Published online Feb 4, 2016. doi: 10.5492/wjccm.v5.i1.36
Peer-review started: October 2, 2015
First decision: October 27, 2015
Revised: December 1, 2015
Accepted: January 8, 2016
Article in press: January 11, 2016
Published online: February 4, 2016
Processing time: 116 Days and 9.8 Hours
Traumatic brain injury (TBI) is a major cause of death and disability in children. Severe TBI is a leading cause of death and often leads to life changing disabilities in survivors. The modern management of severe TBI in children on intensive care unit focuses on preventing secondary brain injury to improve outcome. Standard neuroprotective measures are based on management of intracranial pressure (ICP) and cerebral perfusion pressure (CPP) to optimize the cerebral blood flow and oxygenation, with the intention to avoid and minimise secondary brain injury. In this article, we review the current trends in management of severe TBI in children, detailing the general and specific measures followed to achieve the desired ICP and CPP goals. We discuss the often limited evidence for these therapeutic interventions in children, extrapolation of data from adults, and current recommendation from paediatric guidelines. We also review the recent advances in understanding the intracranial physiology and neuroprotective therapies, the current research focus on advanced and multi-modal neuromonitoring, and potential new therapeutic and prognostic targets.
Core tip: Paediatric traumatic brain injury (TBI) causes significant morbidity and mortality. The modern management of severe TBI in children focuses on preventing secondary brain injury to improve outcome. In this article, we review the current management of severe TBI in children. We also review the recent advances in understanding intracranial physiology and neuroprotective therapies, advanced and multi-modal neuromonitoring, and potential new therapeutic and prognostic targets.
- Citation: Agrawal S, Branco RG. Neuroprotective measures in children with traumatic brain injury. World J Crit Care Med 2016; 5(1): 36-46
- URL: https://www.wjgnet.com/2220-3141/full/v5/i1/36.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v5.i1.36
Traumatic brain injury (TBI) is a major cause of death and disability in children and young adults worldwide. It is considered a “silent epidemic” because the general public is mostly unaware of the scale of the problem[1]. In the United States, it is estimated that around 1.7 million people sustain TBI each year, and in Europe 235 per 100000 people are admitted to hospital following a TBI[2,3]. Data from many parts of the world consistently show peak incidence rates in children, young adults and elderly people.
TBI occurs when head suffers the influence of an external mechanical force. This force can displace brain inside the skull and induce injury against the meningeal membrane or the cranium. Acceleration and deceleration forces can also disrupt nervous tissue and blood vessels of the brain. All grades of injury can occur, ranging from mild to severe TBI with cerebral oedema or large collections of blood. Severe TBI, defined as a post resuscitation Glasgow coma scale (GCS) of less than 9[4], is associated with highest rates of mortality and significant morbidity in survivors often causing life changing disability and cognitive function loss[5].
The mechanism of injury in TBI comprises of primary and secondary injuries. The primary injury is the direct consequence of the initial physical insult. It comprises irreversible cell damage that is the main determinant of clinical outcome. In the secondary injury, inflammatory and neurotoxic responses triggered by the primary injury induce oedema, hypoperfusion, hypoxia and ischaemia[6-8]. These changes often lead to raised intracranial pressure (ICP), temperature dysregulation, loss of autoregulation and seizures[9]. Much of these secondary injuries may be amenable to intervention, and left untreated can significantly increase morbidity and mortality associated with TBI[6].
Raised ICP plays a key role in secondary brain injury[9]. Skull is a rigid fixed volume compartment; the three elements within it namely, the brain parenchyma, blood and cerebro-spinal fluid (CSF) are relatively incompressible and changes in the volume of one leads to compression of the other[10]. Beyond the limits of compensation, the pressure rises sharply, this can severely impact the cerebral blood flow (CBF). The secondary insults can also arise from systemic factors, hypoxia and hypotension post head injury being the key determinants for outcome[7,11].
Early stabilisation post TBI includes rapid assessment for life threatening injuries followed by secondary survey according to ATLS/APLS guidelines[12,13]. After the initial resuscitation to ensure adequate airway, ventilation and haemodynamic stability, early neuro-imaging is required to look for intra-cranial pathologies requiring surgical intervention and neuroprotection[14]. There is evidence to support multi-disciplinary input and protocolized management for improved outcomes from head injury[15]. All children with moderate to severe traumatic brain injury should ideally be managed in centres with expertise and experience in managing such patients. The contemporary post-injury resuscitation and management focuses on prevention and mitigation of secondary insults[7,14]. This review will focus on the neuroprotective measures to decrease the damage caused by secondary brain injury in children with TBI requiring intensive care treatment.
All children with severe TBI and those with deteriorating GCS need definitive airway management with endotracheal intubation. As paediatric definitive airway needs specialist skills and experience, pre-hospital intubation at the scene for children with TBI is controversial[16]. However, early airway control is recommended to avoid hypoxemia, hypercarbia and aspiration[17]. The adequacy of oxygenation and ventilation should be measured continuously with pulse oximetry and end-tidal carbon dioxide (CO2) monitoring respectively and serial blood gas measurements. In children with TBI requiring ventilation, arterial PaO2 should be maintained above 11 kPa (saturations > 90%) and PaCO2 between 4.5-5 kPa. Although there are no randomised controlled trials (RCT) to determine the exact values for PaO2 in TBI, the damaging effects of hypoxia[17,18] and to a lesser extent hyperoxia[19] are well known. Similarly, the effect of CO2 on cerebrovascular reactivity has been widely studied[19-21]. Hypercapnea causes vasodilatation leading to cerebral hyperaemia and hypocapnea causes ischemia by cerebral vasoconstriction[9,21,22].
Hypotension (defined as systolic blood pressure below the fifth percentile for age) or shock any time after injury can have major implications for clinical outcome and should be actively prevented and aggressively treated with fluid boluses and vasoactive agents[16]. Isotonic saline is recommended for fluid resuscitation and maintenance. In the presence of hypotension, patient also needs careful evaluation for extracranial injuries as the potential source of blood loss[23,24]. It is important to consider adrenocorticotropic hormone (ACTH) deficiency in patients with refractory hypotension; TBI induced pituitary dysfunction has been reported in nearly one quarter of children with TBI in the acute phase[25,26]. As the primary injury often impairs cerebral autoregulation, the cerebral perfusion may become directly dependent on the mean arterial pressure. Management of blood pressure in the intensive care is one of the cornerstones of the management of severe TBI[14]. While hypotension can potentially cause brain ischemia, hypertension can exacerbate vasogenic oedema in the cerebral parenchyma[27] and requires careful titration of blood pressure based on various parameters studied (discussed in details under specific interventions).
Although there are no RCTs studying the effect of sedation on outcome, it’s well known that any noxious stimulus increases ICP[28] and cerebral metabolic demand for oxygen[29]. Appropriate sedation and analgesia reduces anxiety and pain, facilitates ventilation and general intensive care management, and helps reduce the cerebral oxygen demand, thereby reducing the risk of secondary brain injury[30]. In children, a combination of benzodiazepines and opioids is most often used. This combination can cause hypotension, so careful titration to the desired effect with continuous monitoring and management of blood pressure is essential to minimize risks of cerebral ischemia. Propofol, often used in adults, has restricted licence status in children, therefore, is only used in exceptional circumstances.
Neuromuscular paralysis can help reduce airway and intrathoracic pressure which improves the cerebral venous return. It can prevent shivering and posturing, and the lack of skeletal muscle movement also helps to reduce cerebral metabolic demand[30]. The main disadvantage of neuromuscular blockade is masking of clinical seizures which should then ideally be monitored by continuous electroencephalograph (EEG). Its continuous use can also induce myopathy, increase length of ventilation, and cause nosocomial pneumonia and cardiovascular side effects[31]. However, judicious neuromuscular blockage use in children with severe TBI can minimize complications[32]. Therefore, neuromuscular blockade is recommended as part of the first tier management of children with severe TBI[14].
There is no single best fluid for children with traumatic brain injury, but isotonic crystalloids are widely used and have good scientific basis. Normal saline or lactated ringer’s solution should be the standard resuscitation fluid until further studies show a clear benefit from other therapies. Use of colloids is not routinely recommended and evidence suggests that use of albumin may have deleterious effects[33]. Fluid restriction is no longer recommended.
Nutritional support is required for tissue repair, wound healing and optimal organ function. Due to lack of evidence, there is no specific recommendation for the nutrition regimen. Adult data supports early introduction of feeds after haemodynamic stability aiming for full feeds, either enteral or parenteral, by the end of first week[34,35]. Hyperglycaemia frequently occurs associated with the stress response to injury; therefore glucose is not routinely added to maintenance fluids in early phase of recovery regardless of the child’s age. Hyperglycaemia has been linked to poor neurological outcome in TBI[36-38] but the optimal glucose target has not been defined. Use of insulin to achieve tight glycaemic control may result in a net reduction in CSF microdialysis glucose and an increase in microdialysis glutamate and lactate pyruvate ratio (LPR) without conveying a functional outcome advantage[39]. Tight glycaemic control has also been associated with reduced cerebral extracellular glucose availability and increased prevalence of brain energy crisis, which in turn correlates with increased mortality[40]. Currently we recommend prevention of severe hyperglycaemia, keeping blood glucose levels below 180 mg/dL (10 mmol/L).
Children should be nursed in neutral head position and head-end elevation by 15o-30o to improve cerebral venous drainage[41,42]. Good nursing care, with regular turning, eye care and physiotherapy are important. Stress ulcer prophylaxis and laxatives are used as per the child’s requirements. Although evidence shows higher incidence of deep vein thrombosis (DVT) with increasing severity of trauma and increasing age in children[43], there are no universal recommendations for regular thromboprophylaxis in this age group. One study supports thromboprophylaxis to prevent DVT in paediatric trauma patients[44]. In our setting, compression stockings are routinely used in fully sedated and paralysed children with severe TBI, but the chemical prophylaxis is restricted to older children and is discussed on case by case basis.
The ICP can rise after TBI from either mass effect (haematoma) or cerebral oedema secondary to the injury. There is a direct association between raised ICP and poor clinical outcomes, and sustained raised ICP is an independent predictor of poor outcome following TBI[45-47]. While majority of evidence supports aggressive management of raised ICP[47-49], recent adult RCT failed to identify any benefit associated with ICP monitoring[50]. The results of this study[50] however need to be interpreted in the context of population studied and may not be generalizable to all TBI victims[51]. The lack of controlled trials for ICP monitoring has limited the recommendation (level III) in the most up-to-date guidelines[14,52] although ICP monitoring remains the integral part in the management of patients with severe TBI in most centres.
There are various different methods for ICP monitoring using either fluid filled catheters or pressure microtransducers. Interventricular catheters are considered to be the gold standard for measuring ICP and also allow CSF drainage if ICP is high. However, there are practical limitations to their use including infection and technical difficulty in insertion in children with small ventricles[53,54]. Pressure microtransducers can reliably measure pressure from brain parenchyma (intraparenchymal) as well as epidural or subarachnoid spaces. Intraparenchymal probes are often preferred because they are easy to insert and have very low infection risk. However, they may not reflect the true ICP if there are pressure gradients within the cranium, and although the zero drift is minimal, they cannot be recalibrated once inserted[53].
The threshold for treating ICP in children has been extrapolated from adult guidelines[52]. There is some suggestion that the treatment thresholds for younger children and infants need to be different as the normal values of mean ABP and hence Cerebral perfusion pressure (CPP) are lower in children[55]. Keeping the ICP < 20 mmHg is the standard part of management of severe TBI on PICU[14].
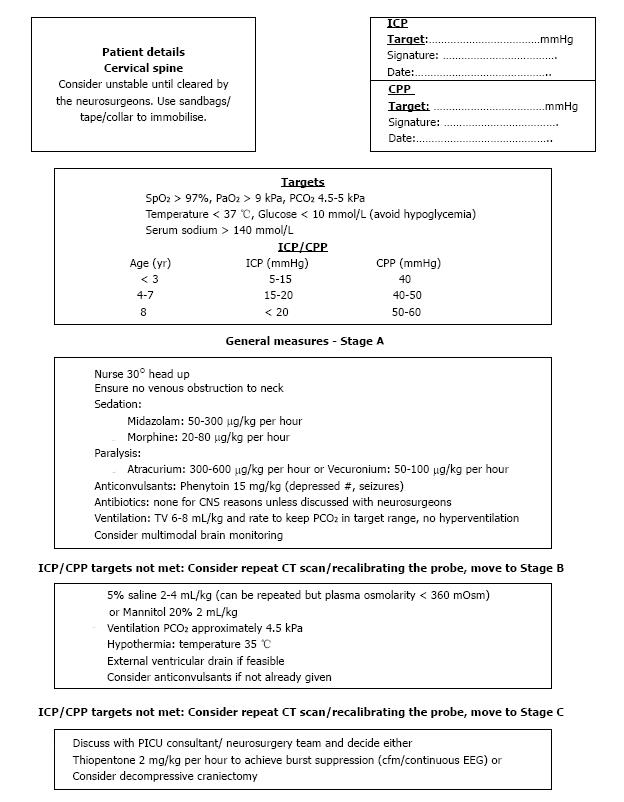
Our current local protocol uses an age related threshold for ICP in children (Figure 1). If the ICP stays above the target, we first optimise sedation and the ventilation targets. If it still stays up, we use hyperosmolar therapy and consider repeat neuroimaging. If the scan doesn’t show any surgically correctible lesion (haematoma evacuation, ventricular drain), we move to tier 2 treatment (hypothermia, anticonvulsants). Decompressive craniectomy and thiopentone coma are used only in exceptional circumstances after multi-disciplinary input.
CPP is defined as the difference between mean arterial pressure (MAP) and ICP, and is considered the driving pressure for cerebral blood flow and perfusion. In the normal brain, cerebral autoregulation maintains CPP within a specific range to couple oxygen delivery with cerebral metabolic rate. However, TBI impairs the cerebral autoregulatory capacity making brain vulnerable to both systemic hypotension and raised ICP. In adults, keeping CPP above a recommended threshold (60 or 70 mmHg) is associated with improved clinical outcomes[52,55]; some paediatric evidence also supports targeting higher CPP in children[56,57]. However, there are age related differences in MAP, CBF, and cerebral metabolic rate and there are no studies to demonstrate active management of CPP above a target threshold reducing mortality or morbidity[14]. Therefore, defining an ideal CPP for children is challenging and the current guidelines support maintaining a minimum CPP of 40 mmHg and a threshold of 40-50 mmHg[14]. Targeting very high CPP with use of vasopressors and fluids is associated with serious systemic toxicity and does not give better outcomes[52]. Also, in the absence of autoregulation, very high CPP can increase cerebral blood volume leading to an increasing ICP and also increase vasogenic oedema by increasing the hydrostatic pressure across the capillary bed[27].
