Published online Jan 23, 2019. doi: 10.5492/wjccm.v8.i1.1
Peer-review started: July 13, 2018
First decision: August 3, 2018
Revised: August 24, 2018
Accepted: October 17, 2018
Article in press: October 17, 2018
Published online: January 23, 2019
Processing time: 194 Days and 21.3 Hours
Expiratory flow limitation (EFL), that is the inability of expiratory flow to increase in spite of an increase of the driving pressure, is a common and unrecognized occurrence during mechanical ventilation in a variety of intensive care unit conditions. Recent evidence suggests that the presence of EFL is associated with an increase in mortality, at least in acute respiratory distress syndrome (ARDS) patients, and in pulmonary complications in patients undergoing surgery. EFL is a major cause of intrinsic positive end-expiratory pressure (PEEPi), which in ARDS patients is heterogeneously distributed, with a consequent increase of ventilation/perfusion mismatch and reduction of arterial oxygenation. Airway collapse is frequently concomitant to the presence of EFL. When airways close and reopen during tidal ventilation, abnormally high stresses are generated that can damage the bronchiolar epithelium and uncouple small airways from the alveolar septa, possibly generating the small airways abnormalities detected at autopsy in ARDS. Finally, the high stresses and airway distortion generated downstream the choke points may contribute to parenchymal injury, but this possibility is still unproven. PEEP application can abolish EFL, decrease PEEPi heterogeneity, and limit recruitment/derecruitment. Whether increasing PEEP up to EFL disappearance is a useful criterion for PEEP titration can only be determined by future studies.
Core tip: Expiratory flow limitation (EFL), the inability of expiratory flow to increase despite increasing driving pressure, is a common unrecognized occurrence during mechanical ventilation in a variety of intensive care unit conditions. It implies cyclic compression/decompression of the airways, is associated with intrinsic positive end-expiratory pressure (PEEPi) and inhomogeneous filling, and is often concomitant with cyclic recruitment/derecruitment. In acute respiratory distress syndrome, the development of abnormally high stresses is potentially injurious for the lung. External PEEP abolishes EFL and decreases ventilation and intrinsic PEEP heterogeneity, improving gas exchange. Moreover, external PEEP prevents cyclic airway collapse/reopening, possibly protecting the parenchyma from low lung volume ventilator-induced lung injury.
- Citation: Koutsoukou A, Pecchiari M. Expiratory flow-limitation in mechanically ventilated patients: A risk for ventilator-induced lung injury? World J Crit Care Med 2019; 8(1): 1-8
- URL: https://www.wjgnet.com/2220-3141/full/v8/i1/1.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v8.i1.1
Expiratory flow limitation (EFL) is present when, at a given lung volume, expiratory flow cannot be augmented by increasing the driving pressure, which is the difference between the pressure at the entrance of the respiratory system and the alveoli[1,2].
During a forced expiratory vital capacity maneuver, EFL is reached after the peak expiratory flow[3] or even during the peak[4]. When EFL is established, flow can not be increased by increasing the expiratory effort and thus is maximal[5].
In most normal subjects, EFL is absent even during maximal exercise[6]. Conversely, in patients with respiratory disorders, it may appear at moderate levels of exercise or even at rest, during tidal breathing[7].
Traditionally, in spontaneously breathing subjects, EFL has been detected by superimposing the flow-volume loop recorded during a tidal breath with that of the same loop recorded during a forced vital capacity maneuver, when the expiratory flow is maximal[8]. If the expiratory flows during tidal breathing are less than the maximal expiratory flow at each volume, tidal EFL is absent. Mead-Whittenberger’s method and the forced oscillation technique method infer the presence of EFL from the increase of alveolar pressure in front of a decreasing flow and from a within-breath difference between inspiration and expiration in terms of reactance, respectively. Both these findings are suggestive but not demonstrative of the presence of EFL[9]. A plethysmographic method for EFL detection not requiring the introduction of an esophageal balloon is under development[10].
The Hyatt’s method requires the subject’s cooperation, and it is affected by methodological problems related to gas compression and variable volume history[11]. To overcome these issues, a new method, the negative expiratory pressure (NEP) technique, was developed a few decades ago[12]. During a test breath, the driving pressure is artificially increased by the application of a small negative pressure (-5 cmH2O) during the expiration, and the resulting flow-volume trajectory is compared with one recorded without NEP application: the superimposition of the two trajectories indicates the presence of tidal EFL. The extent of EFL is quantified as the proportion of tidal volume (VT) over which the expiratory flow with and without NEP superimpose and is expressed as a percentage of the control VT[12]. The NEP technique is currently considered the gold standard for EFL detection in spontaneously breathing subjects.
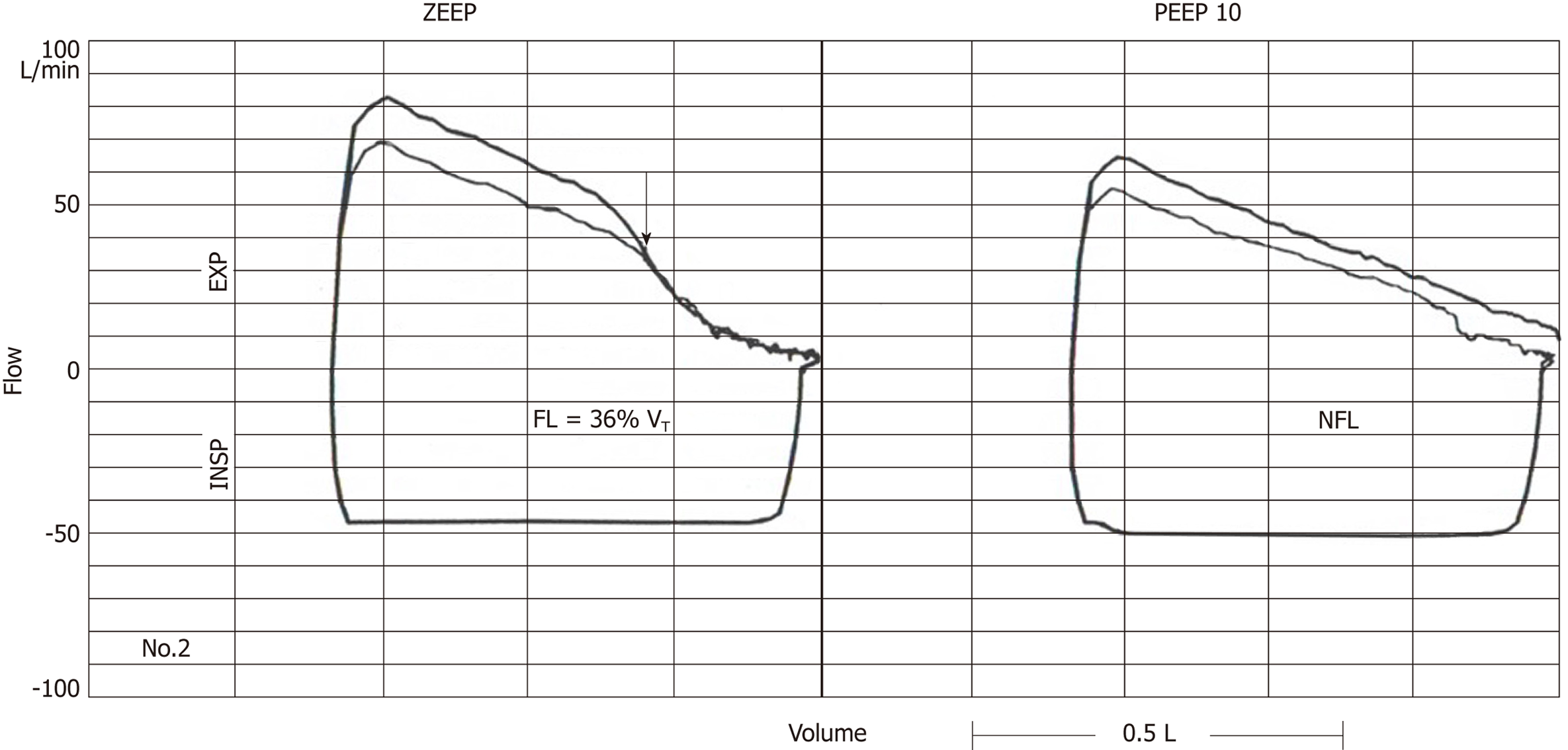
The NEP technique can also be applied to mechanically ventilated patients[12] (Figure 1), but it requires a special apparatus connected with the ventilator. A study using a fixed level of NEP rose concerns regarding the possibility that the NEP technique overestimates the extent of EFL in mechanically ventilated subjects by causing airway collapse[13], but it remains to be determined if the problem can be solved by reducing the level of NEP. Alternatively, EFL can be detected by comparing the expiratory flow-volume loops recorded with two different levels of positive end-expiratory pressure (PEEP) or with PEEP and zero end-expiratory pressure (ZEEP)[14,15]. If at a given volume expiratory flow does not change despite the change in driving pressure, EFL is present. Clearly, the last two techniques cannot be used to detect EFL in patients mechanically ventilated at ZEEP. The driving pressure for expiration can be increased by manually compressing the abdomen, as done in both spontaneously breathing[16] and mechanically ventilated subjects[17]. The interrupter technique can give indications of EFL in mechanically ventilated patients but is demanding in the clinical settings[13]. Additionally, tidal EFL can be assessed as the lack of change in the expiratory flow-volume loop after the insertion a resistance on the expiratory limb of the ventilator[13]. The so called atmosphere method consists of disconnecting the ventilator expiratory limb at end-inflation, a maneuver in patients with tidal EFL that does not elicit any effect in terms of expiratory flow-volume loop[18].
An in-depth discussion of the mechanisms responsible for the genesis of EFL may be found elsewhere[9]. Briefly, EFL may stem from two mechanisms: (1) the coupling between airways compliance and convective acceleration of gas (wave-speed theory)[19]; or (2) the coupling between airways compliance and viscous pressure losses[20]. In a normal subject, the former mechanism, non-dissipative and gas density-dependent, predominates at high lung volumes, whereas the latter, dissipative and gas viscosity-dependent, predominates at low lung volumes.
In pathological conditions, tidal EFL may occur due to a decrease of maximal expiratory flows or to an increase of the expiratory flows secondary to an increased ventilatory demand. Moreover, as maximal expiratory flows are volume-dependent (i.e., they decrease with decreasing lung volume), any decrease of lung volume facilitates the occurrence of tidal EFL.
During spontaneous breathing in the seated position, tidal EFL at rest is present in many chronic obstructive pulmonary disease (COPD)[1,2,7] and in some cystic fibrosis patients[21], conditions characterized by a marked reduction of the maximal expiratory flow. EFL has been detected in 20% of sitting patients with acute heart failure[22], while it is absent in subjects with chronic heart failure in the same position[23,24]. Reducing the ventilatory demand by increasing ventilatory efficiency may cause EFL to disappear in COPD patients[25].
On turning to supine position, the prevalence of EFL increases in COPD and acute heart failure patients[22,26], and EFL appears in chronic heart failure patients[23,24]. Positional changes markedly affect the prevalence of tidal EFL in massively obese subjects, increasing the percentage of subjects with EFL from 22 (sitting) to 59 (supine)[27].
A limited number of studies have investigated the prevalence and severity of tidal EFL in critically ill patients, but the evidence collected so far shows that tidal EFL is a common occurrence in the intensive care unit (ICU).
At ZEEP, tidal EFL is present in the majority of COPD patients requiring mechanical ventilation during an exacerbation[13,28] and in two-thirds of morbidly obese patients who had undergone abdominal surgery[29]. In the former group, tidal EFL may be attributed to the decrease of maximal expiratory flow, whereas in the latter group, the occurrence of tidal EFL should be a consequence of the reduction of functional residual capacity (FRC), compromised by anesthesia, paralysis, abdominal surgery, and supine position[30].
Similarly, the reduction of FRC after induction of anesthesia may in part explain the finding that 30% of patients undergoing major surgery exhibited tidal EFL intraoperatively[31].
Armaganidis et al[32], using the NEP technique, showed that 11 out of 13 patients with acute respiratory failure resulting from pulmonary diseases exhibited tidal EFL. A larger cohort found that about 60% of 100 patients enrolled exhibited tidal EFL at ZEEP[33].
Tidal EFL has also been detected by the NEP technique in the majority of acute respiratory distress syndrome (ARDS) patients mechanically ventilated on ZEEP[34,35]. The prevalence of tidal EFL decreases up to 20% with 5 cmH2O PEEP[18].
A study on 64 ARDS patients found that mortality at the time of discharge was greater in patients with tidal EFL (8/13) than in those without it (12/51)[18]. Moreover, the presence of EFL intraoperatively is a strong predictor of postoperative pulmonary complications[31]. Overall, these data suggest that tidal EFL may play a role in determining outcome. This suggestion is supported by the known clinical consequences of tidal EFL in the ICU settings.
Tidal EFL is associated with pulmonary hyperinflation and intrinsic PEEP (for an excellent review of the topic, see Laghi and Goyal, 2012)[36]. Hyperinflation causes alveolar overdistension, decreases compliance, and worsens diaphragm function by decreasing the zone of apposition[37]. In mechanically ventilated patients, flattening of the diaphragm may facilitate mechanical ventilation-induced diaphragmatic damage[38]. Moreover the presence of PEEPi represents a threshold inspiratory load, which the inspiratory muscles should overcome in order to produce inspiratory flow[39], making weaning difficult and contributing to patient-ventilator asynchrony[40]. Additionally, PEEPi can increase intrathoracic pressure (decreasing preload) and pulmonary vascular resistance (increasing the afterload of the right ventricle)[41], with resultant hemodynamic depression[42].
In patients with acute respiratory failure, PEEPi was on average six times greater in patients with tidal EFL than in patients without it (7.1 vs 1.2 cmH2O)[32], and significant correlations were found between PEEPi and the percentage of the VT in which EFL was present in semirecumbent and supine ARDS patients mechanically ventilated at ZEEP[34]. Similar correlations were found at ZEEP in morbidly obese subjects[29], reinforcing the notion that EFL is the major determinant of PEEPi in most clinical conditions. When PEEPi was measured in semirecumbent and supine ARDS patients, it was lower in the former than in the latter position.
In COPD patients, PEEPi may be reduced by bronchodilators[43], which cause the maximal expiratory flows to increase, reducing hyperinflation, despite the persistence of EFL[44]. To the contrary, pharmacological treatment is limited in ARDS patients[45], and thus the effects of regional or global EFL should be managed by carefully adjusting ventilator settings.
A PEEP of 10 cmH2O abolished EFL and improved arterial blood oxygenation[34] in 10 ARDS patients. Notably, the distribution of regional PEEPi was inhomogeneous in these patients, as indicated by the low ratio between dynamic PEEPi (the pressure that should be applied at the beginning of inspiration to produce the inspiratory flow, PEEPi, dyn) and static PEEPi (the pressure that can be measured after the equilibration of PEEPi in all the communicating lung units, PEEPi, st)[35], indicating that in the presence of EFL, lung emptying is non-homogeneous with consequent ventilation/perfusion mismatch and gas exchange abnormalities[35]. Actually, PEEP application resulted in a decrease of inhomogeneity of regional PEEPi, and in patients with EFL, it improved oxygenation proportionally to the increase of the ratio between PEEPi,dyn and PEEPi,st. Thus, the reduction of PEEPi inequality can be one mechanism by which the application of external PEEP to mechanically ventilated ARDS patients improves oxygenation.
The decrease of FRC and the reduction of the number of functional lung units, which are typical characteristics of the ARDS lungs, may in part explain the diminished expiratory flow reserve and, thus, the occurrence of EFL in these patients. In this regard, it should be noted that breathing at low lung volume promotes airway closure and gas trapping, with further reduction in expiratory flow reserve. Surfactant deficiency should also promote small airway closure in these patients[46,47]. In ARDS patients, the onset of EFL is heralded by a distinctive inflection on the flow-volume curve[34,35], suggesting a reduction in the number of functional units due to small airway closure. Recently, massive reopening of airspaces in ARDS patients have been documented[48], and a reopening pattern on the volume-pressure curve was noted in 11 on 13 ARDS patients with EFL (the same pattern was present in only 10 on 52 patients without EFL)[18]. Note that if a substantial number of units are not in communication with the central airways, PEEPi,st underestimates the average alveolar pressure at end-expiration[48].
Cyclic opening and closing of airspaces during tidal ventilation has several detrimental effects on the lungs in addition to worsened ventilation/perfusion mismatch. In 1984, Robertson et al[49] suggested that ventilation at low lung volume may cause lung injury as a result of shear stresses caused by cyclic opening and closing of peripheral airways. This idea was later substantiated by Muscadere and coworkers[50], who, in an ex vivo model of lavaged rat lung, demonstrated that ventilation with physiologic VT at ZEEP resulted in a significant increase of the injury scores of respiratory and membranous bronchioles relative to ventilation from a PEEP above the lower inflection point on the static inflation pressure-volume curve of the lung. Subsequent experimental research showed that surfactant deficiency is not a prerequisite for this kind of injury, which was also detected in normal open-chest or closed-chest rabbits and rats ventilated with physiological VT below FRC[51-54]. These studies confirmed that ventilation at low lung volume causes epithelial necrosis and sloughing at the bronchial level. Moreover, they showed in the same condition that alveolar-parenchymal uncoupling is produced, that is rupture of the alveolar walls connected to the outer surface of bronchioles, probably as the result of abnormal stresses developing in the heterogeneous parenchyma. Indeed, when aerated lung areas are adjacent to collapsed ones, they function as stress-concentrators, generating excessive strain at the interface between collapsed and expanded alveoli[55]. Bronchiolar and parenchymal damage was associated with leukocytes recruitment in the alveolar septa[52]. Low volume mechanical ventilation has been found to induce transient ruptures of the cell membrane at the level of bronchioles and alveolar septa, with the number of bronchiolar lesions correlating with the increase of airway resistance[56].
All these phenomena may be relevant in mechanically ventilated ARDS because of the reduction of FRC and the gross mechanical heterogeneity of the lung parenchyma. Not surprisingly, small airway abnormalities in ARDS have been confirmed in autopsy studies[57].
Finally, the potential role of tidal EFL in eliciting ventilator-induced lung injury remains a concern.
When EFL develops, choke points appear that move along the tracheobronchial tree as the lung volume decreases. At the choke points, cross-section is small, and velocity is high. Downstream the choke points, the cross-section may further decrease, velocity may become supercritical, and the excess of energy be dissipated in a region where the cross-section suddenly increases together with lateral pressure[9]. Moreover, in the same region, flutter can appear[9]. Are the shear stresses and local deformations so generated sufficiently high to damage lung parenchyma? To the best of our knowledge, there have been no experimental studies specifically aimed to demonstrate a direct injurious effect elicited by this mechanism independently of parenchymal heterogeneity and airway collapse. However, some evidence suggests that this possibility is worth investigating. Indeed, a modeling study showed that heterogeneous narrowing of small airways can amplify several-fold shear stress on the epithelial layer of the airways[58], and, during mechanical ventilation with physiological VT and normal end-expiratory lung volume, parenchymal distortion by itself is able to elicit an inflammatory response in normal animals[59].
In conclusion, EFL during tidal breathing is a frequent occurrence in the ICU. It implies cyclic compression/decompression of the airways, and it is often associated with cyclic recruitment/derecruitment together with inhomogeneous filling of airspaces. In ARDS lungs, this probably entails the development of abnormally high stresses with the risk of low lung volume injury[34,35]. This risk may not be confined to ARDS but could be present in all patients who exhibit EFL during mechanical ventilation, such as morbidly obese patients[29]. The application of external PEEP abolishes EFL[34], improving lung emptying and decreasing the heterogeneity of ventilation distribution and of PEEPi, with a resultant improvement in gas exchange[35]. Even if the NEP technique is no longer available as a clinical tool, EFL can be easily detected in the ICU using simpler methods, such as comparing the expiratory flow-volume loops recorded with two different levels of PEEP or the atmosphere method. Detection of tidal EFL in the ICU may not be of only prognostic value: for example, increasing the external PEEP until the disappearance of tidal EFL may become a useful complementary procedure of PEEP optimization. Only more experimental studies can establish if the prompt recognition of tidal EFL can be useful to optimize the management of patients under mechanical ventilation and improve the outcome.
Manuscript source: Invited manuscript
Specialty type: Critical care medicine
Country of origin: Greece
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Drabek T, Santomauro M, Willms DC S- Editor: Dou Y L- Editor: Filipodia E- Editor: Bian YN
| 1. | Eltayara L, Becklake MR, Volta CA, Milic-Emili J. Relationship between chronic dyspnea and expiratory flow limitation in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1996;154:1726-1734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 179] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 2. | Koulouris NG, Dimopoulou I, Valta P, Finkelstein R, Cosio MG, Milic-Emili J. Detection of expiratory flow limitation during exercise in COPD patients. J Appl Physiol (1985). 1997;82:723-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 87] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 3. | HYATT RE, SCHILDER DP, FRY DL. Relationship between maximum expiratory flow and degree of lung inflation. J Appl Physiol. 1958;13:331-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 187] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Tantucci C, Duguet A, Giampiccolo P, Similowski T, Zelter M, Derenne JP. The best peak expiratory flow is flow-limited and effort-independent in normal subjects. Am J Respir Crit Care Med. 2002;165:1304-1308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Volta CA, Ploysongsang Y, Eltayara L, Sulc J, Milic-Emili J. A simple method to monitor performance of forced vital capacity. J Appl Physiol (1985). 1996;80:693-698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Mota S, Casan P, Drobnic F, Giner J, Ruiz O, Sanchis J, Milic-Emili J. Expiratory flow limitation during exercise in competition cyclists. J Appl Physiol (1985). 1999;86:611-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 42] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | D’Angelo E, Santus P, Civitillo MF, Centanni S, Pecchiari M. Expiratory flow-limitation and heliox breathing in resting and exercising COPD patients. Respir Physiol Neurobiol. 2009;169:291-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | HYATT RE. The interrelationships of pressure, flow, and volume during various respiratory maneuvers in normal and emphysematous subjects. Am Rev Respir Dis. 1961;83:676-683. [PubMed] |
| 9. | Pedersen OF, Butler JP. Expiratory flow limitation. Compr Physiol. 2011;1:1861-1882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 10. | Radovanovic D, Pecchiari M, Pirracchio F, Zilianti C, D’Angelo E, Santus P. Plethysmographic Loops: A Window on the Lung Pathophysiology of COPD Patients. Front Physiol. 2018;9:484. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Calverley PM, Koulouris NG. Flow limitation and dynamic hyperinflation: key concepts in modern respiratory physiology. Eur Respir J. 2005;25:186-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 134] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 12. | Valta P, Corbeil C, Lavoie A, Campodonico R, Koulouris N, Chassé M, Braidy J, Milic-Emili J. Detection of expiratory flow limitation during mechanical ventilation. Am J Respir Crit Care Med. 1994;150:1311-1317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 107] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 13. | Lourens MS, Berg BV, Hoogsteden HC, Bogaard JM. Detection of flow limitation in mechanically ventilated patients. Intensive Care Med. 2001;27:1312-1320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Rossi A, Polese G, Milic-Emili J. Monitoring respiratory mechanics in ventilator-dependent patients. In: Tobin MJ. Principles and practice of intensive care monitoring. New York: McGraw-Hill 1998; 597-616. |
| 15. | Marangoni E, Alvisi V, Ragazzi R, Mojoli F, Alvisi R, Caramori G, Astolfi L, Volta CA. Respiratory mechanics at different PEEP level during general anesthesia in the elderly: a pilot study. Minerva Anestesiol. 2012;78:1205-1214. [PubMed] |
| 16. | Ninane V, Leduc D, Kafi SA, Nasser M, Houa M, Sergysels R. Detection of expiratory flow limitation by manual compression of the abdominal wall. Am J Respir Crit Care Med. 2001;163:1326-1330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Lemyze M, Favory R, Alves I, Perez T, Mathieu D. Manual compression of the abdomen to assess expiratory flow limitation during mechanical ventilation. J Crit Care. 2012;27:37-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Yonis H, Mortaza S, Baboi L, Mercat A, Guérin C. Expiratory Flow Limitation Assessment in Patients with Acute Respiratory Distress Syndrome. A Reappraisal. Am J Respir Crit Care Med. 2018;198:131-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 19. | Dawson SV, Elliott EA. Wave-speed limitation on expiratory flow-a unifying concept. J Appl Physiol Respir Environ Exerc Physiol. 1977;43:498-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 196] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 20. | Shapiro AH. Steady flow in collapsible tubes. J Biomech Eng. 1977;99:126-147. [RCA] [DOI] [Full Text] [Cited by in Crossref: 309] [Cited by in RCA: 315] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 21. | Goetghebeur D, Sarni D, Grossi Y, Leroyer C, Ghezzo H, Milic-Emiri J, Bellet M. Tidal expiratory flow limitation and chronic dyspnoea in patients with cystic fibrosis. Eur Respir J. 2002;19:492-498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 22. | Duguet A, Tantucci C, Lozinguez O, Isnard R, Thomas D, Zelter M, Derenne JP, Milic-Emili J, Similowski T. Expiratory flow limitation as a determinant of orthopnea in acute left heart failure. J Am Coll Cardiol. 2000;35:690-700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 42] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 23. | Pecchiari M, Anagnostakos T, D’Angelo E, Roussos C, Nanas S, Koutsoukou A. Effect of heliox breathing on flow limitation in chronic heart failure patients. Eur Respir J. 2009;33:1367-1373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 24. | Torchio R, Gulotta C, Greco-Lucchina P, Perboni A, Avonto L, Ghezzo H, Milic-Emili J. Orthopnea and tidal expiratory flow limitation in chronic heart failure. Chest. 2006;130:472-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Theodorakopoulou EP, Gennimata SA, Harikiopoulou M, Kaltsakas G, Palamidas A, Koutsoukou A, Roussos C, Kosmas EN, Bakakos P, Koulouris NG. Effect of pulmonary rehabilitation on tidal expiratory flow limitation at rest and during exercise in COPD patients. Respir Physiol Neurobiol. 2017;238:47-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 26. | Pecchiari M, Pelucchi A, D’Angelo E, Foresi A, Milic-Emili J, D’Angelo E. Effect of heliox breathing on dynamic hyperinflation in COPD patients. Chest. 2004;125:2075-2082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 27. | Ferretti A, Giampiccolo P, Cavalli A, Milic-Emili J, Tantucci C. Expiratory flow limitation and orthopnea in massively obese subjects. Chest. 2001;119:1401-1408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 117] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 28. | Alvisi V, Romanello A, Badet M, Gaillard S, Philit F, Guérin C. Time course of expiratory flow limitation in COPD patients during acute respiratory failure requiring mechanical ventilation. Chest. 2003;123:1625-1632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 29. | Koutsoukou A, Koulouris N, Bekos B, Sotiropoulou C, Kosmas E, Papadima K, Roussos C. Expiratory flow limitation in morbidly obese postoperative mechanically ventilated patients. Acta Anaesthesiol Scand. 2004;48:1080-1088. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 27] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 30. | Hedenstierna G, Strandberg A, Brismar B, Lundquist H, Svensson L, Tokics L. Functional residual capacity, thoracoabdominal dimensions, and central blood volume during general anesthesia with muscle paralysis and mechanical ventilation. Anesthesiology. 1985;62:247-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 232] [Cited by in RCA: 161] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 31. | Spadaro S, Caramori G, Rizzuto C, Mojoli F, Zani G, Ragazzi R, Valpiani G, Dalla Corte F, Marangoni E, Volta CA. Expiratory Flow Limitation as a Risk Factor for Pulmonary Complications After Major Abdominal Surgery. Anesth Analg. 2017;124:524-530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 32. | Armaganidis A, Stavrakaki-Kallergi K, Koutsoukou A, Lymberis A, Milic-Emili J, Roussos C. Intrinsic positive end-expiratory pressure in mechanically ventilated patients with and without tidal expiratory flow limitation. Crit Care Med. 2000;28:3837-3842. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 33. | Natalini G, Tuzzo D, Rosano A, Testa M, Grazioli M, Pennestrì V, Amodeo G, Berruto F, Fiorillo M, Peratoner A, Tinnirello A, Filippini M, Marsilia PF, Minelli C, Bernardini A; VENTILAB group. Effect of external PEEP in patients under controlled mechanical ventilation with an auto-PEEP of 5 cmH2O or higher. Ann Intensive Care. 2016;6:53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 34. | Koutsoukou A, Armaganidis A, Stavrakaki-Kallergi C, Vassilakopoulos T, Lymberis A, Roussos C, Milic-Emili J. Expiratory flow limitation and intrinsic positive end-expiratory pressure at zero positive end-expiratory pressure in patients with adult respiratory distress syndrome. Am J Respir Crit Care Med. 2000;161:1590-1596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 70] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 35. | Koutsoukou A, Bekos B, Sotiropoulou C, Koulouris NG, Roussos C, Milic-Emili J. Effects of positive end-expiratory pressure on gas exchange and expiratory flow limitation in adult respiratory distress syndrome. Crit Care Med. 2002;30:1941-1949. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 61] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 36. | Laghi F, Goyal A. Auto-PEEP in respiratory failure. Minerva Anestesiol. 2012;78:201-221. [PubMed] |
| 37. | Laghi F, Tobin MJ. Disorders of the respiratory muscles. Am J Respir Crit Care Med. 2003;168:10-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 384] [Cited by in RCA: 359] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 38. | Ottenheijm CA, Heunks LM, Dekhuijzen PN. Diaphragm muscle fiber dysfunction in chronic obstructive pulmonary disease: toward a pathophysiological concept. Am J Respir Crit Care Med. 2007;175:1233-1240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 89] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 39. | Smith TC, Marini JJ. Impact of PEEP on lung mechanics and work of breathing in severe airflow obstruction. J Appl Physiol (1985). 1988;65:1488-1499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 342] [Cited by in RCA: 260] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 40. | Thille AW, Rodriguez P, Cabello B, Lellouche F, Brochard L. Patient-ventilator asynchrony during assisted mechanical ventilation. Intensive Care Med. 2006;32:1515-1522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 496] [Cited by in RCA: 496] [Article Influence: 26.1] [Reference Citation Analysis (0)] |
| 41. | Gottfried SB. The role of PEEP in the mechanically ventilated COPD patient. In: Roussos C, Marini JJ. Ventilatory failure. Berlin: Springer 1991; 392-418. [RCA] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 42. | Pepe PE, Marini JJ. Occult positive end-expiratory pressure in mechanically ventilated patients with airflow obstruction: the auto-PEEP effect. Am Rev Respir Dis. 1982;126:166-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 56] [Reference Citation Analysis (0)] |
| 43. | Dal Vecchio L, Polese G, Poggi R, Rossi A. “Intrinsic” positive end-expiratory pressure in stable patients with chronic obstructive pulmonary disease. Eur Respir J. 1990;3:74-80. [PubMed] |
| 44. | Tantucci C, Duguet A, Similowski T, Zelter M, Derenne JP, Milic-Emili J. Effect of salbutamol on dynamic hyperinflation in chronic obstructive pulmonary disease patients. Eur Respir J. 1998;12:799-804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 112] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 45. | Boyle AJ, Mac Sweeney R, McAuley DF. Pharmacological treatments in ARDS; a state-of-the-art update. BMC Med. 2013;11:166. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 95] [Cited by in RCA: 109] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 46. | Eissa NT, Milic-Emili J, Pochen EJ, Granier EG, Green E. Effects of positive end-expiratory pressure in adult respiratory distress syndrome. Pochen EJ, Granier EG, Green E. Pulmonary radiology. Boston: The Fleischner Society 1993; 169-178. |
| 47. | D’Angelo E, Pecchiari M, Gentile G. Dependence of lung injury on surface tension during low-volume ventilation in normal open-chest rabbits. J Appl Physiol (1985). 2007;102:174-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 48. | Chen L, Del Sorbo L, Grieco DL, Shklar O, Junhasavasdikul D, Telias I, Fan E, Brochard L. Airway Closure in Acute Respiratory Distress Syndrome: An Underestimated and Misinterpreted Phenomenon. Am J Respir Crit Care Med. 2018;197:132-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 119] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 49. | Robertson B. Lung surfactant. In: Robertson B, Van Golde L, Batenbourg J. Pulmonary surfactant. Amsterdam: Elsevier 1984; 384-417. |
| 50. | Muscedere JG, Mullen JB, Gan K, Slutsky AS. Tidal ventilation at low airway pressures can augment lung injury. Am J Respir Crit Care Med. 1994;149:1327-1334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 862] [Cited by in RCA: 745] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 51. | D’Angelo E, Pecchiari M, Baraggia P, Saetta M, Balestro E, Milic-Emili J. Low-volume ventilation causes peripheral airway injury and increased airway resistance in normal rabbits. J Appl Physiol (1985). 2002;92:949-956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 94] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 52. | D’Angelo E, Pecchiari M, Saetta M, Balestro E, Milic-Emili J. Dependence of lung injury on inflation rate during low-volume ventilation in normal open-chest rabbits. J Appl Physiol (1985). 2004;97:260-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 53] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 53. | D’Angelo E, Pecchiari M, Della Valle P, Koutsoukou A, Milic-Emili J. Effects of mechanical ventilation at low lung volume on respiratory mechanics and nitric oxide exhalation in normal rabbits. J Appl Physiol (1985). 2005;99:433-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 50] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 54. | D’Angelo E, Koutsoukou A, Della Valle P, Gentile G, Pecchiari M. Cytokine release, small airway injury, and parenchymal damage during mechanical ventilation in normal open-chest rats. J Appl Physiol (1985). 2008;104:41-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 37] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 55. | Retamal J, Bergamini BC, Carvalho AR, Bozza FA, Borzone G, Borges JB, Larsson A, Hedenstierna G, Bugedo G, Bruhn A. Non-lobar atelectasis generates inflammation and structural alveolar injury in the surrounding healthy tissue during mechanical ventilation. Crit Care. 2014;18:505. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 68] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 56. | Pecchiari M, Monaco A, Koutsoukou A, D’Angelo E. Plasma membrane disruptions with different modes of injurious mechanical ventilation in normal rat lungs*. Crit Care Med. 2012;40:869-875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 57. | Morales MM, Pires-Neto RC, Inforsato N, Lanças T, da Silva LF, Saldiva PH, Mauad T, Carvalho CR, Amato MB, Dolhnikoff M. Small airway remodeling in acute respiratory distress syndrome: a study in autopsy lung tissue. Crit Care. 2011;15:R4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 56] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 58. | Nucci G, Suki B, Lutchen K. Modeling airflow-related shear stress during heterogeneous constriction and mechanical ventilation. J Appl Physiol (1985). 2003;95:348-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 62] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 59. | Pecchiari M, Monaco A, Koutsoukou A, Della Valle P, Gentile G, D’Angelo E. Effects of various modes of mechanical ventilation in normal rats. Anesthesiology. 2014;120:943-950. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |