Published online Sep 29, 2022. doi: 10.5495/wjcid.v12.i2.61
Peer-review started: April 30, 2022
First decision: June 8, 2022
Revised: June 15, 2022
Accepted: August 21, 2022
Article in press: August 21, 2022
Published online: September 29, 2022
Processing time: 148 Days and 22.5 Hours
Leishmaniasis is a neglected zoonotic disease, endemic in Sudan. Estimating this disease is very important to inform the health care policymakers and the gove
To find out the frequency and distribution of human leishmaniasis based on sex and age for 5 years in the West Kordofan state, Sudan.
A 5-year retrospective study from 2016 through 2020 was carried out using local hospital records of leishmaniasis patients. The positive results were recorded after performing at least one of the following leishmaniasis standard tests: direct agglutination test, enzyme-linked immunosorbent assay and leishmania skin test. The sex and age of each patient were recorded. The collected data were analyzed using STATA package version 16.
A total of 162443 patient records from 2016 to 2020 were retrieved. Of these, 4.39% were found to be positive for leishmaniasis. The disease has been more common in males (65.3%) than in females (34.7%). The highest reported prevalence (6.58%) was in patients 15-44 years, and the lowest prevalence (1.95%) was among patients ≥ 65 years.
The results of the current study indicate that leishmaniasis is endemic in the study area even though the numbers of patients in the 5 consecutive years were varying. In addition, the disease was common in males and adults. The interpretation of these findings should take into consideration the absence of information about some important confounding factors.
Core Tip: A 5-year retrospective study was conducted to find the frequency and distribution of human leishmaniasis in the West Kordofan state and was based on sex and age. A total of 162443 patient records were retrieved. Of these, 4.39% were found to be positive for leishmaniasis. The disease has been more common in males than in females. The highest reported prevalence was in patients 15-44 years, and the lowest prevalence was among patients ≥ 65 years. The current study indicates that leishmaniasis is endemic in the study area even though the numbers of patients in the 5 consecutive years were varying.
- Citation: Abdulslam Abdullah A, Ahmed M, Gadeed A, Eltayeb A, Ahmed S, Hamad S, Hussein M. Five-year retrospective hospital-based study on epidemiological data regarding human leishmaniasis in West Kordofan state, Sudan. World J Clin Infect Dis 2022; 12(2): 61-68
- URL: https://www.wjgnet.com/2220-3176/full/v12/i2/61.htm
- DOI: https://dx.doi.org/10.5495/wjcid.v12.i2.61
Leishmaniasis is a parasitic zoonotic disease caused by the Leishmania parasite[1]. The disease is mainly transmitted by the bite of infected female phlebotomine sandflies[2]. The World Health Organization classified the disease as a neglected tropical disease[2,3]. There are several forms of human leis
Sudan is a highly endemic country for leishmaniasis (both CL and VL). The disease represents a serious health problem that may affect the whole healthcare system[16]. The geographical distribution of the disease in Sudan have a high relation to the distribution of the vectors. Studies revealed that VL is endemic in the savannah area, which starts from the Gadarif state in the east to the White Nile State in the west and from the Kassala state in the northeast to the Blue Nile State in the south. Also, VL was reported in some scattered foci in the Kordofan state and Darfur state. Moreover, CL is found in a fluctuating pattern mainly in the northern, central and western parts of the country[17-26].
West Kordofan is the 18th state of Sudan. It was established in July 2013 on the border with the Republic of South Sudan in the east, North Kordofan state in the North and South Darfur state in the west. People of West Kordofan, especially the Mesairya tribe, continuously move to and from South Sudan where leishmaniasis disease is endemic[7]. The state also contains many south Sudanese refugee camps spread almost all over the state. The geographical location together with the high presence of the suspected infected refugees makes the people of the West Kordofan state very vulnerable to leishmaniasis (for both CL and VL). A community-based study in two West Kordofan cities, namely Muglad and Babnousa, reported that out of 1781 randomly selected volunteers, 238 persons (13%) tested positive for leishmaniasis[27]. Based on that, there is still a need for a deeper look at the epidemiology of the disease in the whole state, in both males and females and in all age groups, to design and implement suitable prevention and eradication programs for the disease at the state level. Thus, this study aimed to find out the frequency and distribution of human leishmaniasis based on sex and age in the West Kordofan state for 5 years.
The present retrospective study was conducted among patients who were admitted to any hospital in the West Kordofan state, Sudan from January 1, 2016 to December 31, 2020 to test the presence of human leishmaniasis of any type in the population of West Kordofan. In addition to the clinical symptom and signs, the positive results were recorded after performing at least one of the following leishmaniasis standard tests: direct agglutination test, enzyme-linked immunosorbent assay and leishmania skin test. Data of age, sex and presence of any type of leishmaniasis were retrieved from the medical records department in the Ministry of Health West Kordofan, with the approval of the ministry ethical committee. The medical record department follows the guidelines of the International Classification of Diseases 10 coding.
Descriptive statistics and data analysis were done using STATA package version 16 (Stata Corp LLC, College Station, TX). Z test was applied to compare the proportions between the study groups. If the P value was less than or equal to 0.05, it indicated that there was a significant difference between the proportions of the two groups.
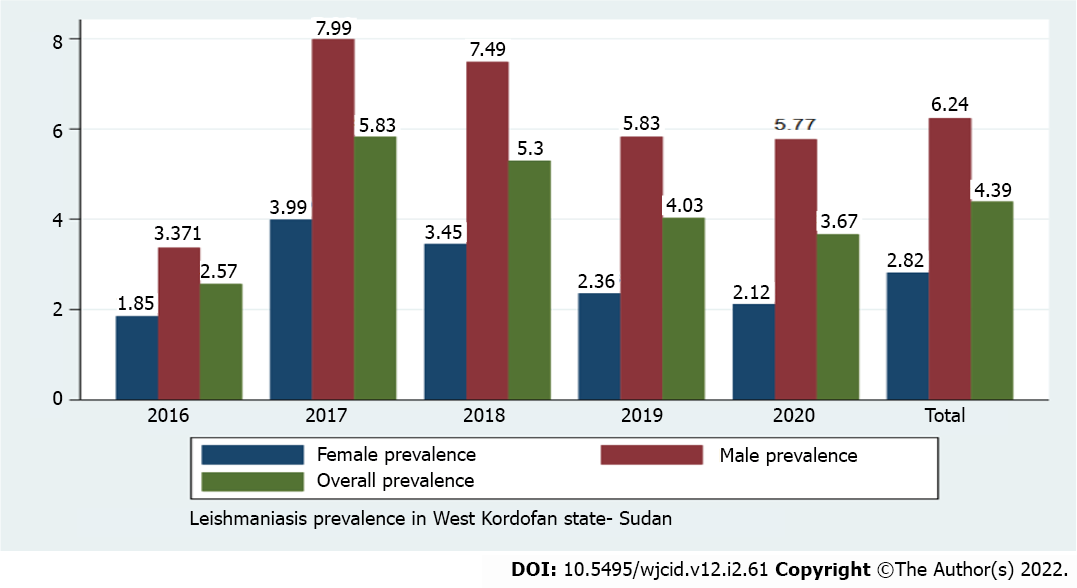
A total of 162443 patient records (87847 female and 74596 male patients) from 2016 to 2020 were retrieved. Of these, 4.39% were found to be positive for leishmaniasis. Among them, 34.7% were females and 65.3% were males. The diagnostic prevalence of the infection was first found to be very low in 2016 (2.57%). After 1 year in 2017, the highest reported prevalence of 5.83% was observed and then started to decrease (with some fluctuation) to 3.67% in 2020 (Figure 1).
Sex-related differences in leishmaniasis prevalence are presented in Table 1. The prevalence was significantly higher (P ≤ 0.05) in males compared to females in the period from 2017 to 2020, while in 2016 there was no significant variation between the sexes (P > 0.05). The prevalence of leishmaniasis was relatively increased with participant age in both females and males. The prevalence reached its peak in patients 15-44 years, which was 6.58%, then decreased to be the lowest of 1.95% among patients ≥ 65 years (Tables 2 and 3). In addition to that in all age groups, males had a higher prevalence of leishmaniasis than females.
| Year | Female, n (%) | Male, n (%) | Total, n (%) | P value |
| 2016 | 244 (1.85) | 405 (3.37) | 649 (2.57) | 0.2277 |
| 2017 | 780 (3.99) | 1322 (7.99) | 2102 (5.83) | 0.0002 |
| 2018 | 621 (3.45) | 1142 (7.49) | 1763 (5.30) | 0.0002 |
| 2019 | 409 (2.36) | 941 (5.83) | 1350 (4.03) | 0.0015 |
| 2020 | 420 (2.12) | 844 (5.77) | 1264 (3.67) | 0.0008 |
| Total | 2474 (2.82) | 4654 (6.24) | 7128 (4.39) | 0.0001 |
| Age group | Female, % | Male, % | Total, % | P value |
| < 1 yr | 2.22 | 5.05 | 3.52 | 0.0001 |
| 1-4 yr | 3.93 | 4.5 | 4.19 | 0.2523 |
| 5-14 yr | 5.47 | 7.89 | 6.57 | 0.0001 |
| 15-44 yr | 5.63 | 7.68 | 6.58 | 0.0001 |
| 45-64 yr | 2.81 | 4.42 | 3.55 | 0.0012 |
| ≥ 65 yr | 1.73 | 2.2 | 1.95 | 0.3452 |
| Year | Sex | Age group | |||||
| Females | < 1% | 1%-4% | 5%-14% | 15%-44% | 45%-64% | ≥ 65% | |
| 2016 | 1.19 | 2.66 | 4.52 | 3.51 | 1.85 | 1.06 | |
| 2017 | 2.16 | 1.80 | 6.00 | 4.97 | 2.47 | 2.01 | |
| 2018 | 1.44 | 3.35 | 4.97 | 5.55 | 2.39 | 1.55 | |
| 2019 | 3.54 | 3.90 | 5.54 | 6.81 | 2.98 | 1.77 | |
| 2020 | 2.51 | 4.83 | 5.98 | 6.73 | 4.04 | 2.03 | |
| Total | 2.22 | 3.93 | 5.47 | 5.63 | 2.81 | 1.73 | |
| 2016 | Males | 0.92 | 3.81 | 6.59 | 5.20 | 2.30 | 1.19 |
| 2017 | 2.06 | 5.26 | 8.30 | 6.90 | 3.70 | 2.35 | |
| 2018 | 3.26 | 3.69 | 7.64 | 8.50 | 3.81 | 2.08 | |
| 2019 | 4.64 | 3.75 | 6.90 | 7.20 | 5.08 | 2.12 | |
| 2020 | 14.11 | 5.90 | 9.84 | 10.23 | 6.84 | 3.14 | |
| Total | 5.05 | 4.50 | 7.89 | 7.68 | 4.42 | 2.20 | |
Leishmaniasis is an endemic neglected zoonotic disease in Sudan, widespread all over the country from the eastern states to the western states and from southern states to northern states[16]. However, few data about the epidemiological and demographical distribution of the disease in western states is available, especially in West Kordofan, and it seems to be overlooked[20,24,25,27]. Thus the current study is the first comprehensive attempt to describe the epidemiological and demographical distribution of the disease in the state.
In this study, the data on human leishmaniasis was collected from the annual health statistical reports for 5 years (2016–2020) and was analyzed to show the burden of the disease in the West Kordofan state, Sudan. The results highlight that a total of 162443 people were admitted to the hospitals and health care centers in the state. Of these, 7128 people were infected during this period. In 2016 the prevalence of leishmaniasis was found to be very low at 2.57%. Surprisingly, it was raised to 5.83% in 2017, and from then it seemed to decrease. The reason could be that the government of Sudan in collaboration with the World Health Organization and other related international organizations developed diagnostic and control strategies to limit the spread of the disease in October 2014[28,29]. The first 2 years (2015 and 2016) were for training the health care professionals in the state on the new diagnostic and prevention methods. That may explain the low prevalence in the 1st study year because of the use of the low sensitivity diagnostic test. Then after implementing the new diagnostic method in 2017 the rate was raised. In line with that, after 2017 the prevalence of leishmaniasis was decreasing because of implementing the new control strategies.
The current study found that the overall prevalence of leishmaniasis in West Kordofan was lower than that reported by Sharief et al[27] in 2019. This may be due to the difference in sample size and study period, which were bigger and longer, respectively, in the current study compared with the other study. Nevertheless, the study area could have a great impact on the result. In their study, Sharief et al[27] collected data in two districts in the state, but the current study collected data from all 14 districts.
Sex-related distribution of human leishmaniasis in the study revealed that males were highly affected compared to females with an overall percentage of 65.3% and 34.7%, respectively. This is in line with Awadalla et al[30], Ebrahim et al[25] and Collis et al[31] and disagrees with Mohammed et al[20]. This result might be justified because the majority of males are nomads. They are moving seasonally to the tropic and subtropic areas in South Sudan whereby the exposure to the risk of sandflies bites is high. The same exposure of males in different agricultural areas may be a contributing factor to the infections. Consequently, males are more vulnerable than females.
Age-wise distribution found that people in the age group 15-44 had the highest prevalence among all populations. Similar results were reported by Awadalla et al[30], Osman et al[24], Ebrahim et al[25] and Collis et al[31]. These studies indicated that the adult men and women aged between 15-44 years were more affected by the disease compared to the lower and higher age groups. This can be put in the context that this age group is the working-age group in all fields, especially the agricultural field. In contrast, a study conducted by Mohammed et al[20] indicated that the most affected age groups were children between 1-year-old and 5-years-old.
In addition, the lowest reported prevalence in this study was found in the age group > 65 years. Although this group of people is more vulnerable to infections because the immune system weakens, they have a relevant low prevalence of the disease. The possible reason that these patients might have less exposure to the infection is due to their lifestyle, which keeps them away from the areas where the carrier host exists, especially in the agricultural areas.
This study provided important epidemiological information about human leishmaniasis in West Kordofan, which is missing from the scientific literature despite its urgent need to design a collaborative effort and immediate action by policymakers and governments (federal and state government) for prevention and eradication programs in light of the one health concept. However, the absence of data about the infection (type, site and status), Leishmania parasite and other potential risk factors in some included studies are considered as limitations of the current study.
The results of the current study indicate that leishmaniasis is endemic in the study area even though the numbers of patients in the 5 consecutive years were varying. In addition, the disease was common in males and adults. The interpretation of these findings should take into consideration the absence of information about some important confounding factors. Further studies need to be carried out to clarify the economic impact of the disease on the public health sector in the state and the role of domestic animals in the epidemiology of the disease in Sudan.
In Sudan, human leishmaniasis is endemic, and the prevalence of the disease varies throughout the country. Although the disease in Sudan is serious, there is no overall estimation of the prevalence of human leishmaniasis in the western parts of the country, especially in the West Kordofan state.
The lack of published studies about human leishmaniasis in the western parts of Sudan especially in the West Kordofan state may cause a problem for the policymakers and local governments to develop and adopt a suitable prevention program to deal with the disease at the state level and the country level.
The objective of this study was to find the frequency and distribution of human leishmaniasis based on sex and age in West Kordofan, Sudan for 5 years.
A 5-year retrospective study from 2016 through 2020 was carried out using local hospital records of leishmaniasis patients. The positive results were recorded after performing at least one of the following leishmaniasis standard tests: direct agglutination test, enzyme-linked immunosorbent assay and leishmania skin test.
A total of 162443 patient records from 2016 to 2020 were retrieved. Of these, 4.39% were found to be positive for leishmaniasis. The disease has been more common in males (65.3%) than in females (34.7%). The highest reported prevalence (6.58%) was in patients 15-44 years, and the lowest prevalence (1.95%) was among patients ≥ 65 years.
The results of the current study indicate that leishmaniasis is endemic in the study area even though the numbers of patients in the 5 consecutive years were varying. In addition, the disease was common in males and adults.
Further studies need to be carried out to clarify the economic impact of the disease on the public health sector in the state and the role of domestic animals in the epidemiology of the disease in Sudan.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Tropical medicine
Country/Territory of origin: Sudan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Wang T, China; Yang X, China S-Editor: Wu YXJ L-Editor: Filipodia P-Editor: Wu YXJ
| 1. | Torres-Guerrero E, Quintanilla-Cedillo MR, Ruiz-Esmenjaud J, Arenas R. Leishmaniasis: a review. F1000Res. 2017;6:750. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 461] [Cited by in RCA: 681] [Article Influence: 85.1] [Reference Citation Analysis (0)] |
| 2. | Elaagip A, Ahmed A, Wilson MD, Boakye DA, Abdel Hamid MM. Studies of host preferences of wild-caught Phlebotomus orientalis and Ph. papatasi vectors of leishmaniasis in Sudan. PLoS One. 2020;15:e0236253. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Alvar J, Yactayo S, Bern C. Leishmaniasis and poverty. Trends Parasitol. 2006;22:552-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 478] [Cited by in RCA: 524] [Article Influence: 27.6] [Reference Citation Analysis (0)] |
| 6. | Shirzadi MR, Javanbakht M, Vatandoost H, Jesri N, Saghafipour A, Fouladi-Fard R, Omidi-Oskouei A. Impact of Environmental and Climate Factors on Spatial Distribution of Cutaneous Leishmaniasis in Northeastern Iran: Utilizing Remote Sensing. J Arthropod Borne Dis. 2020;14:56-67. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 7. | Al-Salem W, Herricks JR, Hotez PJ. A review of visceral leishmaniasis during the conflict in South Sudan and the consequences for East African countries. Parasit Vectors. 2016;9:460. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 77] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 8. | Diro E, Lynen L, Ritmeijer K, Boelaert M, Hailu A, van Griensven J. Visceral Leishmaniasis and HIV coinfection in East Africa. PLoS Negl Trop Dis. 2014;8:e2869. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 112] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 9. | Alvar J, Vélez ID, Bern C, Herrero M, Desjeux P, Cano J, Jannin J, den Boer M; WHO Leishmaniasis Control Team. Leishmaniasis worldwide and global estimates of its incidence. PLoS One. 2012;7:e35671. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3243] [Cited by in RCA: 3662] [Article Influence: 281.7] [Reference Citation Analysis (1)] |
| 10. | Seaman J, Pryce D, Sondorp HE, Moody A, Bryceson AD, Davidson RN. Epidemic visceral leishmaniasis in Sudan: a randomized trial of aminosidine plus sodium stibogluconate versus sodium stibogluconate alone. J Infect Dis. 1993;168:715-720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 82] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 11. | Seaman J, Mercer AJ, Sondorp E. The epidemic of visceral leishmaniasis in western Upper Nile, southern Sudan: course and impact from 1984 to 1994. Int J Epidemiol. 1996;25:862-871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 140] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 12. | Ashford RW, Seaman J, Schorscher J, Pratlong F. Epidemic visceral leishmaniasis in southern Sudan: identity and systematic position of the parasites from patients and vectors. Trans R Soc Trop Med Hyg. 1992;86:379-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 56] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Perea WA, Moren A, Ancelle T, Sondorp E. Epidemic visceral leishmaniasis in southern Sudan. Lancet. 1989;2:1222-1223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 21] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Gebre-Michael T, Balkew M, Alamirew T, Gudeta N, Reta M. Preliminary entomological observations in a highland area of Amhara region, northern Ethiopia, with epidemic visceral leishmaniasis. Ann Trop Med Parasitol. 2007;101:367-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | el-Safi SH, Peters W. Studies on the leishmaniases in the Sudan. 1. Epidemic of cutaneous leishmaniasis in Khartoum. Trans R Soc Trop Med Hyg. 1991;85:44-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 36] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 16. | Osman AA. Evaluation of molecular genotyping in clinical and epidemiological study of leishmaniasis in Sudan. Sci Parasitol. 2011;12:131-137. [DOI] [Full Text] |
| 17. | el-Hassan AM, Zijlstra EE. Leishmaniasis in Sudan. Cutaneous leishmaniasis. Trans R Soc Trop Med Hyg. 2001;95 Suppl 1:S1-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Osman OF, Kager PA, Oskam L. Leishmaniasis in the Sudan: a literature review with emphasis on clinical aspects. Trop Med Int Health. 2000;5:553-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Jones CM, Welburn SC. Leishmaniasis Beyond East Africa. Front Vet Sci. 2021;8:618766. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 20. | Mohammed MA, Khalid NM, Aboud MA. Kala-azar in Darfur: Evidence for indigenous transmission in Al-Malha Locality, North Darfur, western Sudan. Parasit Vectors. 2018;11:149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 21. | Khalid Shamboul Musab M. A study on the transmission potential of Leishmania donovani in Rahad, Upper Atbara and Blue Nile areas. PhD. Thesis, University of Khartoum. 2012. Available from: http://khartoumspace.uofk.edu/items/bbdb1504-b34c-4b48-82c2-5d9920b4931c/full. [DOI] [Full Text] |
| 22. | Elamin EM, Guizani I, Guerbouj S, Gramiccia M, El Hassan AM, Di Muccio T, Taha MA, Mukhtar MM. Identification of Leishmania donovani as a cause of cutaneous leishmaniasis in Sudan. Trans R Soc Trop Med Hyg. 2008;102:54-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 34] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 23. | Khalil EA, Zijlstra EE, Kager PA, El Hassan AM. Epidemiology and clinical manifestations of Leishmania donovani infection in two villages in an endemic area in eastern Sudan. Trop Med Int Health. 2002;7:35-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 53] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 24. | Osman A. Epidemiology of leishmaniasis in south Kordofan region, western Sudan. Res J Med Scien. 2011;5:108-111. [DOI] [Full Text] |
| 25. | Ebrahim NAA. Occurrence of Visceral Leishmaniasis and its Determinants in North Darfur State, Sudan (2013). M.Sc. Thesis, University of Gezira. 2016. Available from: http://repo.uofg.edu.sd/handle/123456789/1427.. [DOI] [Full Text] |
| 26. | Khalil EA, Musa AM, Elgawi SH, Meshasha A, Gamar Eldawla I, Elhassan MO, Eljaleel KA, Younis BM, Elfaki ME, El-Hassan AM. Revival of a focus of visceral leishmaniasis in central Sudan. Ann Trop Med Parasitol. 2008;102:79-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 27. | Sharief A, Khalil E, Elmagzoub R, Omer S. Spectrum of Leishmania donovani infection in the Southwest of Sudan: a rapid epidemiological mapping. Ann Syst Biol. 2019;2:008-011. [DOI] [Full Text] |
| 28. | Republic of Sudan Federal Ministry of Health. Manual for the diagnosis and treatment of leishmaniasis. In: (NTDs) NTDD, editor. First ed: Federal Ministry of Health 2014: 49. [DOI] [Full Text] |
| 29. | World Health Organization. Framework for action on cutaneous leishmaniasis in the Eastern Mediterranean Region 2014-2018. Report No.: ISBN: 978-92-9021-944-6. |
| 30. | Awadalla H, El-Samani F, Soghaier MA, Makki M. Risk Factors Associated with the Development of Tuberculosis Among HIV-Infected Patients in Khartoum in 2010. AIMS Public Health. 2015;2:784-792. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 31. | Collis S, El-Safi S, Atia AA, Bhattacharyya T, Hammad A, Den Boer M, Le H, Whitworth JA, Miles MA. Epidemiological and molecular investigation of resurgent cutaneous leishmaniasis in Sudan. Int J Infect Dis. 2019;88:14-20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |