Published online Sep 18, 2020. doi: 10.5495/wjcid.v10.i3.42
Peer-review started: July 9, 2020
First decision: July 21, 2020
Revised: August 2, 2020
Accepted: September 1, 2020
Article in press: September 1, 2020
Published online: September 18, 2020
Processing time: 63 Days and 16.1 Hours
The hypercoagulable state associated with coronavirus disease 2019 (COVID-19) has been shown to complicate the course of this viral illness with both venous and arterial clots. Often presenting after hospitalization and known COVID-19 diagnosis, the etiology of thrombosis has been attributed to the hyperinflammatory state and endothelial dysfunction associated with COVID-19. This report portrays a patient who experienced an aortic thrombosis resulting in back and leg pain with subsequent loss of motor function of his legs as his initial presentation of COVID-19.
Patient is a 60-year-old Caucasian male with no medical history who presented with sudden onset pain in his lower back and lower extremities. He went on to experience complete motor loss of the lower extremities two hours after admission. Chest pain and shortness of breath developed one day later but were not present at time of presentation. Computed tomography angiography of the chest, abdomen, and pelvis revealed occlusion by thrombosis of the abdominal aorta in addition to multifocal pulmonary ground-glass opacities prompting COVID-19 PCR, which was positive. He was taken to surgery for attempted thrombectomy and the thrombus was retrieved starting from the right common femoral artery, but a second thrombus had immediately reformed in place of the prior thrombectomy site resulting in conclusion of the procedure. He was continued on unfractionated heparin and received a dose of tocilizumab 400 mg, but rapidly developed hemodynamic compromise and expired from cardiac arrest.
This presentation emphasizes the importance of evaluating patients for COVID-19 who experience unusual thromboses without superior explanation.
Core Tip: Aortic thrombosis preceding respiratory symptoms should raise suspicion for testing for coronavirus disease 2019 in patients with unusual thrombosis presentation.
- Citation: Webster WZ, Sraow A, Cruz Morel K. Abdominal aortic thrombosis as initial presentation of COVID-19 infection: A case report. World J Clin Infect Dis 2020; 10(3): 42-46
- URL: https://www.wjgnet.com/2220-3176/full/v10/i3/42.htm
- DOI: https://dx.doi.org/10.5495/wjcid.v10.i3.42
The known hypercoagulable state associated with coronavirus disease 2019 (COVID-19) infection has been implicated as a common cause of morbidity and mortality. The presentation can range from microthrombi to large thromboses in both intra- and extrapulmonary vessels. In addition, the diagnosis of thrombosis often occurs days to weeks after the initial onset of respiratory symptoms, resulting in worsening of overall clinical status and prognosis. One study in France showed that pulmonary embolism (PE) was diagnosed with a mean of 12 days since initial onset of symptoms in COVID positive patients[1]. The converse, of having an obvious thrombotic event preceding onset of respiratory symptoms, may lead providers away from testing a patient for COVID-19. There have been two reports of aortic thromboses in patients with COVID-19 pneumonia, but thrombosis occurred after the patient was already known to be positive for COVID-19. The hypercoagulable state associated with this infection should be considered in patients with no obvious risk factors for thrombosis or evidence of thrombosis in an unusual location, as endothelial dysfunction coupled with hyperinflammation are thought to be mediators of this hypercoagulable state. In this case report, we describe a patient who presented with back and leg pain, and further work up revealed extensive thrombosis in the aorta, iliac, and superior mesenteric arteries (SMA). His abnormal chest imaging prompted PCR testing for COVID-19, which was positive. Our case displays the importance of appreciating the hypercoagulability associated with COVID-19 and raises awareness to a variety of possible presentations.
Patient is a 60-year-old incarcerated Caucasian male with no past medical history who presented to the hospital with complaints of sudden onset pain in his lower back and lower extremities.
He went on to experience complete motor loss of the lower extremities two hours after admission. Chest pain and shortness of breath developed one day later but were not present at time of presentation. He did not have any other symptoms indicative of infection including fever, chills, or cough. He was not taking any medications.
Patient has no past medical history.
Vitals at presentation were blood pressure 99/47, pulse 126 beats per minute, temperature 36.8 oC, respirations 15 per minute, and oxygenation 99% on room air. Neurologic exam of the lower extremities initially revealed 3/5 motor strength, but sensation was intact. Repeat exam in 2 hours revealed complete motor loss of the lower extremities. Dorsalis pedis and posterior tibial pulses were not palpable and femoral pulses were weak at 1+. Pulmonary exam revealed diffuse rhonchi in all lung fields. Cardiac exam revealed tachycardia, but no murmurs were noted, and the rhythm was regular. He was alert and oriented to person, place, and time.
Patient had a positive COVID-19 PCR blood test. His laboratory values were remarkable for leukocytosis of 22.3 cells/L (4.5-11.0) with an absolute lymphocyte count of 0.58 K/uL (1.32-3.57), PT 16.4 seconds (12-14.5), INR 1.3 U (< 1.0), PTT 28.9 seconds (23.9-36.6), and d-dimer > 20 µg/mL (< 0.5). Ferritin was significantly elevated at > 40000 µg/L (22-275), C reactive protein was 210 mg/L (0-5), and creatine phosphokinase was 46800 U/L (0-200).
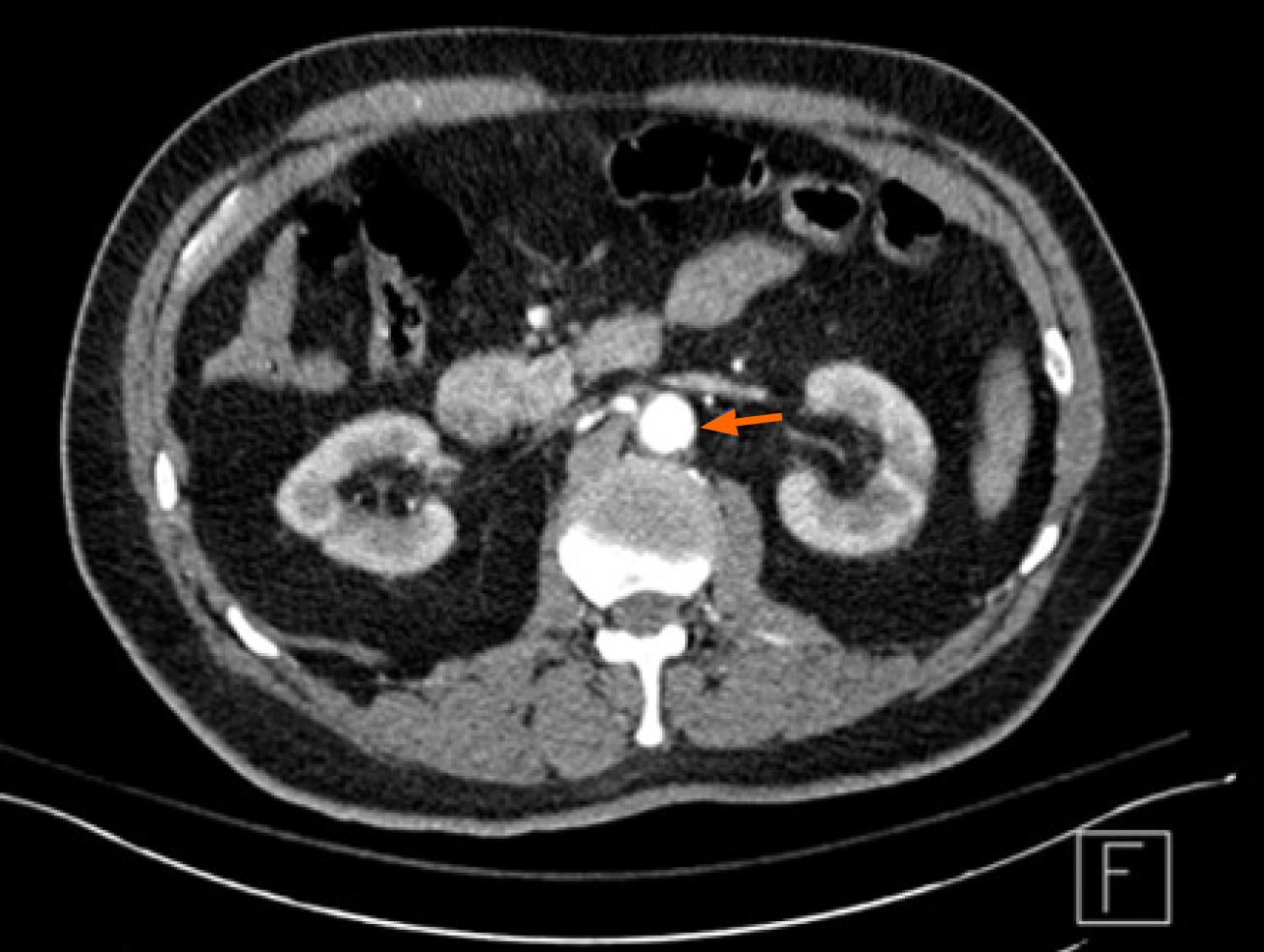
Patient underwent computed tomography (CT) angiography of the chest, abdomen, and pelvis which revealed occlusion by thrombosis of the abdominal aorta, depicted in Figures 1 and 2, in the infrarenal segment with extension to his iliac arteries with reconstitution of flow in the bilateral common femoral arteries. Additional nonocclusive thrombosis in the SMA was noted. In addition to these thromboses, multifocal ground-glass opacities were visualized in the bilateral lung fields which prompted COVID-19 PCR testing.
This patient suffered from an occlusive abdominal aortic thrombosis secondary to COVID-19 infection.
Patient was emergently taken to surgery for attempted thrombectomy and a heavy burden of thrombus was retrieved starting initially from the right common femoral artery. After several minutes of closing of vasculature, it was noted that the femoral artery pulsation had weakened and disappeared and it was noted that a second thrombus had formed again in place of the prior thrombectomy site after reevaluation despite running of heparin. At this point, the procedure was concluded as it was clear that the patient was hypercoagulable due to his COVID-19 infection.
Patient remained intubated following the operation due to respiratory compromise in the setting of his known COVID-19 pneumonia. He was continued solely on unfractionated heparin infusion at 18 U/kg/h. He also received a dose of Tocilizumab 400 mg, but continued to worsen from a hemodynamic standpoint, requiring the initiation of vasopressors. No additional anti-viral agents or COVID-19 targeted therapies were employed.
Despite ventilatory support and triple vasopressors with norepinephrine, phenylephrine, and epinephrine, patient continued to deteriorate and soon expired from cardiac arrest in the setting of his occlusive abdominal thrombosis.
As a respiratory virus, COVID-19 typically presents with signs of lung infection including shortness of breath, cough, and fever which can progress to acute respiratory distress syndrome. Patients requiring admission to an intensive care unit (ICU) have been found to have acute thromboses, most commonly being PE in the setting of the severe inflammatory response, endothelial dysfunction, and multi-organ system failure elicited by the virus. Overt thrombosis has been reported to be as high as 25%-50% in this population[2]. Unlike traditional thrombotic events in ICU patients, COVID-19-associated thrombosis has a higher incidence of arterial clot and a greater mortality[3,4]. In a study of three Dutch hospitals, there was a 31% incidence of thrombosis in ICU patients, with 3.7% being arterial[5]. Markers such as D-dimer, lactate dehydrogenase, ferritin, and CRP have been used to stratify patients for risk of thrombosis and potential benefit with prophylactic anticoagulation, but degree of elevation associated with arterial clot has yet to be appreciated.
A report by Berre et al[6] presented a patient who was found to have acute aortic thrombosis and concomitant pulmonary embolism after being diagnosed with COVID-19 pneumonia. This patient was found to have a D-dimer of 17.28 µg/mL with normal platelets and prothrombin time. An additional report by Katchanov et al[7] described a patient with extensive aortic thrombosis and a D-dimer level of 15.28 µg/mL. Consistent with this trend of severely elevated inflammatory markers, particularly D-dimer, our patient’s D-dimer was severely elevated at > 20 µg/mL and ferritin > 40000 µg/L. These findings suggest that extensive thrombosis involving the arterial circulation may be more likely at the far end of the spectrum of extreme inflammation and endothelial dysfunction. Interestingly, both our patient and the above case presented by Katchanov et al[7] showed involvement of the abdominal aorta and iliac arteries in addition to occlusion of the SMA. Given these two reports of SMA occlusion and the possibility of intestinal ischemia, providers should consider this in patients to receive the anti-IL-6 agent tocilizumab for severe inflammatory dysregulation, as intestinal perforation is a known side effect despite its single-dose indication[8]. Alternative COVID-19 directed therapies include the anti-viral remdesivir and convalescent plasma, as these agents may have been additional options for this patient in absence of his rapid clinical decline. Due to the fact that his decline was thought to be more related to his aortic thrombosis and not to COVID-19 induced lung dysfunction, the mainstay of therapy was unfractionated heparin, which was chosen due to rapid reversibility compared to newer direct oral anticoagulants such as apixaban or rivaroxaban.
As arterial thrombi may not always be visualized with routine CT angiography PE protocols, it is important to consider additional scanning for patients with severely elevated inflammatory markers in which suspicion is high for arterial clot. A contrast CT of the abdomen or aortic CT angiography may be necessary to diagnose these aortic thromboses, and our patient was diagnosed with CT angiography of the chest, abdomen, and pelvis given his overt lower back and lower extremity pain as his presenting symptoms. The most impressive finding in our patient was the evidence of a rapidly forming thrombi after successfully removing the initial thrombi and reperfusion of the lower extremities. This echoes the profound hypercoagulable state as a result of COVID-19.
Acute thrombosis in the setting of COVID-19 can be a devastating complication with a drastic increase in morbidity and mortality. Our case highlights the profound hypercoagulable state of severe inflammatory response due to COVID-19, with the rapid formation of a thrombi immediately following thrombectomy, compromising perfusion and hastening refractory shock and death. We hope to raise awareness in the importance of recognizing arterial thrombi as a result of COVID-19 in patients with no other obvious explanation, as a prompt diagnosis may influence potential treatment options and lead to better outcomes.
Thanks given to the Prisma Health Richland ICU staff for their dedication to their patients in this COVID-19 era.
Manuscript source: Unsolicited manuscript
Specialty type: Infectious diseases
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Moschovi MA, Nagahara H, Sipos F, Wang YP, Wang W S-Editor: Gong ZM L-Editor: A P-Editor: Xing YX
| 1. | Radiological Society of North America. "New research highlights blood clot dangers of COVID-19." ScienceDaily. April 2020. Available from: www.sciencedaily.com/releases/2020/04/200423143100.htm. |
| 2. | Beun R, Kusadasi N, Sikma M, Westerink J, Huisman A. Thromboembolic events and apparent heparin resistance in patients infected with SARS-CoV-2. Int J Lab Hematol. 2020;42 Suppl 1:19-20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 98] [Cited by in RCA: 122] [Article Influence: 24.4] [Reference Citation Analysis (0)] |
| 3. | Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18:1094-1099. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2447] [Cited by in RCA: 2509] [Article Influence: 501.8] [Reference Citation Analysis (1)] |
| 4. | Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:844-847. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3992] [Cited by in RCA: 4039] [Article Influence: 807.8] [Reference Citation Analysis (0)] |
| 5. | Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, Kaptein FHJ, van Paassen J, Stals MAM, Huisman MV, Endeman H. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145-147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3488] [Cited by in RCA: 3407] [Article Influence: 681.4] [Reference Citation Analysis (0)] |
| 6. | Le Berre A, Marteau V, Emmerich J, Zins M. Concomitant acute aortic thrombosis and pulmonary embolism complicating COVID-19 pneumonia. Diagn Interv Imaging. 2020;101:321-322. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 69] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 7. | Katchanov J, Kalisch J, Herzing W, Knorr F, Havla M, Klink T, Dommke C. Extensive Aortic Thrombosis in a Patient With COVID-19. Ann Emerg Med. 2020;76:373-374. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Vikse J, Henry BM. Tocilizumab in COVID-19: Beware the risk of intestinal perforation. Int J Antimicrob Agents. 2020;56:106009. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |