Published online Apr 26, 2022. doi: 10.5495/wjcid.v12.i1.41
Peer-review started: January 6, 2022
First decision: February 21, 2022
Revised: March 6, 2022
Accepted: April 3, 2022
Article in press: April 3, 2022
Published online: April 26, 2022
Processing time: 109 Days and 6.8 Hours
Infected aortic aneurysms are uncommon and difficult to treat. We present a case of infected aortic aneurysm with recurrent nontyphoidal Salmonella bacteremia.
A 68-year-old gentleman presented with non-specific symptoms and was found to have nontyphoidal Salmonella bacteremia and was treated with intravenous ceftriaxone. However his condition did not improve, and he developed a multiloculated right pleural effusion. Thoracocentesis was done to drain hemorrhagic pleural fluid. Chest computed tomography demonstrated descending thoracic aorta saccular aneurysm with periaortic hematoma likely due to recent bleed and extending to the right pleural cavity. He was referred to cardiothoracic surgery team and was planned for medical therapy in view of hemodynamic stability and no evidence of active leakage. He completed intravenous antibiotic for 5 wk and refused surgical intervention. Unfortunately, he was admitted twice for recurrent nontyphoidal Salmonella bacteremia. Finally, he agreed for surgical intervention and underwent endovascular aortic repair 3 mo later. Postoperatively, his condition remained stable with no recurrence of infection.
Our case highlights the importance of high index of suspicion of infected aortic aneurysm in patients with Salmonella bacteremia with high-risk factors such as atherosclerosis.
Core Tip: Infected aortic aneurysm is a rare condition with high mortality. Our aim of this case report is to highlight the importance of high index of suspicion of infected aortic aneurysm in patients with Salmonella bacteremia with additional literature review to help clinician in the management of this disease. Medical therapy alone in this condition is associated with poor outcome.
- Citation: Lee KT, Leong KN, Chow TS, Wong PS. Unusual cause of hemorrhagic pleural effusion: A case report . World J Clin Infect Dis 2022; 12(1): 41-46
- URL: https://www.wjgnet.com/2220-3176/full/v12/i1/41.htm
- DOI: https://dx.doi.org/10.5495/wjcid.v12.i1.41
Infected aneurysm is a rare disease associated with significant morbidity and mortality. Initial symptoms are non-specific, and due to lack of conclusive signs and symptoms, patients are often subjected to various investigations until a diagnosis is made. Standard treatment consists of antibiotic therapy and open surgery with surgical debridement and vascular reconstruction. However, there are no clear guidelines or randomized controlled trial on the best approach for the management of this condition. We report a patient with nontyphoidal Salmonella infected aortic aneurysm who was treated with medical therapy initially and complicated with recurrence. He was successfully treated with endovascular aortic repair and was well during follow-up with no recurrence of infection. Relevant literature is reviewed.
A 68-year-old man presented to our hospital with fever associated with lethargy, reduced oral intake, and dyspnea.
The patient’s presenting symptoms had lasted for 1 wk.
His medical illness includes diabetes mellitus, hypertension, ischemic heart disease, and chronic kidney disease.
No relevant family history.
He was febrile and required the support of face mask oxygen during presentation. Examination revealed reduced air entry over right lower zone with bilateral lower zone crepitations.
Laboratory results showed white blood cell count of 16 × 109/L, hemoglobin level of 8.3 g/dL, urea 16.9 mmol/L, and creatinine 301 μmol/L.
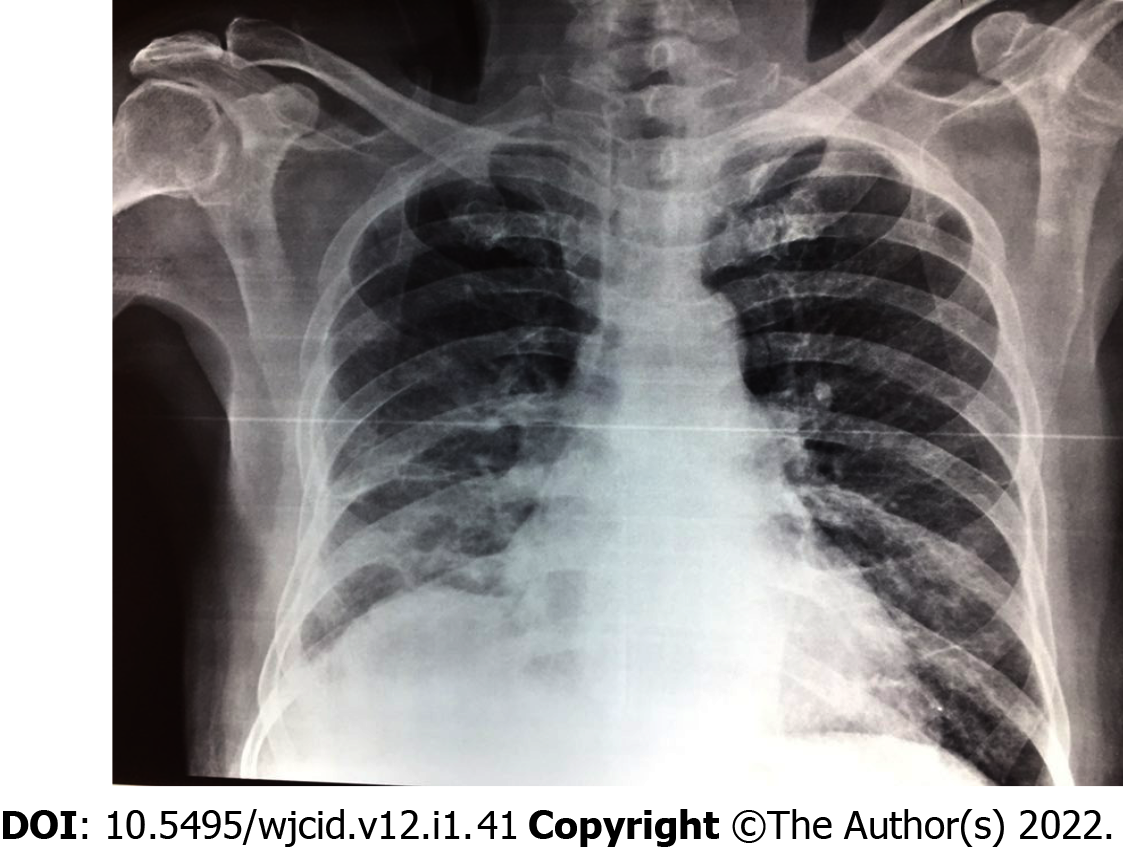
Chest X-ray on admission showed blunted right costophrenic angle (Figure 1).
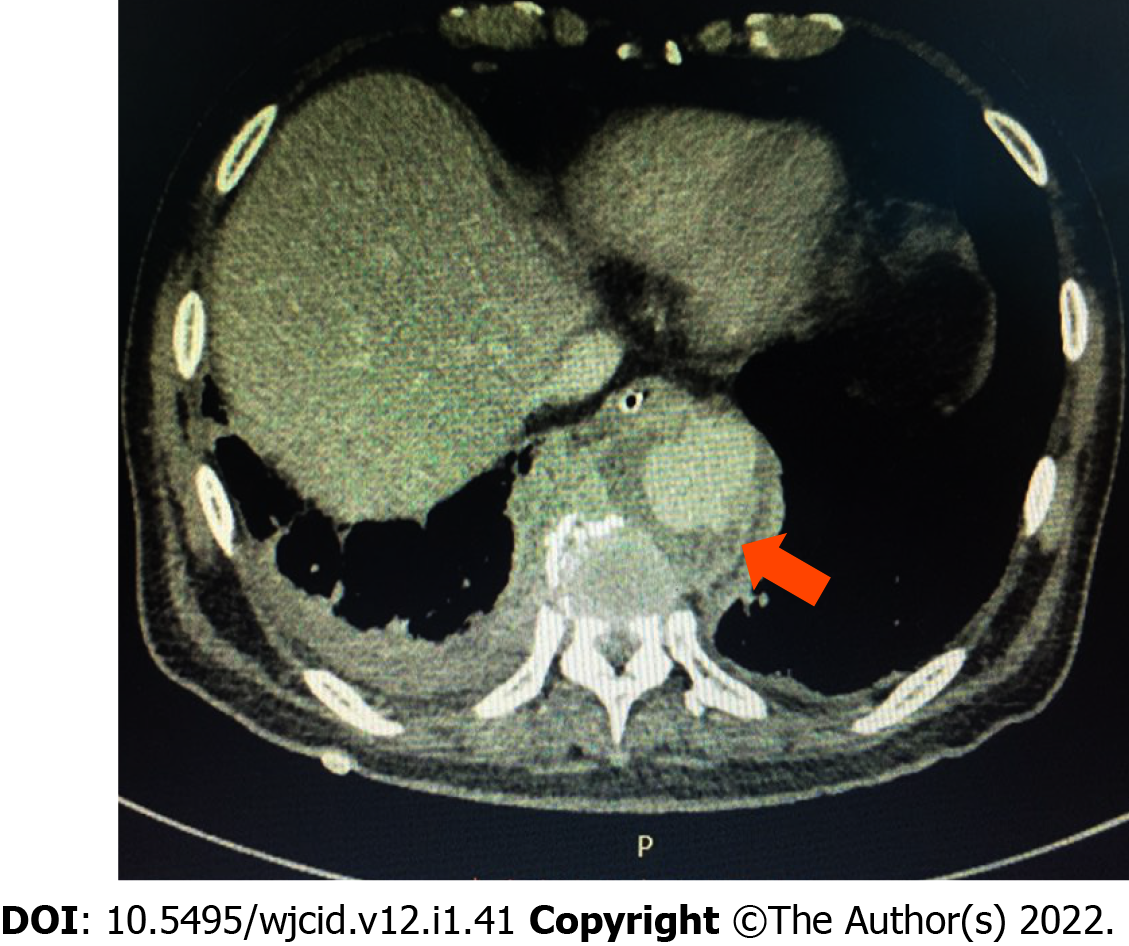
He was admitted to the medical ward with the diagnosis of pneumonia and acute on chronic kidney disease. He was started on intravenous (IV) ceftriaxone 2 g daily. Blood culture on admission was positive for nontyphoidal Salmonella spp. During the course of admission, he became more tachypneic, and right thoracocentesis was done in view of worsening pleural effusion, which drained out 250 mL of blood stained fluid. Lung ultrasound showed multiseptated right pleural effusion. Despite ultrasound guided pigtail drainage of right pleural effusion, his condition did not improve. Chest computed tomography (CT) demonstrated descending thoracic aorta saccular aneurysm with periaortic hematoma (Figure 2), likely due to recent bleed, and extending to the right pleural cavity. Pleural fluid culture was negative.
Salmonella infected aortic aneurysm.
He was referred to cardiothoracic surgery team and was planned for medical therapy in view of hemodynamical stability and no evidence of active leakage. There were multiple changes in his antibiotics regimen due to persistent fever (which included ceftazidime, piperacillin-tazobactam, meropenem, and cefepime). He completed 5 wk of antibiotics and was planned for a CT angiography of aorta at a later date to decide on surgical intervention.
Unfortunately, the patient was readmitted 2 mo later with abdominal discomfort and unable to pass motion for 1 wk. Abdominal X-ray demonstrated dilated large intestine. CT abdomen and pelvis showed descending thoracic aorta saccular aneurysm (slightly larger) with features suggestive of superimposed infection of periaortic hematoma; size of aneurysm: 2.4 cm × 3.6 cm and fecal laden bowels with features of impending intestinal obstruction. No obvious bowel related mass was seen. He was treated conservatively for the ileus, which resolved after 1 d. Blood culture on this admission was positive again for nontyphoidal Salmonella spp. Echocardiogram did not show any vegetations. He completed 6 wk of IV ampicillin and was discharged well. A repeated CT scan after 2 mo showed resolved periaortic hematoma; however, the patient refused surgical intervention and was given lifelong prophylactic oral antibiotic. Unfortunately, patient presented again with second recurrence after 1 mo, and blood culture was positive again for non-typhoidal Salmonella. He completed IV antibiotic and finally agreed for surgical intervention. He underwent endovascular aortic repair, and his condition remained stable with no recurrence of infection during his last follow-up after 2 years.
Infected aneurysm is a serious clinical condition. The term mycotic aneurysm was first described by William Osler in 1885[1], however the nomenclature of mycotic aneurysm vs infected aneurysm remains controversial as a majority of infected aneurysms are due to bacterial infection. Etiology of infected aneurysm includes direct bacterial inoculation, bacteremic seeding of existing intimal injury, atherosclerotic plaque, or preexisting aneurysm, contiguous infection, or septic emboli from heart, which can occlude vasa vasorum of blood vessel and lead to infected aneurysm.
Infected aortic aneurysm is a rare but life-threatening condition with devastating outcomes. Initial clinical presentations are often non-specific; therefore, misdiagnosis is common. Infected aortic aneurysms may manifest as vague pain at the back, chest, or abdomen. Some patients may present as pyrexia of unknown origin and remain undiagnosed until rupture of aneurysm. In our patient, he was only diagnosed with infected aortic aneurysm after 3 wk of admission.
Salmonella species and Staphylococcus aureus are the most common pathogens of infected aortic aneurysm, followed by other organisms such as Streptococci species, Treponema pallidum, and Mycobacterium spp[2-4]. In East Asia, gram negative bacteria related infected aortic aneurysm is more prevalent, where Salmonella species are the most common organisms[2,3,5,6]. It is important to obtain a microbiological diagnosis given the need for protracted courses of antimicrobial therapy. However, blood cultures are negative in around 50% of cases[5,7,8]. Initial empirical treatment is often required and guided by the most likely infecting organism according to the individual and clinical circumstances. It is also prudent to use antibiotics judiciously as prolonged broad spectrum antibiotics may lead to development of antimicrobial resistance. Salmonella has a strong affinity for large blood vessels and can easily adhere to the damaged vascular wall, strongly affecting the natural course of the disease. However, studies showed that non-Salmonella infections are associated with higher aneurysm-related complications and mortality after treatment[9].
The study by Oderich et al[10], with 43 patients with infected aortic aneurysm, found that the risk factors of aneurysm-related death were extensive periaortic infection, female gender, Staphylococcus aureus infection, aneurysm rupture, and suprarenal aneurysm location. Another larger series done in Taiwan reported that the independent predictors of aneurysm-related death were advanced age, non-Salmonella infection, and non-surgical treatment[2].
Until now, there are no randomized clinical trials to guide the management of infected aneurysm. Therapy mainly includes the control of infections by antibiotic and surgical debridement with or without reconstruction of arterial circulation. Management strategies are primarily based upon clinical experience guided by case series. The optimal duration of antibiotic therapy remains inconclusive. Most studies recommend at least 6 wk of antibiotic and stopping only when there is no longer clinical and laboratory evidence of ongoing sepsis[11,12].
Medical therapy alone is associated with devastating outcomes, with in-hospital mortality of 50%[13]. Since infected aortic aneurysm is at high risk of rupture, surgical treatment is encouraged in the absence of absolute contraindications. Open surgery with extensive debridement of infected tissue and in situ or extra-anatomical reconstruction has been the gold standard treatment. However, it is associated with high risk of morbidity and mortality[3,14-16]. Recently, endovascular techniques has become an emerging treatment alternative, especially in the treatment of patients at prohibitive risk for open surgery. Few studies have shown that endovascular treatment of infected aortic aneurysm is feasible and that it is a durable treatment option for high risk patients[17,18]. Luo et al[18] reported that survival at 1 mo, 6 mo, 1 year, and 5 year was 90%, 82%, 71%, and 53%, respectively. In addition, a European multicenter study of endovascular treatment for infected aortic aneurysm also showed similar results[17].
Infected aortic aneurysm is a rare clinical entity with high mortality. Due to non-specificity of the early symptoms, misdiagnosis is common. Our case highlights the importance of high index of suspicion of infected aortic aneurysm in patient with recurrent nontyphoidal Salmonella bacteremia. Endovascular technique has become an emerging treatment option.
We thank the Director-General of Health Malaysia for the permission to present these findings.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Infectious diseases
Country/Territory of origin: Malaysia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Schoenhagen P, United States; Shiryajev YN, Russia S-Editor: Wang LL L-Editor: Filipodia P-Editor: Wang LL
| 1. | Osler W. The Gulstonian Lectures, on Malignant Endocarditis. Br Med J. 1885;1:467-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 448] [Cited by in RCA: 438] [Article Influence: 31.3] [Reference Citation Analysis (0)] |
| 2. | Lin CH, Hsu RB. Primary Infected Aortic Aneurysm: Clinical Presentation, Pathogen, and Outcome. Acta Cardiol Sin. 2014;30:514-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 3. | Hsu RB, Chen RJ, Wang SS, Chu SH. Infected aortic aneurysms: clinical outcome and risk factor analysis. J Vasc Surg. 2004;40:30-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 184] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 4. | Jackman JD Jr, Radolf JD. Cardiovascular syphilis. Am J Med. 1989;87:425-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 95] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 5. | Hsu RB, Tsay YG, Wang SS, Chu SH. Surgical treatment for primary infected aneurysm of the descending thoracic aorta, abdominal aorta, and iliac arteries. J Vasc Surg. 2002;36:746-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 130] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 6. | Kan CD, Lee HL, Yang YJ. Outcome after endovascular stent graft treatment for mycotic aortic aneurysm: a systematic review. J Vasc Surg. 2007;46:906-912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 280] [Cited by in RCA: 275] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 7. | Johnson JR, Ledgerwood AM, Lucas CE. Mycotic aneurysm. New concepts in therapy. Arch Surg. 1983;118:577-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 126] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 8. | Maeda H, Umezawa H, Goshima M, Hattori T, Nakamura T, Umeda T, Shiono M. Primary infected abdominal aortic aneurysm: surgical procedures, early mortality rates, and a survey of the prevalence of infectious organisms over a 30-year period. Surg Today. 2011;41:346-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 56] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 9. | Wang JH, Liu YC, Yen MY, Wang JH, Chen YS, Wann SR, Cheng DL. Mycotic aneurysm due to non-typhi salmonella: report of 16 cases. Clin Infect Dis. 1996;23:743-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 70] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Oderich GS, Panneton JM, Bower TC, Cherry KJ Jr, Rowland CM, Noel AA, Hallett JW Jr, Gloviczki P. Infected aortic aneurysms: aggressive presentation, complicated early outcome, but durable results. J Vasc Surg. 2001;34:900-908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 300] [Cited by in RCA: 301] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 11. | Clough RE, Black SA, Lyons OT, Zayed HA, Bell RE, Carrell T, Waltham M, Sabharwal T, Taylor PR. Is endovascular repair of mycotic aortic aneurysms a durable treatment option? Eur J Vasc Endovasc Surg. 2009;37:407-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 97] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 12. | Deipolyi AR, Rho J, Khademhosseini A, Oklu R. Diagnosis and management of mycotic aneurysms. Clin Imaging. 2016;40:256-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 13. | Hsu RB, Chang CI, Wu IH, Lin FY. Selective medical treatment of infected aneurysms of the aorta in high risk patients. J Vasc Surg. 2009;49:66-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 52] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 14. | Müller BT, Wegener OR, Grabitz K, Pillny M, Thomas L, Sandmann W. Mycotic aneurysms of the thoracic and abdominal aorta and iliac arteries: experience with anatomic and extra-anatomic repair in 33 cases. J Vasc Surg. 2001;33:106-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 474] [Cited by in RCA: 450] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 15. | Yu SY, Hsieh HC, Ko PJ, Huang YK, Chu JJ, Lee CH. Surgical outcome for mycotic aortic and iliac anuerysm. World J Surg. 2011;35:1671-1678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 16. | Dubois M, Daenens K, Houthoofd S, Peetermans WE, Fourneau I. Treatment of mycotic aneurysms with involvement of the abdominal aorta: single-centre experience in 44 consecutive cases. Eur J Vasc Endovasc Surg. 2010;40:450-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 90] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 17. | Sörelius K, Mani K, Björck M, Sedivy P, Wahlgren CM, Taylor P, Clough RE, Lyons O, Thompson M, Brownrigg J, Ivancev K, Davis M, Jenkins MP, Jaffer U, Bown M, Rancic Z, Mayer D, Brunkwall J, Gawenda M, Kölbel T, Jean-Baptiste E, Moll F, Berger P, Liapis CD, Moulakakis KG, Langenskiöld M, Roos H, Larzon T, Pirouzram A, Wanhainen A; European MAA collaborators. Endovascular treatment of mycotic aortic aneurysms: a European multicenter study. Circulation. 2014;130:2136-2142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 196] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 18. | Luo CM, Chan CY, Chen YS, Wang SS, Chi NH, Wu IH. Long-term Outcome of Endovascular Treatment for Mycotic Aortic Aneurysm. Eur J Vasc Endovasc Surg. 2017;54:464-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 52] [Article Influence: 6.5] [Reference Citation Analysis (0)] |