Peer-review started: November 10, 2014
First decision: November 27, 2014
Revised: December 9, 2014
Accepted: December 18, 2014
Article in press: December 19, 2014
Published online: February 23, 2015
Processing time: 95 Days and 4.2 Hours
Association of diabetes with hypertension is frequent and it well known that high blood pressure potentiates the probability of diabetic patients to develop macrovascular and microvascular complications. Strong evidence obtained in a number of large scale prospective studies indicates that adequate blood pressure control in diabetic patients is highly beneficial for prevention of cardiovascular events. Nonetheless, only a limited proportion of hypertensive-diabetic individuals included in studies on anti-hypertensive treatment has met the predefined blood pressure goal. The optimal blood pressure goal to be pursued in diabetic patients with hypertension to guarantee effective protection from cardiovascular outcomes is still under intense debate and recommendations of current guidelines on hypertension treatment are still inconsistent. We comment here on the most important studies and conclude that current evidence does not conclusively support the need to reach a blood pressure target in hypertensive patients with diabetes different from nondiabetic hypertensive individuals.
Core tip: Hypertension potentiates the probability of diabetic patients to develop macrovascular and microvascular complications and prospective studies demonstrate that adequate blood pressure control in diabetic patients is highly beneficial for prevention of cardiovascular events. Blood pressure targets in diabetic patients with high blood pressure are under debate and are discussed in this editorial.
- Citation: Catena C, Colussi G, Nait F, Brosolo G, Sechi LA. Diabetes, diabetic complications, and blood pressure targets. World J Hypertens 2015; 5(1): 1-5
- URL: https://www.wjgnet.com/2220-3168/full/v5/i1/1.htm
- DOI: https://dx.doi.org/10.5494/wjh.v5.i1.1
Diabetes mellitus and arterial hypertension are important modifiable risk factors for cardiovascular mobidity and mortality. Association of diabetes with hypertension is frequent and if, on one hand, incidence of hypertension in patients with type-2 diabetes is two times higher than in matched subjects without diabetes[1], on the other hand risk of patients with hypertension to develop diabetes is three-fold that of patients with normal blood pressure (BP)[2]. The frequent association between diabetes and hypertension may depend from a variety of mechanisms. These mechanisms include primarily aging, increased body weight, and insulin resistance[3,4], although a contribution of vasoconstriction and vascular rarefaction has also been suggested[5].
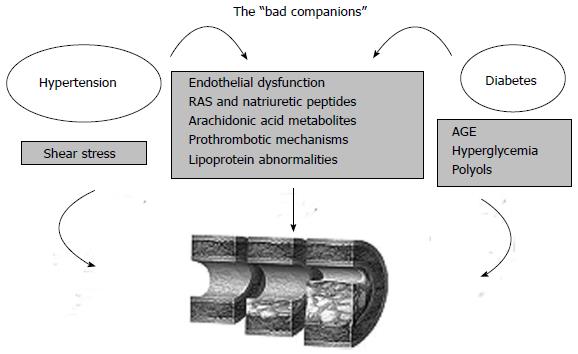
Presence of hypertension potentiates the probability of diabetic patients to develop macrovascular and microvascular complications and this is why these two conditions have been often identified as “the bad companions” (Figure 1). In addition to mechanisms that are peculiar of each disease such as effects of hyperglycemia, advanced glycation products, and polyols on the side of diabetes, and increased shear stress on the side of hypertension, these two conditions share many pathophysiologic mechanisms that contribute to cardiac and vascular damage. These mechanisms include endothelial dysfunction, activation of the renin-angiotensin system, proinflammatory and prothrombotic mechanisms, lipoprotein abnormalities, and changes in arachidonic acid metabolites levels. Type-2 diabetic patients with hypertension are at increased risk of coronary heart disease, stroke, heart failure, and renal insufficiency and association with additional comorbidities such as dyslipidemia and obesity contribute to this risk[6]. It is known that presence of hypertension doubles the risk of coronary heart disease and stroke in patients with diabetes[7]. Moreover, diabetes is a major risk factor for left ventricular dysfunction and heart failure. In a Scottish study, incidence of left ventricular dysfunction in diabetic patients was four-fold that of nondiabetic individuals[8] and in the Framingham Study the relative risk of heart failure in diabetic women was 5.5 as compared to nondiabetic women[9]. These diabetic patients have a poor prognosis that can be explained by underlying diabetic cardiomyopathy that is exacerbated by hypertension[10].
As a proof of the contribution of hypertension to diabetic complications, robust clinical evidence indicates that adequate BP control in diabetic patients is highly beneficial[11]. These benefits have been clearly demonstrated in a number of large scale prospective studies[12-18]. However, diabetic patients require more intense treatment and only a minority of them meets the BP target[19]. Cumulative analyses of major clinical trials on hypertension treatment that have included patients with diabetes have shown that in these patients target diastolic BP values were met in approximately half of the studies whereas none of the studies met the target systolic BP[20]. The target BP to be achieved to provide effective protection from cardiovascular events to diabetic-hypertensive patients has been intensively debated and recommendation of recent guidelines on treatment of hypertension are somehow inconsistent[21-27] (Table 1) due to different relevance that has been given to some major randomized controlled trials (RCTs) showing the opportunity to reach lower BP levels in diabetic than nondiabetic hypertensive individuals[12,13].
The United Kingdom Prospective Diabetes Study (UKPDS 38)[12] was the first important RCT to investigate whether tighter control of BP prevents macrovascular and microvascular complications of diabetes reporting a 24% reduction of diabetes related endpoints as compared to patients on a more conventional anti-hypertensive treatment. The Hypertension Optimal Treatment study[13] allocated 18790 hypertensive patients to three different diastolic BP goals (< 90, < 85, and < 80 mmHg, respectively) and reported a 51% reduction in major cardiovascular events in patients with diabetes in the target group < 80 mmHg as compared to the target group < 90 mmHg. Prompted by these and other observations a meta-analysis of 27 RCTs that included 33395 hypertensive-diabetic patients compared the effects of different BP lowering regimens on cardiovascular events and death[28]. In this meta-analysis, evidence that lower BP goals produce better outcomes in hypertensive individuals with vs without diabetes was limited to cardiovascular events, but was not reported for the combined endpoint of cardiovascular events and death. Thus, it was concluded that the cardiovascular effects of more less intensive BP lowering regimens were broadly comparable in patients with or without diabetes.
Traditional BP-treatment strategies set levels at which treatment is initiated and goals to which treatment should be titrated. Due to the uncertain cardiovascular benefit of more aggressive BP lowering regimens in diabetics, the Action in Diabetes and Vascular Disease trial[29] investigated the effects on cardiovascular events of the routine administration of a fixed-dose angiotensin converting enzyme inhibitor-diuretic combination as an alternative to the more traditional BP goal-driven therapy. In this study the relative risk of combined macrovascular and microvascular events was reduced by 9% in diabetic patients treated with the fixed combination showing the possible validity of this alternative treatment approach. Later on, the Steno-2 Study[30] tested in 160 type-2 diabetic patients a multifactorial intervention with an intensive approach to correct blood pressure, glycated hemoglobin, and plasma cholesterol and triglyceride levels that was compared to conventional therapy. Blood pressure target was set at values below 130/80 mmHg in the intensively treated group and, in these patients, mortality and cardiovascular events were reduced by 50% by 29% respectively, as compared to conventional treatment in a follow-up of 13 years. Because of the weak evidence obtained in RCTs in support of a strategy of lowering systolic BP below 130 mmHg as recommended in some hypertension guidelines published in the late 2010s[31,32], the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial[33] was specifically designed to test whether a systolic BP treatment target < 120 mmHg was more effective than a target < 140 mmHg in prevention of major cardiovascular events in high-risk patients with type-2 diabetes. A total of 4733 patients were randomly assigned to intensive or standard therapy and the primary composite outcome of nonfatal myocardial infarction, nonfatal stroke, or cardiovascular death was assessed after and average follow-up of 4.7 years. In this study, despite a sustained and significant difference in systolic BP, the annual rates of the composite primary outcome, myocardial infarction, stroke, and all cause death were not different from the intensive-treatment and standard-treatment group. Conversely, serious adverse events that could be attributed to anti-hypertensive treatment were significantly more frequent in the intensive-therapy group. Thus, despite the many limitations of the ACCORD trial (e.g., open-label design, low-rate of cardiovascular events in treatment groups, exclusion of patients younger than 40 year, etc.) the current evidence, by no means, indicates the need to pursue in hypertensive individuals with diabetes lower BP goals than in the rest of people with high blood pressure.
The writing of guidelines is a difficult task and in the case of hypertension a myriad of factors can contribute to definition of blood pressure targets that should be reached with treatment. Frequency of disease and its complications is variable in different populations and, for instance, incidence of diabetes increases at different rates around the world. Also the impact of disease on organ complications and pattern of comorbidities are largely different explaining why the evidence obtained in randomized clinical trails often translates in different recommendations. Variability in drug responses among different populations, urbanization, availability of resources, and, last but not least, vested interests of governments or industry can have relevance[34]. Overall, the old tenet that one size does not fit all holds well when discussing blood pressure targets. And this is particularly true in diabetics in whom age, comorbidities, different types of organ complications have serious impact on treatment choices. For instance, elderly patients have no evidence of benefits when systolic blood pressure is reduced below 140 mmHg[21]. And in this view, specific consideration deserve diabetic patients with proteinuric nephropathy who notoriously are at very high risk of cardiovascular events and based upon the results of systematic reviews[35] guidelines still recommend a target blood pressure of less than 130 mmHg.
In conclusion, the BP target to be achieved in hypertensive patients with diabetes to guarantee effective protection from major cardiovascular events is still subject of intense debate. Although many hypertension guidelines had recommended a BP goal of less than 130/80 mmHg in these patients, a reappraisal of the available evidence[36] mainly based upon the results of the ACCORD trial does not support this recommendation and it appears that in hypertensive patients with diabetes the same BP targets of nondiabetic hypertensive individuals should be recommended. Based upon this evidence the most recent guidelines for treatment of hypertension have changed their previous indications, but inconsistencies still exist making clear that further research will be needed to reach a shared opinion on this important topic.
P- Reviewer: Li CG, Tasci I S- Editor: Tian YL L- Editor: A E- Editor: Wu HL
| 1. | Sowers JR. Recommendations for special populations: diabetes mellitus and the metabolic syndrome. Am J Hypertens. 2003;16:41S-45S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 65] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 2. | Gress TW, Nieto FJ, Shahar E, Wofford MR, Brancati FL. Hypertension and antihypertensive therapy as risk factors for type 2 diabetes mellitus. Atherosclerosis Risk in Communities Study. N Engl J Med. 2000;342:905-912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 812] [Cited by in RCA: 747] [Article Influence: 29.9] [Reference Citation Analysis (0)] |
| 3. | Crawford AG, Cote C, Couto J, Daskiran M, Gunnarsson C, Haas K, Haas S, Nigam SC, Schuette R. Prevalence of obesity, type II diabetes mellitus, hyperlipidemia, and hypertension in the United States: findings from the GE Centricity Electronic Medical Record database. Popul Health Manag. 2010;13:151-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 96] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 4. | Sechi LA. Mechanisms of insulin resistance in rat models of hypertension and their relationships with salt sensitivity. J Hypertens. 1999;17:1229-1237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 59] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Sowers JR. Insulin resistance and hypertension. Am J Physiol Heart Circ Physiol. 2004;286:H1597-H1602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 304] [Cited by in RCA: 306] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 6. | Bonow RO, Mitch WE, Nesto RW, O’Gara PT, Becker RC, Clark LT, Hunt S, Jialal I, Lipshultz SE, Loh E. Prevention Conference VI: Diabetes and Cardiovascular Disease: Writing Group V: management of cardiovascular-renal complications. Circulation. 2002;105:e159-e164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Stevens RJ, Coleman RL, Adler AI, Stratton IM, Matthews DR, Holman RR. Risk factors for myocardial infarction case fatality and stroke case fatality in type 2 diabetes: UKPDS 66. Diabetes Care. 2004;27:201-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 201] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 8. | McDonagh TA, Morrison CE, Lawrence A, Ford I, Tunstall-Pedoe H, McMurray JJ, Dargie HJ. Symptomatic and asymptomatic left-ventricular systolic dysfunction in an urban population. Lancet. 1997;350:829-833. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 392] [Cited by in RCA: 435] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 9. | Iribarren C, Karter AJ, Go AS, Ferrara A, Liu JY, Sidney S, Selby JV. Glycemic control and heart failure among adult patients with diabetes. Circulation. 2001;103:2668-2673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 479] [Cited by in RCA: 504] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 10. | Bell DS. Heart failure: the frequent, forgotten, and often fatal complication of diabetes. Diabetes Care. 2003;26:2433-2441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 290] [Cited by in RCA: 304] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 11. | Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352:854-865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5771] [Cited by in RCA: 5271] [Article Influence: 195.2] [Reference Citation Analysis (0)] |
| 12. | Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study Group. BMJ. 1998;317:703-713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4930] [Cited by in RCA: 4267] [Article Influence: 158.0] [Reference Citation Analysis (0)] |
| 13. | Hansson L, Zanchetti A, Carruthers SG, Dahlöf B, Elmfeldt D, Julius S, Ménard J, Rahn KH, Wedel H, Westerling S. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet. 1998;351:1755-1762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3920] [Cited by in RCA: 3558] [Article Influence: 131.8] [Reference Citation Analysis (0)] |
| 14. | Curb JD, Pressel SL, Cutler JA, Savage PJ, Applegate WB, Black H, Camel G, Davis BR, Frost PH, Gonzalez N. Effect of diuretic-based antihypertensive treatment on cardiovascular disease risk in older diabetic patients with isolated systolic hypertension. Systolic Hypertension in the Elderly Program Cooperative Research Group. JAMA. 1996;276:1886-1892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 15. | Tuomilehto J, Rastenyte D, Birkenhäger WH, Thijs L, Antikainen R, Bulpitt CJ, Fletcher AE, Forette F, Goldhaber A, Palatini P. Effects of calcium-channel blockade in older patients with diabetes and systolic hypertension. Systolic Hypertension in Europe Trial Investigators. N Engl J Med. 1999;340:677-684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 642] [Cited by in RCA: 540] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 16. | Estacio RO, Jeffers BW, Gifford N, Schrier RW. Effect of blood pressure control on diabetic microvascular complications in patients with hypertension and type 2 diabetes. Diabetes Care. 2000;23 Suppl 2:B54-B64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 17. | Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICRO-HOPE substudy. Heart Outcomes Prevention Evaluation Study Investigators. Lancet. 2000;355:253-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2440] [Cited by in RCA: 2070] [Article Influence: 82.8] [Reference Citation Analysis (0)] |
| 18. | Cooper-DeHoff RM, Gong Y, Handberg EM, Bavry AA, Denardo SJ, Bakris GL, Pepine CJ. Tight blood pressure control and cardiovascular outcomes among hypertensive patients with diabetes and coronary artery disease. JAMA. 2010;304:61-68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 511] [Cited by in RCA: 454] [Article Influence: 30.3] [Reference Citation Analysis (0)] |
| 19. | Suh DC, Kim CM, Choi IS, Plauschinat CA, Barone JA. Trends in blood pressure control and treatment among type 2 diabetes with comorbid hypertension in the United States: 1988-2004. J Hypertens. 2009;27:1908-1916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 69] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 20. | Mancia G, Grassi G. Systolic and diastolic blood pressure control in antihypertensive drug trials. J Hypertens. 2002;20:1461-1464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 180] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 21. | Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31:1281-1357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3425] [Cited by in RCA: 3342] [Article Influence: 303.8] [Reference Citation Analysis (0)] |
| 22. | James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5429] [Cited by in RCA: 5503] [Article Influence: 500.3] [Reference Citation Analysis (0)] |
| 23. | Hackam DG, Quinn RR, Ravani P, Rabi DM, Dasgupta K, Daskalopoulou SS, Khan NA, Herman RJ, Bacon SL, Cloutier L. The 2013 Canadian Hypertension Education Program recommendations for blood pressure measurement, diagnosis, assessment of risk, prevention, and treatment of hypertension. Can J Cardiol. 2013;29:528-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 136] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 24. | American Diabetes Association. Standards of medical care in diabetes--2013. Diabetes Care. 2013;36 Suppl 1:S11-S66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2371] [Cited by in RCA: 2481] [Article Influence: 206.8] [Reference Citation Analysis (0)] |
| 25. | Chapter 4: Blood pressure management in CKD ND patients with diabetes mellitus. Kidney Int Suppl (2011). 2012;2:363-369. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | National Institute for Health and Clinical Excellence. Hypertension: Clinical management of primary hypertension in adults (updated 2013 October). Available from: http: //www.nice.org.uk/guidance/cg127. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 27. | López-Jaramillo P, Sánchez RA, Diaz M, Cobos L, Bryce A, Parra Carrillo JZ, Lizcano F, Lanas F, Sinay I, Sierra ID. Latin American consensus on hypertension in patients with diabetes type 2 and metabolic syndrome. J Hypertens. 2013;31:223-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 53] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 28. | Turnbull F, Neal B, Algert C, Chalmers J, Chapman N, Cutler J, Woodward M, MacMahon S. Effects of different blood pressure-lowering regimens on major cardiovascular events in individuals with and without diabetes mellitus: results of prospectively designed overviews of randomized trials. Arch Intern Med. 2005;165:1410-1419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 585] [Cited by in RCA: 602] [Article Influence: 30.1] [Reference Citation Analysis (0)] |
| 29. | Patel A, MacMahon S, Chalmers J, Neal B, Woodward M, Billot L, Harrap S, Poulter N, Marre M, Cooper M. Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus (the ADVANCE trial): a randomised controlled trial. Lancet. 2007;370:829-840. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1475] [Cited by in RCA: 1428] [Article Influence: 79.3] [Reference Citation Analysis (0)] |
| 30. | Gaede P, Lund-Andersen H, Parving HH, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med. 2008;358:580-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2459] [Cited by in RCA: 2351] [Article Influence: 138.3] [Reference Citation Analysis (0)] |
| 31. | Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560-2572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13416] [Cited by in RCA: 13291] [Article Influence: 604.1] [Reference Citation Analysis (0)] |
| 32. | Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S. 2007 Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2007;25:1105-1187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 33. | Cushman WC, Evans GW, Byington RP, Goff DC, Grimm RH, Cutler JA, Simons-Morton DG, Basile JN, Corson MA, Probstfield JL. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575-1585. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2787] [Cited by in RCA: 2453] [Article Influence: 163.5] [Reference Citation Analysis (0)] |
| 34. | Jennings GL, Touyz RM. Hypertension guidelines: more challenges highlighted by Europe. Hypertension. 2013;62:660-665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 35. | Upadhyay A, Earley A, Haynes SM, Uhlig K. Systematic review: blood pressure target in chronic kidney disease and proteinuria as an effect modifier. Ann Intern Med. 2011;154:541-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 264] [Cited by in RCA: 231] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 36. | Arguedas JA, Leiva V, Wright JM. Blood pressure targets for hypertension in people with diabetes mellitus. Cochrane Database Syst Rev. 2013;10:CD008277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |