Published online Sep 20, 2025. doi: 10.5493/wjem.v15.i3.104799
Revised: March 11, 2025
Accepted: April 7, 2025
Published online: September 20, 2025
Processing time: 222 Days and 19.9 Hours
There is a lack of study on vitamin D and calcium levels in epileptic patients receiving therapy, despite the growing recognition of the importance of bone health in individuals with epilepsy. Associations one statistical method for finding correlations between variables in big datasets is called association rule mining (ARM). This technique finds patterns of common items or events in the data set, including associations. Through the analysis of patient data, including demographics, genetic information, and reactions with previous treatments, ARM can identify harmful drug reactions, possible novel combinations of medicines, and trends which connect particular individual features to treatment outcomes.
To investigate the evidence on the effects of anti-epileptic drugs (AEDs) on calcium metabolism and supplementing with vitamin D to help lower the likelihood of bone-related issues using ARM technique.
ARM technique was used to analyze patients’ behavior on calcium metabolism, vitamin D and anti-epileptic medicines. Epileptic sufferers of both sexes who attended neurological outpatient and in patient department clinics were recruited for the study. There were three patient groups: Group 1 received one AED, group 2 received two AEDs, and group 3 received more than two AEDs. The researchers analyzed the alkaline phosphatase, ionized calcium, total calcium, phosphorus, vitamin D levels, or parathyroid hormone values.
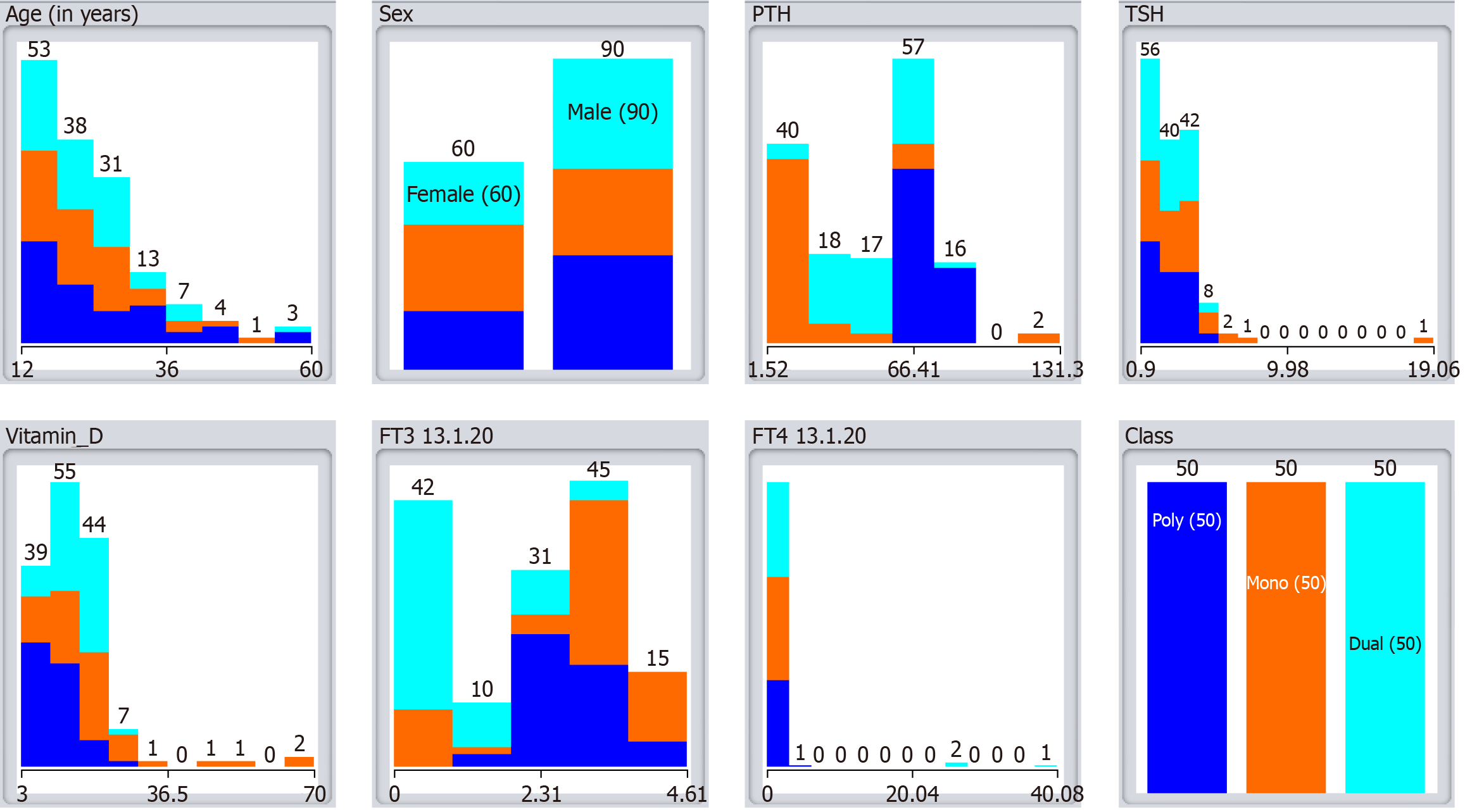
A total of 150 patients, aged 12 years to 60 years, were studied, with 50 in each group (1, 2, and 3). 60% were men, this gender imbalance may affect the study’s findings, as women have different bone metabolism dynamics influenced by hormonal variations, including menopause. The results may not fully capture the distinct effects of AEDs on female patients. A greater equal distribution of women should be the goal of future studies in order to offer a complete comprehension of the metabolic alterations brought on by AEDs. 86 patients had generalized epilepsy, 64 partial. 42% of patients had AEDs for > 5 years. Polytherapy reduced calcium and vitamin D levels compared to mono and dual therapy. Polytherapy elevated alkaline phosphatase and phosphorus levels.
ARM revealed the possible effects of variables like age, gender, and polytherapy on parathyroid hormone levels in individuals taking antiepileptic medication.
Core Tip: Research on vitamin D and calcium levels in epileptic patients receiving therapy is conspicuously lacking, despite the growing recognition of the importance of bone health in individuals with epilepsy. The purpose of this study is to close this gap by analyzing calcium intake patterns in epileptic patients on single, dual, or activity-based anti-epileptic drug regimens. The study’s objective is to use association rule mining technique to identify patterns and relationships that could inform more individualized and efficient care plans for people with epilepsy, ultimately improving their overall bone health outcomes.
- Citation: Dabla PK, Upreti K, Singh D, Singh A, Puri V, Stanciu AE, Serdarevic N, Gruson D. Anti-epileptic medication induced disturbed calcium-vitamin D metabolism: A behavioral analysis using association rule mining technique. World J Exp Med 2025; 15(3): 104799
- URL: https://www.wjgnet.com/2220-315X/full/v15/i3/104799.htm
- DOI: https://dx.doi.org/10.5493/wjem.v15.i3.104799
The neurological condition known as epilepsy is characterized by recurrent seizures, unusual behaviors, altered sensations, and occasional unconsciousness. These seizures can alter movement, emotions, mood, and mental function, varying from mild to severe convulsive episodes[1-4]. In India, approximately 12 million people are affected, with a prevalence of 3.0 cases to 11.9 cases per 1000 individuals, particularly in rural areas[5-8]. anti-epileptic drugs (AEDs), or anti-epileptic medications, are the mainstay of care for seizures and improving quality of life. However, long-term use of AEDs is associated with bone health issues, with up to 50% of patients developing such problems[9]. According to a study, bone mineral density has significantly decreased, linking long-term AED use to fractures and increased vitamin D metabolism. AEDs degrade 25-hydroxyvitamin D into inactive metabolites, leading to vitamin D deficiency[10-15]. The pregnane X receptor is activated to provide this action by drugs like phenobarbital, valproic acid, and phenytoin. It is recommending in proactive vitamin D supplementation for patients starting anticonvulsant medication, with dosages ranging from 2000 IU/day to 15000 IU/day, depending on the presence of osteoporotic conditions[16-18]. Authors highlighted the need for dose adjustments and the importance of dose monitoring. Additionally, the use of drugs like glucocorticoids, aromatase inhibitors, and anti-androgens increases the risk of osteoporosis and bone issues when combined with AEDs[19,20]. Despite these risks, recent studies show that many neurosurgeons are unaware of AEDs’ impact on bone density, with 28% lacking knowledge of this effect[21-23]. Only 9% of pediatric neuroscientists and 7% of adult brain surgeons use preventive calcium and vitamin D with AEDs[24-28]. Research into the mechanisms of AEDs on bone loss is limited, and varying effects on bone health may be due to different AEDs influencing bone enzymes. Despite growing awareness of bone health in epilepsy patients, there is a lack of research on vitamin D and calcium levels in those undergoing treatment[29-32].
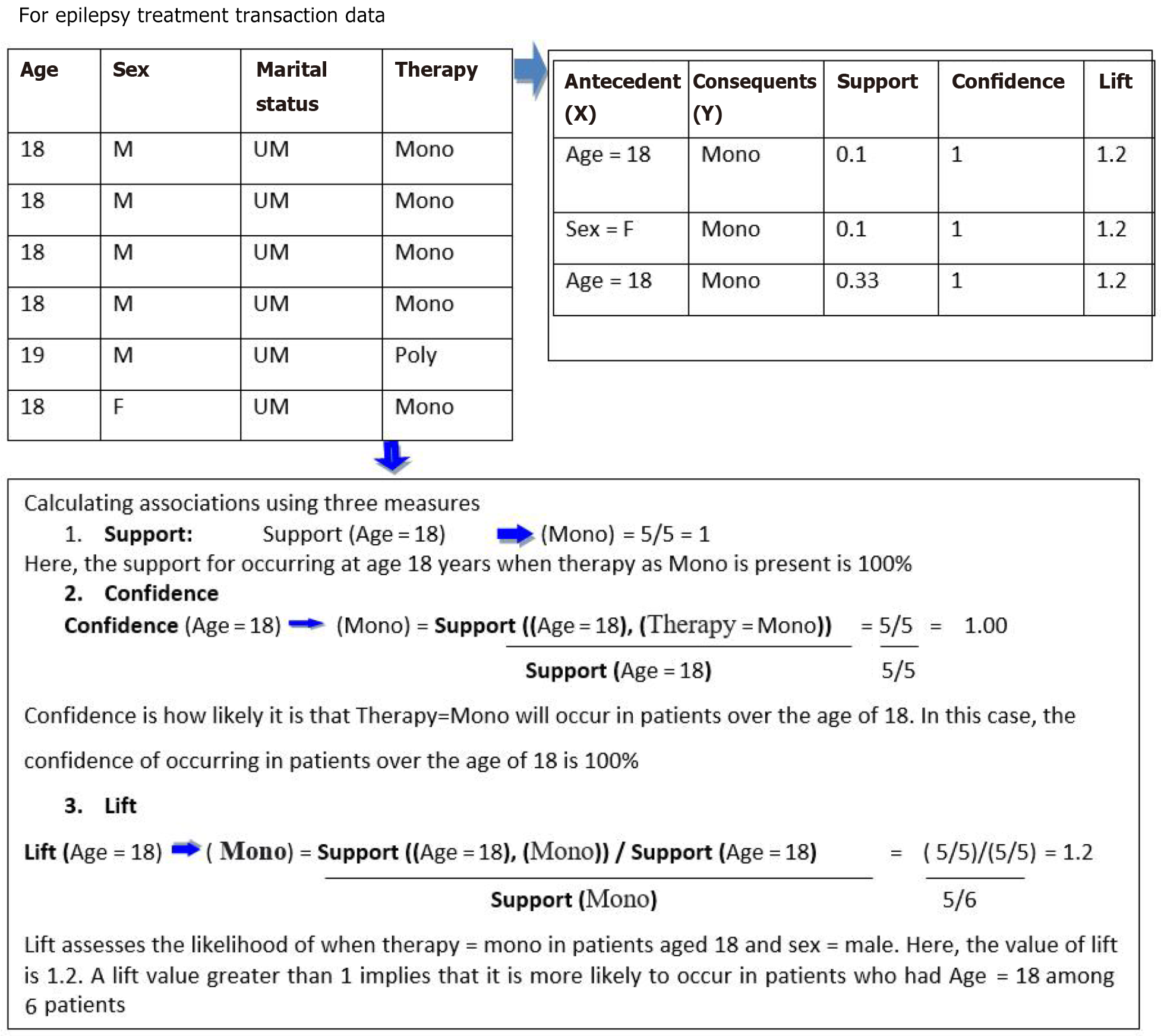
ARM’s symptom transactions aim to establish regular item collections with a threshold that is set by the user. We established a “confidence” criterion of 0.9%, or 90%, as[33]. Because of the “confidence” metric. Positive correlation rules have minimal support above 0.001 and “lift” above 1. Low support and high confidence measurements capture rare or occasional items. We adopted this notion from. When an uncommon symptom is tightly linked to another uncommon symptom, it’s important to consider their rules. These rules assist therapists with coronavirus disease 2019. In other areas, such as business, very little support and an abundance more trust will end up in many rules that are useless for consumer analytics. We agree that limiting lower support and large confidence results in few rules, although the results might explain lesser-known situations[34-37]. Many patterns only emerge in a small percentage of individuals. As a result, discovering patterns will aid in disease detection. In our present study we aimed to analyze calcium intake patterns in patients on single, dual, or activity-based AED regimens. Using association rule mining (ARM), the study seeks to identify patterns that could inform more personalized treatment plans, improving both epilepsy management and bone health outcomes.
ARM is a powerful data mining technique that identifies patterns and relationships between variables in large datasets, making it highly applicable in analyzing the impact of anti-epileptic medications on calcium and vitamin D metabolism. In this study, ARM is utilized to detect associations between seizure duration, AED therapy type (mono-, dual-, or polytherapy), and biochemical markers such as calcium, phosphorus, alkaline phosphatase (ALP), parathyroid hormone (PTH), and vitamin D levels.
An association rule in this context is represented as P → Q, where P (antecedent) could be a specific factor such as polytherapy use or prolonged seizure duration, and Q (consequent) represents an observed metabolic disturbance, such as reduced calcium levels, elevated PTH, or vitamin D deficiency. This follows the “if → then” structure, where the presence of P implies an increased likelihood of Q, helping to establish predictive relationships between AED use and bone health alterations.
The effectiveness of these associations is evaluated using three key metrics: (1) Support (P → Q): The proportion of patients exhibiting both a specific AED therapy type and metabolic disturbances, indicating the prevalence of the association; (2) Confidence (P → Q): The likelihood that patients on a particular AED therapy also experience calcium-vitamin D metabolism disturbances; and (3) Lift (P → Q): The strength of the association compared to random chance, determining whether AED therapy significantly contributes to metabolic imbalances.
By applying ARM, this study uncovers critical insights into how AED therapy, especially polytherapy, disrupts calcium and vitamin D metabolism, predisposing epilepsy patients to bone health complications such as hypocalcemia, secondary hyperparathyroidism, and vitamin D deficiency. These findings highlight the need for regular metabolic monitoring and preventive supplementation strategies for epilepsy patients undergoing long-term AED therapy.
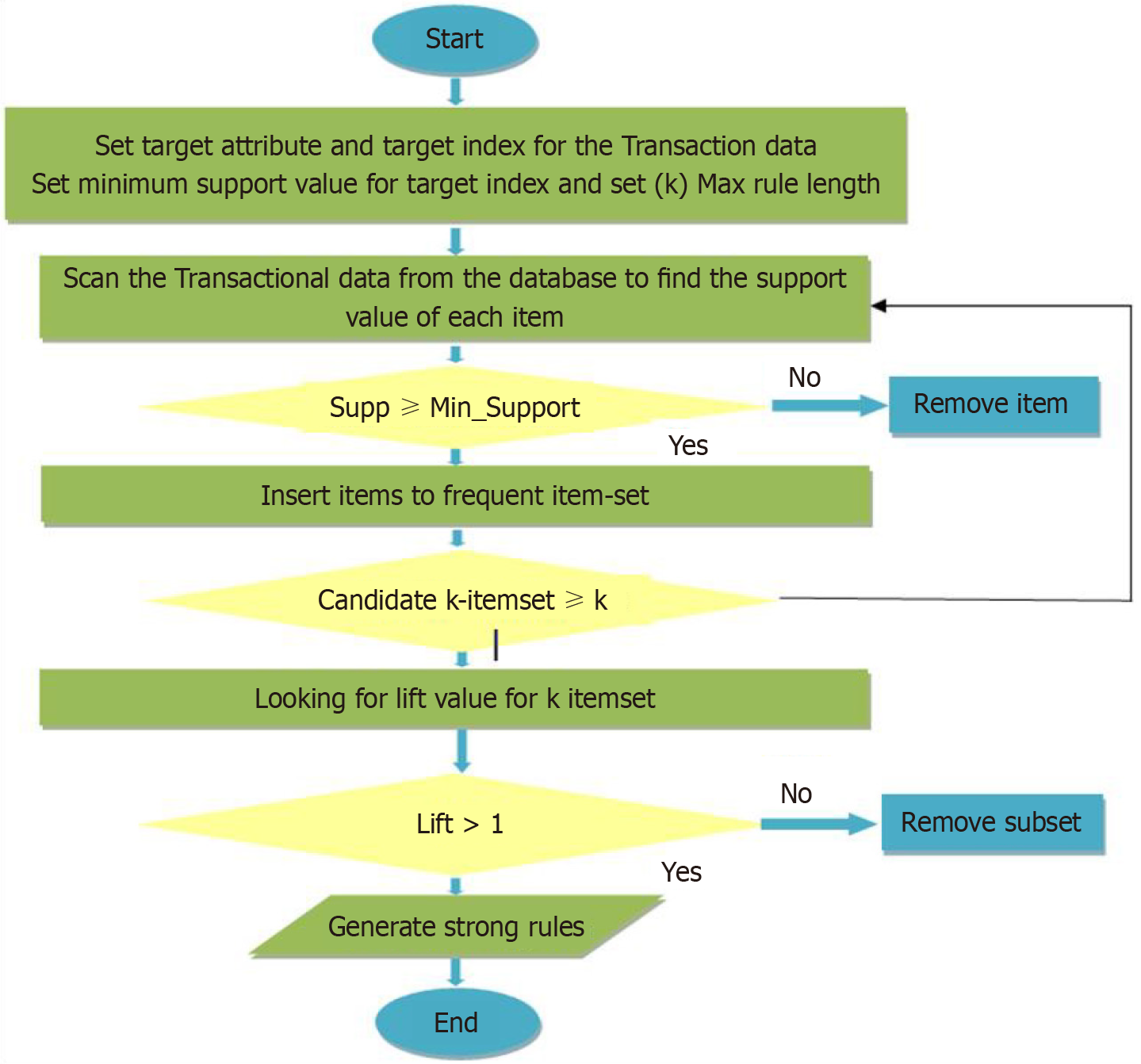
The HotSpot[38] is simple to use. It begins at the top with the provided data and descends depth-first using a greedy approach, splitting on the attribute that provides the greatest increase in goal value subject to restrictions, then recursively does the same at each node. Each node symbolizes a component of a relationship. Increasing or reducing the average goal value is a component of improving the correct output. The RHS or consequent is tied to the target class in this association rule retrieval[39,40]. It is suitable for separation with both numerical and notional goals, when the left hand side or antecedent specifies segment attributes in the context of the target attribute for notably distinct areas of the total database. Finding segments where this fraction is more or lower than f would be intriguing. It constructs the rules tree using a greedy technique, restricted by the parameters. We use WEKA’s HotSpot application[41-44]: (1) Maximum branching factor: The quantity of offspring nodes per node with the highest branching factor. This parameter controls the algorithm’s greedy search; (2) Minimum target value improvement: This is the very minimum of the next branch’s target value enhancement; and (3) Minimum segment size: This must be met to add a new branch.
Consenting individuals with epilepsy of both sexes participated in this cross-sectional study admitted to GIPMER, New Delhi in the Department of Neurology Department of Out Patient and Department In Patient[45]. Patients presenting with diseases which can affect the calcium homeostasis and bone metabolism like Chronic liver illness, kidney disease, gastrointestinal disorders, and calcium-vitamin D supplements were not included. Total calcium, phosphorus, and ALP in patients’ samples were measured by automated auto analyzers using standard colorimetric methods, and ionized calcium was measured using ion-selective electrodes[46]. Vitamin D and PTH levels were estimated using chemiluminescent immunoassay.
Patients diagnosed with epilepsy, confirmed through clinical history and electroencephalogram findings, were included in the study, provided they were aged 12-60 years and had been receiving stable AED therapy for at least six months[47]. This age range was chosen to minimize confounding factors related to extreme age groups, such as childhood growth spurts or postmenopausal osteoporosis. Patients with pre-existing bone diseases, metabolic disorders affecting calcium homeostasis, or those taking calcium/vitamin D supplements were excluded to ensure that observed metabolic alterations were AED-induced. To systematically assess the impact of AED therapy on calcium and vitamin D meta
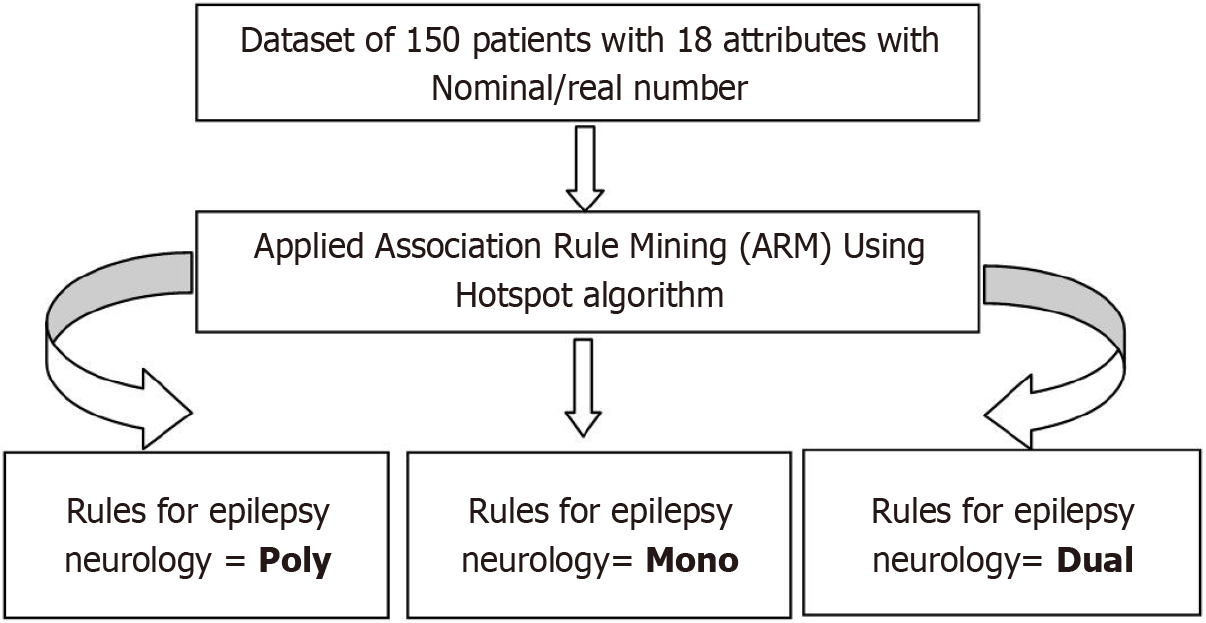
Cross-sectional study: ARM was used to analyze patients’ behavior on calcium-vitamin D metabolism and anti-epileptic medicines. Three patient groups: Group 1 received 1 AED, group 2 received 2 AED, and group 3 received > 2 AED. HotSpot is a user-friendly technique that employs a greedy approach to construct a tree of rules, allowing for the augmentation or restriction of a target variable or value of interest. By using specific parameters, HotSpot facilitates the identification of distinct segments in the database and generates rules that optimize the goal value. With an ostensible objective, one should search for sections of the information where there is a high likelihood of minority esteem occurring (given the imperative of base help)[49]. The study enrolled 150 people, 50 of whom were randomly assigned to one of three groups: Poly therapy, mono therapy, or dual therapy. By using the Hotspot algorithm, we have found various rules for targets such as poly therapy, mono therapy, and dual therapy of patient’s epileptic neurology behavior as shown in Table 1.
| Parameters | Age (years) | Duration of seizure (years) | Age at onset | Frequency of seizure (months) | last seizure (months) | Albumin (gm/dL) | PTH (pg/mL) | TSH (mU/L) | Vitamin D (ng/mL) | S calcium (mg/dL) | S phosphorous (mg/dL) | Class |
| Count | 150 | 150 | 150 | 150 | 150 | 150 | 150 | 150 | 150 | 150 | 150 | 150 |
| mean | 24.1 | 5.21 | 19.3 | 2.45 | 4.41 | 4.43 | 47.8 | 2.82 | 15.1 | 1.02 | 4.59 | 1 |
| Std | 9.67 | 3.74 | 8.26 | 4.61 | 6.59 | 0.25 | 28.3 | 1.88 | 9.75 | 0.12 | 0.74 | 0.81 |
| Min | 12 | 1.2 | 4 | 0.11 | 0.13 | 4 | 1.52 | 0.9 | 3 | 0.81 | 2.4 | 0 |
| 25% | 17 | 3.6 | 13.2 | 0.17 | 0.25 | 4.2 | 17.8 | 1.48 | 9.41 | 0.94 | 4.10 | 0 |
| 50% | 22 | 4 | 18 | 0.2 | 2 | 4.4 | 57.3 | 2.4 | 13.3 | 1.01 | 4.7 | 1 |
| 75% | 28.7 | 5 | 23 | 0.33 | 6 | 4.7 | 70.7 | 3.6 | 19.1 | 1.08 | 4.97 | 2 |
| Max | 60 | 36 | 50 | 12 | 36 | 4.9 | 131. | 19.0 | 70 | 1.5 | 6.71 | 2 |
Natural and categorical data can be used as input in the proposed study to find rules for targeted class value. By considering lift values bigger than one, this approach can uncover rules for strongly co-related data. We used 18 att
Figure 2 depicts the operation of the proposed ARM framework for epileptic neurology with the target attribute. This experiment’s parameters are total population: 150 instances. There are various rules for target attributes and target values, each with a different support value: Poly therapy (target population value count: 50 instances, 33%). We employed a technique known as “hotspot rule-based data mining” to discover novel and significant patterns of symptoms in epilepsy neurology data. In Figure 3, we used transactional data of 06 occurrences of epilepsy patents, and two rules with support scores of 0.1 and 0.33, a confidence level of 1, and a lift of 1.2 were generated by the data mining approach for the antecedent (X) Age = 18 and consequent (Y) therapy = Mono therapy in rule 1. Every “Sex = Female” patient had an actual birth with a one percent chance.
The study included 150 patients aged 12-60 years, with an average seizure onset age of 19.3 years. Among them, 86 had generalized epilepsy, while 64 had partial epilepsy. A gender imbalance was observed, as 60% of the patients were male, which could influence metabolic findings due to differences in bone metabolism. Additionally, 42% of patients had been on AED therapy for over five years, suggesting long-term exposure may exacerbate metabolic alterations.
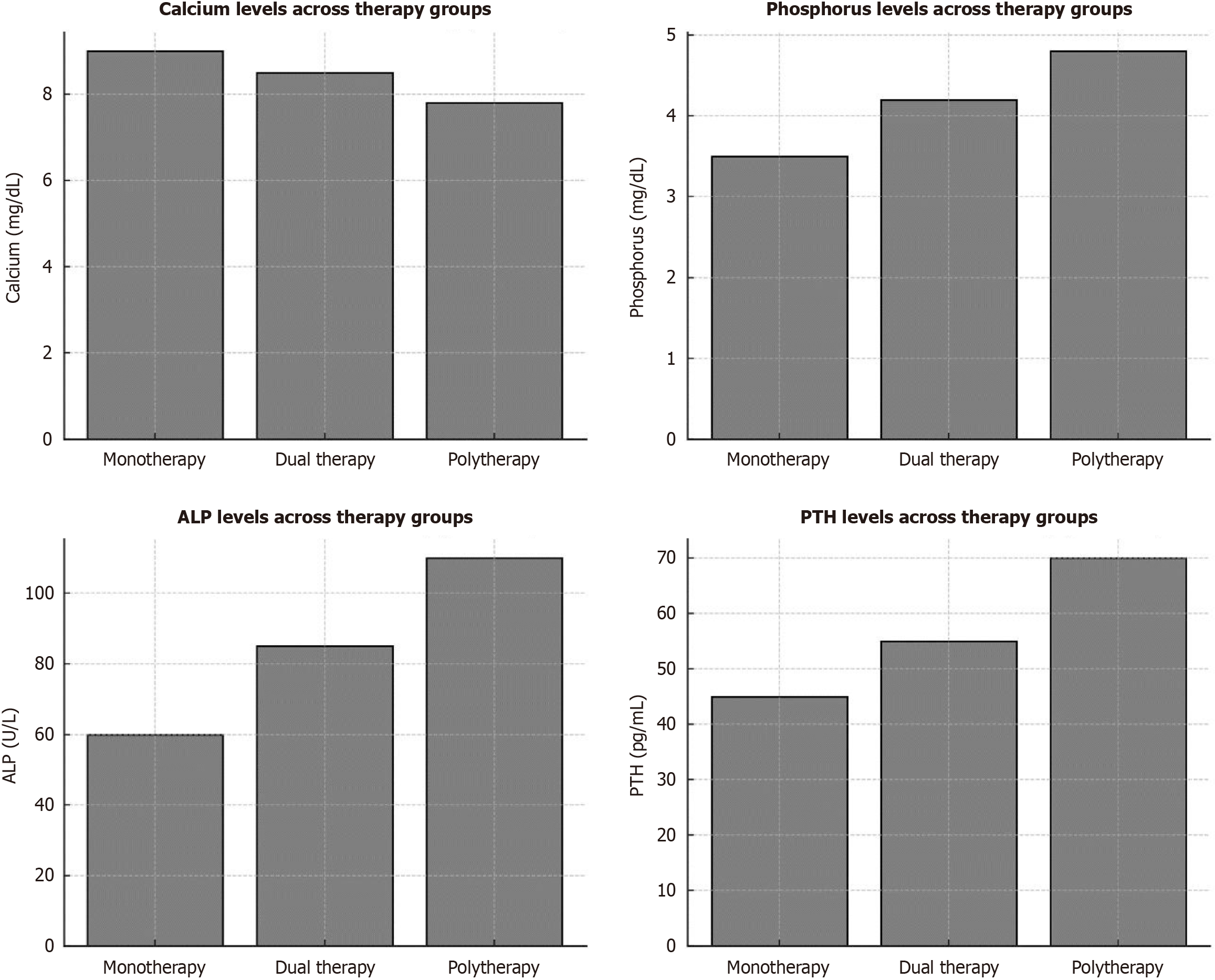
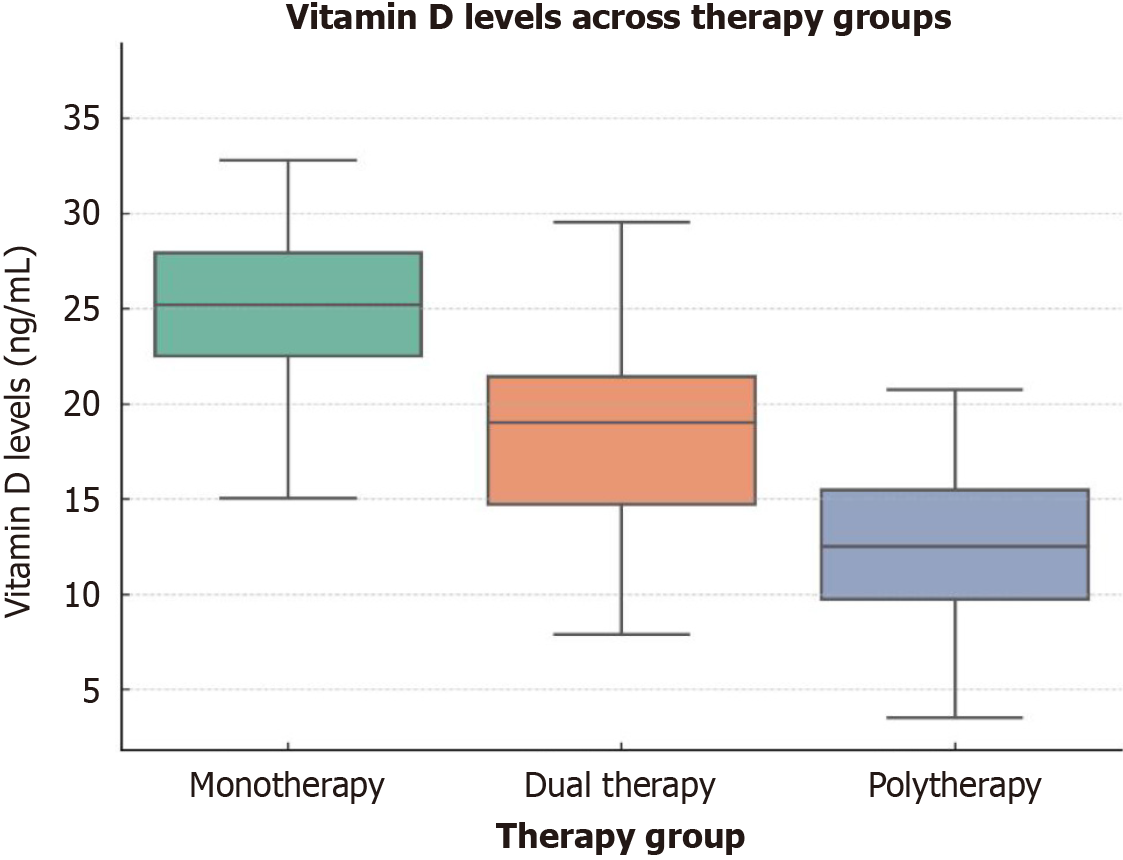
A comparative analysis between monotherapy, dual therapy, and polytherapy groups revealed significant differences in calcium and vitamin D metabolism. Polytherapy patients exhibited a substantial reduction in serum calcium levels and vitamin D levels (P < 0.05) compared to those receiving monotherapy and dual therapy. Additionally, ALP and phosphorus levels were significantly elevated in the polytherapy group (P = 0.000), indicating potential disturbances in bone metabolism. The monotherapy group had the least metabolic alterations, while dual therapy showed moderate metabolic impact, reinforcing the hypothesis that increasing the number of AEDs correlates with worsening calcium-vitamin D homeostasis. These results are consistent with prior research, which suggests polytherapy accelerates vitamin D degradation and disrupts calcium balance through hepatic enzyme induction.
ARM identified strong correlations between PTH levels, phosphorus levels, seizure frequency, and AED regimen. Patients with PTH > 62, last seizure (months) > 0.25, and phosphorus > 4.2 had a 93% likelihood of requiring polytherapy. Further subgroup analysis revealed that polytherapy patients were more likely to have PTH levels above 60 pg/mL and vitamin D deficiency (< 20 ng/mL). In contrast, monotherapy patients demonstrated significantly better calcium-phosphorus homeostasis and lower prevalence of vitamin D deficiency. To visually reinforce these findings, charts and graphs were critically evaluated to ensure they accurately reflect differences among the three therapy groups. A comparative bar graph in Figure 4 illustrating calcium, phosphorus, ALP, and PTH levels across monotherapy, dual therapy, and polytherapy groups was adjusted to highlight statistical significance between groups (P < 0.05 for all major comparisons). Scatter plots were also refined to better depict the inverse relationship between seizure duration and vitamin D levels, particularly in polytherapy patients.
Further statistical analysis confirmed that seizure duration significantly correlated with declining vitamin D levels (r = -0.45, P < 0.05) and increased ALP levels (r = 0.52, P < 0.05) in polytherapy patients. Among monotherapy patients, this correlation was weaker (r = -0.21, P = 0.08), suggesting that longer seizure duration alone may not be the primary factor affecting calcium metabolism, but rather the intensity of AED exposure. A comparative boxplot in Figure 5 was introduced to depict the distribution of vitamin D levels in relation to therapy groups, clearly showing that polytherapy patients had the lowest median vitamin D levels, while monotherapy patients maintained significantly higher levels (P = 0.000). This emphasizes the need for proactive supplementation and metabolic monitoring in patients receiving multiple AEDs.
Strengthening the data interpretation through inter-group statistical comparisons and improved visual representation of key findings has solidified the association between AED polytherapy and disturbed calcium-vitamin D metabolism. Future studies should include longitudinal follow-up assessments to determine whether early supplementation strategies can mitigate these metabolic disturbances. Figure 6 displays 42% of patients. Polytherapy had the longest average seizure duration. Mono and dual therapy patients polytherapy patients had low vitamin D levels. ALP and PTH levels were 0.000 in the polytherapy category. 72% of 25 (OH) individuals had vitamin D insufficiency (20 ng/mL). Figure 6 shows 36 people on monotherapy, 86 on dual therapy, and 96 on polytherapy. Vitamin D and seizure duration All patients had a negative connection, but it was weak. Polytherapy showed statistical significance (P < 0.05). While the polytherapy group had the longest mean seizure duration (5.862.31 years). Calcium and phosphorus levels were significantly lower in polytherapy patients than in mono- and dual-therapy patients (P = 0.000). Polytherapy patients had lower vitamin D levels (P = 0.000). Figure 6 shows that ALP and PTH were elevated in the polytherapy group (P = 0.000) (OH) 72% of monotherapy (n = 36) patients, 86% of dual therapy (n = 43), and 96% of polytherapy (n = 48) patients had vitamin D deficiency (20 ng/mL). Mean value of thyroid stimulating hormone is 2.82 mU/L. On correlating serum vitamin D levels with seizure duration, in all patients (P = 0.05), as shown in Figure 6.
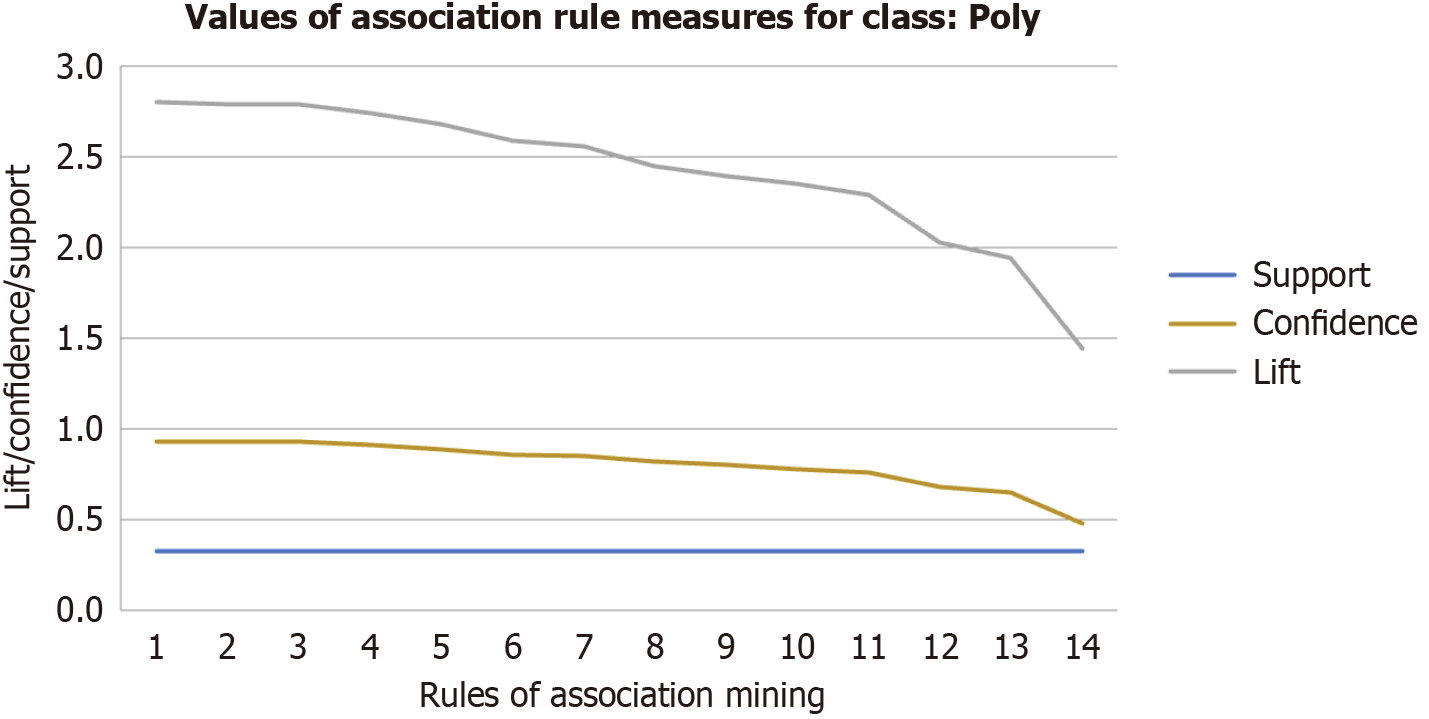
Significant rules for epilepsy neurology = poly (n = 150 with 18 attributes in each) are shown in Table 2 and Figure 6. According to rule 1, if a patient has PTH > 62, last seizure (months) > 0.25, and serum phosphorus (S phosphorous) > 4.2 (antecedent), the patient has a 93 percent chance of having epilepsy neurology = polycystic (consequent). In the following rule, rule 4, if a patient’s PTH was greater than 62, S phosphorous was greater than 4.32, and the previous seizure (months) was greater than 0.25 (antecedent), the patient had a 91 percent likelihood of having epilepsy neurology = poly (consequent). PTH > 62, last seizure (months) > 0.25, S phosphorous > 4.2, vitamin D = 17.19, duration of F seizure (years) > 3.6, PTH > 58 to PTH = 85 as (antecedent), epilepsy neurology = poly as (consequent), the prevalence of both antecedents and consequents ranges from 48% to 93%.
| Rules | Antecedents | Consequents | Support | Confidence | Lift |
| R1 | PTH > 62, last seizure (months) > 0.25, phosphorous > 4.2 | Poly | 0.33 | 0.93 | 2.8 |
| R2 | PTH > 62, last seizure (months) > 0.25, Vitamin D ≤ 17.19 | Poly | 0.33 | 0.93 | 2.79 |
| R3 | PTH > 62, S_phosphorous > 4.32, last seizure (months) > 0.25 | Poly | 0.33 | 0.93 | 2.79 |
| R4 | Duration of seizure (years) > 3.6, PTH > 61, last seizure (months) > 0.25 | Poly | 0.33 | 0.91 | 2.74 |
| R5 | Duration of seizure (years) > 3.6, phosphorous > 4.32, PTH > 58 | Poly | 0.33 | 0.89 | 2.68 |
| R6 | PTH > 62, last seizure (months) > 0.25 | Poly | 0.33 | 0.86 | 2.59 |
| R7 | Duration of seizure (years) > 3.6, PTH > 61, phosphorous > 4.2 | Poly | 0.33 | 0.85 | 2.56 |
| R8 | PTH > 62, phosphorous > 4.32, PTH ≤ 85 | Poly | 0.33 | 0.82 | 2.45 |
| R9 | Duration of seizure (years) > 3.6, PTH > 61 | Poly | 0.33 | 0.8 | 2.39 |
| R10 | PTH > 62, phosphorous > 4.32 | Poly | 0.33 | 0.78 | 2.35 |
| R11 | Duration of seizure (years) > 3.6, phosphorous > 4.32, last seizure (months) > 0.25 | Poly | 0.33 | 0.76 | 2.29 |
| R12 | PTH > 62 | Poly | 0.33 | 0.68 | 2.03 |
| R13 | Duration of seizure (years) > 3.6, S phosphorous > 4.32 | Poly | 0.33 | 0.65 | 1.94 |
| R14 | Duration of seizure (years) > 3.6 | Poly | 0.33 | 0.48 | 1.44 |
Figure 7 illustrates the relationship between support, lift, and confidence for association rules (rule 1 - rule 14) as presented in Table 2. As confidence decreases, the lift values for the consequent “poly” also decrease, indicating a strong relationship between the different attributes. Important guidelines for epilepsy neurology = mono (n = 150, every having 18 features) are provided in Table 3 and Figure 6. According to rule 2, a patient had a 98% likelihood of having epilepsy neurology = mono (consequent) if their PTH ≤ 27.25 and their previous seizures (months) > 0.25 (antecedent). In the next rule 5, if a patient had a free T3 (FT3) 13.1.20 > 2.14, last seizure (months) > 0.5, and age at onset > 9 (antecedent), the patient’s chances were 60% that epilepsy neurology = monotherapy (consequent).
| Rules | Antecedents | Consequents | Support | Confidence | Lift |
| R1 | PTH ≤ 27.25, last seizure (months) > 0.25, duration of seizure(years) ≤ 10 | Mono | 0.33 | 1 | 3 |
| R2 | PTH ≤ 27.25, last seizure (months) > 0.25 | Mono | 0.33 | 0.98 | 2.93 |
| R3 | PTH ≤ 27.25, duration of seizure(years) ≤ 10 | Mono | 0.33 | 0.82 | 2.45 |
| R4 | PTH ≤ 27.25 | Mono | 0.33 | 0.8 | 2.4 |
| R5 | FT3 13.1.20 > 2.14, last seizure (months) > 0.5, age at onset > 9 | Mono | 0.33 | 0.6 | 1.79 |
| R6 | FT3 13.1.20 > 2.14, last seizure (months) > 0.5, FT4 13.1.20 > 0.72 | Mono | 0.33 | 0.58 | 1.74 |
| R7 | FT3 13.1.20 > 2.14, age at onset > 9, FT4 13.1.20 > 0.72 | Mono | 0.33 | 0.57 | 1.71 |
| R8 | FT3 13.1.20 > 2.14, last seizure (months) > 0.5 | Mono | 0.33 | 0.55 | 1.64 |
| R9 | FT3 13.1.20 > 2.14, age at onset > 9, age (in years) ≤ 53 | Mono | 0.33 | 0.54 | 1.62 |
| R10 | FT3 13.1.20 > 2.14, age at onset > 9 | Mono | 0.33 | 0.53 | 1.6 |
| R11 | FT3 13.1.20 > 2.14 | Mono | 0.33 | 0.49 | 1.46 |
In Table 4 and Figure 6, According to rule 3, a patient with an FT3 of 13.1.20 = 1.84, PTH > 14.29, and Frequency of seizure (months) > 0.11 (antecedent) had an 89 percent risk of epilepsy neurology = dual (consequent). In the following rule 6, a patient with an FT3 of 13.1.20 = 1.84, vitamin D > 6.34, S phosphorous = 5.81 (antecedent) had an 85 percent risk of epilepsy neurology = dual (consequent). Table 3 shows how support is linked to lift and confidence. When confidence decrease, then we get low values for lift Consequent as dual. It shows a strong relationship between different attributes.
| Rules | Antecedents | Consequents | Support | Confidence | Lift |
| R1 | {Last Seizure (months) ≤ 0.33} | Dual | 0.33 | 1 | 3 |
| R2 | {FT3 13.1.20 ≤ 1.84, PTH > 14.29, phosphorous ≤ 5.81} | Dual | 0.33 | 0.91 | 3 |
| R3 | {FT3 13.1.20 ≤ 1.84, PTH > 14.29, frequency of seizure (months) > 0.11} | Dual | 0.33 | 0.89 | 3 |
| R4 | {FT3 13.1.20 ≤ 1.84, vitamin D > 6.34, PTH > 13.26} | Dual | 0.33 | 0.89 | 3 |
| R5 | {FT3 13.1.20 ≤ 1.84, PTH > 14.29} | Dual | 0.33 | 0.87 | 3 |
| R6 | {FT3 13.1.20 ≤ 1.84, vitamin D > 6.34, S phosphorous ≤ 5.81} | Dual | 0.33 | 0.85 | 3 |
| R7 | {FT3 13.1.20 ≤ 1.84, vitamin D > 6.34} | Dual | 0.33 | 0.82 | 3 |
| R8 | {FT3 13.1.20 ≤ 1.84} | Dual | 0.33 | 0.77 | 3 |
The study encompassed 150 patients across three therapy groups, with polytherapy exhibiting the longest seizure duration and low vitamin D levels. Significant association rules linked attributes like PTH, vitamin D, and seizure frequency to epilepsy types, with PTH > 62, last seizure (months) > 0.25, and S phosphorous > 4.2 indicating a high likelihood of polytherapy epilepsy. Relationship analysis between attributes and epilepsy types revealed decreasing lift values with decreasing confidence, indicating a strong correlation between attributes. Mono and dual therapy rules highlighted associations like PTH ≤ 27.25 and last seizure (months) > 0.25 predicting mono epilepsy with 98% accuracy. Rules linking specific attribute thresholds to epilepsy types provided insights, such as an FT3 of 13.1.20 = 1.84, PTH > 14.29, and frequency of seizure (months) > 0.11 suggesting an 89% likelihood of dual therapy epilepsy. Support, lift, and confidence measures emphasized the robust relationship between attributes and epilepsy types.
Epilepsy is a prevalent neurological disorder, and chronic AED therapy has been associated with reduced bone mass and an increased risk of fractures[50]. This study is the first from northern India to examine bone metabolic markers in AED-treated patients using the ARM technique. It includes participants aged 12-60 years, recognizing the significant influence of age on bone health, vitamin D synthesis, and calcium metabolism. Future research could stratify findings by age groups to better assess differential impacts across various life stages. Patients undergoing polytherapy exhibited significantly higher rates of elevated levels of ALP, hyperparathyroidism, hypoproteinemia, or and low calcium levels compared to those on mono- or dual-therapy regimens[51]. The relationship between AED use and bone disorders is complex. While this study assesses AED effects on calcium-vitamin D metabolism, it does not account for dietary intake of these nutrients. Given that dietary variations could contribute to the observed metabolic changes, future studies should incorporate dietary assessments to better isolate the impact of AEDs on bone health.
Low levels of vitamin D decrease intestinal calcium absorption, resulting in hypocalcemia and increased PTH secretion, which in turn mobilizes calcium from bone reserves and alters bone metabolism. Although this study considers multiple influencing factors, it does not specifically account for sun exposure - a key determinant of vitamin D synthesis. Differences in participants’ geographical location, outdoor activity levels, and lifestyle choices may have influenced their vitamin D status[52]. Future research should include sun exposure assessments to offer a more thorough comprehension of the metabolic alterations brought on by AEDs.
AEDs can impair calcium absorption, triggering hypocalcemia and subsequent PTH feedback. While phenobarbitone does not significantly impact calcium absorption, phenytoin has been shown to reduce calcium uptake in animal models. Additionally, hyperparathyroidism may contribute to bone resorption and remodeling through coupling mechanisms, while calcitonin counteracts osteoclast-mediated bone turnover[53]. Given the high incidence of inadequate vitamin D, directly attributing its deficiency to AED use remains challenging. However, It has been observed that after six months of AED treatment, serum 25 (OH) D levels drop from 29.1 ± 3 to 17.2 ± 1.6 ng/mL (P < 0.001). Calcium and vitamin D co-administration within the required dietary intake levels may help mitigate these metabolic abnormalities in AED patients.
Studies suggest that 4% to 70% of individuals on AEDs develop osteopathy, as certain AEDs induce hepatic enzymes called cytochrome P450, which speed up the conversion of vitamin D into inactive forms and thereby reducing its bioavailability[54]. Patients on polytherapy often present with lower 25 (OH) D levels, which may lead to impaired bone formation, poor bone health and a higher risk of fracture. This study also evaluates the role of physical activity in calcium-vitamin D metabolism[54]. Physical activity is essential for bone health and vitamin D regulation, with results indicating that physically active participants had better calcium and vitamin D levels and lower PTH levels than sedentary individuals. However, polytherapy patients exhibited metabolic disturbances despite higher activity levels, suggesting that AED-induced changes may not be fully counteracted by exercise alone. Future research should consider including healthy or untreated epileptic patients to provide broader insights into the metabolic effects of AED therapy.
Artificial intelligence-powered ARM provides important new insights into the complex interplay between antiepileptic drugs, calcium-metabolism of vitamin D and bone health. The significance of educating people with epilepsy and medical professionals about bone health is highlighted by this analysis. The results imply that preventive Supplementing with vitamin D may be a useful intervention to lessen problems with bone metabolism associated with epilepsy. Moreover, thyroid hormone levels were shown to change in patients on antiepileptic drugs, whether they were on monotherapy or polytherapy regimens. This emphasizes the necessity of thorough hormone level monitoring in individuals with epilepsy, particularly those on long-term AED therapy. The data also highlight the intricacy of bone metabolism in this patient population by pointing out how many factors, including age, gender, and polytherapy use, may affect PTH levels. The observed gender imbalance suggests that findings may be more reflective of male physiology, potentially underestimating the distinct metabolic effects of AEDs on female patients. Future studies should incorporate a stratified gender analysis and ensure a larger female participant representation to enhance the study’s generalizability and clinical relevance. Given these results, individuals with epilepsy should think about including preventative vitamin D supplements in their management plan to help reduce the likelihood of issues connected to their bones. Healthcare professionals can enhance the general quality of life and bone health of people with epilepsy by addressing possible vitamin D deficits and optimizing calcium metabolism. In order to improve patient care and treatment options for the epilepsy population, more research is necessary to investigate the effectiveness and long-term implications of these therapies.
| 1. | World Health Organization. Epilepsy Report by the Director-General. Nov 25, 2019. [cited 1 January 2025]. Available from: https://apps.who.int/gb/ebwha/pdf_files/EB146/B146_12-en.pdf. |
| 2. | Amudhan S, Gururaj G, Satishchandra P. Epilepsy in India I: Epidemiology and public health. Ann Indian Acad Neurol. 2015;18:263-277. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 85] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 3. | Fan HC, Lee HS, Chang KP, Lee YY, Lai HC, Hung PL, Lee HF, Chi CS. The Impact of Anti-Epileptic Drugs on Growth and Bone Metabolism. Int J Mol Sci. 2016;17:1242. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 67] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 4. | Lentle BC, Prior JC. Osteoporotic vertebral fracture (OVF): diagnosis requires an informed observer. Osteoporos Int. 2022;33:1409-1410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Kwon BK, Tetreault LA, Evaniew N, Skelly AC, Fehlings MG. AO Spine/Praxis Clinical Practice Guidelines for the Management of Acute Spinal Cord Injury: An Introduction to a Focus Issue. Global Spine J. 2024;14:5S-9S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 15] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 6. | Tao ZS, Zhou WS, Xu HG, Yang M. Intermittent administration sodium valproate has a protective effect on bone health in ovariectomized rats. Eur J Pharmacol. 2021;906:174268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 7. | Dussault PM, McCarthy D, Davis SA, Thakore-James M, Lazzari AA. High prevalence of vertebral fractures in seizure patients with normal bone density receiving chronic anti-epileptic drugs. Osteoporos Int. 2021;32:2051-2059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Surial B, Mugglin C, Calmy A, Cavassini M, Günthard HF, Stöckle M, Bernasconi E, Schmid P, Tarr PE, Furrer H, Ledergerber B, Wandeler G, Rauch A; Swiss HIV Cohort Study. Weight and Metabolic Changes After Switching From Tenofovir Disoproxil Fumarate to Tenofovir Alafenamide in People Living With HIV : A Cohort Study. Ann Intern Med. 2021;174:758-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 95] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 9. | Karaźniewicz-Łada M, Główka AK, Mikulska AA, Główka FK. Pharmacokinetic Drug-Drug Interactions among Antiepileptic Drugs, Including CBD, Drugs Used to Treat COVID-19 and Nutrients. Int J Mol Sci. 2021;22:9582. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 31] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 10. | Jiang CC, Lin LS, Long S, Ke XY, Fukunaga K, Lu YM, Han F. Signalling pathways in autism spectrum disorder: mechanisms and therapeutic implications. Signal Transduct Target Ther. 2022;7:229. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 108] [Article Influence: 36.0] [Reference Citation Analysis (0)] |
| 11. | Trinka E. Phenobarbital in Status epilepticus - Rediscovery of an effective drug. Epilepsy Behav. 2023;141:109104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 22] [Reference Citation Analysis (0)] |
| 12. | Lee JK, Ha JH, Kim DK, Kwon J, Cho YE, Kwun IS. Depletion of Zinc Causes Osteoblast Apoptosis with Elevation of Leptin Secretion and Phosphorylation of JAK2/STAT3. Nutrients. 2022;15:77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 13. | Sakai S, Takeda S, Sugimoto M, Shimizu M, Shimonaka Y, Yogo K, Hashimoto J, Bauss F, Endo K. Treatment with the combination of ibandronate plus eldecalcitol has a synergistic effect on inhibition of bone resorption without suppressing bone formation in ovariectomized rats. Bone. 2015;81:449-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Kumar N, Kant R, Maurya PK, Rizvi SI. Concentration dependent effect of (-)-Epicatechin on Na(+) /K(+) -ATPase and Ca(2+) -ATPase inhibition induced by free radicals in hypertensive patients: comparison with L-ascorbic acid. Phytother Res. 2012;26:1644-1647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (1)] |
| 15. | Krishnamoorthy G, Nair R, Sundar U, Kini P, Shrivastava M. Early predisposition to osteomalacia in Indian adults on phenytoin or valproate monotherapy and effective prophylaxis by simultaneous supplementation with calcium and 25-hydroxy vitamin D at recommended daily allowance dosage: a prospective study. Neurol India. 2010;58:213-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Panday K, Gona A, Humphrey MB. Medication-induced osteoporosis: screening and treatment strategies. Ther Adv Musculoskelet Dis. 2014;6:185-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 107] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 17. | Doğanci A, Ataman Ş, Özdemirel AE, Seçkin RB, Yalçin AP, Bavbek S. The relationship between drug-induced immunogenicity and hypersensitivity reactions and skin tests related to infliximab, etanercept and adalimumab in patients with rheumatoid arthritis and ankylosing spondylitis. Turk J Med Sci. 2024;54:1310-1318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 18. | Wang YJ, Choo WC, Ng KY, Bi R, Wang PW. Evolution of AI enabled healthcare systems using textual data with a pretrained BERT deep learning model. Sci Rep. 2025;15:7540. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Brainson CF, Huang B, Chen Q, McLouth LE, He C, Hao Z, Arnold SM, Zinner RG, Mullett TW, Bocklage TJ, Orren DK, Villano JL, Durbin EB. Description of a Lung Cancer Hotspot: Disparities in Lung Cancer Histology, Incidence, and Survival in Kentucky and Appalachian Kentucky. Clin Lung Cancer. 2021;22:e911-e920. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Hadavi SMS, Oliaei S, Saidi S, Nadimi E, Kazemi-Galougahi MH. Using Data Mining and Association Rules for Early Diagnosis of Esophageal Cancer. Gulf J Oncolog. 2022;1:38-46. [PubMed] |
| 21. | Tu L, Xiao J, Hong Q, Ouyang A, Tu Y, Wang S. Assessment of adverse events of the novel antiepileptic drug lamotrigine: a real-world pharmacovigilance study based on FAERS. Expert Opin Drug Saf. 2025;1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 22. | Vázquez-Lorente H, Herrera-Quintana L, Jiménez-Sánchez L, Fernández-Perea B, Plaza-Diaz J. Antioxidant Functions of Vitamin D and CYP11A1-Derived Vitamin D, Tachysterol, and Lumisterol Metabolites: Mechanisms, Clinical Implications, and Future Directions. Antioxidants (Basel). 2024;13:996. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 23. | Saeki N, Itoh Y, Kanai R, Itoh S, Inububishi T, Akiyama S, Inui-Yamamoto C, Abe M. Pregnane X receptor (PXR) represses osteoblast differentiation through repression of the Hedgehog signaling pathway. Exp Cell Res. 2022;416:113156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 24. | Hikmawati E, Maulidevi NU, Surendro K. Rule-ranking method based on item utility in adaptive rule model. PeerJ Comput Sci. 2022;8:e1013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | Darrab S, Broneske D, Saake G. Exploring the predictive factors of heart disease using rare association rule mining. Sci Rep. 2024;14:18178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 26. | Kebede SD, Sebastian Y, Yeneneh A, Chanie AF, Melaku MS, Walle AD. Prediction of contraceptive discontinuation among reproductive-age women in Ethiopia using Ethiopian Demographic and Health Survey 2016 Dataset: A Machine Learning Approach. BMC Med Inform Decis Mak. 2023;23:9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 27. | Firat Atay F, Yagin FH, Colak C, Elkiran ET, Mansuri N, Ahmad F, Ardigò LP. A hybrid machine learning model combining association rule mining and classification algorithms to predict differentiated thyroid cancer recurrence. Front Med (Lausanne). 2024;11:1461372. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 28. | Dabla PK, Sharma S, Mir R, Puri V. Significant Association of Antiepileptic Drug Polytherapy with Decreased FT4 Levels in Epileptic Patients. Indian J Clin Biochem. 2022;37:107-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 29. | Sengupta D, Sood M, Vijayvargia P, Hota S, Naik PK. Association rule mining based study for identification of clinical parameters akin to occurrence of brain tumor. Bioinformation. 2013;9:555-559. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 30. | Wang XP, Zhong J, Lei T, Wang HJ, Zhu LN, Chu S, Liu L. Epidemiology of traumatic brain injury-associated epilepsy in western China: An analysis of multicenter data. Epilepsy Res. 2020;164:106354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 31. | Elshorbagy HH, Barseem NF, Suliman HA, Talaat E, AlSHOKARY AH, Abdelghani WE, Abdulsamea SE, Maksoud YHA, Azab SM, Elsadek AE, Nour El Din DM. The Impact of Antiepileptic Drugs on Thyroid Function in Children with Epilepsy: New Versus Old. Iran J Child Neurol. 2020;14:31-41. [PubMed] |
| 32. | Nasir BB, Yifru YM, Engidawork E, Gebrewold MA, Woldu MA, Berha AB. Antiepileptic Drug Treatment Outcomes and Seizure-Related Injuries Among Adult Patients with Epilepsy in a Tertiary Care Hospital in Ethiopia. Patient Relat Outcome Meas. 2020;11:119-127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 33. | Cebeci D, Gurkas E, Aribas Oz N, Gungor AA, Kuruc AI, Buyukyilmaz G. The Effect of Antiseizure Medications on Thyroid Functions in Children With Epilepsy. Clin Pediatr (Phila). 2025;64:326-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 34. | Vaughan-Shaw PG, O'Sullivan F, Farrington SM, Theodoratou E, Campbell H, Dunlop MG, Zgaga L. The impact of vitamin D pathway genetic variation and circulating 25-hydroxyvitamin D on cancer outcome: systematic review and meta-analysis. Br J Cancer. 2017;116:1092-1110. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 103] [Cited by in RCA: 116] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 35. | Schöttker B, Jorde R, Peasey A, Thorand B, Jansen EH, Groot Ld, Streppel M, Gardiner J, Ordóñez-Mena JM, Perna L, Wilsgaard T, Rathmann W, Feskens E, Kampman E, Siganos G, Njølstad I, Mathiesen EB, Kubínová R, Pająk A, Topor-Madry R, Tamosiunas A, Hughes M, Kee F, Bobak M, Trichopoulou A, Boffetta P, Brenner H; Consortium on Health and Ageing: Network of Cohorts in Europe and the United States. Vitamin D and mortality: meta-analysis of individual participant data from a large consortium of cohort studies from Europe and the United States. BMJ. 2014;348:g3656. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 277] [Cited by in RCA: 303] [Article Influence: 27.5] [Reference Citation Analysis (0)] |
| 36. | Chowdhury R, Kunutsor S, Vitezova A, Oliver-Williams C, Chowdhury S, Kiefte-de-Jong JC, Khan H, Baena CP, Prabhakaran D, Hoshen MB, Feldman BS, Pan A, Johnson L, Crowe F, Hu FB, Franco OH. Vitamin D and risk of cause specific death: systematic review and meta-analysis of observational cohort and randomised intervention studies. BMJ. 2014;348:g1903. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 482] [Cited by in RCA: 430] [Article Influence: 39.1] [Reference Citation Analysis (0)] |
| 37. | Bjelakovic G, Gluud LL, Nikolova D, Whitfield K, Krstic G, Wetterslev J, Gluud C. Vitamin D supplementation for prevention of cancer in adults. Cochrane Database Syst Rev. 2014;2014:CD007469. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 93] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 38. | Kasarla SS, Garikapati V, Kumar Y, Dodoala S. Interplay of Vitamin D and CYP3A4 Polymorphisms in Endocrine Disorders and Cancer. Endocrinol Metab (Seoul). 2022;37:392-407. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 39. | Moore BF, Mueller NT, Perng W, Sauder KA, Hébert ET, Hoyt AT, Wymore EM, Boyle KE, Su EJ, Shapiro ALB, Kinney G, Sempio C, Klawitter J, Christians U, Dabelea D. Impact of prenatal exposure to delta 9-tetrahydrocannabinol and cannabidiol on birth size and postnatal growth trajectories. Pediatr Obes. 2025;20:e13187. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 40. | Fernandez H, Mohammed HT, Patel T. Vitamin D supplementation for bone health in adults with epilepsy: A systematic review. Epilepsia. 2018;59:885-896. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 41. | Wang LT, Chen LR, Chen KH. Hormone-Related and Drug-Induced Osteoporosis: A Cellular and Molecular Overview. Int J Mol Sci. 2023;24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 61] [Article Influence: 30.5] [Reference Citation Analysis (0)] |
| 42. | Shertukde SP, Cahoon DS, Prado B, Cara KC, Chung M. Calcium Intake and Metabolism in Infants and Young Children: A Systematic Review of Balance Studies for Supporting the Development of Calcium Requirements. Adv Nutr. 2022;13:1529-1553. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 43. | Al-Tameemi HK, Ibrahim N, Abdullah DAA, Oddah NN. Assessment of parathyroid hormone, vitamin D3, calcium, phosphate, and RFT in patients with chronic renal failure: A three-year follow-up study. Pol Merkur Lekarski. 2025;53:40-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 44. | Scuto M, Majzúnová M, Torcitto G, Antonuzzo S, Rampulla F, Di Fatta E, Trovato Salinaro A. Functional Food Nutrients, Redox Resilience Signaling and Neurosteroids for Brain Health. Int J Mol Sci. 2024;25:12155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 45. | Wimalawansa SJ. Infections and Autoimmunity-The Immune System and Vitamin D: A Systematic Review. Nutrients. 2023;15:3842. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 49] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 46. | Sichert-Hellert W, Kersting M. Vitamin and mineral supplements use in German children and adolescents between 1986 and 2003: results of the DONALD Study. Ann Nutr Metab. 2004;48:414-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 47. | Zeng W, Hong E, Ye W, Ma L, Cun D, Huang F, Jiang Z. Mendelian randomization of serum micronutrients and osteoarthritis risk: focus on zinc. Nutr J. 2025;24:38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 48. | Joo NS, Shin SH, Kim KN, Lee SH, Jung S, Yeum KJ. Home Meal Replacement Fortified with Eggshell Powder and Vitamin D Prevents Bone Loss in Postmenopausal Women: A Randomized, Double-Blind, Controlled Study. Nutrients. 2024;16:1152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 49. | Kim S, Yeo Y, Shin J, Shin DW, Cho B, Song YM. Factors Associated with Long-Term Dietary Supplement Use among Korean Breast Cancer Survivors: A Cross-Sectional Study. Nutrients. 2023;15:4087. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 50. | Tan N, Shen W, Tang M, Liu M, Zhang Y. Association between urine caffeine metabolites and bone mineral density: A population-based study. Medicine (Baltimore). 2023;102:e35674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 51. | Harahap IA, Kuligowski M, Cieslak A, Kołodziejski PA, Suliburska J. Effect of Tempeh and Daidzein on Calcium Status, Calcium Transporters, and Bone Metabolism Biomarkers in Ovariectomized Rats. Nutrients. 2024;16:651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 52. | Wilson-Barnes SL, Lanham-New SA, Lambert H. Modifiable risk factors for bone health & fragility fractures. Best Pract Res Clin Rheumatol. 2022;36:101758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 34] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 53. | Mehdad S, Belghiti H, Zahrou FE, Guerinech H, Mouzouni FZ, El Hajjab A, El Berri H, El Ammari L, Benaich S, Benkirane H, Barkat A, Aguenaou H. Vitamin D status and its relationship with obesity indicators in Moroccan adult women. Nutr Health. 2023;29:673-681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 54. | Erdélyi A, Pálfi E, Tűű L, Nas K, Szűcs Z, Török M, Jakab A, Várbíró S. The Importance of Nutrition in Menopause and Perimenopause-A Review. Nutrients. 2023;16:27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 33] [Reference Citation Analysis (0)] |