types of living donors. The last decade has seen significant legislative changes that have permitted directed donation from unrelated donors, following a formal approval process, which has also been further simplified in the last few years. We consider this change a fundamentally positive step into the new era of transplantation, although official data on its practical applicability so far are lacking. To our knowledge, unrelated undirected, i.e., altruistic, kidney donation, has not yet taken place in Greece due to legislative restrictions. From a practical perspective, the extent to which such donation would make an actual difference in transplant rates is probably very limited, based on cultural perceptions. Indeed, a quite thorough study on the patterns of blood donation in Greece revealed that the concept of “need” is a stronger motivator than the sense of altruistic “offer” for blood donors[13].
The emergence of unrelated donors has inevitably introduced new challenges for the transplant community. Quite a few donors will have an incompatible blood group with the recipient and/or a positive immunological crossmatch. There is sufficient evidence and experience worldwide to suggest that ABO-incompatible kidney transplants have comparable graft and patient outcomes and should be routinely considered as a valid option in suitable pairs[14]. Blood group-incompatible kidney tran
The issue of antibody-incompatible kidney transplantation has a few possible solutions, all of which are available in Greece, albeit still underdeveloped to a variable extent. These solutions include paired exchange or kidney sharing schemes (programmes of kidney exchange between incompatible donor-recipient pairs) and have transformed living donor kidney transplantation over the last two decades[15,16]. Despite several points of criticism and concerns from both patients and clinicians, the huge success of these programmes has established their role in daily practice. Even well-established and active antibody-incompatible programmes have now shrunk to serve only a small number of patients that cannot be transplanted through paired exchange. In the United Kingdom, for example, the combined number of ABO- and HLA-incompatible kidney transplants has declined gradually from 171 in 2012 to 25 in 2021, as shown graphically in the most recent annual activity report[17].
Engagement from all participating units in a country is obviously of paramount importance to allow the creation of a candidate pool large enough to facilitate ABO and HLA matching. Long chains of such pairs are possible, although logistical issues should be considered to minimise ischaemia times and optimise outcomes. The combination of kidney exchange with altruistic donation has enabled kidney transplantation for highly sensitised or difficult-to-match patients at the end of commonly long chains. In-centre kidney exchange has taken place in Greece in the recent past, however this is potentially more complicated from a logistical perspective, e.g., access to operating theatres, where nephrectomies and transplants all take place on the same day. Between-centres kidney exchange poses its own challenges, but certainly still remains an underutilised option. With appropriate communication and standardisation of donor and recipient procedures, as well as HLA typing and matching, transplant units in Greece could easily transition into a new era of collaboration.
Building a large enough pool possibly requires a radically new approach to living donation alto
Incompatible donors are legally allowed to donate to the deceased donor waiting list, in exchange for their recipient to be prioritised on the waiting list to receive the first available deceased donor kidney. Although there are reasonable concerns around matching the quality of a living donor kidney to a kidney from a deceased donor, in terms of age, medical background, cause of death and terminal kidney function, it remains a valid option for some recipients, compared to a long average waiting time of 8 years. Recipients that fall into this prioritisation list are also allowed to turn down an offer that does not “match” their living donor. Although this is a relatively new option, it is becoming increasingly popular among incompatible pairs, and 17 pairs have been successfully transplanted so far through this scheme.
Antibody-incompatible transplantation remains a popular option, particularly for ABO-incompatible pairs. The literature clearly supports ABO-i kidney transplantation over remaining on haemodialysis[18], thus we believe every transplant unit in Greece could develop an ABO-i programme to enable transplantation for the relatively small number of patients that will proceed with this form of transplant, at least until a robust national paired exchange programme becomes established. Clearly, some centres will accumulate greater expertise in this field, but smaller units could enable transplants with lower anti-A or anti-B titres at the early stages of their development[19]. HLA-incompatible transplantation, although proven superior to haemodialysis[4], remains a challenging procedure with significant risks for the recipients. Early antibody-mediated rejection possibly contributes to inferior graft survival up to 5 years post-transplant[20]. Enhanced immunosuppression may lead to serious bacterial and viral complications that may threaten both graft and patient survival[14]. Indeed, a recent meta-analysis showed increased mortality risk in ABO-i recipients up to 8 years post-transplant[20]. At the same time, the actual number of potential ABO-incompatible transplants in Greece may not adequately justify the risks at this point in time.
Transplant units need to adapt and invest in the novel options that are now available to our recipients, particularly under the burden of very long waiting times on the deceased donor list. Direct or “indirect” living kidney donation is key to the existence and development of all the above options. Clearly, the kind intentions of every living donor should be honoured in the best possible way after detailed discussion with both the donor and the recipient[21]. The mental and psychological process involved in every aspect of living donation deserves dedication in time and resources to ensure donors will not be discouraged by logistical complexities or delays. Training and education of all staff involved is of utmost importance to provide a seamless and positive experience to donors, who will become advocates of living donation in the community. Emphasizing the safety and quick recovery after living donation with minimally invasive techniques as well as the excellent long-term health outcomes for donors compared to the age-matched general population are also essential to reassure the public and promote living donation[22].
Introducing new concepts around living kidney donation in Greece should also start early to allow for adequate public discussion and engagement. Donation from offspring to parent rarely takes place in Greece. Although any adult individual may be considered for donation by law, there is reluctance even among transplant clinicians to consider young donors. Donation at an early age is a well-established and accepted practice in other countries, with excellent psychological and medical outcomes for both donors and recipients. In 2021 in the United Kingdom, 20% of all living donors were aged 18-34[17]. During the same period, only one donor (1%) was younger than 30 years in Greece. The age distribution of living donors over the last few years is depicted in Table 1, where it becomes evident that most donors are middle-aged or older. Clearly, widening the age criteria for donation in transplant units with appropriate consenting of younger donors will enable more transplants in the future.
| Age group | Number of living donors by year | |||||
| 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | |
| 20-30 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (1) |
| 31-40 | 2 (4) | 4 (6) | 5 (7) | 2 (3) | 1 (1) | 8 (9) |
| 41-50 | 9 (18) | 9 (13) | 16 (23) | 19 (28) | 19 (21) | 12 (13) |
| 51-60 | 14 (29) | 24 (35) | 16 (23) | 22 (32) | 34 (38) | 34 (37) |
| 61-70 | 19 (39) | 22 (32) | 27 (40) | 20 (3) | 23 (26) | 24 (27) |
| 71-90 | 5 (10) | 9 (14) | 5 (7) | 5 (7) | 12 (14) | 12 (13) |
| Total | 49 (100) | 68 (100) | 69 (100) | 68 (100) | 89 (100) | 91 (100) |
Transplant candidates are often reluctant to approach and recruit living donors. Separating the advocate from the patient has proved to be an effective strategy but needs appropriate training[23]. The introduction of programmes aiming to facilitate identification of potential donors and elicit their interest to proceed with donation should form a part of a national strategy. Examples of successful imple
Donating indirectly to someone via a waiting list “voucher” is an emerging concept worldwide that still remains to be validated but certainly shows the direction of modern transplantation and proves the concept that every living donor deserves to be “utilised” in the best possible way. This approach usually applies to donors that would probably be too old to donate when their recipient would actually need a kidney transplant, e.g., a grandfather donating to their grandchild via the general waiting list. Simply put, transplant vouchers provide a means to overcome chronological incompatibility between donation and transplantation. The donor donates in the deceased donor list and the prospective recipient receives a “voucher” or a “priority ticket” that can be redeemed for a future transplant that will probably take place years later[27].
Reducing financial barriers for living donation and accounting for potential income losses remains a matter of debate for many years across the globe. Despite concerns around commercialisation of donation, a rational approach to protect and support prospective donors in their decision was proposed a few years ago by the American Society of Transplantation’s Live Donor Community of Practice after careful and systematic exploration of factors such as employment, insurance and medical cost of donation. It became clear that the creation of a standardised financial toolkit for donors, adapted to each country’s requirements and limitations is a perfectly actionable way to encourage living donation and remove any sense of insecurity in the process before and after donation[28].
Lastly, but equally important, we believe that further research is needed to understand living donation trends and perceptions in the public. These may vary significantly between different parts of the world. Therefore, extrapolation of conclusions from previous work elsewhere should be done with caution. Focus groups with patients and donors at a local level will shed light on various cultural barriers that could be potentially resolved with appropriate targeted campaigns. Additionally, transplant clinicians will have a unique opportunity to understand what matters most for living donors and how to better support them through the journey of donation[29,30].
Living donor kidney transplantation is undergoing a phase of transformation in Greece. New legislation and crucial changes in transplant policies pave the way for expansion of the donor pool, especially through living donation. The role of transplant professionals in this process of change and adaptation is to lead the developments in a safe and productive way for the benefit of patients. We have a duty to campaign for all the above and extend this knowledge to all parts involved in transplantation, from central organisation to local patient groups. Through living donation we have a unique opportunity to make progress and catch up with the growing need for more transplants in Greece by creating a positive environment in the community around transplantation in general. Every prospective living donor deserves to receive education, delivered responsibly, and high-quality care in every step of the way to donation, knowing that their generous offer will be fully appreciated. Clinicians on the other hand need to continue to explore ways that will encourage living donors to come forward. Identifying potential barriers to donation is the first important step into the future.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Transplantation
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Dayal C, South Africa; He GF, China; Sureshkumar KK, United States; Zhou ST, China S-Editor: Liu GL L-Editor: Filipodia P-Editor: Liu GL
| 1. | Hart A, Lentine KL, Smith JM, Miller JM, Skeans MA, Prentice M, Robinson A, Foutz J, Booker SE, Israni AK, Hirose R, Snyder JJ. OPTN/SRTR 2019 Annual Data Report: Kidney. Am J Transplant. 2021;21 Suppl 2:21-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 282] [Article Influence: 70.5] [Reference Citation Analysis (0)] |
| 2. | Medin C, Elinder CG, Hylander B, Blom B, Wilczek H. Survival of patients who have been on a waiting list for renal transplantation. Nephrol Dial Transplant. 2000;15:701-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 63] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Montgomery RA. Renal transplantation across HLA and ABO antibody barriers: integrating paired donation into desensitization protocols. Am J Transplant. 2010;10:449-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 125] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 4. | Orandi BJ, Luo X, Massie AB, Garonzik-Wang JM, Lonze BE, Ahmed R, Van Arendonk KJ, Stegall MD, Jordan SC, Oberholzer J, Dunn TB, Ratner LE, Kapur S, Pelletier RP, Roberts JP, Melcher ML, Singh P, Sudan DL, Posner MP, El-Amm JM, Shapiro R, Cooper M, Lipkowitz GS, Rees MA, Marsh CL, Sankari BR, Gerber DA, Nelson PW, Wellen J, Bozorgzadeh A, Gaber AO, Montgomery RA, Segev DL. Survival Benefit with Kidney Transplants from HLA-Incompatible Live Donors. N Engl J Med. 2016;374:940-950. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 275] [Article Influence: 30.6] [Reference Citation Analysis (0)] |
| 5. | Furian L, Nicolò A, Di Bella C, Cardillo M, Cozzi E, Rigotti P. Kidney exchange strategies: new aspects and applications with a focus on deceased donor-initiated chains. Transpl Int. 2020;33:1177-1184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Wall AE, Veale JL, Melcher ML. Advanced Donation Programs and Deceased Donor-Initiated Chains-2 Innovations in Kidney Paired Donation. Transplantation. 2017;101:2818-2824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | European Parliamentary Research Service (EPRS). Organ donation and transplantation. Facts, figures and European Union action-April 2020 briefing. [Internet] [cited 20 December 2022]. Available from: https://www.europarl.europa.eu/thinktank/en/document/EPRS_BRI(2020)649363. |
| 8. | NHS Blood and Transplant (NHSBT). Annual report on kidney transplantation 2020-2021. [Internet] [cited 20 December 2022]. Available from: https://www.odt.nhs.uk/statistics-and-reports/organ-specific-reports/. |
| 9. | Georgiadou E, Sounidakis N, Mouloudi E, Giaglis P, Giasnetsova T, Marmanidou K, Gritsi-Gerogianni N. Attitudes and behavior toward organ donation in Greece. Transplant Proc. 2012;44:2698-2701. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | United Network for Organ Sharing (UNOS). UNOS ambassadors. [Internet] [cited 15 December 2022]. Available from: https://unos.org/community/unos-ambassadors/. |
| 11. | Liyanage L, Muzaale A, Henderson M. The true risk of living kidney donation. Curr Opin Organ Transplant. 2019;24:424-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Kute VB, Prasad N, Shah PR, Modi PR. Kidney exchange transplantation current status, an update and future perspectives. World J Transplant. 2018;8:52-60. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 13. | Kalargirou AA, Beloukas AI, Kosma AG, Nanou CI, Saridi MI, Kriebardis AG. Attitudes and behaviours of Greeks concerning blood donation: recruitment and retention campaigns should be focused on need rather than altruism. Blood Transfus. 2014;12:320-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 14. | de Weerd AE, Betjes MGH. ABO-Incompatible Kidney Transplant Outcomes: A Meta-Analysis. Clin J Am Soc Nephrol. 2018;13:1234-1243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 98] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 15. | Kher V, Jha PK. Paired kidney exchange transplantation - pushing the boundaries. Transpl Int. 2020;33:975-984. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 16. | Biró P, Haase-Kromwijk B, Andersson T, Ásgeirsson EI, Baltesová T, Boletis I, Bolotinha C, Bond G, Böhmig G, Burnapp L, Cechlárová K, Di Ciaccio P, Fronek J, Hadaya K, Hemke A, Jacquelinet C, Johnson R, Kieszek R, Kuypers DR, Leishman R, Macher MA, Manlove D, Menoudakou G, Salonen M, Smeulders B, Sparacino V, Spieksma FCR, Valentín MO, Wilson N, van der Klundert J; ENCKEP COST Action. Building Kidney Exchange Programmes in Europe-An Overview of Exchange Practice and Activities. Transplantation. 2019;103:1514-1522. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 54] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 17. | NHS Blood and Transplant (NHSBT). Annual Activity Report 2021-2022. [Internet] [cited 15 December 2022]. Available from: https://www.odt.nhs.uk/statistics-and-reports/annual-activity-report/. |
| 18. | Massie AB, Orandi BJ, Waldram MM, Luo X, Nguyen AQ, Montgomery RA, Lentine KL, Segev DL. Impact of ABO-Incompatible Living Donor Kidney Transplantation on Patient Survival. Am J Kidney Dis. 2020;76:616-623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 19. | Lo P, Sharma A, Craig JC, Wyburn K, Lim W, Chapman JR, Palmer SC, Strippoli GF, Wong G. Preconditioning Therapy in ABO-Incompatible Living Kidney Transplantation: A Systematic Review and Meta-Analysis. Transplantation. 2016;100:933-942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 52] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 20. | Scurt FG, Ewert L, Mertens PR, Haller H, Schmidt BMW, Chatzikyrkou C. Clinical outcomes after ABO-incompatible renal transplantation: a systematic review and meta-analysis. Lancet. 2019;393:2059-2072. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 95] [Article Influence: 15.8] [Reference Citation Analysis (1)] |
| 21. | Lentine KL, Lam NN, Segev DL. Risks of Living Kidney Donation: Current State of Knowledge on Outcomes Important to Donors. Clin J Am Soc Nephrol. 2019;14:597-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 104] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 22. | Krishnan N, Mumford L, Lipkin G, Gill P, Fletcher S, Dasgupta I, Ryan R, Raymond NT. Comparison of Medium-term Outcomes of Living Kidney Donors With Longitudinal Healthy Control in the United Kingdom. Transplantation. 2020;104:e65-e74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 23. | Garonzik-Wang JM, Berger JC, Ros RL, Kucirka LM, Deshpande NA, Boyarsky BJ, Montgomery RA, Hall EC, James NT, Segev DL. Live donor champion: finding live kidney donors by separating the advocate from the patient. Transplantation. 2012;93:1147-1150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 111] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 24. | Live Donor Champion Program. [Internet] [cited 15 December 2022]. Available from: https://www.hopkinsmedicine.org/transplant/patient_information/Live-donor-program.html. |
| 25. | Caruso C, Zell C, Swaytha G, Angela B, Sarah S, Elaine L, Susan P, Travis W, Abhinav H. UPMC Living Donor Champion Program [abstract]. [Internet] [cited 15 December 2022]. Available from: https://atcmeetingabstracts.com/abstract/upmc-living-donor-champion-program/. |
| 26. | LaPointe Rudow D, Geatrakas S, Armenti J, Tomback A, Khaim R, Porcello L, Pan S, Arvelakis A, Shapiro R. Increasing living donation by implementing the Kidney Coach Program. Clin Transplant. 2019;33:e13471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 27. | Veale JL, Nassiri N, Capron AM, Danovitch GM, Gritsch HA, Cooper M, Redfield RR, Kennealey PT, Kapur S. Voucher-Based Kidney Donation and Redemption for Future Transplant. JAMA Surg. 2021;156:812-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 28. | Tushla L, Rudow DL, Milton J, Rodrigue JR, Schold JD, Hays R; American Society of Transplantation. Living-Donor Kidney Transplantation: Reducing Financial Barriers to Live Kidney Donation--Recommendations from a Consensus Conference. Clin J Am Soc Nephrol. 2015;10:1696-1702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 96] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 29. | Hanson CS, Ralph AF, Manera KE, Gill JS, Kanellis J, Wong G, Craig JC, Chapman JR, Tong A. The Lived Experience of "Being Evaluated" for Organ Donation: Focus Groups with Living Kidney Donors. Clin J Am Soc Nephrol. 2017;12:1852-1861. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 30. | Burnapp L, Van Assche K, Lennerling A, Slaats D, Van Dellen D, Mamode N, Citterio F, Zuidema W, Weimar W, Dor FJMF. Raising awareness of unspecified living kidney donation: an ELPAT view. Clin Kidney J. 2020;13:159-165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |