Published online Feb 4, 2016. doi: 10.5492/wjccm.v5.i1.103
Peer-review started: August 23, 2015
First decision: October 8, 2015
Revised: December 8, 2015
Accepted: January 8, 2016
Article in press: January 11, 2016
Published online: February 4, 2016
Processing time: 154 Days and 3.7 Hours
AIM: To identify patient, cardiac arrest and management factors associated with hospital survival in comatose survivors of cardiac arrest.
METHODS: A retrospective, single centre study of comatose patients admitted to our intensive care unit (ICU) following cardiac arrest during the twenty year period between 1993 and 2012. This study was deemed by the Human Research Ethics Committee (HREC) of Monash Health to be a quality assurance exercise, and thus did not require submission to the Monash Health HREC (Research Project Application, No. 13290Q). The study population included all patients admitted to our ICU between 1993 and 2012, with a discharge diagnosis including “cardiac arrest”. Patients were excluded if they did not have a cardiac arrest prior to ICU admission (i.e., if their primary arrest was during their admission to ICU), or were not comatose on arrival to ICU. Our primary outcome measure was survival to hospital discharge. Secondary outcome measures were ICU and hospital length of stay (LOS), and factors associated with survival to hospital discharge.
RESULTS: Five hundred and eighty-two comatose patients were admitted to our ICU following cardiac arrest, with 35% surviving to hospital discharge. The median ICU and hospital LOS was 3 and 5 d respectively. There was no survival difference between in-hospital and out-of-hospital cardiac arrests. Males made up 62% of our cardiac arrest population, were more likely to have a shockable rhythm (56% vs 37%, P < 0.001), and were more likely to survive to hospital discharge (40% vs 28%, P = 0.006). On univariate analysis, therapeutic hypothermia, regardless of method used (e.g., rapid infusion of ice cold fluids, topical ice, “Arctic Sun”, passive rewarming, “Bair Hugger”) and location initiated (e.g., pre-hospital, emergency department, intensive care) was associated with increased survival. There was however no difference in survival associated with target temperature, time at target temperature, location of initial cooling, method of initiating cooling, method of maintaining cooling or method of rewarming. Patients that survived were more likely to have a shockable rhythm (P < 0.001), shorter time to return of spontaneous circulation (P < 0.001), receive therapeutic hypothermia (P = 0.03), be of male gender (P = 0.006) and have a lower APACHE II score (P < 0.001). After multivariate analysis, only a shockable initial rhythm (OR = 6.4, 95%CI: 3.95-10.4; P < 0.01) and a shorter time to return of spontaneous circulation (OR = 0.95, 95%CI: 0.93-0.97; P < 0.01) was found to be independently associated with survival to hospital discharge.
CONCLUSION: In comatose survivors of cardiac arrest, shockable rhythm and shorter time to return of spontaneous circulation were independently associated with increased survival to hospital discharge.
Core tip: Admission to intensive care after cardiac arrest is increasing. With the improvements in intensive care practice the survival to hospital discharge is being reported in up to 50% of patients. This study, one of the largest series published so far, was aimed to identify any association between patient factors, cardiac arrest characteristics and post-cardiac arrest management strategies with survival to hospital discharge. The results of this study confirm that of all the factors studied, shockable rhythm and shorter time to return of spontaneous circulation were independently associated with increased survival to hospital discharge.
- Citation: Sathianathan K, Tiruvoipati R, Vij S. Prognostic factors associated with hospital survival in comatose survivors of cardiac arrest. World J Crit Care Med 2016; 5(1): 103-110
- URL: https://www.wjgnet.com/2220-3141/full/v5/i1/103.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v5.i1.103
Cardiovascular disease accounts for 37% of deaths in Australia, the majority being due to cardiac arrest, with an incidence of 148 per 100000[1]. Unconscious survivors of primary cardiac arrest are at high risk of death and neurological injury[2,3]. Hospital survival rates of up to 50% have been described[4,5].
Recent focus on the hospital management of patients following cardiac arrest has been on therapeutic hypothermia, or targeted temperature management (TTM). Therapeutic hypothermia has been described in human survivors of cardiac arrest as early as the 1950’s[6]. Animal studies were undertaken in the early 1990’s[7], followed by feasibility studies on humans[8-10]. Two landmark trials published in 2002[3,11] demonstrated therapeutic hypothermia improved survival and neurological recovery in comatose survivors of out-of-hospital VF arrest. In 2011, two systematic reviews[12,13] showed no benefit of therapeutic hypothermia over normothermia, and in 2013, the “TTM” trial[4] showed no benefit (or harm) between a targeted temperature of 33 °C and a targeted temperature of 36 °C. All TTM trial subjects were also maintained below 37.5 °C for the first 72 h following cardiac arrest, even after rewarming, however this was not the standard practice for our hospital. A higher temperature prior to cooling has already been associated with greater survival[5], however we chose to use the time frame described in the TTM trial (see "MAX-TEMP" below).
A range of different cooling regimes have been described, including “moderate” hypothermia (33 °C for 12 h), 33 °C for 24 h, and “mild” hypothermia (32-34 °C for 24 h)[3,9-11]. Multiple methods have been described for inducing cooling, maintaining cooling and rewarming[3,9,11,14-16]. The optimal approach to inducing and maintaining a targeted temperature remains uncertain[5].
Dandenong Hospital has over twenty years’ experience in the management of comatose survivors of cardiac arrest, providing a large pool of patient data to allow for identification of any association between patient factors, cardiac arrest characteristics and post-cardiac arrest management strategies with survival to hospital discharge.
We undertook a single centre retrospective study at the intensive care unit (ICU) of Dandenong Hospital (DDH). DDH is a 530 bed metropolitan teaching hospital affiliated with Monash University. The emergency department sees 58000 patients per annum, and the hospital has 48000 acute admissions per annum. The ICU is a 14 bed level 2 general ICU with 1100 annual admissions and 8.6% mortality.
This study was deemed by the Human Research Ethics Committee (HREC) of Monash Health to be a quality assurance exercise, and thus did not require submission to the Monash Health HREC (Research Project Application No. 13290Q). The study population included all patients admitted to our ICU between 1993 and 2012, with a discharge diagnosis including “cardiac arrest”. Patients were excluded if they did not have a cardiac arrest prior to ICU admission (i.e., if their primary arrest was during their admission to ICU), or were not comatose on arrival to ICU.
Patients were identified using the ICU database. Acute physiology and chronic health evaluation (APACHE) data (APACHE II and III) were obtained from the ICU database. APACHE data were only available for patients admitted from July 1999. Further patient information was extracted from the hospital medical records. The baseline characteristics collected were age, gender, admission diagnosis, location of cardiac arrest (i.e., in-patient vs out-of-hospital), initial rhythm, time to return of spontaneous circulation, hospital admission source and ICU admission source. Information collected describing management were documentation of therapeutic hypothermia plan, decision to institute cooling, location of initial cooling, method of initiating cooling, method of maintaining cooling, targeted temperature, time taken to achieve target temperature, time at target temperature (both planned and actual), method of rewarming and the maximum temperature reached in the first 72 h following cardiac arrest (MAX-TEMP). The “MAX-TEMP” variable was created to investigate any association between hospital survival and hyperthermia within the first 72 h following cardiac arrest, using the same 37.5 °C cut-off used in the TTM trial.
Primary outcome measure was survival to hospital discharge. Secondary outcome measures were ICU length of stay (LOS), hospital LOS and the patient, cardiac arrest and management factors associated with survival to hospital discharge.
IBM SPSS Statistics (release 22.0.0.0, IBM Corp., Armonk, NY, United States) was used to analyse our data. Continuous data were presented as mean [standard deviation (SD)] and compared using student t-test. Parametric data were presented as median [interquartile range (IQR)] and compared using Mann-Whitney test. Nominal data were analysed using Chi-squared test. Binary logistic regression analysis was used to identify independent associations with hospital survival. P-values less than 0.05 were considered significant.
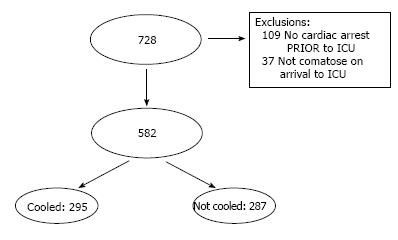
The ICU database search identified 728 patients admitted to our ICU between 1993 and 2012 with a discharge diagnosis including “cardiac arrest” (Figure 1). 109 patients were excluded for not having a cardiac arrest prior to ICU admission and a further 37 patients for not being comatose on arrival to ICU, leaving a total of 582 patients. There were no APACHE data available for patients admitted prior to July 1999 (n = 155, 26.6%). These patients were excluded from further analysis involving APACHE data, but were still included for all other analyses.
Overall survival to hospital discharge was 35%, with median ICU and hospital length of stays (LOS) of 3 and 5 d respectively (Table 1). Table 2 separates our patients into survivors and non-survivors, identifying statistically significant differences in initial rhythm, time to return of spontaneous circulation, APACHE II score, gender and the institution of therapeutic hypothermia. There was no survival difference between in-hospital and out-of-hospital cardiac arrests. Males made up 62% of our cardiac arrest population (Table 1), were more likely to have a shockable rhythm (56% vs 37%, P < 0.001) (data not presented), and were more likely to survive to hospital discharge (40% vs 28%, P = 0.006) (Table 2).
| Variable | All patients n = 582 |
| Patient | |
| Age (yr) - mean (SD) (n = 581) | 63 (16) |
| Gender (male) - n (%) (n = 579) | 361 (62) |
| Cardiac arrest | |
| Time to ROSC (min) - mean (SD) (n = 571) | 23 (15) |
| Presenting rhythm (shockable) - n (%) (n = 582) | 286 (49) |
| Location of arrest (OHCA) - n (%) (n = 582) | 408 (70) |
| Apache 2 score - mean (SD) (n = 427) | 28 (8.4) |
| Apache 3 score - mean (SD) (n = 427) | 78 (37.8) |
| Management | |
| Cooled - n (%) (n = 582) | 295 (51) |
| Target temperature (°C) - median (IQR) (n = 290) | 33 (33-33) |
| Time to temp1 (h) - mean (SD) (n = 288) | 2.1 (3.0) |
| Time at temp2 (h) - median (IQR) (n = 290) | 24 (12-24) |
| Outcome | |
| Survived to hospital discharge - n (%) (n = 582) | 206 (35) |
| ICU LOS (d) - median (IQR) (n = 582) | 3 (1-5) |
| Hospital LOS (d) - median (IQR) (n = 581) | 5 (2-14) |
| Variable | Died n = 376 (65%) | Survived n = 206 (35%) | P value |
| Patient | |||
| Age (yr) - mean (SD) (n = 581) | 64 (17) | 63 (15) | 0.28 |
| Gender (male) - n (%) (n = 579) | 218 (58) | 143 (70) | 0.006 |
| Cardiac arrest | |||
| Time to ROSC (min) - mean (SD) (n = 571) | 26 (14.5) | 18 (14.3) | < 0.001 |
| Presenting rhythm (shockable) - n (%) (n = 582) | 134 (36) | 152 (72) | < 0.001 |
| Location of arrest (OHCA) - n (%) (n = 582) | 269 (72) | 139 (67) | 0.3 |
| Apache 2 score - mean (SD) (n = 427) | 30 (7.6) | 24 (8.5) | < 0.001 |
| Apache 3 score - mean (SD) (n = 427) | 79 (37.9) | 77 (37.8) | 0.5 |
| Management | |||
| Cooled - n (%) (n = 582) | 178 (47) | 117 (57) | 0.03 |
| Target temperature (°C) - median ( IQR) (n = 290) | 33 (33-33) | 33 (33-33) | 0.44 |
| Time to temp1 (h) - mean (SD) (n = 288) | 1.8 (2.9) | 2.5 (3.1) | 0.04 |
| Time at temp2 (h) - median (IQR) (n = 290) | 24 (12-24) | 24 (12-24) | 0.84 |
| Outcome | |||
| ICU LOS (d) - median (IQR) (n = 582) | 2 (1- 4) | 4 (2-7) | < 0.001 |
| Hospital LOS (d) - median (IQR) (n = 581) | 3 (1-6) | 15 (8-27) | < 0.001 |
On univariate analysis, therapeutic hypothermia, regardless of method used (e.g., rapid infusion of ice cold fluids, topical ice, “Arctic Sun”, passive rewarming, “Bair Hugger”) and location initiated (e.g., pre-hospital, emergency department, intensive care) was associated with increased survival (Table 2). There was however no additional difference in survival associated with target temperature, time at target temperature, location of initial cooling, method of initiating cooling, method of maintaining cooling or method of rewarming (data not presented). There was greater survival associated with MAX-TEMP higher than 37.5 °C (41% vs 27%, P < 0.001) (data not presented).
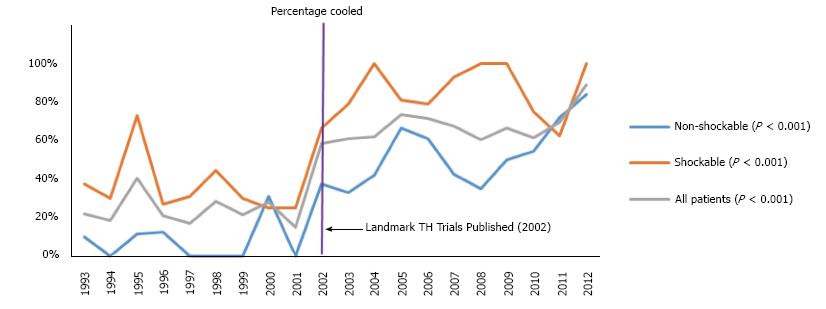
Comparing patients that presented before and after 2002 (Table 3), the second decade had statistically significant increases in non-shockable rhythms, time to return of spontaneous circulation, out-of-hospital cardiac arrests, prescription of therapeutic hypothermia and APACHE II scores. Patients in this group took longer to cool and were cooled for a longer period of time. There was a statistically significant decrease in mean age and a non-significant decrease in survival in the second period. There was a statistically significant increase in ICU LOS, but a non-significant decrease in the hospital LOS in the second period. There was also a statistically significant increase in the implementation of therapeutic hypothermia over the course of the study period (Figure 2).
| Variable | 1993-2002 n = 257 (44%) | 2003-2012 n = 325 (56%) | P value |
| Patient | |||
| Age (yr) - mean (SD) (n = 581) | 65 (15) | 62 (16) | 0.04 |
| Gender (male) - n (%) (n = 579) | 161 (63) | 200 (62) | 0.73 |
| Cardiac arrest | |||
| Time to ROSC (min) - mean (SD) (n = 571) | 21 (14) | 24 (15) | 0.02 |
| Presenting rhythm (shockable) - n (%) (n = 582) | 151 (59) | 135 (42) | < 0.001 |
| Location of arrest (OHCA) - n (%) (n = 582) | 165 (64) | 243 (75) | 0.006 |
| Apache 2 score - mean (SD) (n = 427) | 26 (8.3) | 29 (8.3) | 0.007 |
| Apache 3 score - mean (SD) (n = 427) | 75 (35.9) | 79 (38.2) | 0.23 |
| Management | |||
| Cooled - n (%) (n = 582) | 73 (28) | 222 (68) | < 0.001 |
| Target temperature (°C) - median (IQR) (n = 290) | 33 (33-33) | 33 (33-33) | 0.62 |
| Time to temp1 (h) - mean (SD) (n = 288) | 1.3 (2.2) | 2.4 (3.2) | 0.04 |
| Time at temp2 (h) - median (IQR) (n = 290) | 12 (12-24) | 24 (12-24) | 0.56 |
| Outcome | |||
| Survived to hospital discharge - n (%) (n = 582) | 99 (38) | 107 (33) | 0.16 |
| ICU LOS (d) - median (IQR) (n = 582) | 2 (1-4) | 3 (1-6) | 0.008 |
| Hospital LOS (d) - median (IQR) (n = 581) | 6 (2-15) | 4 (2-13) | 0.18 |
Binary logistic regression analysis identified only a shockable initial rhythm (OR = 6.4, 95%CI: 3.95-10.4; P < 0.01) and a shorter time to return of spontaneous circulation (OR = 0.95, 95%CI: 0.93-0.97; P < 0.01) to be independently associated with survival to hospital discharge (Table 4).
| Variables | B | SE | Wald | df | Sig. | OR | 95%CI | |
| Lower | Upper | |||||||
| ROSC | -0.048 | 0.009 | 27.588 | 1 | 0.000 | 0.953 | 0.937 | 0.971 |
| Shockable rhythm | 1.860 | 0.248 | 56.222 | 1 | 0.000 | 6.422 | 3.949 | 10.441 |
| APACHE II | -0.001 | 0.003 | 0.156 | 1 | 0.693 | 0.999 | 0.993 | 1.005 |
| Therapeutic hypothermia | 0.088 | 0.248 | 0.126 | 1 | 0.722 | 1.092 | 0.672 | 1.775 |
| Gender | -0.456 | 0.247 | 3.388 | 1 | 0.066 | 0.634 | 0.390 | 1.030 |
| Constant | -0.210 | 0.410 | 0.263 | 1 | 0.608 | 0.810 | ||
This twenty year retrospective study identified multiple patient factors, cardiac arrest characteristics and post-cardiac arrest management strategies that were associated with increased survival to hospital discharge in comatose survivors of cardiac arrest.
A shockable rhythm, and a shorter time to return of spontaneous circulation were both associated with increased survival (Table 2). The Victorian Ambulance Cardiac Arrest Register (VACAR)[17] showed there was a higher chance of survival in patients found with a shockable rhythm. In addition, patients found with a shockable rhythm were more likely to have an earlier return of spontaneous circulation and survive to hospital admission[18,19]. These variables were the only two factors identified in our study to be independently associated with survival to hospital discharge following multivariate analysis.
The association between male gender and increased survival to hospital discharge (Table 2) was expected, as men are more likely to have an out-of-hospital cardiac arrest[20], are more likely to survive to hospital admission[21] and are more likely to survive to hospital discharge[19,20]. Men are also more likely to have coronary artery disease and to have a shockable rhythm, both resulting in better survival following cardiac arrest[20,22].
There was a statistically significant association between lower APACHE II scores and increased survival, but not with APACHE III. The original APACHE score included 34 physiological variables[23], which was reduced to 12 with APACHE II, along with inclusions of age, chronic health and surgical procedures[24]. APACHE III was later introduced with 17 physiological variables, increased chronic health categories, less weighting for chronic health and a section for ICU admission source[25]. APACHE IV has subsequently been released, however due to its complexity, APACHE II and APACHE III are still used in mainstream practice[26]. Of the above, only APACHE II measured at 24 h has been shown to correlate with mortality in patients following cardiac arrest[27]. The alteration in the chronic health section and the different weighting given to it, may explain the lack of correlation between the APACHE II and APACHE III scoring systems in our study population.
In addition to the TTM trial[4], there have been many other trials from Scandinavia looking at the management of patients following cardiac arrest[28-31]. Initially, because patients were selected for cooling based on “hypothermia after cardiac arrest” (HACA) inclusion criteria[3], only 28% received therapeutic hypothermia[28]. However, as with our study, the percentage of patients receiving therapeutic hypothermia increased over time (28% in 2007[28], 44% in 2012[29], and 61.7% in 2013[30]) (Figure 2).
Our study identified no association between survival and the location of cooling, method of initiating cooling, method of maintaining cooling or method of rewarming. This may have been confounded by our lack of information on the efficacy of the different cooling strategies implemented. The RICH trial previously documented that pre-hospital cooling added no survival benefit over in-hospital cooling[16]. Other studies have documented the ability of various devices to achieve and maintain a specified temperature[14,15], however it is unclear whether improved efficacy directly translates to improved survival. Despite advances in cooling technology, patients that presented in the second half of the study took longer to achieve target temperature compared to those in the first half (Table 3).
The time of publication of the two practice-changing therapeutic hypothermia trials[3,11] evenly divided our study period into two ten year intervals. Looking at these two periods, there was no statistically significant difference in survival to hospital discharge (Table 3). In fact, there was a non-significant trend to worsening survival (38% vs 33%, P = 0.16), despite a higher percentage of patients being cooled and a younger group of patients. There are a number of explanations for this. To begin with, the latter group had sicker patients, as indicated by a higher mean APACHE II score, which has previously been associated with worse outcomes following cardiac arrest[27]. There was also an increase in non-shockable rhythms and a higher mean time to return of spontaneous circulation, both of which have been associated with worse hospital survival[18,19]. This non-significant decrease in survival also came with the cost of a statistically significant increase in ICU length of stay.
The finding that survival was associated with a higher maximum temperature in the first 72 h (MAX-TEMP) following cardiac arrest (37.4 °C vs 37.9 °C, P = 0.003) was unexpected. Fever is present in 42%-52% of patients post cardiac arrest[32,33], and has previously been associated with a poor outcome[34,35]. A multicentered observational cohort study from Canada, however, identified that a higher temperature prior to cooling was associated with greater survival (35.6 °C vs 36.1 °C, P < 0.0001)[5]. We are uncertain whether a difference of only 0.5 °C in mean temperatures prior to cooling, or maximum temperatures following cardiac arrest, are significant enough to justify having an effect on outcome. In our study, a lower MAX-TEMP was associated with a shorter median ICU LOS (1 d vs 4 d, P = 0.016) implying that many patients in our study may have died while still in the cooling process. In addition, for those regaining consciousness, fever may have been tolerated by the treating team, but we were unable to support this statement with the data available.
Another unexpected finding was the association between a longer time to target temperature and greater survival. We found a difference of 42 min (1.8 h vs 2.5 h, P = 0.04) between the mean time to target temperature of the survivors and non-survivors. This was also noted in the Canadian study mentioned previously, where the difference in means between survivors and non-survivors was 54 min (3.4 h vs 4.3 h, P = 0.001)[5]. We are unsure whether a difference of less than an hour to achieve a target temperature is sufficient to influence survival. Our finding may have been confounded by our study period overlapping with the start of the RINSE trial[36], resulting in the introduction of non-selective pre-hospital cooling and increased number of patients presenting to ICU who were already hypothermic.
Our study had a number of limitations. We undertook a study that was retrospectively analysed and only involved a single site, raising concerns regarding causality and generalizability. Our primary endpoint was hospital survival, and did not include data on functional outcome, nor follow-up post discharge. Our data lacked many peri-arrest details, preventing us from using Utstein reporting. We lacked APACHE data for patients admitted prior to July 1999. Even though our twenty years of study data enabled comparison before and after the practice changing papers, there were also many other major changes, not only in the management of patients following cardiac arrest, but also in ICU management overall. In addition, this period overlapped with many therapeutic hypothermia studies[9,11,16,36], resulting in changes to therapeutic hypothermia protocols, including the introduction of pre-hospital cooling.
Over the twenty years during which this study encompassed, there was no appreciable change in survival to hospital discharge for comatose survivors of cardiac arrest admitted to our ICU. Increased survival to hospital discharge was found to be independently associated with a shockable initial rhythm and a shorter time to return of spontaneous circulation.
A similar study will need to be repeated following the translation of the TTM Trial findings into clinical practice.
Dr. Julian Hunt-Smith, Supervisor of Training, Intensive Care Unit, Royal Melbourne Hospital, 300 Grattan St, Parkville, VIC 3050, Australia. Alexandra Gorelik, Senior Statistician, Melbourne EpiCentre, Royal Melbourne Hospital, 300 Grattan St., Parkville, VIC 3050, Australia.
The intensive care management of patients following cardiac arrest is variable. This is particularly the case with regard to temperature management. Therapeutic hypothermia has been used in patients following cardiac arrest since the 1950’s. However, more than 6 decades later, its role in the management of patients following cardiac arrest, and the parameters targeted, still remain up for debate.
The targeted temperature management (TTM) trial has made us review our original thoughts on the use of therapeutic hypothermia in patients following cardiac arrest, leading to a new era in TTM. These new strategies have now been incorporated into international post-resuscitation guidelines.
This study looks at a twenty-year time period of the treatment of patients following cardiac arrest in a single institution enabling an insight into the practice changes that have occurred.
The study was conducted using retrospective data, allowing us to make a number of associations. Using out findings, further studies can be designed to not only look at temperature as a means of therapy, but potentially also as potential prognostic indicator for patients following cardiac arrest.
“TTM” is a medical therapy where a patient’s core body temperature is actively controlled to maintain a desired level; “Therapeutic hypothermia” is a subset of TTM where the desired core body temperature is set to a target below 35 °C; “Cardiac arrest” is the failure of the heart to pump blood, resulting in cessation of circulation; “Shockable rhythm” is an electrical cardiac rhythm causing a cardiac arrest that may be responsive to cardiac defibrillation, such as ventricular fibrillation and ventricular tachycardia’; “Non-shockable rhythm” is an electrical cardiac rhythm causing a cardiac arrest that is not responsive to cardiac defibrillation, such as asystole and pulseless electrical activity.
This is an interesting article describing the experience of a single center on the outcomes of cardiac arrest patients admitted to the intensive care unit.
P- Reviewer: Jayaraman D, Zhang ZH S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Jennings PA, Cameron P, Walker T, Bernard S, Smith K. Out-of-hospital cardiac arrest in Victoria: rural and urban outcomes. Med J Aust. 2006;185:135-139. [PubMed] |
| 2. | Bernard S. Outcome from prehospital cardiac arrest in Melbourne, Australia. Emerg Med. 1998;10:25-29. [RCA] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 46] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346:549-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3961] [Cited by in RCA: 3780] [Article Influence: 164.3] [Reference Citation Analysis (0)] |
| 4. | Nielsen N, Wetterslev J, Cronberg T, Erlinge D, Gasche Y, Hassager C, Horn J, Hovdenes J, Kjaergaard J, Kuiper M. Targeted temperature management at 33°C versus 36°C after cardiac arrest. N Engl J Med. 2013;369:2197-2206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1992] [Cited by in RCA: 2088] [Article Influence: 174.0] [Reference Citation Analysis (0)] |
| 5. | Lin S, Scales DC, Dorian P, Kiss A, Common MR, Brooks SC, Goodman SG, Salciccioli JD, Morrison LJ. Targeted temperature management processes and outcomes after out-of-hospital cardiac arrest: an observational cohort study*. Crit Care Med. 2014;42:2565-2574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Benson DW, Williams GR, Spencer FC, Yates AJ. The use of hypothermia after cardiac arrest. Anesth Analg. 1959;38:423-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 144] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 7. | Sterz F, Safar P, Tisherman S, Radovsky A, Kuboyama K, Oku K. Mild hypothermic cardiopulmonary resuscitation improves outcome after prolonged cardiac arrest in dogs. Crit Care Med. 1991;19:379-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 270] [Cited by in RCA: 248] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 8. | Zeiner A, Holzer M, Sterz F, Behringer W, Schörkhuber W, Müllner M, Frass M, Siostrzonek P, Ratheiser K, Kaff A. Mild resuscitative hypothermia to improve neurological outcome after cardiac arrest. A clinical feasibility trial. Hypothermia After Cardiac Arrest (HACA) Study Group. Stroke. 2000;31:86-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 169] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 9. | Bernard SA, Jones BM, Horne MK. Clinical trial of induced hypothermia in comatose survivors of out-of-hospital cardiac arrest. Ann Emerg Med. 1997;30:146-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 289] [Cited by in RCA: 262] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 10. | Felberg RA, Krieger DW, Chuang R, Persse DE, Burgin WS, Hickenbottom SL, Morgenstern LB, Rosales O, Grotta JC. Hypothermia after cardiac arrest: feasibility and safety of an external cooling protocol. Circulation. 2001;104:1799-1804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 98] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 11. | Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, Smith K. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346:557-563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4038] [Cited by in RCA: 3811] [Article Influence: 165.7] [Reference Citation Analysis (0)] |
| 12. | Nielsen N, Friberg H, Gluud C, Herlitz J, Wetterslev J. Hypothermia after cardiac arrest should be further evaluated--a systematic review of randomised trials with meta-analysis and trial sequential analysis. Int J Cardiol. 2011;151:333-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 128] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 13. | Walters JH, Morley PT, Nolan JP. The role of hypothermia in post-cardiac arrest patients with return of spontaneous circulation: a systematic review. Resuscitation. 2011;82:508-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 69] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 14. | Mayer SA, Kowalski RG, Presciutti M, Ostapkovich ND, McGann E, Fitzsimmons BF, Yavagal DR, Du YE, Naidech AM, Janjua NA. Clinical trial of a novel surface cooling system for fever control in neurocritical care patients. Crit Care Med. 2004;32:2508-2515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 176] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 15. | Kliegel A, Losert H, Sterz F, Kliegel M, Holzer M, Uray T, Domanovits H. Cold simple intravenous infusions preceding special endovascular cooling for faster induction of mild hypothermia after cardiac arrest--a feasibility study. Resuscitation. 2005;64:347-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 131] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 16. | Bernard SA, Smith K, Cameron P, Masci K, Taylor DM, Cooper DJ, Kelly AM, Silvester W. Induction of therapeutic hypothermia by paramedics after resuscitation from out-of-hospital ventricular fibrillation cardiac arrest: a randomized controlled trial. Circulation. 2010;122:737-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 236] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 17. | Fridman M, Barnes V, Whyman A, Currell A, Bernard S, Walker T, Smith KL. A model of survival following pre-hospital cardiac arrest based on the Victorian Ambulance Cardiac Arrest Register. Resuscitation. 2007;75:311-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 58] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 18. | Bernard S. Hypothermia after cardiac arrest: expanding the therapeutic scope. Crit Care Med. 2009;37:S227-S233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 50] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 19. | Herlitz J, Engdahl J, Svensson L, Angquist KA, Young M, Holmberg S. Factors associated with an increased chance of survival among patients suffering from an out-of-hospital cardiac arrest in a national perspective in Sweden. Am Heart J. 2005;149:61-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 147] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 20. | Akahane M, Ogawa T, Koike S, Tanabe S, Horiguchi H, Mizoguchi T, Yasunaga H, Imamura T. The effects of sex on out-of-hospital cardiac arrest outcomes. Am J Med. 2011;124:325-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 87] [Article Influence: 6.2] [Reference Citation Analysis (1)] |
| 21. | Kitamura T, Kiyohara K, Iwami T. The great east Japan earthquake and out-of-hospital cardiac arrest. N Engl J Med. 2013;369:2165-2167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 22. | Albert CM, McGovern BA, Newell JB, Ruskin JN. Sex differences in cardiac arrest survivors. Circulation. 1996;93:1170-1176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 151] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 23. | Knaus WA, Zimmerman JE, Wagner DP, Draper EA, Lawrence DE. APACHE-acute physiology and chronic health evaluation: a physiologically based classification system. Crit Care Med. 1981;9:591-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1381] [Cited by in RCA: 1435] [Article Influence: 32.6] [Reference Citation Analysis (33)] |
| 24. | Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818-829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10902] [Cited by in RCA: 11135] [Article Influence: 278.4] [Reference Citation Analysis (0)] |
| 25. | Knaus WA, Wagner DP, Draper EA, Zimmerman JE, Bergner M, Bastos PG, Sirio CA, Murphy DJ, Lotring T, Damiano A. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991;100:1619-1636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2591] [Cited by in RCA: 2719] [Article Influence: 80.0] [Reference Citation Analysis (0)] |
| 26. | Niewiński G, Starczewska M, Kański A. Prognostic scoring systems for mortality in intensive care units--the APACHE model. Anaesthesiol Intensive Ther. 2014;46:46-49. [PubMed] |
| 27. | Donnino MW, Salciccioli JD, Dejam A, Giberson T, Giberson B, Cristia C, Gautam S, Cocchi MN. APACHE II scoring to predict outcome in post-cardiac arrest. Resuscitation. 2013;84:651-656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 47] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 28. | Oksanen T, Pettilä V, Hynynen M, Varpula T. Therapeutic hypothermia after cardiac arrest: implementation and outcome in Finnish intensive care units. Acta Anaesthesiol Scand. 2007;51:866-871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 44] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 29. | Reinikainen M, Oksanen T, Leppänen P, Torppa T, Niskanen M, Kurola J. Mortality in out-of-hospital cardiac arrest patients has decreased in the era of therapeutic hypothermia. Acta Anaesthesiol Scand. 2012;56:110-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 30. | Vaahersalo J, Hiltunen P, Tiainen M, Oksanen T, Kaukonen KM, Kurola J, Ruokonen E, Tenhunen J, Ala-Kokko T, Lund V. Therapeutic hypothermia after out-of-hospital cardiac arrest in Finnish intensive care units: the FINNRESUSCI study. Intensive Care Med. 2013;39:826-837. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 108] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 31. | Lindner TW, Langørgen J, Sunde K, Larsen AI, Kvaløy JT, Heltne JK, Draegni T, Søreide E. Factors predicting the use of therapeutic hypothermia and survival in unconscious out-of-hospital cardiac arrest patients admitted to the ICU. Crit Care. 2013;17:R147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 52] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 32. | Gebhardt K, Guyette FX, Doshi AA, Callaway CW, Rittenberger JC. Prevalence and effect of fever on outcome following resuscitation from cardiac arrest. Resuscitation. 2013;84:1062-1067. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 97] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 33. | Cocchi MN, Boone MD, Giberson B, Giberson T, Farrell E, Salciccioli JD, Talmor D, Williams D, Donnino MW. Fever after rewarming: incidence of pyrexia in postcardiac arrest patients who have undergone mild therapeutic hypothermia. J Intensive Care Med. 2013;29:365-369. [PubMed] |
| 34. | Bro-Jeppesen J, Hassager C, Wanscher M, Søholm H, Thomsen JH, Lippert FK, Møller JE, Køber L, Kjaergaard J. Post-hypothermia fever is associated with increased mortality after out-of-hospital cardiac arrest. Resuscitation. 2013;84:1734-1740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 116] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 35. | Leary M, Grossestreuer AV, Iannacone S, Gonzalez M, Shofer FS, Povey C, Wendell G, Archer SE, Gaieski DF, Abella BS. Pyrexia and neurologic outcomes after therapeutic hypothermia for cardiac arrest. Resuscitation. 2013;84:1056-1061. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 101] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 36. | Deasy C, Bernard S, Cameron P, Jacobs I, Smith K, Hein C, Grantham H, Finn J. Design of the RINSE trial: the rapid infusion of cold normal saline by paramedics during CPR. BMC Emerg Med. 2011;11:17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |