Published online Jul 18, 2022. doi: 10.5500/wjt.v12.i7.204
Peer-review started: December 12, 2021
First decision: February 15, 2022
Revised: April 6, 2022
Accepted: June 13, 2022
Article in press: June 13, 2022
Published online: July 18, 2022
Processing time: 214 Days and 17.6 Hours
Portal vein thrombosis (PVT) is a frequent complication occurring in 5% to 26% of cirrhotic patients candidates for liver transplantation (LT). In cases of extensive portal and or mesenteric vein thrombosis, complex vascular reconstruction of the portal inflow may become necessary for a successful orthotopic LT (OLT).
A 54-year-old male with history of cirrhosis secondary to schistosomiasis complicated with extensive portal and mesenteric vein thrombosis and severe portal hypertension who underwent OLT with portal vein-left gastric vein anastomosis.
We review the various types of PVT, the portal venous inflow reconstruction techniques.
Core Tip: The portal vein-variceal anastomosis is a challenging physiological non-anatomical technique of portal vein inflow reconstruction used and described rarely. Herein we review the various types of portal vein thrombosis, the portal venous inflow reconstruction techniques and describe an extraordinary case of portal vein-left gastric vein anastomosis for the portal inflow reconstruction during orthotopic liver transplantation.
- Citation: Gravetz A. Portal vein-variceal anastomosis for portal vein inflow reconstruction in orthotopic liver transplantation: A case report and review of literature. World J Transplant 2022; 12(7): 204-210
- URL: https://www.wjgnet.com/2220-3230/full/v12/i7/204.htm
- DOI: https://dx.doi.org/10.5500/wjt.v12.i7.204
Portal vein thrombosis (PVT) is a frequent and serious complication in patients with cirrhosis, with a prevalence ranging from 5% to 26%[1-4]. Patients with PV and/or mesenteric vein thrombosis while awaiting liver transplantation (LT) pose a significant surgical challenge for the reconstruction of the liver portal inflow, an essential step for successful orthotopic LT (OLT)[5-6]. While an end-to-end donor to recipient portal vein anastomosis is fashioned in the majority of liver transplant recipients, approximately 2% of recipients will require a complex vascular reconstruction due to inadequate recipient portal vein inflow[7,8].
The portal vein-variceal anastomosis is a challenging physiological non-anatomical technique of portal vein inflow reconstruction used and described rarely. Herein we review the various types of PVT, the portal venous inflow reconstruction techniques and describe an extraordinary case of portal vein-left gastric vein (LGV) anastomosis for the portal inflow reconstruction during OLT.
A 54-year-old male of Ethiopian origin who presented back in 1993 with variceal bleeding leading to a subsequent diagnosis of non-cirrhotic portal hypertension with splenomegaly and PVT with cavernous transformation.
The presence of granulomas and periportal fibrosis with preserved hepatic architecture on liver biopsy, together with positive serologic tests for antischistosomal antibodies and the patient origin suggested the diagnosis of hepatosplenic schistosomiasis. Further work up revealed protein C deficiency. Whether the patient received anthelmintic therapy upon diagnosis is unclear, however, prior to transplant no specific prophylactic treatment was administered as there was no evidence of active hepatic or systemic disease.
The patient in 1993 with variceal bleeding leading to a subsequent diagnosis of non-cirrhotic portal hypertension with splenomegaly and PVT with cavernous transformation.
The patient has none personal and family history.
Medical management of portal hypertension complications included diuretics, beta-blockers and periodic upper endoscopy with sclerotherapy and esophageal varices ligation. The patient eventually presented with severe decompensation and model for end-stage liver disease score of 25 necessitating LT.
His physical examination revealed signs of cachexia, jaundice, abdominal distention, umbilical hernia, caput medusa and impression of moderate to large volume ascites. Laboratory results showed total white blood cell count of 2.67 × 109/L, hemoglobin levels of 8 g/dL, platelet count of 33 × 109/L, international normalized ratio 2.43, total bilirubin of 7.5 mg/dL (and direct bilirubin of 3.6 mg/dL), serum sodium 140 mEq/L, serum creatinine 1.1 mg/dL and albumin levels of 2.5 gr/dL.
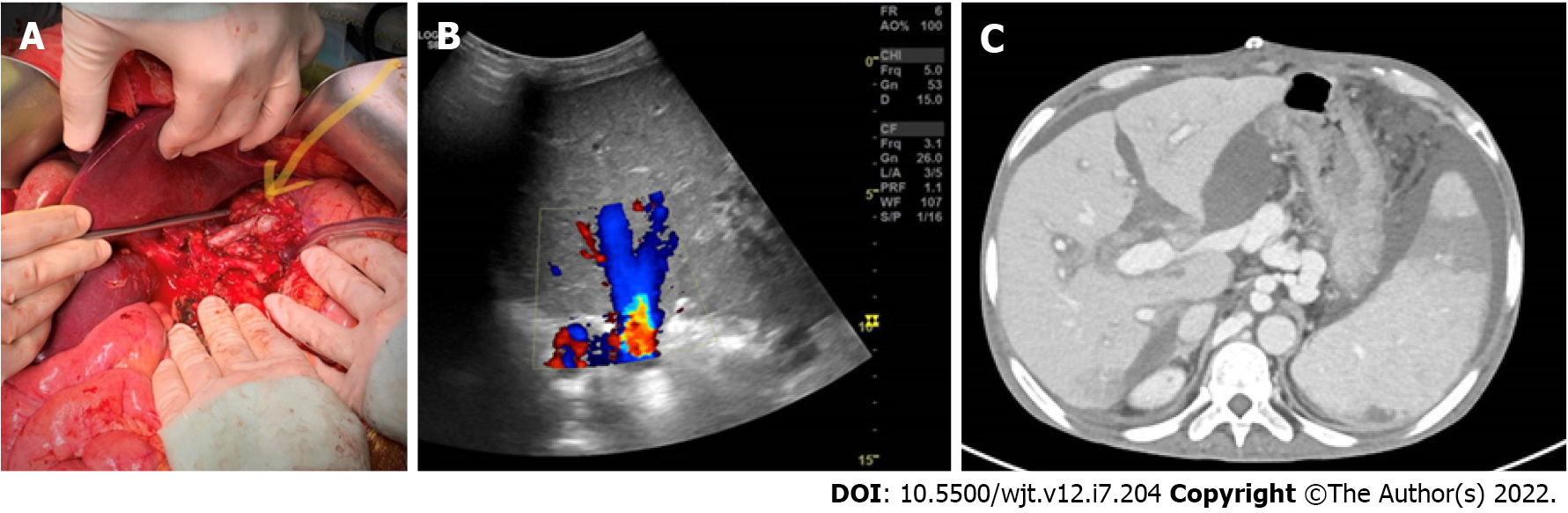
Preoperative esophagogastroduodenoscopy showed grade III esophageal varices and portal hypertensive gastropathy. Imaging revealed liver cirrhosis, extensive portal and mesenteric vein thrombosis with cavernous transformation, splenomegaly, with the spleen measuring 20 cm in diameter, and splanchnic varices comprising a large left gastric varix (Figure 1).
Over the years the patient gradually developed compensated liver fibrosis and cirrhosis as seen on various imaging modalities and worsening liver synthetic function.
The patient underwent OLT on April 2021 with piggyback venous outflow reconstruction and a portal vein-left gastric varix anastomosis for portal inflow. During the procedure the LGV was carefully dissected cephalad at the level of the mid lesser curvature of the stomach. Adequate venous flow was confirmed prior to creation of end-to-side porto-LGV anastomosis performed using polypropylene 5-0 suture (Figure 2A). Postoperative Doppler sonography documented patent anastomosis with adequate flow (Figure 2B), a finding which was confirmed by a contrast abdominal computed tomography performed on postoperative day 16 (Figure 2C).
The patient had a relatively benign postoperative course characterized by mild to moderate ascites, as anticipated, controlled initially with drainage and medical treatment and eventually resolved prior to discharge. Ten months post-operatively the patient is doing well with excellent liver function.
Schistosomiasis (bilharzia) is a chronic parasitic entero-pathogenic disease caused by a genus of trematodes commonly known as blood flukes[1]. Hepatic schistosomiasis represents the best known form of chronic disease and represents the most important cause of non-cirrhotic portal hypertension in Latin America, Africa, and Asia[2]. The pathogenesis of schistosomiasis is related to the host cellular immune response. This leads to granuloma formation and neo-angiogenesis with subsequent irreversible periportal fibrosis and, consequently, severe portal hypertension manifesting with splenomegaly and esophageal varices[3,4]. Traditionally the diagnosis of Schistosoma infection is based upon demonstration of parasite eggs in patient secretions or tissues. However, in the case of liver disease, detection of ova often fails and the diagnosis is established using serologic tests along with DNA amplification techniques and characteristic liver biopsy findings[5-7]. Praziquantel is the drug of choice to treat laboratory-proven Schistosoma infection[8]. The effect of antischistosomal treatment on disease manifestations varies by stage. Early liver involvement is known to resolve after anthelmintic therapy, but late manifestations, such as fibrosis, do not change and treatment is focused on tempering portal hypertension manifestations[9]. LT represents a curative option for patients who develop severe hepatic fibrosis and portal hypertension secondary to hepatic schistosomiasis[10], and no specific treatment is indicated for the recipients[11].
PVT is a frequent and serious complication in patients with cirrhosis, with a prevalence ranging from 5% to 26%[12-17]. Patients with cirrhosis presenting with or developing PV and/or superior mesenteric vein (SMV) thrombosis while awaiting LT pose a significant surgical challenge for the reconstruction of the liver portal inflow, an essential step for successful OLT[18,19]. Although PVT has long been considered an absolute contraindication to OLT, it is currently regarded as a relative contraindication, depending on the patient clinical status, type of PVT and collateral venous flow, and the surgeon’s experience[20,21]. While an end-to-end donor to recipient portal vein anastomosis is fashioned in the majority of liver transplant recipients, approximately 2% of recipients will require a complex vascular reconstruction due to inadequate recipient portal vein inflow[22,23].
The type of PVT is classified according to the nature of the occlusion (complete vs partial) and the extension in the portal vein, the venous confluence and its contributories - the SMV and the splenic vein (SV). Various classification systems of PVT have been proposed with the Yerdel classification being widely used because it correlates thrombus extent and surgical management[24-28]. Yerdel’s classification defines grade I as partial PVT (< 50% of the lumen) with or without minimal extension into the SMV, grade II as partial PVT (> 50% of the lumen), grade III - complete thrombosis of both PV and proximal SMV and grade IV with complete PV and both proximal and distal SMV.
For the reconstruction of the liver portal inflow in the presence of PV-SMV thrombosis there are 3 main strategies: Anatomical (and physiological), physiological (non-anatomical) and non-physiological[19,29]. For Yerdel grades I to III, an anatomical reconstruction may be achieved; operative techniques include thrombectomy, whether the thrombus is removed en-bloc with the liver or through an intraoperative PV/SMV thrombectomy, followed by direct porto-portal anastomosis or indirect using an interposition venous graft.
For more complex cases of complete occlusion or proximal extension of the thrombus, such as in Yerdel’s grade IV and some grade III cases, alternative approaches should be used to redirect the portal venous flow into the graft[29,30]. Some of those extraordinary cases of extensive thrombosis may be considered as a contraindication to transplant. However, when evaluated by highly experienced transplant centers, a complex vascular reconstruction may be attempted or else, a multivisceral transplant may be considered. That is, for Yerdel’s grade IV and some grade III cases, a physiological (non-anatomical) or non-physiological (inflow achieved by reno-portal anastomosis, cavo-portal hemi-transposition or portal vein arterialization), approach may be used.
The portal vein-variceal anastomosis is a challenging physiological non-anatomical technique of portal vein inflow reconstruction used and described rarely. In those procedures, enlarged splanchnic varices[31-34], LGV[35-38], or pericholedochal varix[39,40] is used. Use of a splanchnic varix such as a dilated LGV necessitates a meticulous and very careful dissection in a hostile surrounding of other dilated fragile varices. Furthermore, length of the donor’s liver portal vein should be sufficient or else an interposition venous graft may be used for the anastomosis. From the functional standpoint, adequate portal flow should be assessed, using direct (needle- transducer) or indirect (ultrasound Doppler) method. In the occurrence of slow venous flow, proximal ligation of the varix may be considered in order to divert splanchnic venous drainage towards the neo-liver and to avoid the siphon effect of the peri-gastric varices and SV. In cases of extensive SMV thrombosis there is also a concern for inadequate venous intestinal drainage, despite a successful and functional anastomosis, and a as result refractory ascites.
Although challenging, good outcomes are possible in patients with extensive PV/SMV thrombosis undergoing LT. Meticulous patient selection, preoperative imaging planning and highly experienced surgical team are crucial for a successful transplantation and reconstruction of the portal inflow in those complex clinical scenarios. This case shows the feasibility of this unusual approach, using a dilated left gastric varix for the reconstruction of the liver portal inflow, giving a patient in an extreme condition access to life-saving LT.
Although challenging, good outcomes are possible in patients with extensive PV/SMV thrombosis undergoing LT. Meticulous patient selection, preoperative imaging planning and highly experienced surgical team are crucial for a successful transplantation and reconstruction of the portal inflow in those complex clinical scenarios. This case shows the feasibility of this unusual approach, using a dilated left gastric varix for the reconstruction of the liver portal inflow, giving a patient in an extreme condition access to life-saving LT.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Transplantation
Country/Territory of origin: Israel
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Singh N, United States; Soresi M, Italy A-Editor: Liu X, China S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Ross AG, Olds GR, Cripps AW, Farrar JJ, McManus DP. Enteropathogens and chronic illness in returning travelers. N Engl J Med. 2013;368:1817-1825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 86] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 2. | Bodh V, Chawla Y. Noncirrhotic intrahepatic portal hypertension. Clin Liver Dis (Hoboken). 2014;3:129-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Elbaz T, Esmat G. Hepatic and intestinal schistosomiasis: review. J Adv Res. 2013;4:445-452. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 114] [Cited by in RCA: 135] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 4. | Andrade ZA. Schistosomiasis and liver fibrosis. Parasite Immunol. 2009;31:656-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 184] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 5. | Guimarães Cavalcanti M, Marcello de Araujo-Neto J, Mauro Peralta J. Schistosomiasis: Clinical management of liver disease. Clin Liver Dis (Hoboken). 2015;6:59-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Tamarozzi F, Fittipaldo VA, Orth HM, Richter J, Buonfrate D, Riccardi N, Gobbi FG. Diagnosis and clinical management of hepatosplenic schistosomiasis: A scoping review of the literature. PLoS Negl Trop Dis. 2021;15:e0009191. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 7. | Weerakoon KG, Gordon CA, McManus DP. DNA Diagnostics for Schistosomiasis Control. Trop Med Infect Dis. 2018;3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 60] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 8. | Vale N, Gouveia MJ, Rinaldi G, Brindley PJ, Gärtner F, Correia da Costa JM. Praziquantel for Schistosomiasis: Single-Drug Metabolism Revisited, Mode of Action, and Resistance. Antimicrob Agents Chemother. 2017;61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 243] [Article Influence: 30.4] [Reference Citation Analysis (0)] |
| 9. | Deng WC, Li JX, Pan K, Kong GQ, He YK, Li YS. [Recommendation of a new clinical classification of advanced schistosomiasis]. Zhongguo Xue Xi Chong Bing Fang Zhi Za Zhi. 2012;24:235-236. [PubMed] |