Our management targets are described in Figure 1, we achieve target CPP by maintaining systemic blood pressure towards the upper limit of normal blood pressure for age with the use of fluids to achieve normovolemia and inotropic support (most commonly noradrenaline infusion). However, if the ICP is very high, we do not increase MBP beyond the age related MBP limits and instead, focus on improving CPP by reduction in ICP.
Hyperosmolar therapy has been the hallmark of ICP management for decades. Hyperosmolar agents create osmotic gradient across the cerebral vascular bed, thereby decreasing oedema. They work best for acute rises in ICP. Various osmotic agents have been studied in the treatment of TBI, but mannitol and hypertonic saline are the most widely used.
Mannitol has been used to reduce raised ICP for close to a century. It reduces ICP by reducing blood viscosity (rapid response) and by an osmotic effect (delayed response)[58]. These effects are more pronounced when the blood brain barrier is intact and autoregulation is preserved. In TBI, these mechanisms may be disrupted, so the response can be variable[59]. Mannitol can also reduce intravascular volume by causing osmotic diuresis (which could have a negative impact on CPP) and has the potential to induce reverse osmotic gradient by accumulating in the brain parenchyma (which could cause an increase in ICP) especially with prolonged use[60].
Hypertonic saline has been studied extensively in the last few decades as treatment for raised ICP. It shares the same rheologic and osmolar properties with mannitol that lower the ICP. It can also act as a volume expander, enhance cardiac output, improve CBF and inhibit inflammation[61-63]. Current guidelines support the use of hypertonic saline, but make no specific recommendation on the concentration[14]. Different studies and institutions use various concentrations from 1.7% to 29.2%[64,65]; in our institute, we use 5% saline (Figure 1). Delivery through a central access is recommended (but not essential) due to high osmolality. We use 2-4 mL/kg boluses of 5% saline (Figure 1).
Serum osmolarity plays an important role in determining fluid shifts in injured brain. Low serum osmolarity can increase vasogenic brain oedema, so hyperosmolar agents are used to normalise or increase serum osmolarity. Different upper limits of osmolarity are recommended for treatment with mannitol (320 mOsm) and hypertonic saline (360 mOsm), respectively. If using hypertonic saline, serum sodium levels need to be monitored as well and kept < 160 mmol/L. Due to lack of evidence for mannitol use in children with TBI, hypertonic saline has been recommended as the preferred osmotic agent in management of paediatric TBI[65,66].
Children with TBI are also susceptible to develop disorders of salt and water, like central diabetes insipidus, cerebral salt wasting and syndrome of inappropriate anti-diuretic hormone. A detailed description of these is beyond the scope of this article, but a careful understanding and monitoring of serum and urine electrolytes and osmolarity is required[67].
Hyperthermia can cause significant secondary brain injury by increasing cerebral metabolic demand, promoting inflammation and decreasing the seizure threshold, so needs to be avoided aggressively to protect brain[68]. Temperature control to avoid hyperthermia has become an integral part of neuroprotection in children with TBI[14]. Inducing hypothermia to reduce cerebral metabolic demand, inflammation and seizures, is more contentious. The theoretical benefits of induced hypothermia have not been confirmed in multi-centric trials despite a consistent decrease in ICP in the hypothermic patients. Rebound rise in ICP during rewarming and the delay to achieve target temperature have been suggested as the limiting factors that lead to no difference in neurological outcome of children receiving hypothermia[69,70]. Despite the lack of evidence, induced moderate hypothermia (32 °C-33 °C) is used as a second tier strategy to control ICP if the first tier strategies (sedation, analgesia, paralysis, osmolar therapy) have failed. The specific recommendation is to induce hypothermia early (within 8 h) for 48 h followed by very gradual rewarming (≤ 0.5 °C/h)[14].
We use cooling blankets to keep patients normothermic (36 °C-37 °C) and only use hypothermia (35 °C) for uncontrolled ICP after optimising other therapies and ruling out surgically correctible pathologies (Figure 1).
CO2 is a potent determinant of cerebral vessel diameter. Lowering CO2 reduces ICP by causing vasoconstriction, but it also causes cerebral ischemia with a reduction in cerebral blood flow[21,22,71]. For this reason, hyperventilation cannot be recommended for treatment of ICP unless the patient has advanced neuromonitoring in place[14]. Despite the lack of evidence to support this strategy, evidence suggests it remains the most commonly used strategy to lower ICP[22,72]. We do not hyperventilate children with severe TBI and actively manage PaCO2 levels between 4.5-5 kPa (Figure 1).
Barbiturates lower ICP through suppression of cerebral metabolic demand and alteration of vascular tone[73,74]. It improves coupling of regional blood flow to metabolic demands resulting in improved brain oxygenation at lower cerebral blood flow and decreased ICP. Although barbiturates are effective in lowering ICP, some studies suggest it does not improve clinical outcome in adults[75] and the literature in children is very scarce. Barbiturates have very significant systemic side effects, most notably severe haemodynamic compromise and increased intrapulmonary shunt. These side effects significantly limit the use of barbiturates in PICU and may be responsible for a number of complications observed in patients receiving this therapy. Also, the agent half-life is very long, making neurological assessment difficult. Barbiturates currently cannot be recommended for routine use in care of patients with raised ICP[76], but may be used as a rescue therapy in raised ICP unresponsive to first line treatment. Continuous EEG monitoring is recommended in children with TBI using barbiturates, and the agent should be titrated to achieve burst suppression[14].
Seizures are common post head injury and are often missed as patients are sedated and paralysed, but not always receive continuous EEG monitoring[77]. Although there is limited evidence to support the use of prophylactic anti-convulsants in severe TBI patients, the current guidelines still make a level III recommendation for their use to reduce early post traumatic seizures[14].
Surgical management is a crucial part of management in TBI. If there is space-occupying haematoma post head-injury, its evacuation is the most effective mechanism of reducing ICP and avoiding secondary brain insult. Neuro-imaging is the cornerstone for diagnosing these and should be repeated for any persistent ICP rise. Space occupying lesions are often time-sensitive injuries and surgical evacuation should be performed as soon as possible, without delays.
Other surgical options for controlling ICP are CSF diversion (ventricular/lumbar drain) and decompressive craniectomy. CSF diversion can reduce CSF volume and ICP, and is recommended for eligible patients[14]. External ventricular drain (EVD) is a common method for CSF diversion and can also be used for monitoring ICP. Insertion of an EVD can be technically challenging in injured brain and may not offer any benefit if there is significant cerebral oedema causing collapsed ventricles[78]. Lumbar drain is only advised in conjunction with the EVD when there is no mass effect and cisterns are open[79].
Decompressive craniectomy can reduce ICP by allowing oedematous brain to expand by raising a bone flap and opening the dura. Although the technique lowers ICP, its benefits for outcome are not proven[80]. The current guidelines only make a level III recommendation for its use in refractory intracranial hypertension which is resistant to other treatment strategies[14]. A recent randomized controlled trial in adults suggested that decompressive craniectomy increase the number of unfavourable outcomes despite lowering ICP and shortening length of ICU stay[80].
The pathophysiology of secondary brain injury is complex. It involves interactions between cerebral metabolic demand and supply with a complex relationship of cerebral blood flow, oxygenation, autoregulatory mechanisms and physiological derangements within an injured brain. Monitoring and maintaining ICP and CPP may be too simplistic to prevent secondary insults and there is growing evidence to support that factors other than ICP and CPP independently relate to the outcome. Some of these factors can be monitored with additional therapeutic targets with a potential to improve patient outcome. Although limited in paediatric TBI, some of these modalities are being increasingly studied and hold promise. The most common targets are CBF, cerebral autoregulation, cerebral oxygenation and metabolism. Also continuous monitoring of various physiological parameters in modern intensive care environment, such as oxygen saturations, respiratory rate, heart rate, ECG, CO2, temperature, blood pressure and intracranial pressure allow for the development of multi-modal monitoring in neurocritical care. Multi-modal monitoring can interpret the relationship of these different parameters with each other and give unique information over and above the individual numbers that could be used to optimise clinical management[81].
CBF is the single most important parameter in defining the outcome after TBI. The normal brain is able to maintain near constant CBF over a range of systemic blood pressure fluctuations from about 50 to 150 mmHg by cerebrovascular pressure reactivity and autoregulation mechanisms[82]. Impaired cerebral autoregulation is common post TBI and influences the patient outcome[83-86].
Pressure reactivity index (PRx), which is a correlation coefficient between ABP and ICP, relating the ABP changes with slow fluctuations in ICP, has been studied extensively[87,88]. In intact autoregulation state, fluctuations in ABP are compensated by reactive changes in vasomotor tone. For example, a drop in ABP induces vasodilatation which increases cerebral blood volume and ICP, giving a negative correlation between ABP and ICP, and a negative PRx. Impaired autoregulation on the other hand, would lead to passive transmission of ABP fluctuations to ICP and hence a positive PRx[87]. By continuously studying cerebrovascular reactivity through PRx and plotting it against CPP, the CPP at which the vasculature is most reactive can be calculated and the optimum CPP (CPPopt) can be estimated[89,90]. This is particularly important in young children in whom CPP data is scarce and CPPopt gives an ideal therapeutic target. It is important to remember that autoregulation is dynamic and changes both between individuals and at different times within an individual patient depending on type of injury and time since injury[91,92]. Therefore, PRx and CPPopt also provide dynamic values in real time that can be used to individualise therapeutic targets for a given patient and changing targets over time depending on the state of cerebral autoregulation[93,94]. The time CPP stays above or below CPPopt has been shown to be associated with outcome[89]; whether an active management of PRx and CPPopt would affect the outcome remains to be proven in randomised controlled trial.
Transcranial Doppler ultrasonography (TCD) is a non-invasive method that measures the flow velocity in middle cerebral artery[95]. It gives non quantitative estimate of CBF and state of cerebral autoregulation based on the assumption that the diameter of the vessels insonated is relatively constantly maintained despite changes in BP and PaCO2, so the changes in flow velocity would estimate the changes in CBF. It is easy to use and can be repeated bedside, however, it is difficult to get a continuous assessment and it is liable to inter-observer variability. Various indices have been developed to interpret state of CBF and autoregulation, CPP and ICP and CO2 reactivity by using TCD. One such index called pulsatility index (PI) is based on analysing the waveform of diastolic and systolic flows in the middle cerebral artery. PI has been used to assess brain compliance and CPP, and has been shown to have an association with ICP[96,97]. Cerebrovascular resistance is estimated by a ratio of MAP to changes in flow velocity measured by TCD which is then used to calculate autoregulation index which reflects the state of autoregulation[86,98]. Alternatively, manipulation of systemic blood pressure can also be used to study the effect of ABP changes in the TCD parameters to assess autoregulation[85,86]. TCD is being increasingly used in children[85,86]; further studies are required to validate the preliminary results.
Adequate oxygen delivery to brain tissue is important to prevent secondary brain injury. The relationship between oxygen demand (cerebral metabolic rate, CMRO2) and supply (CBF) is complex post head injury due to unknown changes in metabolic demands at the cellular level, hence optimal management of ICP and CPP (surrogates for CBF) does not always prevent brain hypoxia[99].
Direct brain tissue oxygenation monitoring (PbtO2) has been used for over two decades and there is significant evidence to support its use in paediatric TBI[56,100]. The latest guidelines make a level III recommendation to keep PbtO2 above 10 mmHg in paediatric TBI[14]. The commonest method used to monitor PbtO2 is by insertion of a polarographic electrode in the brain parenchyma with the ICP bolt and the value measured is the oxygen accumulated in the brain parenchyma at the tip of the transducer, which is influenced by oxygen supply, demand and utilization. The probe placement is crucial. In focal injury, it should be placed in the pericontusional area while in diffuse injuries; it is usually placed in the non-dominant hemisphere. Although the normal values of PbtO2 are not clearly understood, animal studies suggest 20-30 mmHg as the normal values for normal uninjured brain[101]. A threshold of 10 mmHg has been accepted as the ischemic threshold and PbtO2 levels below 10 mmHg have been associated with poor outcome. PbtO2 values can be improved by increasing inspired oxygen/ventilation, haemoglobin levels and MBP[57,102].
Continuous jugular venous saturation monitoring (SjvO2) is another method used to understand the relationship between CBF and brain metabolism and gives the difference between cerebral oxygen supply and demand. A retrograde catheter inserted in the jugular venous bulb measures continuous SjvO2. There is no consensus for normal levels of SjvO2 in children but in adults 50%-75% is considered normal. Values outside this range are considered abnormal and have been shown to be associated with poor outcome[52,103]. Due to technical difficulties, paediatric experience with the use of SjvO2 is limited. It is also not a good indicator of regional changes in the injured brain.
Regional cerebral blood flow can be measured directly by thermal diffusion probes (TDP) inserted in brain parenchyma. The technique has been validated with good agreement between TDP and xenon-CT for regional CBF measurements. In combination with PbtO2, TDP can be potentially useful in optimizing management of CPP[104].
It is possible to study the concentration of chemicals found in the brain parenchyma by using microdialysis and is now frequently used in monitoring and managing adult TBI. It is possible to measure markers of brain metabolism (glucose, lactate and pyruvate), neurotransmitters (glutamate) and tissue damage (glycerol) at select intervals on small amounts of interstitial fluid collected by the microdialysis catheter inserted into the brain parenchyma alongside the ICP monitor and PbtO2 probe and there are established normal values for adults for some of these chemicals[105]. LPR is of particular interest as it signifies the balance between aerobic and anaerobic metabolism; LPR can also be elevated in states of hyperglycolysis or mitochondrial dysfunction[105,106]. Sustained elevations of LPR have been identified in pericontusional tissue[107] and have been shown to be associated with poor outcome[108]. Similarly, brain glucose levels can be used to guide optimal threshold for blood glucose levels[40]. At present, microdialysis is predominantly used for research purposes, but holds promise for future. Similar to PbtO2 probe, the position of the catheter is crucial and influences the results.
Paediatric TBI is a complex disease and requires multi-disciplinary input. Advancements in the field of paediatric neurocritical care and improved understanding of TBI pathophysiology are being translated to bedside therapies but clinical benefit from most of these therapies is yet to be proved in clinical trials. Despite this, implementations of guideline-based management protocols have impacted significantly on the outcome of TBI in recent years. New monitoring techniques have improved our ability to recognise adverse events and mechanisms of secondary brain injury. The role of these new techniques of individualized management need to be further evaluated.
P- Reviewer: Demirci H, Tanriverdi F S- Editor: Qiu S L- Editor: A E- Editor: Lu YJ
| 1. | Langlois JA, Marr A, Mitchko J, Johnson RL. Tracking the silent epidemic and educating the public: CDC’s traumatic brain injury-associated activities under the TBI Act of 1996 and the Children’s Health Act of 2000. J Head Trauma Rehabil. 2005;20:196-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Faul M, Xu L, Wald MM, Coronado VG. Traumatic brain injury in the United States: emergency department visits, hospitalizations and deaths 2002-2006. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Available from: http://www.cdc.gov/TraumaticBrainInjury. |
| 3. | Tagliaferri F, Compagnone C, Korsic M, Servadei F, Kraus J. A systematic review of brain injury epidemiology in Europe. Acta Neurochir (Wien). 2006;148:255-268; discussion 268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 781] [Cited by in RCA: 743] [Article Influence: 39.1] [Reference Citation Analysis (0)] |
| 4. | Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Shaklai S, Peretz R, Spasser R, Simantov M, Groswasser Z. Long-term functional outcome after moderate-to-severe paediatric traumatic brain injury. Brain Inj. 2014;28:915-921. [PubMed] [DOI] [Full Text] |
| 6. | Pigula FA, Wald SL, Shackford SR, Vane DW. The effect of hypotension and hypoxia on children with severe head injuries. J Pediatr Surg. 1993;28:310-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 219] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 7. | Chesnut RM, Marshall LF, Klauber MR, Blunt BA, Baldwin N, Eisenberg HM, Jane JA, Marmarou A, Foulkes MA. The role of secondary brain injury in determining outcome from severe head injury. J Trauma. 1993;34:216-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1522] [Cited by in RCA: 1335] [Article Influence: 41.7] [Reference Citation Analysis (0)] |
| 8. | Stocchetti N, Furlan A, Volta F. Hypoxemia and arterial hypotension at the accident scene in head injury. J Trauma. 1996;40:764-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 237] [Cited by in RCA: 190] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 9. | Muizelaar JP, Marmarou A, DeSalles AA, Ward JD, Zimmerman RS, Li Z, Choi SC, Young HF. Cerebral blood flow and metabolism in severely head-injured children. Part 1: Relationship with GCS score, outcome, ICP, and PVI. J Neurosurg. 1989;71:63-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 180] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 10. | Andrews PJ, Citerio G. Intracranial pressure. Part one: historical overview and basic concepts. Intensive Care Med. 2004;30:1730-1733. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 31] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Unterberg AW, Stover J, Kress B, Kiening KL. Edema and brain trauma. Neuroscience. 2004;129:1021-1029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 604] [Cited by in RCA: 621] [Article Influence: 29.6] [Reference Citation Analysis (0)] |
| 12. | Advanced Paediatric Life Support: The practical approach. In: Samuels M, Wieteska S, editors. UK: Wiley-Blackwell 2011; 139-200. |
| 13. | Advanced Trauma Life Support: ATLS student course manual. 9th ed. American College of Surgeons Committee on Trauma. UK: Wiley-Blackwell 2012; 246-270. |
| 14. | Kochanek PM, Carney N, Adelson PD, Ashwal S, Bell MJ, Bratton S, Carson S, Chesnut RM, Ghajar J, Goldstein B. Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents--second edition. Pediatr Crit Care Med. 2012;13 Suppl 1:S1-S82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 314] [Article Influence: 24.2] [Reference Citation Analysis (0)] |
| 15. | Pineda JA, Leonard JR, Mazotas IG, Noetzel M, Limbrick DD, Keller MS, Gill J, Doctor A. Effect of implementation of a paediatric neurocritical care programme on outcomes after severe traumatic brain injury: a retrospective cohort study. Lancet Neurol. 2013;12:45-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 16. | Adelson PD, Bratton SL, Carney NA, Chesnut RM, du Coudray HE, Goldstein B, Kochanek PM, Miller HC, Partington MP, Selden NR. Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents. Chapter 19. The role of anti-seizure prophylaxis following severe pediatric traumatic brain injury. Pediatr Crit Care Med. 2003;4:S72-S75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 231] [Cited by in RCA: 209] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 17. | Stiefel MF, Udoetuk JD, Spiotta AM, Gracias VH, Goldberg A, Maloney-Wilensky E, Bloom S, Le Roux PD. Conventional neurocritical care and cerebral oxygenation after traumatic brain injury. J Neurosurg. 2006;105:568-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 133] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 18. | Davis DP, Meade W, Sise MJ, Kennedy F, Simon F, Tominaga G, Steele J, Coimbra R. Both hypoxemia and extreme hyperoxemia may be detrimental in patients with severe traumatic brain injury. J Neurotrauma. 2009;26:2217-2223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 178] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 19. | Lee JH, Kelly DF, Oertel M, McArthur DL, Glenn TC, Vespa P, Boscardin WJ, Martin NA. Carbon dioxide reactivity, pressure autoregulation, and metabolic suppression reactivity after head injury: a transcranial Doppler study. J Neurosurg. 2001;95:222-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 73] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 20. | McLaughlin MR, Marion DW. Cerebral blood flow and vasoresponsivity within and around cerebral contusions. J Neurosurg. 1996;85:871-876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 97] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 21. | Stringer WA, Hasso AN, Thompson JR, Hinshaw DB, Jordan KG. Hyperventilation-induced cerebral ischemia in patients with acute brain lesions: demonstration by xenon-enhanced CT. AJNR Am J Neuroradiol. 1993;14:475-484. [PubMed] |
| 22. | Curry R, Hollingworth W, Ellenbogen RG, Vavilala MS. Incidence of hypo- and hypercarbia in severe traumatic brain injury before and after 2003 pediatric guidelines. Pediatr Crit Care Med. 2008;9:141-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 23. | Weinberg JA. Head trauma. Indian J Pediatr. 1988;55:739-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 24. | Cantor RM, Leaming JM. Evaluation and management of pediatric major trauma. Emerg Med Clin North Am. 1998;16:229-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 25. | Hannon MJ, Crowley RK, Behan LA, O’Sullivan EP, O’Brien MM, Sherlock M, Rawluk D, O’Dwyer R, Tormey W, Thompson CJ. Acute glucocorticoid deficiency and diabetes insipidus are common after acute traumatic brain injury and predict mortality. J Clin Endocrinol Metab. 2013;98:3229-3237. [PubMed] [DOI] [Full Text] |
| 26. | Ulutabanca H, Hatipoglu N, Tanriverdi F, Gökoglu A, Keskin M, Selcuklu A, Kurtoglu S, Kelestimur F. Prospective investigation of anterior pituitary function in the acute phase and 12 months after pediatric traumatic brain injury. Childs Nerv Syst. 2014;30:1021-1028. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 27. | Grände PO, Asgeirsson B, Nordström C. Aspects on the cerebral perfusion pressure during therapy of a traumatic head injury. Acta Anaesthesiol Scand Suppl. 1997;110:36-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 28. | Raju TN, Vidyasagar D, Torres C, Grundy D, Bennett EJ. Intracranial pressure during intubation and anesthesia in infants. J Pediatr. 1980;96:860-862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 56] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 29. | Nilsson B, Rehncrona S, Siesjö BK. Coupling of cerebral metabolism and blood flow in epileptic seizures, hypoxia and hypoglycaemia. Ciba Found Symp. 1978;56:199-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 30. | Vernon DD, Witte MK. Effect of neuromuscular blockade on oxygen consumption and energy expenditure in sedated, mechanically ventilated children. Crit Care Med. 2000;28:1569-1571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 71] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 31. | Greenberg SB, Vender J. The use of neuromuscular blocking agents in the ICU: where are we now? Crit Care Med. 2013;41:1332-1344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 32. | Chin KH, Bell MJ, Wisniewski SR, Balasubramani GK, Kochanek PM, Beers SR, Brown SD, Adelson PD. Effect of administration of neuromuscular blocking agents in children with severe traumatic brain injury on acute complication rates and outcomes: a secondary analysis from a randomized, controlled trial of therapeutic hypothermia. Pediatr Crit Care Med. 2015;16:352-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 33. | Myburgh J, Cooper DJ, Finfer S, Bellomo R, Norton R, Bishop N, Kai Lo S, Vallance S. Saline or albumin for fluid resuscitation in patients with traumatic brain injury. N Engl J Med. 2007;357:874-884. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 577] [Cited by in RCA: 471] [Article Influence: 26.2] [Reference Citation Analysis (0)] |
| 34. | Perel P, Yanagawa T, Bunn F, Roberts I, Wentz R, Pierro A. Nutritional support for head-injured patients. Cochrane Database Syst Rev. 2006;4:CD001530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 44] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 35. | Borzotta AP, Pennings J, Papasadero B, Paxton J, Mardesic S, Borzotta R, Parrott A, Bledsoe F. Enteral versus parenteral nutrition after severe closed head injury. J Trauma. 1994;37:459-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 100] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 36. | Cochran A, Scaife ER, Hansen KW, Downey EC. Hyperglycemia and outcomes from pediatric traumatic brain injury. J Trauma. 2003;55:1035-1038. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 130] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 37. | Michaud LJ, Rivara FP, Longstreth WT, Grady MS. Elevated initial blood glucose levels and poor outcome following severe brain injuries in children. J Trauma. 1991;31:1356-1362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 63] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 38. | Elkon B, Cambrin JR, Hirshberg E, Bratton SL. Hyperglycemia: an independent risk factor for poor outcome in children with traumatic brain injury*. Pediatr Crit Care Med. 2014;15:623-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 39. | Vespa P, Boonyaputthikul R, McArthur DL, Miller C, Etchepare M, Bergsneider M, Glenn T, Martin N, Hovda D. Intensive insulin therapy reduces microdialysis glucose values without altering glucose utilization or improving the lactate/pyruvate ratio after traumatic brain injury. Crit Care Med. 2006;34:850-856. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 215] [Article Influence: 11.3] [Reference Citation Analysis (1)] |
| 40. | Oddo M, Schmidt JM, Carrera E, Badjatia N, Connolly ES, Presciutti M, Ostapkovich ND, Levine JM, Le Roux P, Mayer SA. Impact of tight glycemic control on cerebral glucose metabolism after severe brain injury: a microdialysis study. Crit Care Med. 2008;36:3233-3238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 290] [Cited by in RCA: 270] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 41. | Agbeko RS, Pearson S, Peters MJ, McNames J, Goldstein B. Intracranial pressure and cerebral perfusion pressure responses to head elevation changes in pediatric traumatic brain injury. Pediatr Crit Care Med. 2012;13:e39-e47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 42. | Ng I, Lim J, Wong HB. Effects of head posture on cerebral hemodynamics: its influences on intracranial pressure, cerebral perfusion pressure, and cerebral oxygenation. Neurosurgery. 2004;54:593-597; discussion 598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 122] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 43. | Harris DA, Lam S. Venous thromboembolism in the setting of pediatric traumatic brain injury. J Neurosurg Pediatr. 2014;13:448-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 44. | Hanson SJ, Punzalan RC, Arca MJ, Simpson P, Christensen MA, Hanson SK, Yan K, Braun K, Havens PL. Effectiveness of clinical guidelines for deep vein thrombosis prophylaxis in reducing the incidence of venous thromboembolism in critically ill children after trauma. J Trauma Acute Care Surg. 2012;72:1292-1297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 67] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 45. | Michaud LJ, Rivara FP, Grady MS, Reay DT. Predictors of survival and severity of disability after severe brain injury in children. Neurosurgery. 1992;31:254-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 46. | White JR, Farukhi Z, Bull C, Christensen J, Gordon T, Paidas C, Nichols DG. Predictors of outcome in severely head-injured children. Crit Care Med. 2001;29:534-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 119] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 47. | Jagannathan J, Okonkwo DO, Yeoh HK, Dumont AS, Saulle D, Haizlip J, Barth JT, Jane JA, Jane JA. Long-term outcomes and prognostic factors in pediatric patients with severe traumatic brain injury and elevated intracranial pressure. J Neurosurg Pediatr. 2008;2:240-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 71] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 48. | Alberico AM, Ward JD, Choi SC, Marmarou A, Young HF. Outcome after severe head injury. Relationship to mass lesions, diffuse injury, and ICP course in pediatric and adult patients. J Neurosurg. 1987;67:648-656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 236] [Cited by in RCA: 195] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 49. | Tilford JM, Aitken ME, Anand KJ, Green JW, Goodman AC, Parker JG, Killingsworth JB, Fiser DH, Adelson PD. Hospitalizations for critically ill children with traumatic brain injuries: a longitudinal analysis. Crit Care Med. 2005;33:2074-2081. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 49] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 50. | Chesnut RM, Temkin N, Carney N, Dikmen S, Rondina C, Videtta W, Petroni G, Lujan S, Pridgeon J, Barber J. A trial of intracranial-pressure monitoring in traumatic brain injury. N Engl J Med. 2012;367:2471-2481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 931] [Cited by in RCA: 853] [Article Influence: 65.6] [Reference Citation Analysis (0)] |
| 51. | Chesnut RM, Bleck TP, Citerio G, Classen J, Cooper DJ, Coplin WM, Diringer MN, Grände PO, Hemphill JC, Hutchinson PJ. A Consensus-Based Interpretation of the Benchmark Evidence from South American Trials: Treatment of Intracranial Pressure Trial. J Neurotrauma. 2015;32:1722-1724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 76] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 52. | Bratton SL, Chestnut RM, Ghajar J, McConnell Hammond FF, Harris OA, Hartl R, Manley GT, Nemecek A, Newell DW, Rosenthal G. Guidelines for the management of severe traumatic brain injury. XV. Steroids. J Neurotrauma. 2007;24 Suppl 1:S91-S95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 274] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 53. | Steiner LA, Andrews PJ. Monitoring the injured brain: ICP and CBF. Br J Anaesth. 2006;97:26-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 203] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 54. | Aucoin PJ, Kotilainen HR, Gantz NM, Davidson R, Kellogg P, Stone B. Intracranial pressure monitors. Epidemiologic study of risk factors and infections. Am J Med. 1986;80:369-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 55. | Chambers IR, Treadwell L, Mendelow AD. Determination of threshold levels of cerebral perfusion pressure and intracranial pressure in severe head injury by using receiver-operating characteristic curves: an observational study in 291 patients. J Neurosurg. 2001;94:412-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 88] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 56. | Figaji AA, Zwane E, Thompson C, Fieggen AG, Argent AC, Le Roux PD, Peter JC. Brain tissue oxygen tension monitoring in pediatric severe traumatic brain injury. Part 1: Relationship with outcome. Childs Nerv Syst. 2009;25:1325-1333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 88] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 57. | Narotam PK, Burjonrappa SC, Raynor SC, Rao M, Taylon C. Cerebral oxygenation in major pediatric trauma: its relevance to trauma severity and outcome. J Pediatr Surg. 2006;41:505-513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 63] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 58. | Mendelow AD, Teasdale GM, Russell T, Flood J, Patterson J, Murray GD. Effect of mannitol on cerebral blood flow and cerebral perfusion pressure in human head injury. J Neurosurg. 1985;63:43-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 137] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 59. | James HE. Methodology for the control of intracranial pressure with hypertonic mannitol. Acta Neurochir (Wien). 1980;51:161-172. [PubMed] |
| 60. | Bullock R. Mannitol and other diuretics in severe neurotrauma. New Horiz. 1995;3:448-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 58] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 61. | Fisher B, Thomas D, Peterson B. Hypertonic saline lowers raised intracranial pressure in children after head trauma. J Neurosurg Anesthesiol. 1992;4:4-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 160] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 62. | Peterson B, Khanna S, Fisher B, Marshall L. Prolonged hypernatremia controls elevated intracranial pressure in head-injured pediatric patients. Crit Care Med. 2000;28:1136-1143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 174] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 63. | Zornow MH. Hypertonic saline as a safe and efficacious treatment of intracranial hypertension. J Neurosurg Anesthesiol. 1996;8:175-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 84] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 64. | Suarez JI, Qureshi AI, Bhardwaj A, Williams MA, Schnitzer MS, Mirski M, Hanley DF, Ulatowski JA. Treatment of refractory intracranial hypertension with 23.4% saline. Crit Care Med. 1998;26:1118-1122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 162] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 65. | Vialet R, Albanèse J, Thomachot L, Antonini F, Bourgouin A, Alliez B, Martin C. Isovolume hypertonic solutes (sodium chloride or mannitol) in the treatment of refractory posttraumatic intracranial hypertension: 2 mL/kg 7.5% saline is more effective than 2 mL/kg 20% mannitol. Crit Care Med. 2003;31:1683-1687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 263] [Cited by in RCA: 221] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 66. | Mangat HS, Chiu YL, Gerber LM, Alimi M, Ghajar J, Härtl R. Hypertonic saline reduces cumulative and daily intracranial pressure burdens after severe traumatic brain injury. J Neurosurg. 2015;122:202-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 75] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 67. | Rivkees SA. Differentiating appropriate antidiuretic hormone secretion, inappropriate antidiuretic hormone secretion and cerebral salt wasting: the common, uncommon, and misnamed. Curr Opin Pediatr. 2008;20:448-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 30] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 68. | Heindl UT, Laub MC. Outcome of persistent vegetative state following hypoxic or traumatic brain injury in children and adolescents. Neuropediatrics. 1996;27:94-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 55] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 69. | Hutchison JS, Ward RE, Lacroix J, Hébert PC, Barnes MA, Bohn DJ, Dirks PB, Doucette S, Fergusson D, Gottesman R. Hypothermia therapy after traumatic brain injury in children. N Engl J Med. 2008;358:2447-2456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 503] [Cited by in RCA: 397] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 70. | Adelson PD, Wisniewski SR, Beca J, Brown SD, Bell M, Muizelaar JP, Okada P, Beers SR, Balasubramani GK, Hirtz D. Comparison of hypothermia and normothermia after severe traumatic brain injury in children (Cool Kids): a phase 3, randomised controlled trial. Lancet Neurol. 2013;12:546-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 164] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 71. | Muizelaar JP, Marmarou A, Ward JD, Kontos HA, Choi SC, Becker DP, Gruemer H, Young HF. Adverse effects of prolonged hyperventilation in patients with severe head injury: a randomized clinical trial. J Neurosurg. 1991;75:731-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 889] [Cited by in RCA: 675] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 72. | Skippen P, Seear M, Poskitt K, Kestle J, Cochrane D, Annich G, Handel J. Effect of hyperventilation on regional cerebral blood flow in head-injured children. Crit Care Med. 1997;25:1402-1409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 151] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 73. | Kassell NF, Hitchon PW, Gerk MK, Sokoll MD, Hill TR. Alterations in cerebral blood flow, oxygen metabolism, and electrical activity produced by high dose sodium thiopental. Neurosurgery. 1980;7:598-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 74. | Chen HI, Malhotra NR, Oddo M, Heuer GG, Levine JM, LeRoux PD. Barbiturate infusion for intractable intracranial hypertension and its effect on brain oxygenation. Neurosurgery. 2008;63:880-886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 33] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 75. | Pittman T, Bucholz R, Williams D. Efficacy of barbiturates in the treatment of resistant intracranial hypertension in severely head-injured children. Pediatr Neurosci. 1989;15:13-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 29] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 76. | Roberts I, Sydenham E. Barbiturates for acute traumatic brain injury. Cochrane Database Syst Rev. 2012;12:CD000033. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 67] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 77. | Arndt DH, Lerner JT, Matsumoto JH, Madikians A, Yudovin S, Valino H, McArthur DL, Wu JY, Leung M, Buxey F. Subclinical early posttraumatic seizures detected by continuous EEG monitoring in a consecutive pediatric cohort. Epilepsia. 2013;54:1780-1788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 117] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 78. | Exo J, Kochanek PM, Adelson PD, Greene S, Clark RS, Bayir H, Wisniewski SR, Bell MJ. Intracranial pressure-monitoring systems in children with traumatic brain injury: combining therapeutic and diagnostic tools. Pediatr Crit Care Med. 2011;12:560-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 79. | Baldwin HZ, Rekate HL. Preliminary experience with controlled external lumbar drainage in diffuse pediatric head injury. Pediatr Neurosurg. 1991;17:115-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 28] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 80. | Cooper DJ, Rosenfeld JV, Murray L, Arabi YM, Davies AR, D’Urso P, Kossmann T, Ponsford J, Seppelt I, Reilly P. Decompressive craniectomy in diffuse traumatic brain injury. N Engl J Med. 2011;364:1493-1502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1063] [Cited by in RCA: 1026] [Article Influence: 73.3] [Reference Citation Analysis (0)] |
| 81. | Carrera EC, Steiner LA, Brady K, Zweifel C, Castellani G, Hiler M, Smielewski P, Czosnyka M. Integration of brain signals in multimodal bedside monitoring after traumatic brain injury. Open Neurosurg J. 2010;3:17-27. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 82. | Lassen NA. Cerebral blood flow and oxygen consumption in man. Physiol Rev. 1959;39:183-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 83. | Czosnyka M, Smielewski P, Lavinio A, Pickard JD, Panerai R. An assessment of dynamic autoregulation from spontaneous fluctuations of cerebral blood flow velocity: a comparison of two models, index of autoregulation and mean flow index. Anesth Analg. 2008;106:234-239, table of contents. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 62] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 84. | Panerai RB, Kerins V, Fan L, Yeoman PM, Hope T, Evans DH. Association between dynamic cerebral autoregulation and mortality in severe head injury. Br J Neurosurg. 2004;18:471-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 63] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 85. | Vavilala MS, Lee LA, Boddu K, Visco E, Newell DW, Zimmerman JJ, Lam AM. Cerebral autoregulation in pediatric traumatic brain injury. Pediatr Crit Care Med. 2004;5:257-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 106] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 86. | Figaji AA, Zwane E, Fieggen AG, Argent AC, Le Roux PD, Siesjo P, Peter JC. Pressure autoregulation, intracranial pressure, and brain tissue oxygenation in children with severe traumatic brain injury. J Neurosurg Pediatr. 2009;4:420-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 56] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 87. | Czosnyka M, Smielewski P, Kirkpatrick P, Laing RJ, Menon D, Pickard JD. Continuous assessment of the cerebral vasomotor reactivity in head injury. Neurosurgery. 1997;41:11-17; discussion 17-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 587] [Cited by in RCA: 640] [Article Influence: 22.9] [Reference Citation Analysis (0)] |
| 88. | Budohoski KP, Czosnyka M, de Riva N, Smielewski P, Pickard JD, Menon DK, Kirkpatrick PJ, Lavinio A. The relationship between cerebral blood flow autoregulation and cerebrovascular pressure reactivity after traumatic brain injury. Neurosurgery. 2012;71:652-660; discussion 660-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 108] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 89. | Aries MJ, Czosnyka M, Budohoski KP, Steiner LA, Lavinio A, Kolias AG, Hutchinson PJ, Brady KM, Menon DK, Pickard JD. Continuous determination of optimal cerebral perfusion pressure in traumatic brain injury. Crit Care Med. 2012;40:2456-2463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 354] [Cited by in RCA: 425] [Article Influence: 32.7] [Reference Citation Analysis (0)] |
| 90. | Depreitere B, Güiza F, Van den Berghe G, Schuhmann MU, Maier G, Piper I, Meyfroidt G. Pressure autoregulation monitoring and cerebral perfusion pressure target recommendation in patients with severe traumatic brain injury based on minute-by-minute monitoring data. J Neurosurg. 2014;120:1451-1457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 115] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 91. | Jaeger M, Dengl M, Meixensberger J, Schuhmann MU. Effects of cerebrovascular pressure reactivity-guided optimization of cerebral perfusion pressure on brain tissue oxygenation after traumatic brain injury. Crit Care Med. 2010;38:1343-1347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 115] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 92. | Jaeger M, Schuhmann MU, Soehle M, Meixensberger J. Continuous assessment of cerebrovascular autoregulation after traumatic brain injury using brain tissue oxygen pressure reactivity. Crit Care Med. 2006;34:1783-1788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 153] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 93. | Lewis PM, Czosnyka M, Carter BG, Rosenfeld JV, Paul E, Singhal N, Butt W. Cerebrovascular Pressure Reactivity in Children With Traumatic Brain Injury. Pediatr Crit Care Med. 2015;16:739-749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 54] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 94. | Brady KM, Shaffner DH, Lee JK, Easley RB, Smielewski P, Czosnyka M, Jallo GI, Guerguerian AM. Continuous monitoring of cerebrovascular pressure reactivity after traumatic brain injury in children. Pediatrics. 2009;124:e1205-e1212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 108] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 95. | Ract C, Le Moigno S, Bruder N, Vigué B. Transcranial Doppler ultrasound goal-directed therapy for the early management of severe traumatic brain injury. Intensive Care Med. 2007;33:645-651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 104] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 96. | Bellner J, Romner B, Reinstrup P, Kristiansson KA, Ryding E, Brandt L. Transcranial Doppler sonography pulsatility index (PI) reflects intracranial pressure (ICP). Surg Neurol. 2004;62:45-51; discussion 51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 318] [Cited by in RCA: 302] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 97. | Splavski B, Radanović B, Vranković D, Has B, Muzević D, Janculjak D, Legcević J. Transcranial doppler ultrasonography as an early outcome forecaster following severe brain injury. Br J Neurosurg. 2006;20:386-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 98. | Paulson OB, Strandgaard S, Edvinsson L. Cerebral autoregulation. Cerebrovasc Brain Metab Rev. 1990;2:161-192. [PubMed] |
| 99. | Oddo M, Levine JM, Mackenzie L, Frangos S, Feihl F, Kasner SE, Katsnelson M, Pukenas B, Macmurtrie E, Maloney-Wilensky E. Brain hypoxia is associated with short-term outcome after severe traumatic brain injury independently of intracranial hypertension and low cerebral perfusion pressure. Neurosurgery. 2011;69:1037-1045; discussion 1045. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 92] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 100. | Stippler M, Ortiz V, Adelson PD, Chang YF, Tyler-Kabara EC, Wisniewski SR, Fink EL, Kochanek PM, Brown SD, Bell MJ. Brain tissue oxygen monitoring after severe traumatic brain injury in children: relationship to outcome and association with other clinical parameters. J Neurosurg Pediatr. 2012;10:383-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 101. | Maas AI, Fleckenstein W, de Jong DA, van Santbrink H. Monitoring cerebral oxygenation: experimental studies and preliminary clinical results of continuous monitoring of cerebrospinal fluid and brain tissue oxygen tension. Acta Neurochir Suppl (Wien). 1993;59:50-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 28] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 102. | Maloney-Wilensky E, Gracias V, Itkin A, Hoffman K, Bloom S, Yang W, Christian S, LeRoux PD. Brain tissue oxygen and outcome after severe traumatic brain injury: a systematic review. Crit Care Med. 2009;37:2057-2063. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 149] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 103. | Cormio M, Valadka AB, Robertson CS. Elevated jugular venous oxygen saturation after severe head injury. J Neurosurg. 1999;90:9-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 104. | Jaeger M, Soehle M, Schuhmann MU, Winkler D, Meixensberger J. Correlation of continuously monitored regional cerebral blood flow and brain tissue oxygen. Acta Neurochir (Wien). 2005;147:51-56; discussion 56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 97] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 105. | Hillered L, Vespa PM, Hovda DA. Translational neurochemical research in acute human brain injury: the current status and potential future for cerebral microdialysis. J Neurotrauma. 2005;22:3-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 284] [Cited by in RCA: 242] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 106. | Vespa P, Bergsneider M, Hattori N, Wu HM, Huang SC, Martin NA, Glenn TC, McArthur DL, Hovda DA. Metabolic crisis without brain ischemia is common after traumatic brain injury: a combined microdialysis and positron emission tomography study. J Cereb Blood Flow Metab. 2005;25:763-774. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 472] [Cited by in RCA: 451] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 107. | Vespa PM, O’Phelan K, McArthur D, Miller C, Eliseo M, Hirt D, Glenn T, Hovda DA. Pericontusional brain tissue exhibits persistent elevation of lactate/pyruvate ratio independent of cerebral perfusion pressure. Crit Care Med. 2007;35:1153-1160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 120] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 108. | Timofeev I, Carpenter KL, Nortje J, Al-Rawi PG, O’Connell MT, Czosnyka M, Smielewski P, Pickard JD, Menon DK, Kirkpatrick PJ. Cerebral extracellular chemistry and outcome following traumatic brain injury: a microdialysis study of 223 patients. Brain. 2011;134:484-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 317] [Cited by in RCA: 264] [Article Influence: 18.9] [Reference Citation Analysis (0)] |