Copyright
©The Author(s) 2016.
World J Transplant. Sep 24, 2016; 6(3): 564-572
Published online Sep 24, 2016. doi: 10.5500/wjt.v6.i3.564
Published online Sep 24, 2016. doi: 10.5500/wjt.v6.i3.564
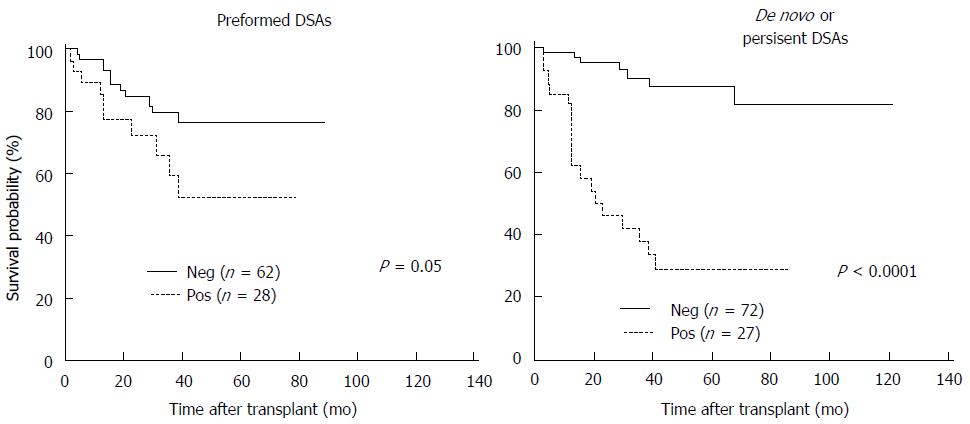
Figure 1 The Kaplan-Meier graft survival for the presence of performed donor-specific antibodies before transplant and newly formed (de novo) donor-specific antibodies after transplant.
Patients with preformed donor-specific antibodies (DSA) had significantly lower graft survival than those without preformed DSA. The graft survival was markedly worse in patients with de novo DSA or persistent DSA.
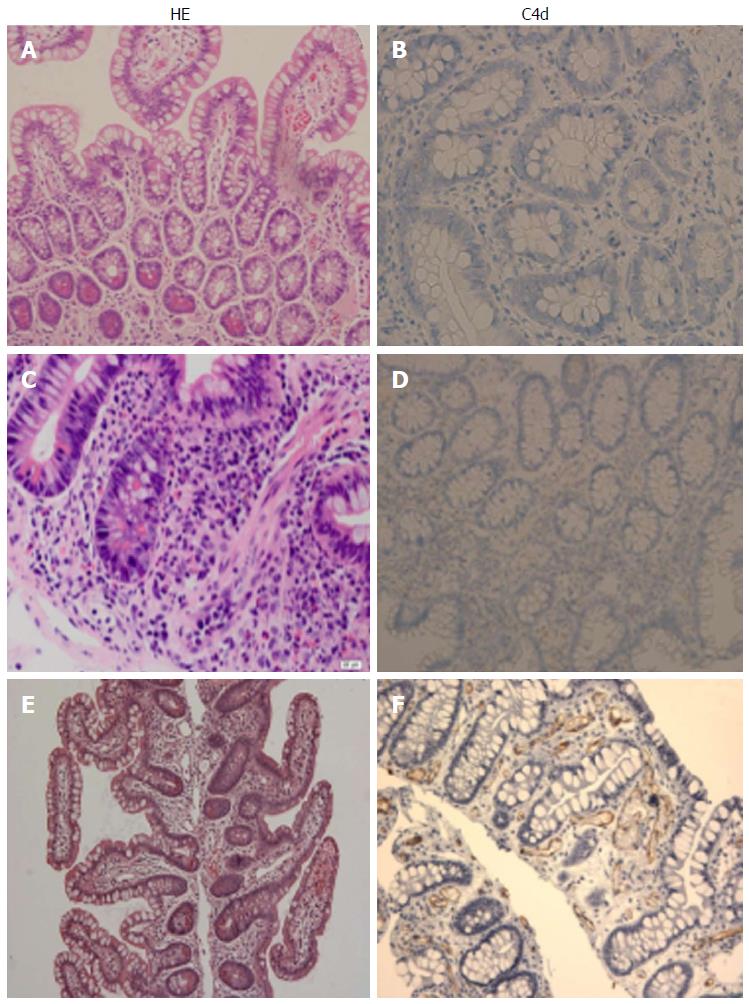
Figure 2 Histopatholgy of the intestinal allografts.
A and B: No rejection: Normal mucosal architecture of small bowel biopsy after transplant. No staining for C4d is seen in the capillaries of the lamina propria; C and D: Acute cellular rejection (ACR): There is mononuclear infiltration, crypt epithelial injury, and apoptotic bodies in the lamina propria. A weak staining for C4d is sometimes present in a patient with ACR; E and F: Acute antibody-mediated rejection: There is prominent hemorrhage and congestion with scattered fibrin thrombin in the lamina propria. Widespread and bright staining for C4d is present in the capillaries of the lamina propria.
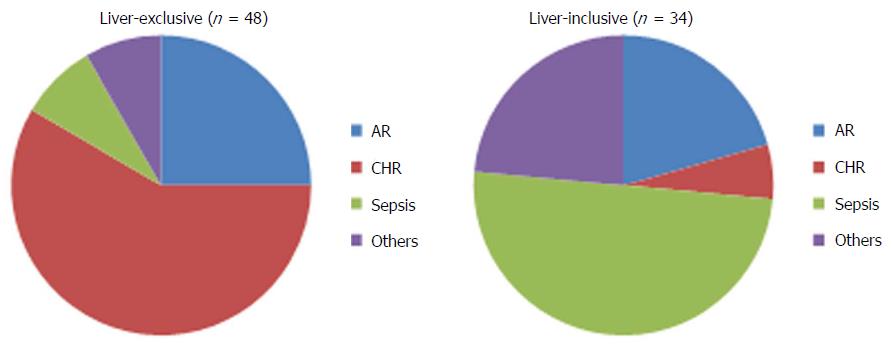
Figure 3 The causes of graft loss in the liver-exclusive and liver-inclusive intestinal transplants.
In liver-exclusive transplants, chronic rejection was the leading cause of graft loss. In liver-inclusive transplants, however, infection was the major cause of graft loss. AR: Acute rejection; CHR: Chronic rejection.
- Citation: Wu GS. Updates on antibody-mediated rejection in intestinal transplantation. World J Transplant 2016; 6(3): 564-572
- URL: https://www.wjgnet.com/2220-3230/full/v6/i3/564.htm
- DOI: https://dx.doi.org/10.5500/wjt.v6.i3.564