| 10. | El Moghazy W, Kashkoush S, O'hali W, Abdallah K. Long-term outcome after liver transplantation for hepatic schistosomiasis: a single-center experience over 15 years. Liver Transpl. 2015;21:96-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Vincenzi R, Neto JS, Fonseca EA, Pugliese V, Leite KR, Benavides MR, Cândido HL, Porta G, Miura IK, Pugliese R, Danesi VB, Guimarães TC, Porta A, Kondo M, Carone E, Chapchap P. Schistosoma mansoni infection in the liver graft: The impact on donor and recipient outcomes after transplantation. Liver Transpl. 2011;17:1299-1303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Garcia-Pagan JC, Valla DC. Portal vein thrombosis: a predictable milestone in cirrhosis? J Hepatol. 2009;51:632-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 47] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 13. | Tao YF, Teng F, Wang ZX, Guo WY, Shi XM, Wang GH, Ding GS, Fu ZR. Liver transplant recipients with portal vein thrombosis: a single center retrospective study. Hepatobiliary Pancreat Dis Int. 2009;8:34-39. [PubMed] |
| 14. | Nery F, Chevret S, Condat B, de Raucourt E, Boudaoud L, Rautou PE, Plessier A, Roulot D, Chaffaut C, Bourcier V, Trinchet JC, Valla DC; Groupe d'Etude et de Traitement du Carcinome Hépatocellulaire. Causes and consequences of portal vein thrombosis in 1,243 patients with cirrhosis: results of a longitudinal study. Hepatology. 2015;61:660-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 348] [Article Influence: 34.8] [Reference Citation Analysis (0)] |
| 15. | Ponziani FR, Zocco MA, Senzolo M, Pompili M, Gasbarrini A, Avolio AW. Portal vein thrombosis and liver transplantation: implications for waiting list period, surgical approach, early and late follow-up. Transplant Rev (Orlando). 2014;28:92-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 66] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 16. | Francoz C, Valla D, Durand F. Portal vein thrombosis, cirrhosis, and liver transplantation. J Hepatol. 2012;57:203-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 184] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 17. | Ravaioli M, Zanello M, Grazi GL, Ercolani G, Cescon M, Del Gaudio M, Cucchetti A, Pinna AD. Portal vein thrombosis and liver transplantation: evolution during 10 years of experience at the University of Bologna. Ann Surg. 2011;253:378-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 90] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 18. | Harding DJ, Perera MT, Chen F, Olliff S, Tripathi D. Portal vein thrombosis in cirrhosis: Controversies and latest developments. World J Gastroenterol. 2015;21:6769-6784. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 82] [Cited by in RCA: 78] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 19. | Hibi T, Nishida S, Levi DM, Selvaggi G, Tekin A, Fan J, Ruiz P, Tzakis AG. When and why portal vein thrombosis matters in liver transplantation: a critical audit of 174 cases. Ann Surg. 2014;259:760-766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 121] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 20. | Qi X, Dai J, Jia J, Ren W, Yang M, Li H, Fan D, Guo X. Association between portal vein thrombosis and survival of liver transplant recipients: a systematic review and meta-analysis of observational studies. J Gastrointestin Liver Dis. 2015;24:51-59, 4 p following 59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 21. | Kotsifa E, Kykalos S, Machairas N, Nikiteas N, Sotiropoulos GC. Management of portal vein thrombosis in cirrhotic patients enlisted for liver transplantation: From diagnosis to treatment (Review). Biomed Rep. 2021;15:94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 22. | Alexopoulos SP, Thomas E, Berry E, Whang G, Matsuoka L. The portal vein-variceal anastomosis: an important technique for establishing portal vein inflow. Clin Transplant. 2014;28:52-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 23. | Singh N, Washburn K, Black S, Schenk A. Techniques for Management of Portal Vein Thrombosis during Liver Transplantation. Case Rep Transplant. 2020;2020:8875196. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 24. | Sarin SK, Philips CA, Kamath PS, Choudhury A, Maruyama H, Nery FG, Valla DC. Toward a Comprehensive New Classification of Portal Vein Thrombosis in Patients With Cirrhosis. Gastroenterology. 2016;151:574-577.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 119] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 25. | Jamieson NV. Changing perspectives in portal vein thrombosis and liver transplantation. Transplantation. 2000;69:1772-1774. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 75] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 26. | Charco R, Fuster J, Fondevila C, Ferrer J, Mans E, García-Valdecasas JC. Portal vein thrombosis in liver transplantation. Transplant Proc. 2005;37:3904-3905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 57] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 27. | Ma J, Yan Z, Luo J, Liu Q, Wang J, Qiu S. Rational classification of portal vein thrombosis and its clinical significance. PLoS One. 2014;9:e112501. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 28. | Yerdel MA, Gunson B, Mirza D, Karayalçin K, Olliff S, Buckels J, Mayer D, McMaster P, Pirenne J. Portal vein thrombosis in adults undergoing liver transplantation: risk factors, screening, management, and outcome. Transplantation. 2000;69:1873-1881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 485] [Cited by in RCA: 525] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 29. | Bhangui P, Lim C, Levesque E, Salloum C, Lahat E, Feray C, Azoulay D. Novel classification of non-malignant portal vein thrombosis: A guide to surgical decision-making during liver transplantation. J Hepatol. 2019;71:1038-1050. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 73] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 30. | Bhangui P, Fernandes ESM, Di Benedetto F, Joo DJ, Nadalin S. Current management of portal vein thrombosis in liver transplantation. Int J Surg. 2020;82S:122-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 31. | Lacerda CM, de Melo PS, Amorim A, Carvalho G, Pereira LB. The left gastric vein as an alternative to portal reconstruction in orthotopic liver transplantation. Transplant Proc. 2002;34:1216-1217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 32. | Teixeira UF, Machry MC, Goldoni MB, Kruse C, Diedrich JA, Rodrigues PD, Giacomazzi CB, Negri EA, Koop M, Gomes CG, Sampaio JA, Fontes PR, Waechter FL. Use of Left Gastric Vein as an Alternative for Portal Flow Reconstruction in Liver Transplantation. Case Rep Surg. 2016;2016:8289045. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 33. | Ravaioli M, Prosperi E, Pinna A, Siniscalchi A, Fallani G, Frascaroli G, Maroni L, Odaldi F, Serenari M, Cescon M. Restoration of portal flow with varix in liver transplantation for patients with total portal vein thrombosis: An effective strategy in the largest center experience. Clin Transplant. 2021;35:e14303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 34. | Pinheiro RS, Cruz RJ Jr, Nacif LS, Vane MF, D'Albuquerque LA. Successful liver allograft inflow reconstruction with the right gastroepiploic vein. Hepatobiliary Pancreat Dis Int. 2016;15:106-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 35. | Czerniak A, Badger I, Sherlock D, Buckels J. Orthotopic liver transplantation in a patient with thrombosis of the hepatic portal and superior mesenteric veins. Transplantation. 1990;50:334-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 36. | Wu TH, Chou HS, Pan KT, Lee CS, Wu TJ, Chu SY, Chen MF, Lee WC. Application of cryopreserved vein grafts as a conduit between the coronary vein and liver graft to reconstruct portal flow in adult living liver transplantation. Clin Transplant. 2009;23:751-755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 37. | Wang Z, Yang L. Gastric coronary vein to portal vein reconstruction in liver transplant: case report. Exp Clin Transplant. 2014;12:562-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 38. | Safwan M, Nagai S, Abouljoud MS. Portal Vein Inflow From Enlarged Coronary Vein in Liver Transplantation: Surgical Approach and Technical Tips: A Case Report. Transplant Proc. 2016;48:3070-3072. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 39. | Lee S, Kim DJ, Kim IG, Jeon JY, Jung JP, Choi GS, Kim JS. Use of pericholedochal plexus for portal flow reconstruction in diffuse portal vein thrombosis: case report. Transplant Proc. 2014;46:977-979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 40. | Kim JD, Choi DL, Han YS. The paracholedochal vein: a feasible option as portal inflow in living donor liver transplantation. Ann Surg Treat Res. 2014;87:47-50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |