Published online May 4, 2017. doi: 10.5492/wjccm.v6.i2.116
Peer-review started: November 13, 2016
First decision: December 1, 2016
Revised: December 18, 2016
Accepted: January 11, 2017
Article in press: January 13, 2017
Published online: May 4, 2017
Processing time: 172 Days and 14.4 Hours
To study the early postoperative intensive care unit (ICU) management and complications in the first 2 wk of patients undergoing cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC).
Our study is a retrospective, observational study performed at Icahn School of Medicine at Mount Sinai, quaternary care hospital in New York City. All adult patients who underwent CRS and HIPEC between January 1, 2007 and December 31, 2012 and admitted to ICU postoperatively were studied. Fifty-one patients came to the ICU postoperatively out of 170 who underwent CRS and HIPEC therapy during the study period. Data analysis was performed using descriptive statistics.
Of the 170 patients who underwent CRS and HIPEC therapy, 51 (30%) came to the ICU postoperatively. Mean ICU length of stay was 4 d (range 1-60 d) and mean APACHE II score was 15 (range 7-23). Thirty-one/fifty-one (62%) patients developed postoperative complications. Aggressive intraoperative and postoperative fluid resuscitation is required in most patients. Hypovolemia was seen in all patients and median amount of fluids required in the first 48 h was 6 L (range 1-14 L). Thirteen patients (25%) developed postoperative hypotension with seven requiring vasopressor support. The major cause of sepsis was intraabdominal, with 8 (15%) developing anastomotic leaks and 5 (10%) developing intraabdominal abscess. The median survival was 14 mo with 30 d mortality of 4% (2/51) and 90 d mortality of 16% (8/51). One year survival was 56.4% (28/51). Preoperative medical co morbidities, extent of surgical debulking, intraoperative blood losses, amount of intra op blood products required and total operative time are the factors to be considered while deciding ICU vs non ICU admission.
Overall, ICU outcomes of this study population are excellent. Triage of these patients should consider preoperative and intraoperative factors. Intensivists should be vigilant to aggressive postop fluid resuscitation, pain control and early detection and management of surgical complications.
Core tip: Our retrospective study highlights the intensive care unit (ICU) management, complications and outcomes of patients undergoing complicated hyperthermic intraperitoneal chemotherapy procedure for peritoneal carcinomatosis. Intensivists need to monitor for physiologic derangements post procedure and assess fluid status, provide adequate pain control and have high degree of suspicion for complications like abdominal sepsis. Not all patients need ICU admission post procedure. Our study enlists the factors to be considered for ICU admission vs the floor.
- Citation: Kapoor S, Bassily-Marcus A, Alba Yunen R, Tabrizian P, Semoin S, Blankush J, Labow D, Oropello J, Manasia A, Kohli-Seth R. Critical care management and intensive care unit outcomes following cytoreductive surgery with hyperthermic intraperitoneal chemotherapy. World J Crit Care Med 2017; 6(2): 116-123
- URL: https://www.wjgnet.com/2220-3141/full/v6/i2/116.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v6.i2.116
Malignant peritoneal surface disease, commonly known as peritoneal carcinomatosis (PC) has been considered to be incurable with poor median survival of six months without treatment[1,2]. Cytoreductive surgery (CRS) combined with perioperative hyperthermic intraperitoneal chemotherapy (HIPEC) has been confirmed as a viable treatment option for peritoneal based tumors in 1980s. Today, CRS and HIPEC therapy is used in select patients for treatment of PC from gastric cancer, colorectal cancer, appendiceal cancer, ovarian cancer and primary peritoneal malignancies like mesotheliomas. Few randomized controlled trials have been conducted and demonstrated better survival in patients undergoing CRS-HIPEC in the treatment of colorectal PC compared to systemic chemotherapy alone[3-5]. Multiple nonrandomized single and multicenter phase II and few phase III trials indicate that CRS and HIPEC may improve survival rate for selected patients with peritoneal metastasis[2,6-8]. There has been an observed increase in survival rates with CRS and HIPEC in colorectal cancer, advanced ovarian cancer, gastric cancer and peritoneal mesothelioma[9-14]. This procedure is technically challenging and has the potential for increased morbidity and mortality[15]. The morbidity and mortality rates reported have ranged from 12%-52% and 0.9%-5.8% respectively at large tertiary hospitals with a high volume of oncology patients[2]. Recent largest reported single center study demonstrated that major prognostic factors include primary site, performance status, completeness of resection and institutional experience[16]. In a recent study, 40% of patients developed at least one postoperative in hospital complication[17]. One serious complication related to HIPEC is peritoneal inflammation and systemic inflammatory response syndrome (SIRS) which leads to physiologic changes in different organ systems. Effects on the cardiovascular status, oxygen consumption and hematopoietic parameters of patients have been described in the literature and have been observed in practice[18-21]. The complexity of perioperative anesthetic management of these patients with particular attention to perioperative fluid, pain management and the patient’s coagulation status has been reported in the anesthesiology literature[22,23]. The extensive peritoneal inflammation and the inflammatory response impacts the early postoperative intensive care unit (ICU) course of this patient population. In the present study, we describe the early (first two weeks) postoperative ICU management, long-term morbidity and mortality (day 30 and day 90) of patients admitted to the ICU after undergoing CRS and HIPEC therapy retrospectively over a six years period.
This retrospective descriptive study was conducted in a 14-bed surgical intensive care unit (SICU) in a large tertiary hospital. With Institutional Review Board approval, all adult patients over 18 years of age who underwent CRS and HIPEC therapy between January 1, 2007 and December 31, 2012 were screened for enrollment in the study (n = 170). Of this, 51 patients were admitted to the SICU postoperatively and were included in the study. Data for this retrospective analysis were retrieved from medical records, operative reports, laboratory and radiologic data. Early (first two weeks) postoperative ICU course, ICU management and long-term surgical morbidity and mortality (day 30 and day 90) were retrospectively studied.
CRS and HIPEC surgery was performed with closed technique and cisplatin and mitomycin C were the chemotherapy agents administered. Patients were often immediately extubated and transferred to the surgical floor. Standard criteria for extubation were used by anesthesiology team including mental status assessment, reversal of muscular paralysis and anesthesia, hemodynamic stability and adequate oxygenation and ventilation in addition to intraoperative course and complications. If they were hemodynamically unstable in OR with mean arterial pressure (MAP) less than 65 mmHg and/or systolic blood pressure (SBP) less than 90 mmHg requiring intravenous fluids and vasopressor support, remained on mechanical ventilation or required higher level of care based on intraoperative course, they were admitted to SICU. This was determined by the anesthesia, surgical and critical care teams. At the initial stages of experience with the HIPEC procedure at our center, all patients came to SICU post operatively. With our growing experience, we became more selective in admitting patients to ICU postoperatively.
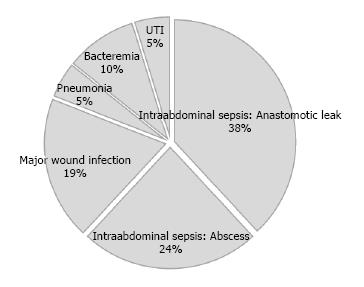
In the present study, 51 out of 170 patients came to the ICU postoperatively. The primary diagnosis was PC secondary to metastatic colon, appendiceal, gastric, mesothelial and ovarian tumors. Median ICU length of stay (LOS) was 4 d (range 1-60 d) and median APACHE II scores was 15 (range 7-23) (Table 1). Twenty-two patients (43%) received postop epidural analgesia by the anesthesia team. Of the patients admitted to the ICU, 31 (62%) had observed post-operative complications. Twenty-nine patients (57%) needed up to 10 L of fluids intraoperatively for hemodynamic instability and fluid/blood losses. All patients were hypovolemic postoperatively in the ICU and required intravenous fluids. Median amount of intravenous fluids required in the first 48 h was 6 L (range 1-14 L). Assessment of hypovolemia was done by clinical exam, hemodynamic monitoring with pulse contour analysis and using standard bedside ultrasonography by assessing cardiac chambers and inferior vena cava. Post-operative complications are listed in Table 2. Postoperative hypotension developed in 13 patients (25%), out of which, 7 (13%) developed septic shock requiring vasopressor support. Acute respiratory failure, defined as requirement of mechanical ventilation for more than 48 h was seen in 18 patients (33%). Five patients (10%) developed acute renal failure but none required renal replacement therapy during their ICU course. Seventeen (25%) patients developed abdominal sepsis including anastomotic leak in eight patients (15%), intra abdominal abscess in five patients (10%) and deep wound infection in four (8%) (Figure 1). There were no Central line-associated bloodstream infections (CLABSIs). Total parenteral nutrition (TPN) was initiated in 9 (18%) patients. Median survival was 14 mo. Thirty-day mortality was 4% (2 patients) and 90 d mortality was 16% (8 patients). One year survival was 56.4% (28/51). We also performed sub group analysis of patients admitted to ICU and those admitted to the surgical floor postoperatively (Table 3). Variables like preoperative co morbidities (high ASA scores), extent of surgical debulking (number of organs resected), amount of blood products required intraoperatively, estimated blood loss, total OR time showed statistically significant difference between ICU and non ICU patients. ICU patients had increased postoperative morbidity and hospital LOS compared to non ICU patients. There was no statistically significant difference in 30 and 90 d mortality between these two sub group of patients.
| Variable | n = 51 |
| Age (yr) | 56 (18-82) |
| Gender | |
| Female | 27 (53%) |
| APACHE II | 15 (7-23) |
| ICU LOS (d) | 4 (1-60) |
| Operative time (min) | 413 (65-815) |
| Primary site | |
| Colon | 19 |
| Appendix | 12 |
| Gastric | 6 |
| Ovarian | 3 |
| Pseudomyxoma peritoneii | 6 |
| Mesothelial | 3 |
| Others | 2 |
| EBL (mL) | 1125 (50-6500) |
| Peritoneal cancer index (intraop) | 13 (3-35) |
| Complication | n = 51 |
| Acute respiratory failure | 18 (33) |
| Postoperative hypovolemia | 51 (100) |
| Postoperative hypotension | 13 (25) |
| Septic shock | 7 (13) |
| Reintubation | 6 (12) |
| Acute blood loss anemia | 18 (33) |
| Pulmonary embolism | 4 (8) |
| Acute renal failure | 5 (10) |
| Tracheostomy | 4 (8) |
| Dilutional coagulopathy | 28 (55) |
| Hypoalbuminemia | 51 (100) |
| Arrythmias | 2 (3) |
| CLABSI | 0 (0) |
| ICU delirium | 3 (6) |
| Surgical complications | |
| Anastomotic leaks | 8 (15) |
| Anastomotic leaks requiring OR | 5 |
| Intra abdominal abscess | 5 (10) |
| Intra abdominal abscess requiring IR drainage | 4 |
| Surgical bleeding | 4 (8) |
| Deep wound infection | 4 (8) |
| Abdominal sepsis: Anastomotic leak, abscess, deep wound infection | 17 (33) |
| Bacteremia | 2 (3) |
| Postoperative parenteral nutrition | 9 (18) |
| Variable, n (%) | ICU group | Non ICU group | P value |
| n = 51 | n =119 | ||
| Age, mean (SD) | 56.6 (12.8) | 54.5 (10.5) | 0.282 |
| ASA, mean (SD) | 3.1 (0.6) | 2.8 (0.5) | 0.009 |
| ASA, > 3 (%) | 12 (24) | 8 (6.7) | < 0.001 |
| Intraop PCI, mean (SD) | 21.5 (8.4) | 13.7 (8.3) | < 0.001 |
| Change in PCI, mean (SD) | 16.2 (7.1) | 10.7 (6.1) | < 0.001 |
| No. of resected organs: Mean (SD) | 5.9 (2.2) | 3.1 (2.1) | < 0.001 |
| EBL, mean (SD) | 1505 (1408) | 423 (519) | < 0.001 |
| Intraop transfusion (%) | 45 (90) | 26 (21.7) | < 0.001 |
| OR time, min, mean (SD) | 456 (122) | 328 (118) | < 0.001 |
| Mortality at | |||
| 30 d (%) | 2 (4) | 2 (1.7) | 0.36 |
| 90 d (%) | 8 (12) | 6 (5) | 0.104 |
| Hospital stay, mean (range) | 18 (5-88) | 8.6 (3-101) | < 0.001 |
| Survival, mo: Median (SE) | 14 (1.8) | 33.4 (5.3) | < 0.001 |
| Readmission rate to ICU (%) | 6/51 (12) | 3/119 (2.5) | 0.01 |
There has been a renewed interest in the field of peritoneal surface malignancies over the last 15-20 years, mainly due to the better understanding of the biology of these tumors with intraperitoneal spread and without systemic metastasis. CRS and HIPEC has evolved into a novel treatment approach in patients with PC secondary to colorectal, appendiceal, ovarian, gastric and primary peritoneal malignancies. The purpose of CRS is the performance of complete or near complete cytoreduction. The purpose of HIPEC administration is the eradication of the microscopic residual tumor. HIPEC is effective in eradicating cancer emboli less than 3 mm in their largest diameter. Hyperthermia leads to direct cytotoxic effects and also increases the depth of penetration of chemotherapy agents[24]. Intraperitoneal loco-regional chemotherapy achieves high local concentration of cytotoxic agents due to the peritoneal-plasma barrier[24]. Completeness of cytoreduction is the most important determinant of outcome after surgery[4,6,25-27].
The procedure is lengthy and involves extensive surgical debulking. Aggressive resuscitation with fluids and blood transfusions are usually required intraoperatively due to blood losses and fluid shifts[22,23]. The current study found approximately 60% of patients required up to 10 L of fluid replacement and up to 5 units of PRBC transfusion intraoperatively. These findings corroborate previous research that found aggressive intraoperative and postop fluid resuscitation in this patient population[22,23,27].
In our study, 31% (51/170) of patients who underwent HIPEC were admitted to the ICU for postoperative management, requirement for mechanical ventilation and overall morbid condition. Previous studies reported a higher percentage (67%-100%) of patients admitted to the ICU postoperatively[22,28,29]. The mean ICU LOS in this patient population was also similar to the previous studies (≤ 5 d)[6,29]. Less than 50% of our patients (22/51) received postoperative epidural analgesia which is significantly less than what is reported in the current literature[6,25]. Hypovolemia is very common in the postoperative period which is exacerbated by fluid losses from peritoneal surface. All of our patients required aggressive postop fluid resuscitation, range 1-14 L, median 6 L. Patients develop systemic vasodilation due to intense SIRS response, leading to hypotension, tachycardia and needing vasopressor support. Standard recommended doses of vasopressors were used, norepinephrine (0-35 mcg/min), vasopressin (0.04 units/min, nontitratable), epinephrine (0-35 mcg/min) and phenylephrine (0-300 mcg/min). Norepinephrine was the vasopressor of choice. Cooksley et al[27] reported 26% patients requiring vasopressors in postoperative period. Most uncomplicated cases are usually extubated within 24 h of the procedure. Up to 33% of patients in our series required postop mechanical ventilation for more than 48 h. The major reasons for respiratory failure in the postsurgical period included acute lung injury or noncardiogenic pulmonary edema due to systemic inflammatory response, fluid overload, aspiration, pneumonia, pulmonary embolism and atelectasis. Our findings are different from previous studies which reported all patients were extubated prior to ICU arrival (Cooksley et al[27]) and a majority of patients were extubated within 3 h of ICU arrival (Schmidt et al[22,23]). The extended mechanical ventilation in the current study can be explained by the level of critical illness in this patient population.
Coagulopathy is commonly seen due to the effects of massive fluid resuscitation, blood transfusion or chemotherapy induced myelosuppression[29]. In our study, 55% patients had coagulopathy defined by INR > 1.5 and or platelet count less than 100000 and 35% required postoperative blood transfusion. This is consistent with previous studies[22,27].
These patients are predisposed to develop perioperative venous thromboembolism. Reported incidence for venous thromboembolism varies between 5%-10% in literature[30-32]. We report 4 cases of postoperative pulmonary embolism in patients admitted to ICU in our series despite being on DVT prophylaxis. Postoperative hypoalbuminemia is a common finding and is not indicative of nutritional status, rather dilutional effect as well as suppression of synthesis due to cytokine release being one of the negative acute phase reactant[33]. Other ICU complications like acute renal failure, bacteremia, arrhythmias and reintubation were seen in this patient population. Of the patients who developed acute renal failure, none required renal replacement therapy. Nobody developed catheter associated bloodstream infection[27-30]. These findings are similar to other studies reported in literature.
Reported morbidity and mortality in the literature is 12%-52% and 0.9%-5.8% respectively at high volume centers[6,15,34-39]. Septic shock and multisystem organ failure is the leading cause of mortality in patients undergoing CRS and HIPEC[2,40]. This is likely attributable to the extensive nature of this procedure, immunosuppression due to previous chemotherapy and the development of surgical complications.
The major surgical complications reported are anastomotic leaks (0%-9%), intraabdominal abscesses (0%-37%), intestinal perforation/peritonitis (0%-10%), fistulas (0%-23%) and prolonged ileus (0%-86%). Intraabdominal bleeding, bile leaks, pancreatitis, major wound infections, acalculous cholecystitis, mesenteric ischemia, mechanical intestinal obstruction are other surgical complications reported[2,4,31,41-43]. The reoperation rates following the procedure for various complications range from 0%-23%[2].
Nutrition is a very important component in the postop care of these patients since they are usually malnourished before surgery. Enteral route is preferred in order to maintain gut integrity and reduce bacterial translocation. Postoperative ileus, sepsis, intraabdominal complications like anastomotic leaks, obstruction and fistulas may be hindrances to enteral nutrition necessitating TPN. We started TPN in our patients if they could not be fed for more than 2-3 d through gut.
Median survival for colorectal cancer varies from 13 to 29 mo and 5 year survival rates range from 11% to 19%[9]. Survival rates for gastric cancer have been 43% at 1 year and 11% at 5 years[44]. Median survival from ovarian cancer ranges from 22 to 64 mo and 12%-66% 5 year survival rate[12,13]. In our series, the long-term median survival collectively was observed to be 14 mo with no ICU mortality, 4% 30 d mortality and 16% 90 d mortality. One year survival was 56.4% (28/51 patients). These findings suggest good ICU outcomes for these patients due to early aggressive resuscitation and vigilance in detection of the anticipated complications observed in this population particularly abdominal sepsis.
Should all patients undergoing CRS and HIPEC be admitted to ICU postoperatively? This question has been addressed in some recent studies[28,45-48]. López-Basave et al[28] concluded that 67% of their patients needed ICU care postoperatively after CRS and HIPEC procedure. They concluded that ICU care should not be a routine standard of care and there should be an individualized approach based on patient characteristics and extent of resection[28]. Another recent study by Mogal et al[45] concluded that ICU observation is not routinely required for all patients treated with CRS/HIPEC. Their criteria for ICU admission used variables like ECOG status (Eastern Cooperative Oncology Group), age, EBL, nutritional status and extent of surgery[45]. Nadeem et al[46] concluded that this procedure can be done safely with no major complications with proper selection criteria for patients. Need for ICU utilization and shorter hospital LOS is seen with more experience with the procedure, thereby referral to a high volume center is important[46]. This is in accordance with experience with the procedure at our center. Malfroy et al[47] studied perioperative risk factors for ICU admission and concluded shock (septic and hemorrhagic), respiratory failure, postoperative acidosis as the reasons for direct ICU admission from operating room. Based on our subgroup analysis of ICU and non ICU patients, we conclude that preoperative co morbidities (ASA score), extent of surgical debulking performed, blood losses during surgery, amount of blood products required intraoperatively and total OR time are the factors to be considered while triaging patients to the ICU or the floor in addition to hemodynamic instability and need for mechanical ventilation.
Our study addresses postoperative ICU management, morbidity and mortality of patients undergoing CRS and HIPEC therapy. We also studied the factors to be considered during postoperative triage of patients to ICU vs the floor. Need for vasopressors and/or mechanical ventilation, preoperative medical co morbidities, extent of surgical debulking, intraoperative blood losses, amount of intra op blood products required and total operative time necessitate ICU admission. Intensivists should be vigilant to aggressive postop resuscitation, need for organ support, monitoring and correcting derangements in the coagulation profile, fluid and electrolytes, pain control, early detection and management of major surgical complications particularly abdominal sepsis. Overall, the ICU outcomes for these patients are excellent.
Peritoneal carcinomatosis (PC) from gastric, colorectal, ovarian, appendiceal tumors is associated with poor prognosis. Cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) has been shown to improve survival in these cases. But the procedure is associated with increased morbidity and mortality. Extensive surgical resection with hyperthermic chemotherapy generates intense inflammatory response in the body, leading to physiologic changes in many organ systems. Intensivists taking care of these patients in the intensive care unit (ICU) postoperatively need to be aware of derangements like fluid and electrolyte abnormalities, hemodynamic instability, need for intravenous fluids, coagulation abnormalities and increased risk of surgical complications like anastomotic leaks and intra-abdominal abscesses. In this study, the authors describe the early postoperative ICU management, morbidity and mortality of patients admitted to ICU after CRS and HIPEC therapy.
CRS and HIPEC therapy is a complex procedure associated with increased morbidity and mortality. Few prior studies have described the postoperative ICU management and complications related to the procedure. The study provides knowledge and guidance to the Intensivists and surgeons managing these patients in the postoperative period in ICU. It also studies variables to be considered while triaging patients to the ICU vs floor postoperatively.
In this study, the authors describe the postoperative ICU management and complications after CRS and HIPEC procedure for PC. Overall, the outcomes of these patients are excellent. Particular attention should be given to postoperative pain management, aggressive fluid resuscitation, electrolyte and coagulation abnormalities and increased risk for surgical complications like anastomotic leaks, intraabdominal abscesses and wound infections. Factors to be weighed in this population during postoperative triage to ICU vs floor include preoperative medical co morbidities, extent of surgical debulking, intraoperative blood losses, amount of intraoperative blood products transfused and total operative time.
This study provides insight about postoperative ICU management of patients undergoing CRS and HIPEC therapy. It also describes the variables to be considered while triaging patients to the ICU vs surgical floor in the postoperative period.
Hyperthermic intraperitoneal chemotherapy (HIPEC): Highly concentrated, heated chemotherapy treatment that is delivered directly to the abdomen during surgery; Cytoreductive surgery (CRS): Surgical procedure used to remove tumors from patients with metastasis or dissemination to the peritoneal cavity.
A very interesting manuscript describing the experience of a center involved in cytoreductive surgery and intraperitoneal chemotherapy.
Manuscript source: Unsolicited manuscript
Specialty type: Critical care medicine
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Belliato M, Cashin PH, Tentes AA, Willms DC S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Glehen O, Mohamed F, Gilly FN. Peritoneal carcinomatosis from digestive tract cancer: new management by cytoreductive surgery and intraperitoneal chemohyperthermia. Lancet Oncol. 2004;5:219-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 295] [Cited by in RCA: 301] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 2. | Chua TC, Yan TD, Saxena A, Morris DL. Should the treatment of peritoneal carcinomatosis by cytoreductive surgery and hyperthermic intraperitoneal chemotherapy still be regarded as a highly morbid procedure?: a systematic review of morbidity and mortality. Ann Surg. 2009;249:900-907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 387] [Cited by in RCA: 422] [Article Influence: 26.4] [Reference Citation Analysis (0)] |
| 3. | Verwaal VJ, Bruin S, Boot H, van Slooten G, van Tinteren H. 8-year follow-up of randomized trial: cytoreduction and hyperthermic intraperitoneal chemotherapy versus systemic chemotherapy in patients with peritoneal carcinomatosis of colorectal cancer. Ann Surg Oncol. 2008;15:2426-2432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 710] [Cited by in RCA: 765] [Article Influence: 45.0] [Reference Citation Analysis (0)] |
| 4. | Verwaal VJ, van Ruth S, de Bree E, van Sloothen GW, van Tinteren H, Boot H, Zoetmulder FA. Randomized trial of cytoreduction and hyperthermic intraperitoneal chemotherapy versus systemic chemotherapy and palliative surgery in patients with peritoneal carcinomatosis of colorectal cancer. J Clin Oncol. 2003;21:3737-3743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1396] [Cited by in RCA: 1512] [Article Influence: 68.7] [Reference Citation Analysis (0)] |
| 5. | Cashin PH, Mahteme H, Spång N, Syk I, Frödin JE, Torkzad M, Glimelius B, Graf W. Cytoreductive surgery and intraperitoneal chemotherapy versus systemic chemotherapy for colorectal peritoneal metastases: A randomised trial. Eur J Cancer. 2016;53:155-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 128] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 6. | Roviello F, Marrelli D, Neri A, Cerretani D, de Manzoni G, Pedrazzani C, Cioppa T, Nastri G, Giorgi G, Pinto E. Treatment of peritoneal carcinomatosis by cytoreductive surgery and intraperitoneal hyperthermic chemoperfusion (IHCP): postoperative outcome and risk factors for morbidity. World J Surg. 2006;30:2033-2040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 63] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 7. | Fujimoto S, Takahashi M, Mutou T, Kobayashi K, Toyosawa T. Successful intraperitoneal hyperthermic chemoperfusion for the prevention of postoperative peritoneal recurrence in patients with advanced gastric carcinoma. Cancer. 1999;85:529-534. [PubMed] |
| 8. | Glehen O, Mithieux F, Osinsky D, Beaujard AC, Freyer G, Guertsch P, Francois Y, Peyrat P, Panteix G, Vignal J. Surgery combined with peritonectomy procedures and intraperitoneal chemohyperthermia in abdominal cancers with peritoneal carcinomatosis: a phase II study. J Clin Oncol. 2003;21:799-806. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 177] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 9. | Yan TD, Black D, Savady R, Sugarbaker PH. Systematic review on the efficacy of cytoreductive surgery combined with perioperative intraperitoneal chemotherapy for peritoneal carcinomatosis from colorectal carcinoma. J Clin Oncol. 2006;24:4011-4019. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 264] [Cited by in RCA: 259] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 10. | Shen P, Stewart JH, Levine EA. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for peritoneal surface malignancy: overview and rationale. Curr Probl Cancer. 2009;33:125-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Sayag-Beaujard AC, Francois Y, Glehen O, Sadeghi-Looyeh B, Bienvenu J, Panteix G, Garbit F, Grandclément E, Vignal J, Gilly FN. Intraperitoneal chemo-hyperthermia with mitomycin C for gastric cancer patients with peritoneal carcinomatosis. Anticancer Res. 1999;19:1375-1382. [PubMed] |
| 12. | Bijelic L, Jonson A, Sugarbaker PH. Systematic review of cytoreductive surgery and heated intraoperative intraperitoneal chemotherapy for treatment of peritoneal carcinomatosis in primary and recurrent ovarian cancer. Ann Oncol. 2007;18:1943-1950. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 13. | Chua TC, Robertson G, Liauw W, Farrell R, Yan TD, Morris DL. Intraoperative hyperthermic intraperitoneal chemotherapy after cytoreductive surgery in ovarian cancer peritoneal carcinomatosis: systematic review of current results. J Cancer Res Clin Oncol. 2009;135:1637-1645. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 142] [Cited by in RCA: 137] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 14. | Bereder J, Glehen O, Habre J, Desantis M, Cotte E, Mounier N, Ray-Cocquard I, Karimdjee B, Bakrin N, Bernard J. Cytoreductive surgery combined with perioperative intraperitoneal chemotherapy for the management of peritoneal carcinomatosis from ovarian cancer: a multiinstitutional study of 246 patients. J Clin Oncol. 2009;27:abstr 5542. |
| 15. | Tabrizian P, Shrager B, Jibara G, Yang MJ, Romanoff A, Hiotis S, Sarpel U, Labow DM. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for peritoneal carcinomatosis: outcomes from a single tertiary institution. J Gastrointest Surg. 2014;18:1024-1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 67] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 16. | Levine EA, Stewart JH, Shen P, Russell GB, Loggie BL, Votanopoulos KI. Intraperitoneal chemotherapy for peritoneal surface malignancy: experience with 1,000 patients. J Am Coll Surg. 2014;218:573-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 212] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 17. | Iversen LH, Rasmussen PC, Hagemann-Madsen R, Laurberg S. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for peritoneal carcinomatosis: the Danish experience. Colorectal Dis. 2013;15:e365-e372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | Shime N, Lee M, Hatanaka T. Cardiovascular changes during continuous hyperthermic peritoneal perfusion. Anesth Analg. 1994;78:938-942. [PubMed] |
| 19. | Kanakoudis F, Petrou A, Michaloudis D, Chortaria G, Konstantinidou A. Anaesthesia for intra-peritoneal perfusion of hyperthermic chemotherapy. Haemodynamic changes, oxygen consumption and delivery. Anaesthesia. 1996;51:1033-1036. [PubMed] |
| 20. | Izzo L, Pierannunzi F, Vari A, Riccardi S, Tarquini S, Fermariello A, Di Giorgio A, Casullo A, Caputo M, Costi U. [Anaesthesiologic problems about hyperthermic intraoperative intraperitoneal chemotherapy]. G Chir. 2004;25:361-364. [PubMed] |
| 21. | Esquivel J, Angulo F, Bland RK, Stephens AD, Sugarbaker PH. Hemodynamic and cardiac function parameters during heated intraoperative intraperitoneal chemotherapy using the open “coliseum technique”. Ann Surg Oncol. 2000;7:296-300. [PubMed] |
| 22. | Schmidt C, Creutzenberg M, Piso P, Hobbhahn J, Bucher M. Peri-operative anaesthetic management of cytoreductive surgery with hyperthermic intraperitoneal chemotherapy. Anaesthesia. 2008;63:389-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 110] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 23. | Schmidt C, Moritz S, Rath S, Grossmann E, Wiesenack C, Piso P, Graf BM, Bucher M. Perioperative management of patients with cytoreductive surgery for peritoneal carcinomatosis. J Surg Oncol. 2009;100:297-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 24. | Esquivel J. Technology of hyperthermic intraperitoneal chemotherapy in the United States, Europe, China, Japan, and Korea. Cancer J. 2009;15:249-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 48] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 25. | Smeenk RM, Verwaal VJ, Zoetmulder FA. Learning curve of combined modality treatment in peritoneal surface disease. Br J Surg. 2007;94:1408-1414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 167] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 26. | Glehen O, Kwiatkowski F, Sugarbaker PH, Elias D, Levine EA, De Simone M, Barone R, Yonemura Y, Cavaliere F, Quenet F. Cytoreductive surgery combined with perioperative intraperitoneal chemotherapy for the management of peritoneal carcinomatosis from colorectal cancer: a multi-institutional study. J Clin Oncol. 2004;22:3284-3292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 860] [Cited by in RCA: 882] [Article Influence: 42.0] [Reference Citation Analysis (0)] |
| 27. | Cooksley TJ, Haji-Michael P. Post-operative critical care management of patients undergoing cytoreductive surgery and heated intraperitoneal chemotherapy (HIPEC). World J Surg Oncol. 2011;9:169. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 62] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 28. | López-Basave HN, Morales-Vasquez F, Mendez-Herrera C, Namendys-Silva SA, Luna-Ortiz K, Calderillo-Ruiz G, Cabrera Rojas J, Ruiz-Garcia E, Herrera-Gomez A, Ruiz-Molina JM. Intensive care unit admission after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Is it necessary? J Oncol. 2014;2014:307317. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 29. | Sugarbaker PH, Alderman R, Edwards G, Marquardt CE, Gushchin V, Esquivel J, Chang D. Prospective morbidity and mortality assessment of cytoreductive surgery plus perioperative intraperitoneal chemotherapy to treat peritoneal dissemination of appendiceal mucinous malignancy. Ann Surg Oncol. 2006;13:635-644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 200] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 30. | Kemal JM, Elshaikh SM, Nabil D, Mohamad AM. The perioperative course and anesthetic challenge for cytoreductive surgery with hyperthermic intraperitoneal chemotherapy. Egyptian Journal of Anesthesia. 2013;29:311-318. [RCA] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 31. | Jacquet P, Stephens AD, Averbach AM, Chang D, Ettinghausen SE, Dalton RR, Steves MA, Sugarbaker PH. Analysis of morbidity and mortality in 60 patients with peritoneal carcinomatosis treated by cytoreductive surgery and heated intraoperative intraperitoneal chemotherapy. Cancer. 1996;77:2622-2629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 32. | Helm CW, Randall-Whitis L, Martin RS, Metzinger DS, Gordinier ME, Parker LP, Edwards RP. Hyperthermic intraperitoneal chemotherapy in conjunction with surgery for the treatment of recurrent ovarian carcinoma. Gynecol Oncol. 2007;105:90-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 63] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 33. | Lanuke K, Mack LA, Temple WJ. A prospective evaluation of venous thromboembolism in patients undergoing cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Can J Surg. 2009;52:18-22. [PubMed] |
| 34. | Roviello F, Caruso S, Marrelli D, Pedrazzani C, Neri A, De Stefano A, Pinto E. Treatment of peritoneal carcinomatosis with cytoreductive surgery and hyperthermic intraperitoneal chemotherapy: state of the art and future developments. Surg Oncol. 2011;20:e38-e54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 76] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 35. | Ahmed S, Oropello JM. Critical care issues in oncological surgery patients. Crit Care Clin. 2010;26:93-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 36. | Glehen O, Osinsky D, Cotte E, Kwiatkowski F, Freyer G, Isaac S, Trillet-Lenoir V, Sayag-Beaujard AC, François Y, Vignal J. Intraperitoneal chemohyperthermia using a closed abdominal procedure and cytoreductive surgery for the treatment of peritoneal carcinomatosis: morbidity and mortality analysis of 216 consecutive procedures. Ann Surg Oncol. 2003;10:863-869. [PubMed] |
| 37. | Elias D, Gilly F, Boutitie F, Quenet F, Bereder JM, Mansvelt B, Lorimier G, Dubè P, Glehen O. Peritoneal colorectal carcinomatosis treated with surgery and perioperative intraperitoneal chemotherapy: retrospective analysis of 523 patients from a multicentric French study. J Clin Oncol. 2010;28:63-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 685] [Cited by in RCA: 737] [Article Influence: 46.1] [Reference Citation Analysis (0)] |
| 38. | Elias D, Goere D, Blot F, Billard V, Pocard M, Kohneh-Shahri N, Raynard B. Optimization of hyperthermic intraperitoneal chemotherapy with oxaliplatin plus irinotecan at 43 degrees C after compete cytoreductive surgery: mortality and morbidity in 106 consecutive patients. Ann Surg Oncol. 2007;14:1818-1824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 107] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 39. | Levine EA, Stewart JH, Russell GB, Geisinger KR, Loggie BL, Shen P. Cytoreductive surgery and intraperitoneal hyperthermic chemotherapy for peritoneal surface malignancy: experience with 501 procedures. J Am Coll Surg. 2007;204:943-953; discussion 953-955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 167] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 40. | Chua TC, Saxena A, Schellekens JF, Liauw W, Yan TD, Fransi S, Zhao J, Morris DL. Morbidity and mortality outcomes of cytoreductive surgery and perioperative intraperitoneal chemotherapy at a single tertiary institution: towards a new perspective of this treatment. Ann Surg. 2010;251:101-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 68] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 41. | Jaehne J. Cytoreductive procedures-strategies to reduce postoperative morbidity and management of surgical complications with special emphasis on anastomotic leaks. J Surg Oncol. 2009;100:302-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 42. | Fujimura T, Yonemura Y, Nakagawara H, Kitagawa H, Fushida S, Nishimura G, Miyazaki I, Shibata K. Subtotal peritonectomy with chemohyperthermic peritoneal perfusion for peritonitis carcinomatosa in gastrointestinal cancer. Oncol Rep. 2000;7:809-814. [PubMed] |
| 43. | Baratti D, Kusamura S, Iusco D, Bonomi S, Grassi A, Virzì S, Leo E, Deraco M. Postoperative complications after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy affect long-term outcome of patients with peritoneal metastases from colorectal cancer: a two-center study of 101 patients. Dis Colon Rectum. 2014;57:858-868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 100] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 44. | Yonemura Y, Fujimura T, Nishimura G, FallaR T, Katayama K, Tsugawa K, Fushida S, Miyazaki I, Tanaka M, Endou Y. Effects of intraoperative chemohyperthermia in patients with gastric cancer with peritoneal dissemination. Surgery. 1996;119:437-444. [PubMed] |
| 45. | Mogal HD, Levine EA, Fino NF, Obiora C, Shen P, Stewart JH, Votanopoulos KI. Routine Admission to Intensive Care Unit After Cytoreductive Surgery and Heated Intraperitoneal Chemotherapy: Not Always a Requirement. Ann Surg Oncol. 2016;23:1486-1495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 46. | Nadeem A, Al-Tarifi A. ICU outcome of patients undergoing cytoreductive surgery followed by hyperthermic intraperitoneal chemotherapy: a single center study. Crit Care. 2015;19:P376. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 47. | Malfroy S, Wallet F, Maucort-Boulch D, Chardonnal L, Sens N, Friggeri A, Passot G, Glehen O, Piriou V. Complications after cytoreductive surgery with hyperthermic intraperitoneal chemotherapy for treatment of peritoneal carcinomatosis: Risk factors for ICU admission and morbidity prognostic score. Surg Oncol. 2016;25:6-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 48. | Padmakumar AV. Intensive Care Management of Patient After Cytoreductive Surgery and HIPEC - A Concise Review. Indian J Surg Oncol. 2016;7:244-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |