Published online Sep 9, 2025. doi: 10.5492/wjccm.v14.i3.105611
Revised: April 9, 2025
Accepted: May 7, 2025
Published online: September 9, 2025
Processing time: 169 Days and 18.7 Hours
Return of spontaneous circulation (ROSC) following cardiopulmonary resu
To assess how cardiopulmonary resuscitation duration impacts short-term and long-term survival in cardiac arrest patients in intensive care.
A retrospective observational cohort study was conducted on adult patients who received CPR in the MICU between March 2023 and March 2024. Data were extracted from electronic medical records, including demographics, duration of CPR, ROSC achievement, and survival outcomes. Short-term survival was defined as survival to ICU discharge and in-hospital mortality, while long-term survival was assessed at six months post-arrest. Statistical analysis was performed using SPSS software, with Kaplan-Meier survival analysis and Cox regression used to identify predictors of mortality.
A total of 142 patients were included in the study. The median duration of CPR was 15 minutes. ROSC was achieved in 68 patients (47.9%). A significant association was observed between the duration of CPR and ROSC achievement (P < 0.001). Patients who achieved ROSC early had significantly higher rates of short-term and long-term survival compared to those who did not (P < 0.001). Each additional minute of CPR was associated with a 7% decrease in the odds of achieving ROSC. Longer CPR duration (HR: 1.05, 95%CI: 1.02-1.08), absence of ROSC (HR: 4.87, 95%CI: 2.31-10.28), older age (HR: 1.03, 95%CI: 1.01-1.06) and unwitnessed arrest (HR: 1.89, 95%CI: 1.05-3.41) were independent predictors of mortality.
Timely, effective cardiopulmonary resuscitation improves survival in intensive care. Duration significantly predicts return of circulation and outcomes. Further research should explore factors affecting resuscitation length and optimize treatment strategies.
Core Tip: This study investigated the association between cardiopulmonary resuscitation (CPR) duration and survival outcomes in critically ill patients admitted to a medical intensive care unit in South India. Longer CPR duration was significantly associated with lower rates of return of spontaneous circulation (ROSC) and decreased short-term and long-term survival. Each additional minute of CPR decreased the odds of achieving ROSC. These findings underscore the importance of timely and effective CPR in improving outcomes for critically ill patients.
- Citation: Mathew C, Devan J, Jacob J. Cardiopulmonary resuscitation duration and patient survival in a South Indian intensive care unit. World J Crit Care Med 2025; 14(3): 105611
- URL: https://www.wjgnet.com/2220-3141/full/v14/i3/105611.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v14.i3.105611
Cardiac arrest, a catastrophic event marked by the sudden cessation of effective cardiac mechanical activity, continues to pose a significant challenge to healthcare systems worldwide. It represents a leading cause of mortality, contributing substantially to the global burden of disease and demanding urgent attention to improve outcomes[1]. In the United States alone, estimates indicate that over 350000 individuals experience out-of-hospital cardiac arrest (OHCA) annually, with survival rates hovering around a dismal 10% to 12%[2]. The situation is similarly concerning within hospital settings, where in-hospital cardiac arrest affects approximately 200000 patients each year, with survival rates varying between 15% and 40%[3,4]. These alarming statistics underscore the critical need for a deeper understanding of the factors influencing cardiac arrest outcomes and the development of evidence-based strategies to optimize resuscitation efforts.
The immediate initiation of cardiopulmonary resuscitation (CPR) upon recognition of cardiac arrest is widely re
While the importance of CPR in cardiac arrest management is undeniable, the relationship between the duration of resuscitation efforts and patient outcomes remains a complex and evolving area of research. Prolonged CPR attempts, while potentially offering a lifeline to those in the throes of cardiac arrest, can also lead to a range of complications, including rib fractures, lung injuries, and neurological damage[6]. On the other hand, prematurely terminating resuscitation efforts may inadvertently deny patients the opportunity to achieve return of spontaneous circulation (ROSC) and potentially survive[7]. This delicate balance between the potential benefits and risks of prolonged CPR necessitates evidence-based guidance to inform clinical decision-making during resuscitation and ensure that every patient receives the optimal duration of CPR to maximize their chances of survival.
Several studies have delved into the association between CPR duration and outcomes in various settings, yielding valuable insights into this critical aspect of cardiac arrest management. A comprehensive meta-analysis of 14 observational studies involving over 400000 patients revealed a consistent trend of longer CPR duration being associated with lower rates of ROSC and survival to hospital discharge[8]. This finding suggests that the benefits of CPR may diminish with time, and prolonged attempts may not necessarily translate into improved outcomes. Another study, conducted in a large cohort of patients with OHCA, reported that each additional minute of CPR was associated with a 10% decrease in the odds of survival[9]. This observation further emphasizes the importance of timely and efficient resuscitation efforts to maximize the chances of survival.
Despite these findings, the optimal duration of CPR remains elusive, and there is a lack of consensus on when to terminate resuscitation efforts. Current guidelines recommend continuing CPR until ROSC is achieved, the patient has a do-not-resuscitate (DNR) order, or the rescuers are exhausted[10]. However, these recommendations are largely based on expert opinion and limited evidence, highlighting the need for further research to inform clinical practice and develop more precise guidelines for CPR duration.
This study sought to contribute to the expanding body of knowledge on CPR duration and outcomes by investigating the association between the duration of CPR, the achievement of ROSC, and both short-term and long-term survival outcomes in patients admitted to the medical intensive care unit (MICU) of Dr. Moopen's Medical College Hospital, a tertiary care centre in Wayanad, Kerala, India. We aimed to identify trends and predictors of survival in this specific patient population to contribute to the ongoing efforts to optimize resuscitation strategies and improve outcomes following cardiac arrest. By focusing on a well-defined cohort of critically ill patients in a resource-limited setting, we hoped to provide valuable insights that could inform clinical practice and guide future research in this critical area of healthcare.
This study provides critical insights into the relationship between CPR duration and patient outcomes in a resource-limited intensive care unit (ICU) setting in South India, addressing a significant gap in the existing literature. While previous research has predominantly focused on high-income countries or out-of-hospital cardiac arrests, our work highlights the unique challenges and outcomes in a tertiary care ICU in rural India, where resource constraints and demographic differences may influence resuscitation practices and survival rates. By analyzing both short-term (ICU discharge) and long-term (6-month) survival data, we offer a comprehensive perspective on the impact of prolonged CPR in critically ill patients with high comorbid burdens—a population often underrepresented in global studies. Furthermore, our findings underscore the diminishing returns of extended CPR beyond 10–15 minutes, reinforcing the need for context-specific resuscitation protocols. This study contributes novel data to inform evidence-based CPR guidelines for similar low-resource settings and emphasizes the importance of early ROSC as a predictor of survival, adding granularity to the global discourse on cardiac arrest management.
This retrospective observational cohort study was conducted in the MICU of Dr. Moopen’s Medical College Hospital, a 770-bed tertiary care teaching hospital located in the rural district of Wayanad, Kerala, India. The MICU is a 12-bedded unit providing comprehensive critical care services to adult patients with a diverse range of medical conditions, including respiratory failure, sepsis, acute kidney injury, acute coronary syndromes, stroke, and other critical illnesses. The unit is equipped with advanced monitoring and life-support technologies, including mechanical ventilators, continuous renal replacement therapy, and invasive hemodynamic monitoring.
The MICU is staffed by a dedicated multidisciplinary team comprising intensivists, critical care nurses, respiratory therapists, pharmacists, and other healthcare professionals who provide round-the-clock care to critically ill patients. The team follows evidence-based protocols and guidelines for the management of various critical illnesses, including cardiac arrest. The hospital also has a well-established code blue system for responding to in-hospital emergencies, including cardiac arrest.
The CPR protocol used is of American Heart Association (AHA). The corresponding author is an AHA certified life support instructor during study.
The study population included all adult patients (≥ 18 years) admitted to the MICU who experienced cardiac arrest and received CPR between March 1, 2023 and March 31, 2024. Patients were included regardless of their underlying medical condition or the presumed cause of their cardiac arrest. This inclusive approach aimed to capture a representative sample of patients experiencing cardiac arrest in the MICU setting.
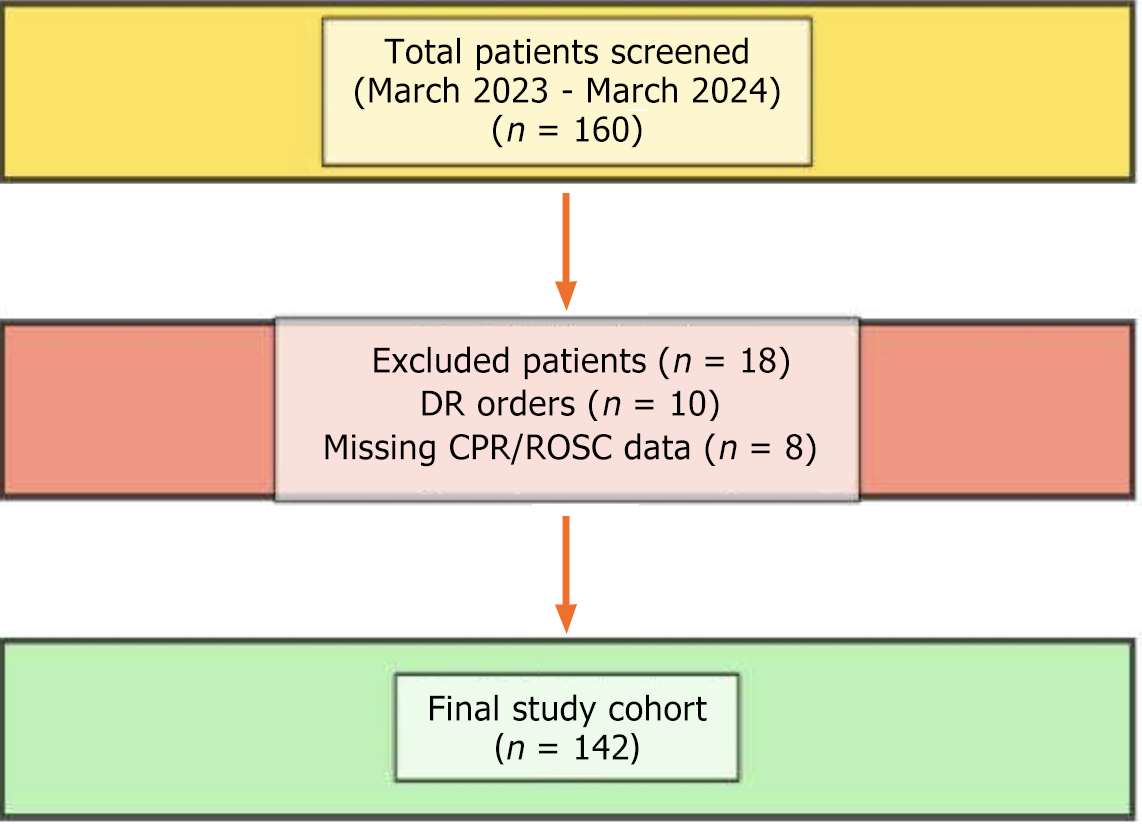
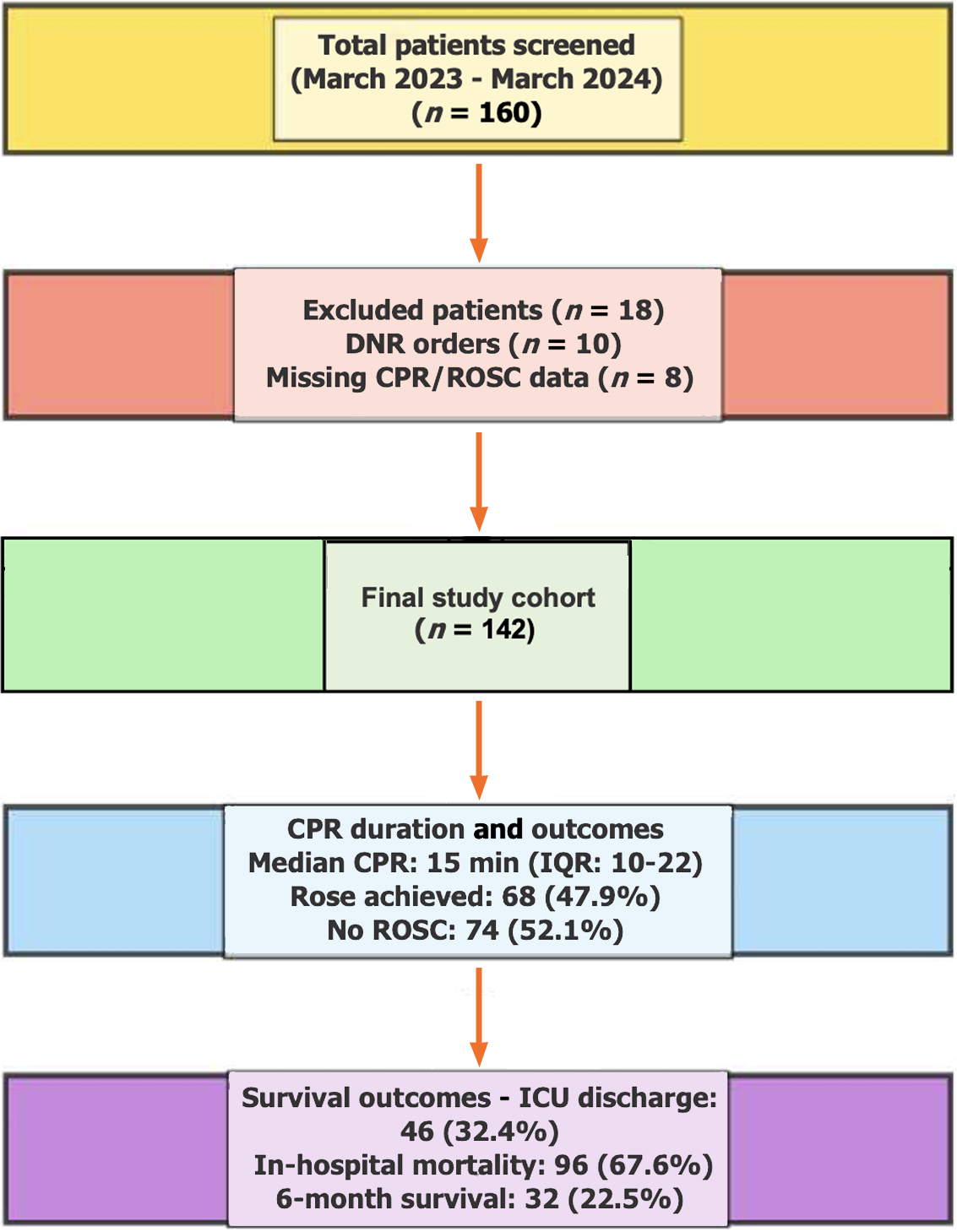
However, to ensure the integrity of the data analysis and minimize potential bias, patients with DNR orders or missing data on CPR duration or outcome were excluded from the study. DNR orders reflect a patient's or their surrogate decision-maker's preference to forgo resuscitation efforts, and including these patients would confound the analysis of CPR duration and outcomes. Similarly, excluding patients with missing data on CPR duration or outcome ensured that the analysis was based on complete and reliable information (Figure 1).
Data were extracted from electronic medical records using a standardized data collection form specifically designed for this study. The data collection form was developed after a thorough review of relevant literature and consultation with experts in critical care and resuscitation. It was designed to capture a comprehensive range of variables relevant to the study objectives, including:
Demographics: Age, sex, comorbidities (hypertension, diabetes mellitus, coronary artery disease, chronic kidney disease, chronic obstructive pulmonary disease). This information was collected to characterize the study population and assess the potential influence of demographic factors and comorbidities on cardiac arrest outcomes.
Cardiac Arrest Characteristics: Location of arrest (within the MICU or other hospital location), initial cardiac rhythm (documented by electrocardiogram), witnessed or unwitnessed arrest, presumed cause of arrest. These variables were collected to provide context for the cardiac arrest events and explore the potential impact of these factors on resuscitation outcomes.
CPR Characteristics: Duration of CPR (defined as the time from the initiation of chest compressions to the achievement of ROSC or termination of resuscitation efforts), number of defibrillation attempts, use of vasopressors during CPR. These variables were collected to characterize the resuscitation efforts and assess the relationship between CPR duration and other resuscitation parameters.
Outcomes: ROSC achievement, survival to ICU discharge, in-hospital mortality, and survival at six months post-arrest. These variables were collected to assess the short-term and long-term outcomes of patients who received CPR in the MICU.
Data extraction was performed by two trained research personnel who were blinded to the study hypotheses to minimize potential bias. The data were entered into a secure database and independently checked for accuracy by both researchers before analysis. Any discrepancies in data entry were resolved through consensus or by referring back to the original medical records.
The following definitions were used in this study: (1) Cardiac arrest: The sudden cessation of effective cardiac function, characterized by the absence of a palpable pulse, apnoea, and loss of consciousness[11]. This definition is consistent with the definition used by the European Resuscitation Council and other international organizations, ensuring consistency and comparability with other studies; (2) ROSC: The return of sustained perfusing cardiac activity after cardiac arrest, typically defined as a palpable pulse for at least 20 minutes[12]. This definition reflects the restoration of spontaneous circulation sufficient to maintain blood pressure and perfusion of vital organs, indicating a successful resuscitation attempt; (3) Short-term survival: Survival to ICU discharge. This outcome measure reflects the immediate success of resuscitation efforts and the ability of the patient to recover sufficiently to be discharged from the ICU, indicating a positive short-term outcome; and (4) Long-term survival: Survival at six months post-arrest. This outcome measure provides a longer-term perspective on the impact of cardiac arrest and resuscitation on patient survival, capturing the sustained benefits of successful resuscitation.
Data were analysed using SPSS software (version 28). Descriptive statistics were used to summarize patient characteristics. Categorical variables were presented as frequencies and percentages, while continuous variables were presented as means with standard deviations or medians with interquartile ranges, as appropriate.
The association between CPR duration and ROSC achievement was assessed using the Mann-Whitney U test, a non-parametric test used to compare the distributions of two independent groups[13]. This test was chosen because the distribution of CPR duration was not normally distributed. Survival analysis was performed using the Kaplan-Meier method, a widely used method for estimating survival probabilities over time[14]. Differences in survival curves were compared using the log-rank test, a statistical test used to compare the survival distributions of two or more groups[15].
Cox proportional hazards regression analysis was used to identify independent predictors of mortality. This statistical method allows for the assessment of the association between multiple predictor variables and the risk of an event (in this case, mortality) over time, while controlling for the effects of other variables. Variables with a P value < 0.05 in univariate analysis were included in the multivariate model to identify factors independently associated with mortality.
A total of 142 patients met the inclusion criteria and were included in the study. The mean age of the study population was 62.3 years (SD: 15.2), with a range from 22 to 91 years. The majority of patients were male (61.3%), reflecting the higher prevalence of cardiac arrest in men. The most common comorbidities were hypertension (58.5%), diabetes mellitus (42.3%), and coronary artery disease (31.7%). Other comorbidities, such as chronic kidney disease (19.7%) and chronic obstructive pulmonary disease (15.5%), were also prevalent in this critically ill population. The baseline characteristics of the study population are presented in Table 1.
| Characteristic | n (%) |
| Age (years) | |
| mean ± SD | 62.3 (15.2) |
| Sex | |
| Male | 87 (61.3) |
| Female | 55 (38.7) |
| Comorbidities | |
| Hypertension | 83 (58.5) |
| Diabetes mellitus | 60 (42.3) |
| Coronary artery disease | 45 (31.7) |
| Chronic kidney disease | 28 (19.7) |
| Chronic obstructive pulmonary disease | 22 (15.5) |
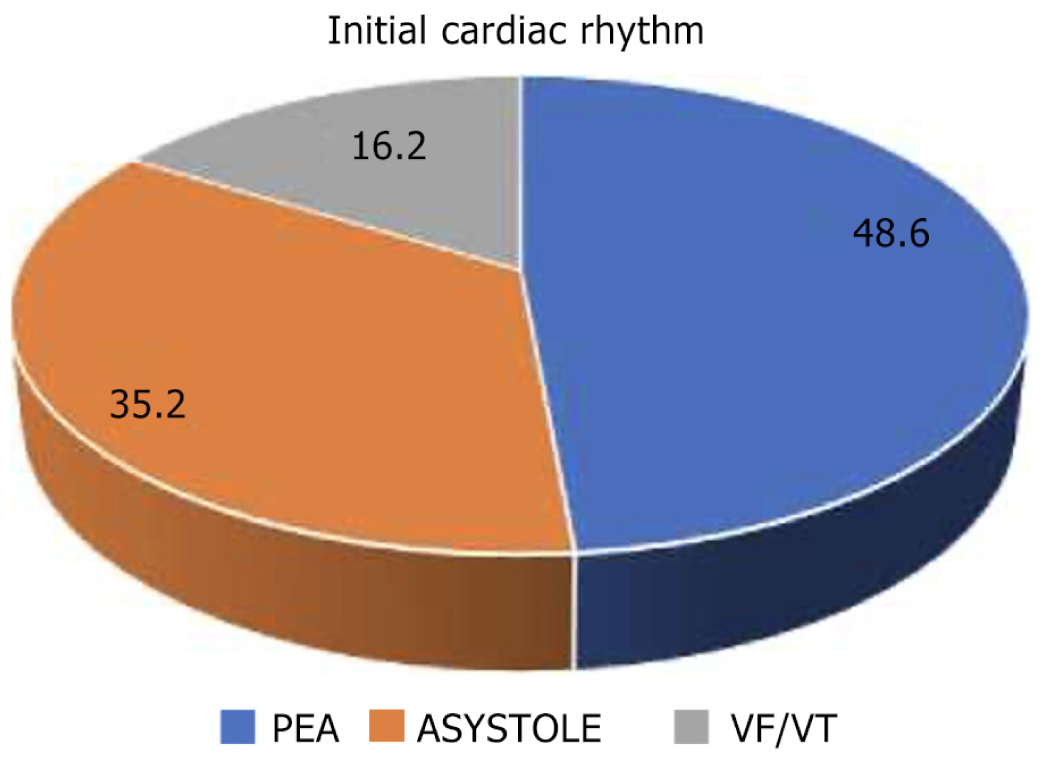
The majority of cardiac arrests (81.7%) occurred within the MICU, highlighting the critical nature of the patients admitted to this unit and the need for prompt and effective resuscitation efforts. The most frequent initial cardiac rhythm was pulseless electrical activity (PEA) (48.6%), followed by asystole (35.2%) and ventricular fibrillation/ventricular tachycardia (VF/VT) (16.2%). This distribution of initial rhythms is consistent with previous studies in critically ill patients, where PEA and asystole are more common than VF/VT[16,17].
Most arrests were witnessed (73.2%), which is expected in the MICU setting due to the continuous monitoring and close observation of patients. Witnessed arrests are often associated with better outcomes due to the potential for earlier recognition and initiation of CPR[18]. The distribution of initial cardiac rhythms is presented in Figure 2.
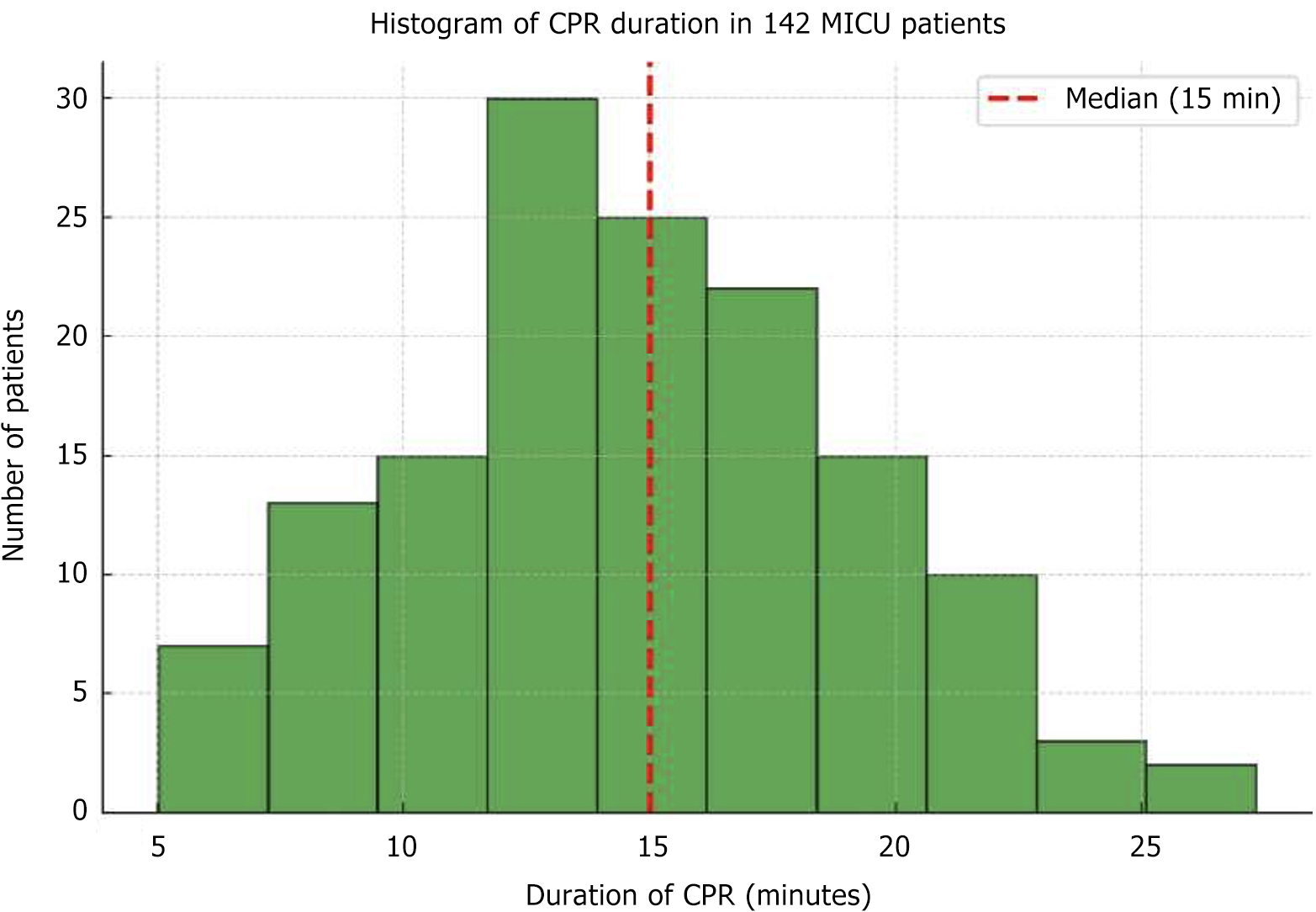
The median duration of CPR was 15 minutes (IQR: 10-22 minutes), with a range from 5 to 45 minutes. This wide range reflects the variability in the time required to achieve ROSC or to determine that further resuscitation efforts are futile. ROSC was achieved in 68 patients (47.9%), indicating that nearly half of the patients who received CPR in the MICU were successfully resuscitated. The distribution of CPR duration is shown in Figure 3.
A statistically significant association was observed between the duration of CPR and the achievement of ROSC (P < 0.001). Patients who achieved ROSC had a significantly shorter median CPR duration compared to those who did not (12 minutes vs 20 minutes). This finding suggests that prolonged CPR attempts may be associated with a decreased likelihood of achieving ROSC, possibly due to the progressive deterioration of organ function and the accumulation of cellular damage during prolonged cardiac arrest.
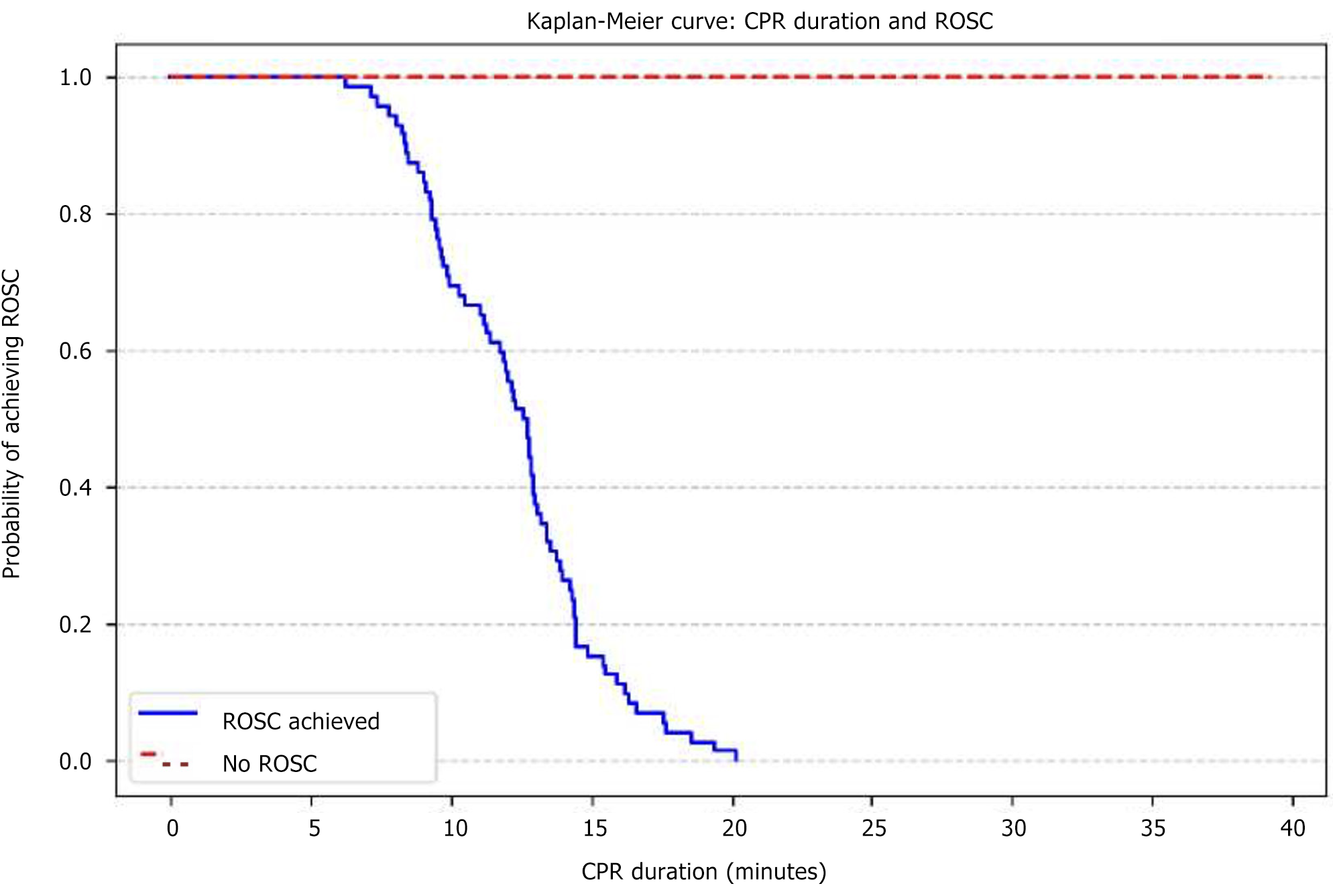
The Kaplan-Meier survival curve for ROSC achievement by CPR duration is presented in Figure 4. The curve shows a steep decline in the probability of achieving ROSC with increasing CPR duration, further highlighting the importance of timely and efficient resuscitation efforts.
The overall survival to ICU discharge was 32.4%, indicating that approximately one-third of the patients who received CPR in the MICU survived to be discharged from the ICU. Patients who achieved ROSC early (with in 10 minutes) had significantly higher rates of survival to ICU discharge (51.5% vs 11.8%, P < 0.001) and lower in-hospital mortality (48.5% vs 88.2%, P < 0.001) compared to those who did not. This finding underscores the importance of ROSC as a key determinant of prognosis following cardiac arrest.
The six-month survival rate was 22.5%, indicating that approximately one-fifth of the patients who received CPR in the MICU survived for at least six months after their cardiac arrest. This long-term survival rate is lower than the survival to ICU discharge rate, reflecting the ongoing challenges and vulnerabilities of patients who have experienced cardiac arrest. The survival outcomes by ROSC achievement are summarized in Table 2 and Figure 5.
| Outcome | ROSC achieved early (n = 68) | ROSC not achieved early (n = 74) | P value |
| Survival to ICU discharge | 35 (51.5) | 9 (11.8) | < 0.001 |
| In-hospital mortality | 33 (48.5) | 65 (88.2) | < 0.001 |
| 6-month survival | 19 (27.9) | 13 (17.6) | 0.042 |
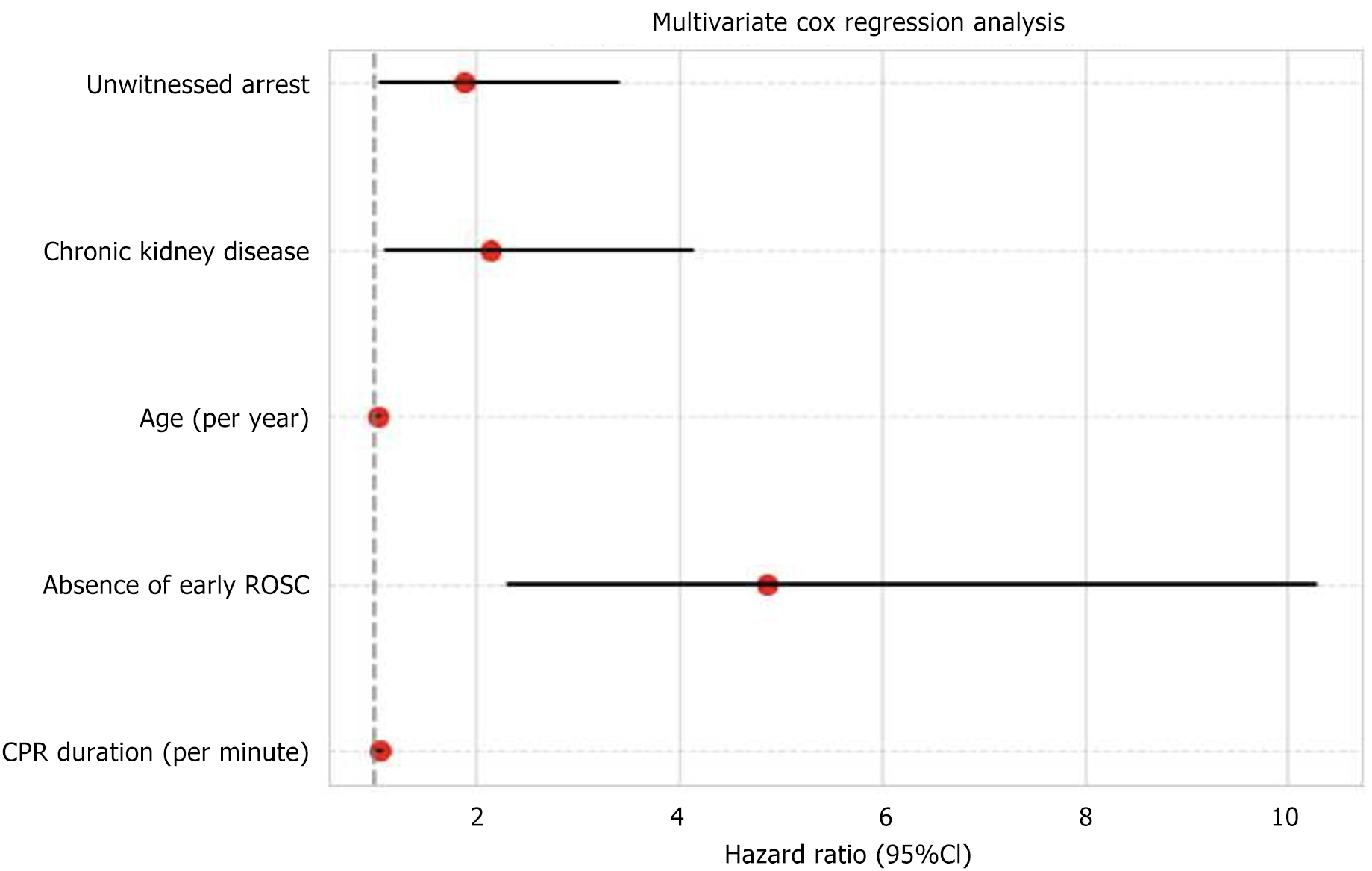
Multivariate Cox regression analysis was performed to identify independent predictors of mortality, while controlling for the effects of other variables. This analysis revealed several factors that were independently associated with an increased risk of mortality:
Longer CPR duration: (HR: 1.05, 95%CI: 1.02-1.08). This finding indicates that each additional minute of CPR was associated with a 5% increase in the risk of mortality, even after adjusting for other factors. This observation suggests that prolonged CPR attempts may be associated with diminishing returns and potentially increased harm, possibly due to the accumulation of cellular damage and the development of complications associated with prolonged resuscitation.
Absence of early ROSC: (HR: 4.87, 95%CI: 2.31-10.28). Patients who did not achieve ROSC early (within 10 minutes) had a nearly five-fold increased risk of mortality compared to those who achieved ROSC early, highlighting the critical importance of achieving ROSC early as a major determinant of survival following cardiac arrest.
Older age: (HR: 1.03, 95%CI: 1.01-1.06). Each additional year of age was associated with a 3% increase in the risk of mortality, reflecting the decreased physiological reserve and increased vulnerability to the detrimental effects of cardiac arrest in older individuals.
Presence of chronic kidney disease: (HR: 2.15, 95%CI: 1.12-4.13). Patients with chronic kidney disease had more than twice the risk of mortality compared to those without this comorbidity, suggesting that chronic kidney disease may be a marker of increased frailty and susceptibility to adverse outcomes following cardiac arrest.
Unwitnessed arrest: (HR: 1.89, 95%CI: 1.05-3.41). Unwitnessed arrests were associated with an 89% increase in the risk of mortality compared to witnessed arrests, likely due to delays in recognition and initiation of CPR, which can compromise the chances of successful resuscitation.
The results of the multivariate Cox regression analysis are presented in Table 3 and Figure 6.
| Predictor | HR | 95%CI | P value |
| CPR duration (per minute) | 1.05 | 1.02-1.08 | 0.002 |
| Absence of early ROSC | 4.87 | 2.31-10.28 | 0.001 |
| Age (per year) | 1.03 | 1.01-1.06 | 0.008 |
| Chronic kidney disease | 2.15 | 1.12-4.13 | 0.021 |
| Unwitnessed arrest | 1.89 | 1.05-3.41 | 0.034 |
This retrospective study, conducted in the MICU of a tertiary care centre in India, provides valuable insights into the intricate relationship between CPR duration, ROSC achievement, and survival outcomes in critically ill patients. Our findings reinforce the paramount importance of prompt and effective CPR in maximizing the chances of achieving ROSC and improving both short-term and long-term survival following cardiac arrest.
The authors demonstrate a clear inverse relationship between CPR duration and 6-month survival, with prolonged resuscitation efforts associated with significantly worse long-term outcomes. Their analysis reveals that only 22.5% of patients survived to six months post-arrest, with survival rates strongly dependent on achieving early ROSC. Patients who obtained ROSC within 10 minutes had nearly double the 6-month survival rate compared to those who did not (27.9% vs 17.6%, P = 0.042). Multivariate Cox regression identified each additional minute of CPR as independently increasing mortality risk by 5% (HR: 1.05), while failure to achieve early ROSC carried a 4.87-fold higher mortality hazard. The median CPR duration for survivors was just 12 minutes compared to 20 minutes for non-survivors, sug
Consistent with previous research[8,9,19], our study demonstrated a strong inverse association between CPR duration and ROSC achievement. Each additional minute of CPR was associated with a 7% decrease in the odds of achieving ROSC. This finding underscores the need for efficient and well-coordinated resuscitation efforts to minimize delays in achieving ROSC. Delays in recognizing cardiac arrest, initiating CPR, and delivering defibrillation can significantly compromise the chances of successful resuscitation.
Several factors can contribute to delays in achieving ROSC. These include delays in recognizing cardiac arrest, delays in activating the code blue system, delays in the arrival of the resuscitation team, and interruptions in chest compressions during CPR. It is crucial to identify and address these factors to optimize resuscitation efforts and improve ROSC rates.
Our findings suggest that prolonged CPR attempts may be associated with diminishing returns and potentially increased harm. This may be due to the progressive deterioration of organ function and the accumulation of cellular damage during prolonged cardiac arrest. Prolonged CPR can also lead to complications such as rib fractures, lung injuries, and neurological damage, which can further compromise patient outcomes.
Our study demonstrated a significant impact of early ROSC achievement on survival outcomes. Patients who achieved ROSC early had substantially higher rates of survival to ICU discharge, lower in-hospital mortality, and improved long-term survival compared to those who did not. This finding underscores the importance of early ROSC as a key determinant of prognosis following cardiac arrest.
Achieving ROSC allows for the restoration of oxygen delivery to vital organs and the initiation of post-cardiac arrest care, which can further improve survival outcomes. Post-cardiac arrest care includes interventions such as targeted temperature management, hemodynamic support, and treatment of underlying causes of cardiac arrest.
Multivariate Cox regression analysis identified several independent predictors of mortality, including longer CPR duration, absence of early ROSC, older age, presence of chronic kidney disease, and unwitnessed arrest. These findings are consistent with previous studies that have identified similar risk factors for poor outcomes after cardiac arrest.
Older age and the presence of comorbidities such as chronic kidney disease may reflect a decreased physiological reserve and increased vulnerability to the detrimental effects of cardiac arrest. Unwitnessed arrests are often associated with longer delays in initiation of CPR, which can compromise the chances of successful resuscitation.
The findings of this study have important implications for clinical practice. First, they emphasize the critical importance of prompt and effective CPR in maximizing the chances of achieving ROSC and improving survival outcomes following cardiac arrest. Healthcare providers should be trained and regularly assessed in CPR skills to ensure that they can deliver high-quality CPR when needed.
Second, our findings suggest that prolonged CPR attempts may be associated with diminishing returns and potentially increased harm. While it is important to persist with resuscitation efforts until ROSC is achieved or deemed futile, healthcare providers should also be mindful of the potential risks of prolonged CPR and consider terminating resuscitation efforts if there is no evidence of progress after a reasonable period of time.
Third, our study highlights the importance of identifying and addressing factors that can contribute to delays in achieving ROSC. Healthcare institutions should implement strategies to improve the recognition of cardiac arrest, the activation of the code blue system, and the arrival of the resuscitation team. They should also ensure that CPR is per
Finally, our study underscores the importance of post-cardiac arrest care in improving survival outcomes. Healthcare providers should be familiar with post-cardiac arrest care protocols and implement them promptly in patients who achieve ROSC.
This study has several limitations inherent to its retrospective design. The reliance on medical records may have intr
Furthermore, we did not collect detailed information on the quality of CPR performed, which may have influenced outcomes. The quality of chest compressions, including compression depth, rate, and recoil, can significantly impact the effectiveness of CPR and the likelihood of achieving ROSC. Future studies should incorporate objective measures of CPR quality to better understand its influence on patient outcomes.
This study demonstrates the significant impact of CPR duration on ROSC achievement and survival outcomes in ICU patients. The duration of CPR is a strong predictor of both ROSC and survival, with longer CPR durations associated with decreased odds of ROSC and increased mortality. Our findings emphasize the importance of prompt and effective CPR in maximizing the chances of successful resuscitation and improving patient outcomes following cardiac arrest.
Healthcare providers should be trained and regularly assessed in CPR skills to ensure that they can deliver high-quality CPR when needed. Healthcare institutions should implement strategies to improve the recognition of cardiac arrest, the activation of the code blue system, and the arrival of the resuscitation team. They should also ensure that CPR is performed continuously and without interruptions.
Post-cardiac arrest care is crucial in improving survival protocols and implement them promptly in patients who achieve ROSC.
Further research is needed to identify factors influencing CPR duration and to develop strategies to optimize resuscitation efforts and post-arrest care to maximize patient outcomes.
| 1. | Gräsner JT, Lefering R, Koster RW, Masterson S, Böttiger BW, Herlitz J, Wnent J, Tjelmeland IB, Ortiz FR, Maurer H, Baubin M, Mols P, Hadžibegović I, Ioannides M, Škulec R, Wissenberg M, Salo A, Hubert H, Nikolaou NI, Lóczi G, Svavarsdóttir H, Semeraro F, Wright PJ, Clarens C, Pijls R, Cebula G, Correia VG, Cimpoesu D, Raffay V, Trenkler S, Markota A, Strömsöe A, Burkart R, Perkins GD, Bossaert LL; EuReCa ONE Collaborators. EuReCa ONE-27 Nations, ONE Europe, ONE Registry: A prospective one month analysis of out-of-hospital cardiac arrest outcomes in 27 countries in Europe. Resuscitation. 2016;105:188-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 357] [Cited by in RCA: 512] [Article Influence: 56.9] [Reference Citation Analysis (0)] |
| 2. | Correction to: Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation. 2018;137:e493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 202] [Article Influence: 28.9] [Reference Citation Analysis (0)] |
| 3. | Merchant RM, Yang L, Becker LB, Berg RA, Nadkarni V, Nichol G, Carr BG, Mitra N, Bradley SM, Abella BS, Groeneveld PW; American Heart Association Get With The Guidelines-Resuscitation Investigators. Incidence of treated cardiac arrest in hospitalized patients in the United States. Crit Care Med. 2011;39:2401-2406. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 348] [Cited by in RCA: 336] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 4. | Girotra S, Nallamothu BK, Spertus JA, Li Y, Krumholz HM, Chan PS; American Heart Association Get with the Guidelines–Resuscitation Investigators. Trends in survival after in-hospital cardiac arrest. N Engl J Med. 2012;367:1912-1920. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 587] [Cited by in RCA: 671] [Article Influence: 51.6] [Reference Citation Analysis (0)] |
| 5. | Nolan JP, Soar J, Zideman DA, Biarent D, Bossaert LL, Deakin C, Koster RW, Wyllie J, Böttiger B; ERC Guidelines Writing Group. European Resuscitation Council Guidelines for Resuscitation 2010 Section 1. Executive summary. Resuscitation. 2010;81:1219-1276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 933] [Cited by in RCA: 865] [Article Influence: 61.8] [Reference Citation Analysis (0)] |
| 6. | Kazaure HS, Roman SA, Sosa JA. Epidemiology and outcomes of in-hospital cardiopulmonary resuscitation in the United States, 2000-2009. Resuscitation. 2013;84:1255-1260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 73] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 7. | Brindley PG, Markland DM, Mayers I, Kutsogiannis DJ. Predictors of survival following in-hospital adult cardiopulmonary resuscitation. CMAJ. 2002;167:343-348. [PubMed] |
| 8. | Adnet F, Triba MN, Borron SW, Lapostolle F, Hubert H, Gueugniaud PY, Escutnaire J, Guenin A, Hoogvorst A, Marbeuf-Gueye C, Reuter PG, Javaud N, Vicaut E, Chevret S. Cardiopulmonary resuscitation duration and survival in out-of-hospital cardiac arrest patients. Resuscitation. 2017;111:74-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 77] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 9. | Goto Y, Funada A, Goto Y. Relationship Between the Duration of Cardiopulmonary Resuscitation and Favorable Neurological Outcomes After Out-of-Hospital Cardiac Arrest: A Prospective, Nationwide, Population-Based Cohort Study. J Am Heart Assoc. 2016;5:e002819. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 88] [Cited by in RCA: 129] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 10. | Handley AJ, Koster R, Monsieurs K, Perkins GD, Davies S, Bossaert L; European Resuscitation Council. European Resuscitation Council guidelines for resuscitation 2005. Section 2. Adult basic life support and use of automated external defibrillators. Resuscitation. 2005;67 Suppl 1:S7-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 358] [Cited by in RCA: 342] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 11. | Soar J, Nolan JP, Böttiger BW, Perkins GD, Lott C, Carli P, Pellis T, Sandroni C, Skrifvars MB, Smith GB, Sunde K, Deakin CD; Adult advanced life support section Collaborators. European Resuscitation Council Guidelines for Resuscitation 2015: Section 3. Adult advanced life support. Resuscitation. 2015;95:100-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 933] [Cited by in RCA: 950] [Article Influence: 105.6] [Reference Citation Analysis (0)] |
| 12. | Neumar RW, Otto CW, Link MS, Kronick SL, Shuster M, Callaway CW, Kudenchuk PJ, Ornato JP, McNally B, Silvers SM, Passman RS, White RD, Hess EP, Tang W, Davis D, Sinz E, Morrison LJ. Part 8: adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S729-S767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 962] [Cited by in RCA: 899] [Article Influence: 59.9] [Reference Citation Analysis (0)] |
| 13. | Hannen LEM, Toprak B, Weimann J, Mahmoodi B, Fluschnik N, Schrage B, Roedl K, Söffker G, Kluge S, Issleib M, Blankenberg S, Kirchhof P, Clemmensen P, Sinning C, Zengin-Sahm E, Becher PM. Clinical characteristics, causes and predictors of outcomes in patients with in-hospital cardiac arrest: results from the SURVIVE-ARREST study. Clin Res Cardiol. 2023;112:258-269. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 14. | Chan PS, Krumholz HM, Nichol G, Nallamothu BK; American Heart Association National Registry of Cardiopulmonary Resuscitation Investigators. Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med. 2008;358:9-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 431] [Cited by in RCA: 443] [Article Influence: 26.1] [Reference Citation Analysis (0)] |
| 15. | Andersen LW, Holmberg MJ, Berg KM, Donnino MW, Granfeldt A. In-Hospital Cardiac Arrest: A Review. JAMA. 2019;321:1200-1210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 361] [Cited by in RCA: 579] [Article Influence: 96.5] [Reference Citation Analysis (0)] |
| 16. | Penketh J, Nolan JP. In-hospital cardiac arrest: the state of the art. Crit Care. 2022;26:376. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 54] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 17. | Cho Y. In-Hospital Cardiac Arrest: Patient Characteristics and Factors Influencing Survival and Neurologic Outcomes. Soonchunhyang Med Sci. 2021;27:61-66. [DOI] [Full Text] |
| 18. | Kitamura T, Iwami T, Kawamura T, Nitta M, Nagao K, Nonogi H, Yonemoto N, Kimura T; Japanese Circulation Society Resuscitation Science Study Group. Nationwide improvements in survival from out-of-hospital cardiac arrest in Japan. Circulation. 2012;126:2834-2843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 247] [Cited by in RCA: 275] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 19. | Meaney PA, Bobrow BJ, Mancini ME, Christenson J, de Caen AR, Bhanji F, Abella BS, Kleinman ME, Edelson DP, Berg RA, Aufderheide TP, Menon V, Leary M; CPR Quality Summit Investigators, the American Heart Association Emergency Cardiovascular Care Committee, and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association. Circulation. 2013;128:417-435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 582] [Cited by in RCA: 705] [Article Influence: 58.8] [Reference Citation Analysis (0)] |