Published online May 23, 2014. doi: 10.5494/wjh.v4.i2.15
Revised: May 4, 2014
Accepted: May 14, 2014
Published online: May 23, 2014
Processing time: 69 Days and 18.7 Hours
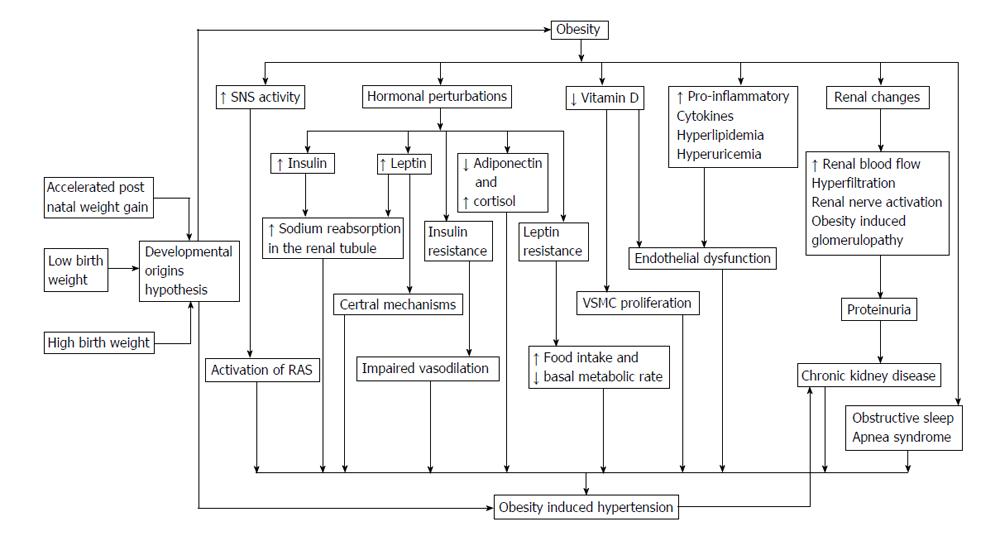
The prevalence of obesity related hypertension has dramatically increased in children with the parallel increase in pediatric obesity. This pediatric health problem may adversely affect cardiovascular health in adult life. The pathogenesis of hypertension in obese children is not widely understood. We therefore undertake this review to raise public awareness. Early childhood parameters like birth weight and postnatal weight gain may play important roles in risk for obesity and obesity related hypertension later in childhood and adult life. Further information is required to confirm this origin of hypertension so that appropriate measures are taken in the peri-natal period. The role of sympathetic nervous system has now been well established as one of the principle mechanisms involved in obesity related hypertension. The Renin-Angiotensin system, insulin resistance due to obesity and as a part of metabolic syndrome along with imbalance in adipokines such as leptin and adiponectin, cause activation of the sympathetic system, vasoconstriction, endothelial dysfunction and sodium reabsorption among other perturbations. Multi-step interventions targeting these various mechanisms are required to break the cycle of obesity and metabolic syndrome. Vitamin D deficiency, sleep apnea due to airway obstruction and hyperuricemia may also play a significant role and should not be ignored in its early stages. Obesity is a risk factor for other co-morbid conditions like chronic kidney disease and fatty liver which further accentuate the risk of hypertension. Increased awareness is required to prevent, diagnose and treat obesity related hypertension among the pediatric population.
Core tip: The obesity epidemic in children is beginning to show its ramifications of increase in chronic diseases in children such as hypertension. Early childhood factors like prematurity and accelerated post-natal weight gain play a role in hypertension in later years and shed light on the multi-factorial prevention strategies that need to be in place. Furthermore, surveillance of factors such as vitamin D deficiency, hyperuricemia, sleep apnea, chronic kidney disease and fatty liver is required in addition to the traditional approach of weight management and pharmacotherapy.
- Citation: Gunta SS, Mak RH. Hypertension in children with obesity. World J Hypertens 2014; 4(2): 15-24
- URL: https://www.wjgnet.com/2220-3168/full/v4/i2/15.htm
- DOI: https://dx.doi.org/10.5494/wjh.v4.i2.15
The prevalence of obesity in children [body mass index (BMI) ≥ 95th percentile] has increased from 13.9% in 1999 to about 17% in 2004 and has remained stable at this rate until 2010 in the United States per National Health and Nutrition Examination Survey (NHANES) data[1,2]. In the two decades prior to that the prevalence of obesity in children more than doubled[2]. The prevalence of hypertension in children is also increasing over the past few decades, in part due to the increasing prevalence of obesity[3].
Analysis of data from NHANES surveys between 1999 and 2008 showed that 14% of adolescents aged 12-19 years had prehypertension or hypertension[4]. In a school based screening program in the United States, the prevalence of hypertension increased progressively as the BMI percentile increased from ≤ 5th percentile (2%) to ≥ 95th percentile (11%)[3]. Among 761 school children in Oklahoma, United States almost 28% were obese and 18% had blood pressure (BP) > 90th percentile on the first screening and 2.8% had persistently elevated BP after three screenings. BMI ≥ 85th percentile was significantly associated with hypertension compared to non-obese children[5]. This trend is also seen in other parts of the world. The prevalence of hypertension was almost 25% and pre-hypertension 34.7% among obese children at one endocrinology referral center in India[6]. A pediatric primary care setting in Italy noted about 35% of a sample of 1310 children to be overweight or obese. The prevalence of prehypertension and hypertension was 7.1% in normal weight, 21.9% in overweight and 42.3% in obese[7]. Among Chinese adolescents, higher prevalence of hypertension was associated with higher BMI percentiles. Non-obese adolescents had less than 5% prevalence of hypertension whereas among those with BMI > 95th percentile, approximately 20% boys and 12% girls had hypertension[8].
Data from two randomized, double-blind, multicenter valsartan trials that recruited children with hypertension, performed at several centers across 9 countries showed that 17% of children age < 6 years, 62% of school-aged children and 60% of adolescents had primary hypertension. BMI was significantly higher in those with primary hypertension compared with those with secondary hypertension. Also noted was a significant age-related increase in BMI in both the primary and secondary hypertension subgroups. Approximately 50% of children 6 to < 17 years in these trials were classified as obese[9]. More than 2 decades ago published reports indicated about 16% of referred pediatric hypertensive cases as primary hypertension and about 45% of the cases as obesity related hypertension in primary care centers[10]. This is in stark contrast to a recent study from four centers of the Midwest Pediatric Nephrology Consortium in the United States, where about 91% of the children were diagnosed with primary hypertension and among these 89% of children had a BMI > 85th percentile[11]. Characteristics of children with primary hypertension may be changing due to obesity epidemic. Among children with primary hypertension at a referral clinic, more than 50% were obese[12]. Other characteristics included higher prevalence of isolated systolic hypertension[12], positive family history of hypertension[12], increased incidence of left ventricular hypertrophy[12,13] and decreased nocturnal dipping[13].
Data from 2001-2008 from several studies in Germany, Switzerland and Austria that included more than 260000 children with overweight or obesity was examined[14]. The most prevalent cardiovascular risk factor in this patient population was hypertension in more than 35% of the cohort. Hypertension mainly correlated with the degree of overweight and these children were also at higher risk of left ventricular hypertrophy and arterial stiffness measured by flow mediated dilatation.
Data analysis from four large prospective cohorts of cardiovascular risk factors-the Bogalusa Heart Study (n = 635), the Muscatine Study (n = 722), the Childhood Determinants of Adult Health Study (n = 2331), and the cardiovascular risk in Young Finns Study (n = 2640) showed the highest cardiovascular risk factors among those who were overweight or obese as children and continued to be obese as adults[15]. The risks (type 2 diabetes, hyperlipidemia, carotid intima media thickness) among overweight and obese children who became non-obese as adults were similar to those among persons who were never obese which may suggest nullifying the effect of childhood obesity by maintaining a normal adult BMI. Only the association between childhood obesity and risk of hypertension remained significant after accounting for adult obesity. Obese adults who were overweight or obese as children had an even higher risk of hypertension than did obese adults who had normal weight as children. This may suggest that childhood adiposity has a lasting effect on risk of hypertension, even after normalization of BMI.
Low birth weight is associated with a higher BMI in childhood. Children with a low birth weight were observed to have more abdominal fat and a higher percentage of total fat than those with higher birth weight[16]. The Atherosclerosis Risk in Young Adults-study[17] showed that birth weight was inversely associated with systolic BP and serum triglycerides and positively associated with waist circumference. This inverse association of birth weight and obesity, hypertension has been previously shown in the Nurses’ Health Study (in women)[18] and the Health Professionals Follow-up study (in men)[19]. Decreased number of nephrons in the low birth weight or premature infant has been proposed to be responsible for compensatory hypertrophy and intraglomerular hypertension in the remaining nephrons subsequently leading to glomerular sclerosis and hypertension[20,21]. It may be due to this reason that some studies show an association of low birth weight with hypertension irrespective of current BMI[22]. Children born with low birth weight or small for gestational age demonstrate blunted circadian rhythms on 24 h ambulatory BP and heart rhythmicity monitoring. This may indicate abnormalities of cardiovascular regulation[23]. The blunted circadian rhythm is seen as early as within first 72 h after birth indicating cardiac vulnerability[24]. Among children born small for gestational age, BMI was positively associated with mean BP, nocturnal dipping, and the circadian amplitude of BP[23]. Obese adolescents have decreased nocturnal dipping compared to their lean counterparts[25] and may indicate similar cardiac dysregulation. Whether low birth weight by itself is a risk factor or if these individuals are at higher risk due to its frequent association with accelerated post natal weight gain remains to be seen.
There is ongoing debate that low birth weight per se might not be a risk factor for adult hypertension but it is the accelerated post natal growth[26]. Intrauterine growth retardation may cause decreased nephron number causing impaired kidney development. When coupled with an excessive infant “catch-up” growth after birth, it results in a mismatch between body size and nephron number. This predisposes to nephron hyperfiltration and hypertension in adulthood[27]. Cluster analysis on a longitudinal Australian birth cohort showed a U-shaped relationship between birth weight and components of metabolic syndrome like obesity and hypertension. The risk was elevated with both low and high birth weights but post-natal weight gain was the dominant factor associated with the high-risk cluster[28].
Rapid weight gain from birth to 2-3 years of age is associated with overweight, high BP and adverse metabolic outcomes in several studies[29,30]. A study from United Kingdom[31], predicted an increased metabolic risk including elevated BP at the age of 17 years based on rapid weight gain during 0-6 mo of infancy. Adjustment for birth weight and BMI at the age 17 years did not alter this significant association. A study of cohort of European American subjects identified weight gain in first week of life to be a critical determinant for the development of obesity several decades later[32]. Prevention of early catch-up growth in a mouse model of low birth weight reversed the development of glucose intolerance and obesity suggesting that accelerated post natal weight gain and not low birth weight may be a risk factor for obesity later in life[33].
A recent systematic review and meta-analysis that included 33 studies (included case-control, cross sectional and cohort studies) showed high birth weight (> 4000 g) to be associated with increased risk of obesity compared with subjects with birth weight < 4000 g[34]. There was no significant association between low birth weight (< 2500 g) and obesity. The authors found that low birth weight was not associated with the risk of obesity in cohort studies, studies with large sample sizes and/or high quality grades. Though case-control and cross sectional studies were largely from China and the cohort studies were from the western world, no evidence of publication bias was found[34]. Several other studies show evidence of correlation between high birth weight and obesity[35-37]. High birth weight, catch up growth and increased weight gain in first year of life were risk factors for obesity at the age of 7 years in a United Kingdom cohort[36].
Another systematic review and meta-analysis showed that high birth weight (> 4000 g) was associated with increased risk of hypertension and higher BP during childhood. However, as these children grew into adults they were less susceptible to hypertension than those with normal birth weight[38]. High birth weight is also associated with other cardiovascular risk factors like increased carotid intima media thickness[39].
Activation of the sympathetic nervous system (SNS) plays a significant role in the pathogenesis of obesity induced hypertension and is thought to be the principal mechanism involved. Even in the absence of hypertension, obesity is characterized by increased sympathetic activity[40]. Studies have shown that BP in obese individuals is more effectively reduced by adrenergic blockade as compared to lean individuals[41] suggesting SNS plays a key role in obesity induced hypertension. Obesity has differential SNS activity in various tissues and is most prominent in the kidney and muscles, whereas the heart has normal to decreased sympathetic activity and depressed parasympathetic activity[42]. The autonomic nervous system balance was found to be impaired in a group of obese children from Turkey in favor of increased SNS activity[43]. In a Study from Japan, obese children were found to have global autonomic depression[44]. Abdominal obesity and visceral adiposity elicits greater SNS activation as compared to individuals with increased subcutaneous fat[45] and weight loss is shown to decrease SNS over activity in obesity[46]. More specifically, the renal sympathetic nerve mediates a significant part of the effects of SNS activation in obesity. Denervation of the kidneys attenuates sodium absorption and decreases BP in experimental animal models[42,47].
Even in the absence of glomerular sclerosis and chronic kidney disease (CKD) in obesity, the increased SNS activity leads to decreased renal blood flow, stimulating renin release and activation of the renin-angiotensin-system (RAS). Visceral obesity also causes fat deposition around and into the renal medulla stimulating renin secretion[48]. Adipose tissue expresses components of RAS. Adipocytes possess functionally active aldosterone synthase that generates aldosterone, which is increased in animal models of obesity[49]. There is also evidence of functioning RAS in adipocytes of humans[50]. Adipose tissue derived angiotensinogen was substantially increased in obese individuals and correlated with systolic BP in a study from Japan[51]. The contribution of adipose tissue renin to circulating renin levels is not well understood. An increase in circulating Angiotensin II may cause a negative feedback loop leading to a decrease in plasma renin activity[52]. This may explain the inverse relationship of plasma renin activity and BP in an obese adolescent cohort in United States. Though, a positive and significant correlation was seen between the plasma renin activity and severity of obesity[53].
Obese individuals have high levels of circulating insulin, considered to be secondary to peripheral insulin resistance. It continues to be debated if hypertension is caused by hyperinsulinemia, insulin resistance or its vascular effects[48]. Insulin directly acts on the renal tubule causing sodium retention[54]. It also has sympatho-excitatory effects and causes increased levels of norepinephrine. Though insulin has vasodilatory effects, its action is impaired in the presence of severe insulin resistance[55].
Leptin is an anorexigenic hormone produced in the adipose tissue and is known to stimulate the SNS[56]. Leptin deficient mice (ob/ob) have a phenotype of severe obesity but do not exhibit hypertension[57]. Leptin may contribute to the pathophysiology of hypertension in obesity through SNS stimulating actions in the kidneys, adrenal glands, brown adipose tissue[48] and endothelial dysfunction via alteration in the expression of NO synthase[58]. Leptin acts via both central mechanism[59] and peripheral mechanism[60] causing hypertension and stimulating renal sodium tubular reabsorption. Obese individuals, including obese children, have high circulating levels of leptin, but they seem to have a resistance to its metabolic actions such as decreased food intake and increased basal metabolic rate. Although, leptin’s role in stimulating the SNS and selective leptin mediated activation of the renal nerve seems to be unaltered in obesity[48,61]. A recently published multi-ethnic study for atherosclerosis[62] confirmed the previously shown association of higher serum leptin level with higher odds of hypertension irrespective of BMI[63].
Obesity in children is associated with low adiponectin levels[64,65] and low levels are known to be predictive of adverse cardiovascular events in adults[66,67]. Low adiponectin level was an independent predictor of cardiovascular risk in a cohort of obese elementary school children in Japan[68]. Serum adiponectin levels were found to be lower in obese and hypertensive children as compared to normal weight and normotensive children with the lowest levels seen in those with both obesity and hypertension[69].
Obesity induced hypertension may have similarities with the phenotype of Cushing’s syndrome resulting from cortisol excess[48]. It is proposed that obese individuals may have increased intra-adipose glucocorticoid action, even in the presence of normal plasma glucocorticoid levels[70].
Recent literature shows an association between vitamin D deficiency (< 50 nmol/L) and cardio-metabolic risk factors that includes insulin resistance, hypertension, and hyperlipidemia, and especially obesity. The evidence on causality is conflicting though[71]. This association is also seen in adolescents[72]. Vitamin D deficiency is significantly higher in obese children (34%-56%) vs healthy control children (16%-21%)[73,74]. There is a dose response relationship between vitamin D levels and hypertension with lower levels of vitamin D associated with higher BP[75].
Vitamin D acts a negative endocrine regulator of RAS by directly suppressing plasma renin expression and also renin gene activity[76]. Vitamin D receptor-knockout mice show increases in plasma expression of renin and angiotensin II with resulting hypertension[77,78].
Vitamin D inhibits the proliferation and migration of vascular smooth muscle cells under endothelial stress[79] and down regulates thrombogenic protein expression[80]. Endothelial dysfunction, a known contributor to hypertension, is seen in vitamin D deficient individuals not just in chronic conditions like renal insufficiency[81] and diabetes[82] but also in healthy, asymptomatic individuals[83].
Obesity is considered a pro-inflammatory state due to insulin resistance, vitamin D deficiency, elevated levels of leptin and decreased adiponectin. Adipose tissue also secretes other pro-inflammatory factors like interleukin-6 and tumor necrosis factor α[84]. Insulin resistance leads to the down regulation of nitric oxide production and up regulation of vasoconstrictor endothelin-1 levels[85]. This imbalance along with other pro-inflammatory cytokines and reactive oxygen species from the adipose tissue lead to endothelial dysfunction[86]. Unfavorable lipid profile in severely obese children also contributes to endothelial dysfunction[87].
Obese children and adolescents have greater carotid artery intima media thickness as compared to the non-obese. These associations are not always dependent of BP[88-90]. Increased carotid artery intima media thickness is a known marker of hypertension and cardiovascular morbidity in adults and may suggest the early preceding changes in obese children.
There is increasing evidence for diastolic hypertension, increased mean BP, non-dipping status of BP and increased BP variability in children with obstructive sleep apnea syndrome[91-93]. Furthermore, the children with obesity and obstructive sleep apnea have even higher prevalence of hypertension[93,94]. Hypertension may persist even after the improvement of apnea-hypopnea index after adeno-tonsillectomy in these patients and hence may require long term BP monitoring[95].
Insulin and leptin have direct actions on the renal tubule causing sodium retention[56,62]. BP in obese adolescents is shown to be sensitive to salt intake. After significant weight loss, this sensitivity of BP to sodium decreases[96]. Salt consumption has a positive association with BMI even when adjusted for consumption of other high calorie foods, seen in both adults[97] and adolescents[98]. Pressure natriuresis is reset to a hypertensive level in obese subjects resulting in volume overload[58]. Decreasing sodium intake has been shown to decrease BP in adults and has a comparatively decreased but significant effect in children too[99]. This decrease in BP is more prominent among the obese children[100].
Hyperuricemia is associated with metabolic syndrome[101,102]. The cause-effect relationship is yet to be established. Evidence points to hyperinsulinemia leading to increased absorption of uric acid in the kidney[103] and also suggests that hyperuricemia increases the risk of developing metabolic syndrome after adjusting for other known risk factors[104,105]. Fructose is implicated in the pathway of hyperuricemia leading to components of metabolic syndrome in adults and adolescents[105,106]. It has an effect on decreased nitric oxide production and endothelial dysfunction[107,108].
Hyperuricemia may also be involved in RAS stimulation leading to hypertension[109]. This, alongside with endothelial dysfunction, may increase cardiovascular disease risk of hyperuricemic individuals[108,110,111]. Hyperuricemia is associated with hypertension not only in adults but also in children and adolescents. Elevated serum uric acid was found in 89% of subjects with primary hypertension, and only in 30% with secondary hypertension and in none of the controls in a tertiary care nephrology program in Texas, United States[112]. Interestingly, the link between obesity and hyperuricemia was not consistent in this cohort[112]. The same group also showed the effect of uric acid lowering agent like Allopurinol to have significant reduction in BP in those with pre-hypertension[113] and stage I essential hypertension[114].
Obesity is shown to be a strong and independent risk factor for CKD in several epidemiological studies. There has been a parallel increase in the prevalence of obesity and CKD[115]. Obese individuals have glomerular hyperperfusion and hyperfiltration[116]. It may eventually lead to obesity related glomerulopathy that initially manifests as glomerulomegaly and in later stages has several features of focal segmental glomerulosclerosis. Clinically it presents as varying degrees of proteinuria and renal insufficiency[117]. Albuminuria is associated with impaired glucose tolerance in overweight/obese teenagers[118] and adults[119].
In obesity, due to glomerular hyperperfusion and presence of renal visceral fat deposition, there is activation of the RAS[120] and plasma renin activity positively correlates with BMI[55]. The unfavorable lipid profile seen in obese children also contributes to the rate of progression of renal disease. Nephron loss in CKD then leads to further elevation of BP[120]. Even pre-hypertension is shown to be associated with decreased renal function and increased proteinuria in children[120]. It is a two-way street with hypertension being a major “cause” and “effect” of renal dysfunction in obese individuals.
The prevalence of nonalcoholic fatty liver disease (NAFLD) parallels that of obesity in children[121] and has been shown to predict the risk of hypertension[122] and CKD[123], the latter is also significant risk factor for hypertension. There is growing consensus that NAFLD should be considered as a criterion for metabolic syndrome[124-126] due to interplay of the pathophysiology with insulin resistance. A recently published cohort study showed increased risk of hypertension with the development of fatty liver disease[127]. Furthermore, resolution of fatty liver disease in this cohort did not decrease their risk for hypertension[127] suggesting the importance of prevention strategies. Genetic factors influence risk of fatty liver disease in hypertensive mice[128] and further research is required to assess similar risks in humans. Interventions to prevent obesity will also be helpful in decreasing the incidence of NAFLD in children thereby further decreasing the risk for hypertension.
Lifestyle interventions are recommended for all children diagnosed with obesity related hypertension. This includes increased physical activity and healthy dietary choices for weight loss and/or decreased rate of weight gain and low sodium diet[129]. The effect of high sodium intake has a more pronounced effect of elevated systolic BP among overweight and obese adolescents as compared to the general population. Correspondingly, decreasing sodium intake may have a greater effect on BP among the obese[100].
Pharmacological and surgical options for treatment of obesity are limited in children[129]. Angiotensin converting enzyme (ACE) inhibitors and calcium channel blockers are the most frequently prescribed drugs for primary hypertension in children and adolescents[130,131]. ACE inhibitors are the drug of choice for treating obesity related hypertension in adults considering that SNS and RAS activation are the most important mechanisms leading to elevated BP in obesity[50]. ACE inhibitors and angiotensin receptor blockers also have additional reno-protective effects and become the ideal drug of choice in co-morbid conditions[132]. Beta blockers are not preferred in children due to their adverse metabolic profile, especially in obesity related hypertension due to impaired glycemic control and potential for increase in triglyceride levels and weight gain[132,133].
Hypertension due to obesity in children is increasing. Understanding the complex interaction of various mechanisms involved, as illustrated in Figure 1, will help design better prevention and treatment strategies. Efforts at prevention should start right from birth or in the pre-natal period due to the possible developmental origin of obesity related hypertension. Addressing co-morbid conditions is also important. Obesity related hypertension is well-recognized in the adult population and increased awareness is required in pediatrics for early diagnosis and implementing prevention and treatment options.
P- Reviewers: Morimoto S, Sato A, Tarantino G S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
| 1. | Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006;295:1549-1555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6297] [Cited by in RCA: 5885] [Article Influence: 309.7] [Reference Citation Analysis (0)] |
| 2. | Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA. 2012;307:483-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2774] [Cited by in RCA: 2669] [Article Influence: 205.3] [Reference Citation Analysis (0)] |
| 3. | Sorof JM, Lai D, Turner J, Poffenbarger T, Portman RJ. Overweight, ethnicity, and the prevalence of hypertension in school-aged children. Pediatrics. 2004;113:475-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 669] [Cited by in RCA: 624] [Article Influence: 29.7] [Reference Citation Analysis (0)] |
| 4. | May AL, Kuklina EV, Yoon PW. Prevalence of cardiovascular disease risk factors among US adolescents, 1999-2008. Pediatrics. 2012;129:1035-1041. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 305] [Cited by in RCA: 283] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 5. | Moore WE, Stephens A, Wilson T, Wilson W, Eichner JE. Body mass index and blood pressure screening in a rural public school system: the Healthy Kids Project. Prev Chronic Dis. 2006;3:A114. [PubMed] |
| 6. | Phatale P, Phatale H. Prevalence of pre-diabetes, diabetes, pre-hypertension, and hypertension in children weighing more than normal. Indian J Endocrinol Metab. 2012;16:S483-S485. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Giussani M, Antolini L, Brambilla P, Pagani M, Zuccotti G, Valsecchi MG, Lucini D, Genovesi S. Cardiovascular risk assessment in children: role of physical activity, family history and parental smoking on BMI and blood pressure. J Hypertens. 2013;31:983-992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 37] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 8. | Cao ZQ, Zhu L, Zhang T, Wu L, Wang Y. Blood pressure and obesity among adolescents: a school-based population study in China. Am J Hypertens. 2012;25:576-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 9. | Flynn J, Zhang Y, Solar-Yohay S, Shi V. Clinical and demographic characteristics of children with hypertension. Hypertension. 2012;60:1047-1054. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 73] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 10. | Feld LG, Springate JE. Hypertension in children. Curr Probl Pediatr Jun. 1988;18:317-373. [RCA] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Kapur G, Ahmed M, Pan C, Mitsnefes M, Chiang M, Mattoo TK. Secondary hypertension in overweight and stage 1 hypertensive children: a Midwest Pediatric Nephrology Consortium report. J Clin Hypertens (Greenwich). 2010;12:34-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Flynn JT, Alderman MH. Characteristics of children with primary hypertension seen at a referral center. Pediatr Nephrol. 2005;20:961-966. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 101] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 13. | Sorof JM, Cardwell G, Franco K, Portman RJ. Ambulatory blood pressure and left ventricular mass index in hypertensive children. Hypertension. 2002;39:903-908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 205] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 14. | l’Allemand-Jander D. Clinical diagnosis of metabolic and cardiovascular risks in overweight children: early development of chronic diseases in the obese child. Int J Obes (Lond). 2010;34 Suppl 2:S32-S36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 99] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 15. | Juonala M, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, Srinivasan SR, Daniels SR, Davis PH, Chen W. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med. 2011;365:1876-1885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1066] [Cited by in RCA: 1142] [Article Influence: 81.6] [Reference Citation Analysis (0)] |
| 16. | Garnett SP, Cowell CT, Baur LA, Fay RA, Lee J, Coakley J, Peat JK, Boulton TJ. Abdominal fat and birth size in healthy prepubertal children. Int J Obes Relat Metab Disord. 2001;25:1667-1673. [RCA] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 84] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 17. | Ramadhani MK, Grobbee DE, Bots ML, Castro Cabezas M, Vos LE, Oren A, Uiterwaal CS. Lower birth weight predicts metabolic syndrome in young adults: the Atherosclerosis Risk in Young Adults (ARYA)-study. Atherosclerosis. 2006;184:21-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 79] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 18. | Curhan GC, Chertow GM, Willett WC, Spiegelman D, Colditz GA, Manson JE, Speizer FE, Stampfer MJ. Birth weight and adult hypertension and obesity in women. Circulation. 1996;94:1310-1315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 480] [Cited by in RCA: 434] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 19. | Curhan GC, Willett WC, Rimm EB, Spiegelman D, Ascherio AL, Stampfer MJ. Birth weight and adult hypertension, diabetes mellitus, and obesity in US men. Circulation. 1996;94:3246-3250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 657] [Cited by in RCA: 607] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 20. | Hoy WE, Bertram JF, Denton RD, Zimanyi M, Samuel T, Hughson MD. Nephron number, glomerular volume, renal disease and hypertension. Curr Opin Nephrol Hypertens. 2008;17:258-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 151] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 21. | Samuel T, Hoy WE, Douglas-Denton R, Hughson MD, Bertram JF. Determinants of glomerular volume in different cortical zones of the human kidney. J Am Soc Nephrol. 2005;16:3102-3109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 86] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 22. | Gamborg M, Byberg L, Rasmussen F, Andersen PK, Baker JL, Bengtsson C, Canoy D, Drøyvold W, Eriksson JG, Forsén T, Gunnarsdottir I, Järvelin MR, Koupil I, Lapidus L, Nilsen TI, Olsen SF, Schack-Nielsen L, Thorsdottir I, Tuomainen TP, Sorensen TI, NordNet Study Group. Birth weight and systolic blood pressure in adolescence and adulthood: meta-regression analysis of sex- and age-specific results from 20 Nordic studies. Am J Epidemiol. 2007;166:634-645. [RCA] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 126] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 23. | Wolfenstetter A, Simonetti GD, Pöschl J, Schaefer F, Wühl E. Altered cardiovascular rhythmicity in children born small for gestational age. Hypertension. 2012;60:865-870. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 24. | Begum EA, Bonno M, Sasaki N, Omori Y, Matsuda K, Sugino N, Tanaka S, Yamamoto H, Ido M. Blunted heart rate circadian rhythms in small for gestational age infants during the early neonatal period. Am J Perinatol. 2012;29:369-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 25. | Framme J, Dangardt F, Mårild S, Osika W, Währborg P, Friberg P. 24-h Systolic blood pressure and heart rate recordings in lean and obese adolescents. Clin Physiol Funct Imaging. 2006;26:235-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 26. | Eriksson J, Forsén T, Tuomilehto J, Osmond C, Barker D. Fetal and childhood growth and hypertension in adult life. Hypertension. 2000;36:790-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 331] [Cited by in RCA: 297] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 27. | Bagby SP. Obesity-initiated metabolic syndrome and the kidney: a recipe for chronic kidney disease? J Am Soc Nephrol. 2004;15:2775-2791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 170] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 28. | Huang RC, Burke V, Newnham JP, Stanley FJ, Kendall GE, Landau LI, Oddy WH, Blake KV, Palmer LJ, Beilin LJ. Perinatal and childhood origins of cardiovascular disease. Int J Obes (Lond). 2007;31:236-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 104] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 29. | Fujita Y, Kouda K, Nakamura H, Iki M. Association of rapid weight gain during early childhood with cardiovascular risk factors in Japanese adolescents. J Epidemiol. 2013;23:103-108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 30. | Thiering E, Brüske I, Kratzsch J, Hoffmann B, Herbarth O, von Berg A, Schaaf B, Wichmann HE, Heinrich J. Peak growth velocity in infancy is positively associated with blood pressure in school-aged children. J Hypertens. 2012;30:1114-1121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 31. | Ekelund U, Ong KK, Linné Y, Neovius M, Brage S, Dunger DB, Wareham NJ, Rössner S. Association of weight gain in infancy and early childhood with metabolic risk in young adults. J Clin Endocrinol Metab. 2007;92:98-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 250] [Cited by in RCA: 241] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 32. | Stettler N, Stallings VA, Troxel AB, Zhao J, Schinnar R, Nelson SE, Ziegler EE, Strom BL. Weight gain in the first week of life and overweight in adulthood: a cohort study of European American subjects fed infant formula. Circulation. 2005;111:1897-1903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 281] [Cited by in RCA: 269] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 33. | Jimenez-Chillaron JC, Hernandez-Valencia M, Lightner A, Faucette RR, Reamer C, Przybyla R, Ruest S, Barry K, Otis JP, Patti ME. Reductions in caloric intake and early postnatal growth prevent glucose intolerance and obesity associated with low birthweight. Diabetologia. 2006;49:1974-1984. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 107] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 34. | Yu ZB, Han SP, Zhu GZ, Zhu C, Wang XJ, Cao XG, Guo XR. Birth weight and subsequent risk of obesity: a systematic review and meta-analysis. Obes Rev. 2011;12:525-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 414] [Cited by in RCA: 374] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 35. | Lausten-Thomsen U, Bille DS, Nässlund I, Folskov L, Larsen T, Holm JC. Neonatal anthropometrics and correlation to childhood obesity--data from the Danish Children’s Obesity Clinic. Eur J Pediatr. 2013;172:747-751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 36. | Reilly JJ, Armstrong J, Dorosty AR, Emmett PM, Ness A, Rogers I, Steer C, Sherriff A. Early life risk factors for obesity in childhood: cohort study. BMJ. 2005;330:1357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1054] [Cited by in RCA: 1063] [Article Influence: 53.2] [Reference Citation Analysis (0)] |
| 37. | Phillips DI, Young JB. Birth weight, climate at birth and the risk of obesity in adult life. Int J Obes Relat Metab Disord. 2000;24:281-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 79] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 38. | Zhang Y, Li H, Liu SJ, Fu GJ, Zhao Y, Xie YJ, Zhang Y, Wang YX. The associations of high birth weight with blood pressure and hypertension in later life: a systematic review and meta-analysis. Hypertens Res. 2013;36:725-735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 71] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 39. | Dratva J, Breton CV, Hodis HN, Mack WJ, Salam MT, Zemp E, Gilliland F, Kuenzli N, Avol E. Birth weight and carotid artery intima-media thickness. J Pediatr. 2013;162:906-911.e1-e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 40. | Grassi G, Seravalle G, Cattaneo BM, Bolla GB, Lanfranchi A, Colombo M, Giannattasio C, Brunani A, Cavagnini F, Mancia G. Sympathetic activation in obese normotensive subjects. Hypertension. 1995;25:560-563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 389] [Cited by in RCA: 392] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 41. | Wofford MR, Anderson DC, Brown CA, Jones DW, Miller ME, Hall JE. Antihypertensive effect of alpha- and beta-adrenergic blockade in obese and lean hypertensive subjects. Am J Hypertens. 2001;14:694-698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 130] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 42. | Hall JE, da Silva AA, do Carmo JM, Dubinion J, Hamza S, Munusamy S, Smith G, Stec DE. Obesity-induced hypertension: role of sympathetic nervous system, leptin, and melanocortins. J Biol Chem. 2010;285:17271-17276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 363] [Cited by in RCA: 351] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 43. | Altuncu ME, Baspinar O, Keskin M. The use of short-term analysis of heart rate variability to assess autonomic function in obese children and its relationship with metabolic syndrome. Cardiol J. 2012;19:501-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 44. | Nagai N, Matsumoto T, Kita H, Moritani T. Autonomic nervous system activity and the state and development of obesity in Japanese school children. Obes Res. 2003;11:25-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 76] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 45. | Alvarez GE, Beske SD, Ballard TP, Davy KP. Sympathetic neural activation in visceral obesity. Circulation. 2002;106:2533-2536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 405] [Cited by in RCA: 416] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 46. | Jung RT, Shetty PS, Barrand M, Callingham BA, James WP. Role of catecholamines in hypotensive response to dieting. Br Med J. 1979;1:12-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 125] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 47. | Hall JE. The kidney, hypertension, and obesity. Hypertension. 2003;41:625-633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 567] [Cited by in RCA: 548] [Article Influence: 24.9] [Reference Citation Analysis (0)] |
| 48. | Kotsis V, Stabouli S, Papakatsika S, Rizos Z, Parati G. Mechanisms of obesity-induced hypertension. Hypertens Res. 2010;33:386-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 350] [Cited by in RCA: 381] [Article Influence: 25.4] [Reference Citation Analysis (0)] |
| 49. | Segal-Lieberman G, Rosenthal T. Animal models in obesity and hypertension. Curr Hypertens Rep. 2013;15:190-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 50. | Thatcher S, Yiannikouris F, Gupte M, Cassis L. The adipose renin-angiotensin system: role in cardiovascular disease. Mol Cell Endocrinol. 2009;302:111-117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 86] [Cited by in RCA: 86] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 51. | Yasue S, Masuzaki H, Okada S, Ishii T, Kozuka C, Tanaka T, Fujikura J, Ebihara K, Hosoda K, Katsurada A. Adipose tissue-specific regulation of angiotensinogen in obese humans and mice: impact of nutritional status and adipocyte hypertrophy. Am J Hypertens. 2010;23:425-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 87] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 52. | Schunkert H, Ingelfinger JR, Jacob H, Jackson B, Bouyounes B, Dzau VJ. Reciprocal feedback regulation of kidney angiotensinogen and renin mRNA expressions by angiotensin II. Am J Physiol. 1992;263:E863-E869. [PubMed] |
| 53. | Shatat IF, Flynn JT. Relationships between renin, aldosterone, and 24-hour ambulatory blood pressure in obese adolescents. Pediatr Res. 2011;69:336-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 54. | DeFronzo RA, Cooke CR, Andres R, Faloona GR, Davis PJ. The effect of insulin on renal handling of sodium, potassium, calcium, and phosphate in man. J Clin Invest. 1975;55:845-855. [PubMed] |
| 55. | Gudbjörnsdottir S, Elam M, Sellgren J, Anderson EA. Insulin increases forearm vascular resistance in obese, insulin-resistant hypertensives. J Hypertens. 1996;14:91-97. [PubMed] |
| 56. | Hall JE, Brands MW, Hildebrandt DA, Kuo J, Fitzgerald S. Role of sympathetic nervous system and neuropeptides in obesity hypertension. Braz J Med Biol Res. 2000;33:605-618. [PubMed] |
| 57. | Mark AL, Shaffer RA, Correia ML, Morgan DA, Sigmund CD, Haynes WG. Contrasting blood pressure effects of obesity in leptin-deficient ob/ob mice and agouti yellow obese mice. J Hypertens. 1999;17:1949-1953. [PubMed] |
| 58. | Korda M, Kubant R, Patton S, Malinski T. Leptin-induced endothelial dysfunction in obesity. Am J Physiol Heart Circ Physiol. 2008;295:H1514-H1521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 59. | Matsumura K, Abe I, Tsuchihashi T, Fujishima M. Central effects of leptin on cardiovascular and neurohormonal responses in conscious rabbits. Am J Physiol Regul Integr Comp Physiol. 2000;278:R1314-R1320. [PubMed] |
| 60. | Beltowski J, Wójcicka G, Marciniak A, Jamroz A. Oxidative stress, nitric oxide production, and renal sodium handling in leptin-induced hypertension. Life Sci. 2004;74:2987-3000. [PubMed] |
| 61. | Belin de Chantemèle EJ, Mintz JD, Rainey WE, Stepp DW. Impact of leptin-mediated sympatho-activation on cardiovascular function in obese mice. Hypertension. 2011;58:271-279. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 81] [Cited by in RCA: 81] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 62. | Allison MA, Ix JH, Morgan C, McClelland RL, Rifkin D, Shimbo D, Criqui MH. Higher leptin is associated with hypertension: the Multi-Ethnic Study of Atherosclerosis. J Hum Hypertens. 2013;27:617-622. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 63. | Agata J, Masuda A, Takada M, Higashiura K, Murakami H, Miyazaki Y, Shimamoto K. High plasma immunoreactive leptin level in essential hypertension. Am J Hypertens. 1997;10:1171-1174. [PubMed] |
| 64. | Asayama K, Hayashibe H, Dobashi K, Uchida N, Nakane T, Kodera K, Shirahata A, Taniyama M. Decrease in serum adiponectin level due to obesity and visceral fat accumulation in children. Obes Res. 2003;11:1072-1079. [PubMed] |
| 65. | Lee S, Bacha F, Gungor N, Arslanian SA. Racial differences in adiponectin in youth. Relationship to visceral fat and insulin sensitivity. Diabetes Care. 2006;29:51-56. [PubMed] |
| 66. | Kumada M, Kihara S, Sumitsuji S, Kawamoto T, Matsumoto S, Ouchi N, Arita Y, Okamoto Y, Shimomura I, Hiraoka H. Association of hypoadiponectinemia with coronary artery disease in men. Arterioscler Thromb Vasc Biol. 2003;23:85-89. [PubMed] |
| 67. | Hashimoto N, Kanda J, Nakamura T, Horie A, Kurosawa H, Hashimoto T, Sato K, Kushida S, Suzuki M, Yano S. Association of hypoadiponectinemia in men with early onset of coronary heart disease and multiple coronary artery stenoses. Metabolism. 2006;55:1653-1657. [PubMed] |
| 68. | Yoshinaga M, Sameshima K, Tanaka Y, Wada A, Hashiguchi J, Tahara H, Kono Y. Adipokines and the prediction of the accumulation of cardiovascular risk factors or the presence of metabolic syndrome in elementary school children. Circ J. 2008;72:1874-1878. [PubMed] |
| 69. | Brambilla P, Antolini L, Street ME, Giussani M, Galbiati S, Valsecchi MG, Stella A, Zuccotti GV, Bernasconi S, Genovesi S. Adiponectin and hypertension in normal-weight and obese children. Am J Hypertens. 2013;26:257-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 70. | Flier JS. Obesity wars: molecular progress confronts an expanding epidemic. Cell. 2004;116:337-350. [PubMed] |
| 71. | Salo A, Logomarsino JV. Relationship of vitamin D status and cardiometabolic risk factors in children and adolescents. Pediatr Endocrinol Rev. 2011;9:456-762. [PubMed] |
| 72. | Pacifico L, Anania C, Osborn JF, Ferraro F, Bonci E, Olivero E, Chiesa C. Low 25(OH)D3 levels are associated with total adiposity, metabolic syndrome, and hypertension in Caucasian children and adolescents. Eur J Endocrinol. 2011;165:603-611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 144] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 73. | Reyman M, Verrijn Stuart AA, van Summeren M, Rakhshandehroo M, Nuboer R, de Boer FK, van den Ham HJ, Kalkhoven E, Prakken B, Schipper HS. Vitamin D deficiency in childhood obesity is associated with high levels of circulating inflammatory mediators, and low insulin sensitivity. Int J Obes (Lond). 2014;38:46-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 47] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 74. | Turer CB, Lin H, Flores G. Prevalence of vitamin D deficiency among overweight and obese US children. Pediatrics. 2013;131:e152-e161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 198] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 75. | Burgaz A, Orsini N, Larsson SC, Wolk A. Blood 25-hydroxyvitamin D concentration and hypertension: a meta-analysis. J Hypertens. 2011;29:636-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 161] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 76. | Gunta SS, Thadhani RI, Mak RH. The effect of vitamin D status on risk factors for cardiovascular disease. Nat Rev Nephrol. 2013;9:337-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 76] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 77. | Xiang W, Kong J, Chen S, Cao LP, Qiao G, Zheng W, Liu W, Li X, Gardner DG, Li YC. Cardiac hypertrophy in vitamin D receptor knockout mice: role of the systemic and cardiac renin-angiotensin systems. Am J Physiol Endocrinol Metab. 2005;288:E125-E132. [PubMed] |
| 78. | Zhou C, Lu F, Cao K, Xu D, Goltzman D, Miao D. Calcium-independent and 1,25(OH)2D3-dependent regulation of the renin-angiotensin system in 1alpha-hydroxylase knockout mice. Kidney Int. 2008;74:170-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 79. | Raymond MA, Désormeaux A, Labelle A, Soulez M, Soulez G, Langelier Y, Pshezhetsky AV, Hébert MJ. Endothelial stress induces the release of vitamin D-binding protein, a novel growth factor. Biochem Biophys Res Commun. 2005;338:1374-1382. [PubMed] |
| 80. | Aihara K, Azuma H, Akaike M, Ikeda Y, Yamashita M, Sudo T, Hayashi H, Yamada Y, Endoh F, Fujimura M. Disruption of nuclear vitamin D receptor gene causes enhanced thrombogenicity in mice. J Biol Chem. 2004;279:35798-35802. [PubMed] |
| 81. | Aihara K, Azuma H, Akaike M, Ikeda Y, Yamashita M, Sudo T, Hayashi H, Yamada Y, Endoh F, Fujimura M. Vitamin D deficiency and endothelial dysfunction in non-dialysis chronic kidney disease patients. Atherosclerosis. 2012;220:265-268. [RCA] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 72] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 82. | Yiu YF, Chan YH, Yiu KH, Siu CW, Li SW, Wong LY, Lee SW, Tam S, Wong EW, Cheung BM. Vitamin D deficiency is associated with depletion of circulating endothelial progenitor cells and endothelial dysfunction in patients with type 2 diabetes. J Clin Endocrinol Metab. 2011;96:E830-E835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 106] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 83. | Al Mheid I, Patel R, Murrow J, Morris A, Rahman A, Fike L, Kavtaradze N, Uphoff I, Hooper C, Tangpricha V. Vitamin D status is associated with arterial stiffness and vascular dysfunction in healthy humans. J Am Coll Cardiol. 2011;58:186-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 222] [Cited by in RCA: 270] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 84. | Wisse BE. The inflammatory syndrome: the role of adipose tissue cytokines in metabolic disorders linked to obesity. J Am Soc Nephrol. 2004;15:2792-2800. [PubMed] |
| 85. | Kim JA, Montagnani M, Koh KK, Quon MJ. Reciprocal relationships between insulin resistance and endothelial dysfunction: molecular and pathophysiological mechanisms. Circulation. 2006;113:1888-1904. [PubMed] |
| 86. | Kim F, Pham M, Maloney E, Rizzo NO, Morton GJ, Wisse BE, Kirk EA, Chait A, Schwartz MW. Vascular inflammation, insulin resistance, and reduced nitric oxide production precede the onset of peripheral insulin resistance. Arterioscler Thromb Vasc Biol. 2008;28:1982-1988. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 282] [Cited by in RCA: 287] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 87. | Tounian P, Aggoun Y, Dubern B, Varille V, Guy-Grand B, Sidi D, Girardet JP, Bonnet D. Presence of increased stiffness of the common carotid artery and endothelial dysfunction in severely obese children: a prospective study. Lancet. 2001;358:1400-1404. [PubMed] |
| 88. | Stabouli S, Kotsis V, Karagianni C, Zakopoulos N, Konstantopoulos A. Blood pressure and carotid artery intima-media thickness in children and adolescents: the role of obesity. Hellenic J Cardiol. 2012;53:41-47. [PubMed] |
| 89. | Leite A, Santos A, Monteiro M, Gomes L, Veloso M, Costa M. Impact of overweight and obesity in carotid intima-media thickness of portuguese adolescents. Acta Paediatr. 2012;101:e115-e121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 90. | Sarkola T, Abadilla AA, Chahal N, Jaeggi E, McCrindle BW. Feasibility of very-high resolution ultrasound to assess elastic and muscular arterial wall morphology in adolescents attending an outpatient clinic for obesity and lipid abnormalities. Atherosclerosis. 2011;219:610-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 91. | Marcus CL, Greene MG, Carroll JL. Blood pressure in children with obstructive sleep apnea. Am J Respir Crit Care Med. 1998;157:1098-1103. [PubMed] |
| 92. | Weber SA, Santos VJ, Semenzati Gde O, Martin LC. Ambulatory blood pressure monitoring in children with obstructive sleep apnea and primary snoring. Int J Pediatr Otorhinolaryngol. 2012;76:787-790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 47] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 93. | Xu Z, Li B, Shen K. Ambulatory blood pressure monitoring in Chinese children with obstructive sleep apnea/hypopnea syndrome. Pediatr Pulmonol. 2013;48:274-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 94. | Leung LC, Ng DK, Lau MW, Chan CH, Kwok KL, Chow PY, Cheung JM. Twenty-four-hour ambulatory BP in snoring children with obstructive sleep apnea syndrome. Chest. 2006;130:1009-1017. [PubMed] |
| 95. | Ng DK, Wong JC, Chan CH, Leung LC, Leung SY. Ambulatory blood pressure before and after adenotonsillectomy in children with obstructive sleep apnea. Sleep Med. 2010;11:721-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 63] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 96. | Rocchini AP, Key J, Bondie D, Chico R, Moorehead C, Katch V, Martin M. The effect of weight loss on the sensitivity of blood pressure to sodium in obese adolescents. N Engl J Med. 1989;321:580-585. [PubMed] |
| 97. | Hulthén L, Aurell M, Klingberg S, Hallenberg E, Lorentzon M, Ohlsson C. Salt intake in young Swedish men. Public Health Nutr. 2010;13:601-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 38] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 98. | Libuda L, Kersting M, Alexy U. Consumption of dietary salt measured by urinary sodium excretion and its association with body weight status in healthy children and adolescents. Public Health Nutr. 2012;15:433-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 82] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 99. | Alderman MH, Cohen H. Lower sodium intake reduces blood pressure in adults and children, but is not associated with a reduced risk of all CVD or all cause mortality. Evid Based Med. 2013;Epub ahead of print. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 100. | Yang Q, Zhang Z, Kuklina EV, Fang J, Ayala C, Hong Y, Loustalot F, Dai S, Gunn JP, Tian N. Sodium intake and blood pressure among US children and adolescents. Pediatrics. 2012;130:611-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 176] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 101. | Choi HK, Ford ES. Prevalence of the metabolic syndrome in individuals with hyperuricemia. Am J Med. 2007;120:442-447. [PubMed] |
| 102. | Sui X, Church TS, Meriwether RA, Lobelo F, Blair SN. Uric acid and the development of metabolic syndrome in women and men. Metabolism. 2008;57:845-852. [PubMed] |
| 103. | Muscelli E, Natali A, Bianchi S, Bigazzi R, Galvan AQ, Sironi AM, Frascerra S, Ciociaro D, Ferrannini E. Effect of insulin on renal sodium and uric acid handling in essential hypertension. Am J Hypertens. 1996;9:746-752. [PubMed] |
| 104. | Osgood K, Krakoff J, Thearle M. Serum uric acid predicts both current and future components of the metabolic syndrome. Metab Syndr Relat Disord. 2013;11:157-162. [PubMed] |
| 105. | Lin WT, Huang HL, Huang MC, Chan TF, Ciou SY, Lee CY, Chiu YW, Duh TH, Lin PL, Wang TN. Effects on uric acid, body mass index and blood pressure in adolescents of consuming beverages sweetened with high-fructose corn syrup. Int J Obes (Lond). 2013;37:532-539. [PubMed] |
| 106. | Nakagawa T, Hu H, Zharikov S, Tuttle KR, Short RA, Glushakova O, Ouyang X, Feig DI, Block ER, Herrera-Acosta J. A causal role for uric acid in fructose-induced metabolic syndrome. Am J Physiol Renal Physiol. 2006;290:F625-F631. [PubMed] |
| 107. | Khosla UM, Zharikov S, Finch JL, Nakagawa T, Roncal C, Mu W, Krotova K, Block ER, Prabhakar S, Johnson RJ. Hyperuricemia induces endothelial dysfunction. Kidney Int. 2005;67:1739-1742. [PubMed] |
| 108. | Mercuro G, Vitale C, Cerquetani E, Zoncu S, Deidda M, Fini M, Rosano GM. Effect of hyperuricemia upon endothelial function in patients at increased cardiovascular risk. Am J Cardiol. 2004;94:932-935. [PubMed] |
| 109. | Mazzali M, Hughes J, Kim YG, Jefferson JA, Kang DH, Gordon KL, Lan HY, Kivlighn S, Johnson RJ. Elevated uric acid increases blood pressure in the rat by a novel crystal-independent mechanism. Hypertension. 2001;38:1101-1106. [PubMed] |
| 110. | Moriarity JT, Folsom AR, Iribarren C, Nieto FJ, Rosamond WD. Serum uric acid and risk of coronary heart disease: Atherosclerosis Risk in Communities (ARIC) Study. Ann Epidemiol. 2000;10:136-143. [PubMed] |
| 111. | Ndrepepa G, Braun S, Haase HU, Schulz S, Ranftl S, Hadamitzky M, Mehilli J, Schömig A, Kastrati A. Prognostic value of uric acid in patients with acute coronary syndromes. Am J Cardiol. 2012;109:1260-1265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 63] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 112. | Feig DI, Johnson RJ. Hyperuricemia in childhood primary hypertension. Hypertension. 2003;42:247-252. [PubMed] |
| 113. | Soletsky B, Feig DI. Uric acid reduction rectifies prehypertension in obese adolescents. Hypertension. 2012;60:1148-1156. [PubMed] |
| 114. | Feig DI, Soletsky B, Johnson RJ. Effect of Allopurinol on Blood Pressure of Adolescents With Newly Diagnosed Essential Hypertension: A Randomized Trial. JAMA. 2008;300:924-932 [DOI 10.1001/jama.300.8.924]. |
| 115. | Wahba IM, Mak RH. Obesity and obesity-initiated metabolic syndrome: mechanistic links to chronic kidney disease. Clin J Am Soc Nephrol. 2007;2:550-562. [PubMed] |
| 116. | Savino A, Pelliccia P, Chiarelli F, Mohn A. Obesity-related renal injury in childhood. Horm Res Paediatr. 2010;73:303-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 61] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 117. | Darouich S, Goucha R, Jaafoura MH, Zekri S, Ben Maiz H, Kheder A. Clinicopathological characteristics of obesity-associated focal segmental glomerulosclerosis. Ultrastruct Pathol. 2011;35:176-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 46] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 118. | Nguyen S, McCulloch C, Brakeman P, Portale A, Hsu CY. Being overweight modifies the association between cardiovascular risk factors and microalbuminuria in adolescents. Pediatrics. 2008;121:37-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 71] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 119. | Chang A, Van Horn L, Jacobs DR, Liu K, Muntner P, Newsome B, Shoham DA, Durazo-Arvizu R, Bibbins-Domingo K, Reis J. Lifestyle-related factors, obesity, and incident microalbuminuria: the CARDIA (Coronary Artery Risk Development in Young Adults) study. Am J Kidney Dis. 2013;62:267-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 114] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 120. | Lubrano R, Travasso E, Raggi C, Guido G, Masciangelo R, Elli M. Blood pressure load, proteinuria and renal function in pre-hypertensive children. Pediatr Nephrol. 2009;24:823-831. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 49] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 121. | Schwimmer JB, Deutsch R, Kahen T, Lavine JE, Stanley C, Behling C. Prevalence of fatty liver in children and adolescents. Pediatrics. 2006;118:1388-1393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1028] [Cited by in RCA: 1056] [Article Influence: 55.6] [Reference Citation Analysis (1)] |
| 122. | Stranges S, Trevisan M, Dorn JM, Dmochowski J, Donahue RP. Body fat distribution, liver enzymes, and risk of hypertension: evidence from the Western New York Study. Hypertension. 2005;46:1186-1193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 98] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 123. | Targher G, Mantovani A, Pichiri I, Mingolla L, Cavalieri V, Mantovani W, Pancheri S, Trombetta M, Zoppini G, Chonchol M. Nonalcoholic Fatty Liver Disease Is Independently Associated With an Increased Incidence of Chronic Kidney Disease in Patients With Type 1 Diabetes. Diabetes Care. 2014;Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 124] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 124. | Tarantino G, Finelli C. What about non-alcoholic fatty liver disease as a new criterion to define metabolic syndrome? World J Gastroenterol. 2013;19:3375-3384. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 111] [Cited by in RCA: 134] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 125. | Knobler H, Schattner A, Zhornicki T, Malnick SD, Keter D, Sokolovskaya N, Lurie Y, Bass DD. Fatty liver--an additional and treatable feature of the insulin resistance syndrome. QJM. 1999;92:73-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 137] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 126. | Chitturi S, Abeygunasekera S, Farrell GC, Holmes-Walker J, Hui JM, Fung C, Karim R, Lin R, Samarasinghe D, Liddle C. NASH and insulin resistance: Insulin hypersecretion and specific association with the insulin resistance syndrome. Hepatology. 2002;35:373-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 807] [Cited by in RCA: 822] [Article Influence: 35.7] [Reference Citation Analysis (0)] |
| 127. | Sung KC, Wild SH, Byrne CD. Development of new fatty liver, or resolution of existing fatty liver, over five years of follow-up, and risk of incident hypertension. J Hepatol. 2014;60:1040-1045. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 116] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 128. | Pravenec M, Kazdova L, Landa V, Zidek V, Mlejnek P, Simakova M, Jansa P, Forejt J, Kren V, Krenova D. Identification of mutated Srebf1 as a QTL influencing risk for hepatic steatosis in the spontaneously hypertensive rat. Hypertension. 2008;51:148-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 129. | Halbach SM, Flynn J. Treatment of obesity-related hypertension in children and adolescents. Curr Hypertens Rep. 2013;15:224-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 130. | Welch WP, Yang W, Taylor-Zapata P, Flynn JT. Antihypertensive drug use by children: are the drugs labeled and indicated? J Clin Hypertens (Greenwich). 2012;14:388-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 34] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 131. | Yoon EY, Cohn L, Rocchini A, Kershaw D, Freed G, Ascione F, Clark S. Antihypertensive prescribing patterns for adolescents with primary hypertension. Pediatrics. 2012;129:e1-e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 132. | Che Q, Schreiber MJ, Rafey MA. Beta-blockers for hypertension: are they going out of style? Cleve Clin J Med. 2009;76:533-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 133. | Cooper-DeHoff RM, Wen S, Beitelshees AL, Zineh I, Gums JG, Turner ST, Gong Y, Hall K, Parekh V, Chapman AB. Impact of abdominal obesity on incidence of adverse metabolic effects associated with antihypertensive medications. Hypertension. 2010;55:61-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 46] [Article Influence: 3.1] [Reference Citation Analysis (0)] |