Published online Jan 9, 2023. doi: 10.5492/wjccm.v12.i1.29
Peer-review started: September 18, 2022
First decision: September 27, 2022
Revised: October 7, 2022
Accepted: November 29, 2022
Article in press: November 29, 2022
Published online: January 9, 2023
Processing time: 107 Days and 7.7 Hours
Diabetic ketoacidosis (DKA) and hyperglycemic hyperosmolar state (HHS) are common acute complications of diabetes mellitus with a high risk of mortality. When combined with hypernatremia, the complications can be even worse. Hypernatremia is a rarely associated with DKA and HHS as both are usually accompanied by normal sodium or hyponatremia. As a result, a structured and systematic treatment approach is critical. We discuss the therapeutic approach and implications of this uncommon presentation.
A 62-year-old man with no known past medical history presented to emergency department with altered mental status. Initial work up in emergency room showed severe hyperglycemia with a glucose level of 1093 mg/dL and severe hypernatremia with a serum sodium level of 169 mEq/L. He was admitted to the intensive care unit (ICU) and was started on insulin drip as per DKA protocol. Within 12 h of ICU admission, blood sugar was 300 mg/dL. But his mental status didn’t show much improvement. He was dehydrated and had a corrected serum sodium level of > 190 mEq/L. As a result, dextrose 5% in water and ringer's lactate were started. He was also given free water via an nasogastric (NG) tube and IV Desmopressin to improve his free water deficit, which improved his serum sodium to 140 mEq/L.
The combination of DKA, HHS and hypernatremia is rare and extremely cha
Core Tip: Hyperglycemia is usually associated with hyperkalemia, but it is rare to see hypernatremia with hyperglycemia as hyperglycemia is usually seen with pseudohyponatremia. Correcting hypernatremia with hyperglycemia is challenging because of the complex fluid requirements in this situation. We are describing a case here with severe hyperglycemia and severe hypernatremia. In our case, we have used free water flushes via nasogastric access and desmopressin to correct the free water deficit, which hasn't been described previously in the literature. This makes our case unique.
- Citation: Lathiya MK, Errabelli P, Cullinan SM, Amadi EJ. Severe hypernatremia in hyperglycemic conditions; managing it effectively: A case report. World J Crit Care Med 2023; 12(1): 29-34
- URL: https://www.wjgnet.com/2220-3141/full/v12/i1/29.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v12.i1.29
Diabetic ketoacidosis (DKA) and hyperglycemic hyperosmolar state (HHS) are common acute complications of diabetes mellitus (DM) with a high risk of mortality. DKA is more common in patients with type 1 diabetes (T1DM), whereas HHS is more common in patients with type 2 diabetes. However, symptoms of DKA and HHS can sometimes overlap and result in a combined laboratory presentation of both conditions[1]. When it comes to managing this overlap presentation, glucose levels, electrolyte levels, and the patient's hemodynamics are all closely monitored because DKA and HHS can cause serious complications like brain edema, rhabdomyolysis, thrombosis[1]. When combined with hype
We present a case of successfully treated severe hypernatremia in an adult with DKA-HHS.
A 62-year-old male, who has not seen a physician for more than a decade presented to a local Eme
He has no known prior medical history.
Not a known alcoholic or a smoker. No history of illicit substance use. No family history of any chronic medical conditions.
He was evaluated in the ED and workup was negative for neurologic findings.
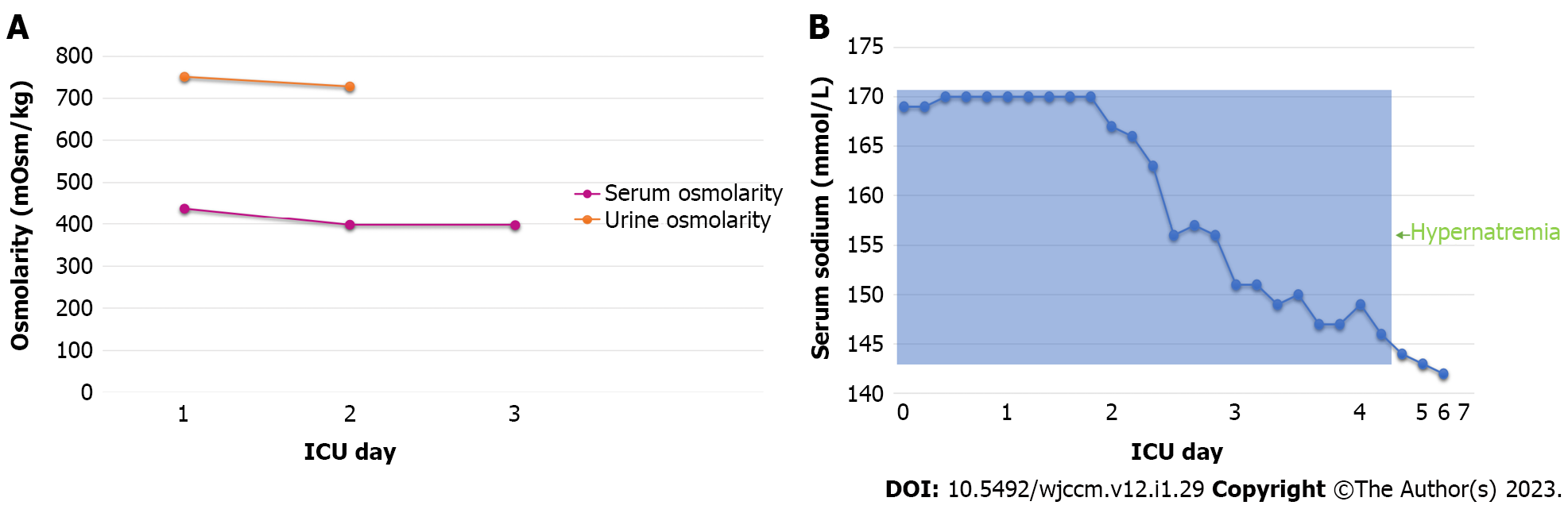
His initial workup revealed sodium 169 mEq/L (Corrected sodium for hyperglycemia is 193 mEq/L), chloride 124 mEq/L, blood glucose 1093 mg/dL, bicarbonate 16 mEq/L, anion gap of 29, serum creatinine 2.27 mg/dL (baseline creatinine was 0.7), and potassium 4.6 mEq/L. Urine osmolality was 751 mOsm/kg, while serum osmolarity was 438 mOsm/kg (Figure 1). In the emergency department, HbA1c was > 18%, Serum lactate was 4.6 and the pH of venous blood gas was 7.33. During hospitalization, his serum bicarbonate, serum lactate, and anion gap were also elevated (Table 1). His arterial blood gas levels were determined during his hospitalization (Table 2). In addition, we have added his fluid balance and diuresis in the period of the first 5 d (Table 3).
| Indicator | Normal value | In the Emergency Department day 1 | Hospital day 2 | Hospital day 3 | Hospital day 4 | Hospital day 5 |
| Serum sodium (Na) | 135-145 mmol/L | 169 | ||||
| Serum chloride (Cl) | 98-107 mmol/L | 124 | ||||
| HCO3- | 22-29 mmol/L | 16 | 24 | 26 | 24 | 21 |
| Glucose | 70-140 mg/dL | 1093 | ||||
| Serum creatinine (Cr) | 0.74-1.35 mg/dL | 2.27 | ||||
| Serum potassium (K) | 3.6-5.2 mmol/L | 4.6 | ||||
| Serum lactate | 5.2-2.2 mmol/L | 4.1 | 4.6 | 3.9 | 1.6 | |
| Serum osmolarity | 276-306 mOsm/kg | 438 | ||||
| Urine osmolarity | 150-1150 mOsm/kg | 751 | ||||
| HbA1c | 5.7%-6.4% | > 18% | ||||
| pH venous blood Gas | 7.32-7.43 | 7.33 | ||||
| Anion gap | 7-15 | 29 | 24 | 16 | 10 | 12 |
| Fio2/Spo2 | 96%-99%/95%-100% | None/92% | 2 Liter (nasal cannula)/92%-98% | Room Air/94%-100% |
| Arterial blood gas | Normal range | Hospital day 1 | Hospital day 2 |
| PH | 7.35-7.45 pH | 7.43; 7.45; 7.48 | 7.51 |
| PCO2 | 35-48 mmHg | 30; 28; 25 | 26 |
| PO2 | 28-108 mmHg | 78; 73; 72 | 78 |
| Day (Hospital period) | Fluid intake (mL) | Fluid output (mL) |
| 1 | 5381 | 950 |
| 2 | 6200 | 2935 |
| 3 | 2650 | 1900 |
| 4 | 1900 | 1205 |
| 5 | 3987 | 1925 |
DKA and Hyperosmolar hyperglycemic syndrome with hyperglycemia-induced hypernatremia were the definitive diagnoses in the case described.
He was started on an insulin drip per DKA protocol and was admitted to the intensive care unit (ICU). On initial evaluation, his calculated serum sodium at this point was > 170 mEq/L and his free water deficit was close to 29 L. After 12 h of admission, the blood sugar was corrected to 300 mg/dL, but serum sodium remained elevated at > 170 mEq/L. Urine output remained suboptimal at 1.09 mL/kg/hr. He was hyperventilating and blood gas showed a PH 7.51, and a PCO2 of 26. Creatine pho
Twenty-four hours after above interventions, serum sodium slowly dropped to 167 mEq/L (Figure 1B), creatinine improved to 1.9 mg/dL (from 2.27 mg/dL) and urine output improved. Desmopressin was continued until serum sodium corrected to 140 mEq/L. At this point his mental status had returned to baseline and NG tube free water replacement was discontinued. Patient eventually recovered with normalization of electrolytes and renal function at the time of discharge. He was discharged on insulin for newly diagnosed DM and atorvastatin for newly diagnosed hyperlipidemia with dietary recommendations.
After 24 h, we were able to achieve the desired decline in sodium level, improvement in both serum creatinine and urine output, improvement in urine and serum osmolarity (Figure 1A) and improvement in the mental status of the patient, suggesting that the altered mental status was driven by his severe hypernatremia.
Complications associated with undiagnosed and untreated DM can be disastrous, especially over an extended duration. The onset and development of this complex disease in our patient is particularly difficult to track due to a prolonged period of health care avoidance. However, the critical state of the patient upon presenting to the ED highlights the severity of several consequences, namely hyper
Hypernatremia, an elevated level of serum sodium, can be attributed to multiple processes, including hypertonic fluid gain, hypotonic fluid loss, or general water depletion. No matter the origin, the increased extracellular osmolality drives water outward from cells, resulting in cell shrinking. Although an ionic osmolytic response serves to counter these dangerous effects, long-term damage is nearly inevitable. Such impairments manifest in various organ systems leading to short-term mortality rates between 50% and 60%[3]. Our patient’s initial measured sodium level of > 170 mEq/L that later progressed to > 200 mEq/L indicated a precarious and time-sensitive situation requiring urgent intervention.
The development of hypernatremia in this patient should be considered in both DKA and HHS, in addition to the combination of these conditions. The appearance of hypernatremia in DKA can be attributed to a fluid imbalance. As significant volumes of free fluid are lost (most commonly by polyuria), electrolyte loss (through vomiting and diarrhea) may lag behind, leading to a very unusual occurrence of hypernatremia with osmolytic imbalance[4]. Although such cases of DKA-induced hypernatremia are infrequent, a 2019 paper reviews the cases of two female patients found to be suffering from hypernatremia secondary to DKA after complaints of altered mental status and other symptoms[5]. Additionally, a 2020 study describes an altered male T1DM patient with a largely unknown medical history suffering from DKA and severe hypernatremia; aggressive treatment of DKA and fluid management yielded a positive outcome. While DKA and HHS diverge in incidence, mechanism, and prognosis, the rare occurrence of hypernatremia in HHS arises for similar reasons: A free water deficit develops through osmotic diuresis. A 2020 case report discusses a female patient with no known history of DM that presented to the ED for confusion amongst many other progressive symptoms. Investigations revealed extremely elevated blood glucose and sodium levels, which led to a diagnosis of HHS[6]. Our case differs from previous literature in that the patient was diagnosed with DKA, HHS, and acute hypernatremia. While a combination of these three constituents is detailed in a 2020 paper referencing two pediatric patients, this combination, to our knowledge, has not been identified in an adult patient[1].
The precise origin of hypernatremia in this patient is complicated by the patient’s past medical history. For one, the incompleteness of his record, due to a ten-plus year hiatus from receiving even primary care, abridges available information to a matter of days before admission. Also, the polydipsia described by the patient himself led to the unintentional ingestion of excessive amounts of sodium, primarily through his beverages of choice. Nevertheless, the patient’s hyperglycemia, hypernatremia, and free water deficit necessitated careful manipulation as a 2022 case series study describes the cases of DKA-HHS induced severe hypernatremia in three adolescents due to high soft drink consumption where one patient died due to development of severe hypovolemia[7]. As increased consumption of carbohydrate-rich beverages exacerbated glucose induced osmotic diuresis and resulted in worsening severe intravascular dehydration. To restore the water deficit, a large amount of fluid is needed. It is also important to choose right fluid to correct plasma sodium level with the aim of avoiding treatment-related dysnatremia. As an improper management of plasma sodium concentration and plasma osmolality during treatment has been associated with two rare potentially life-threatening complications such as hypovolemic shock, cerebral edema and osmotic demyelination syndrome. Previous literature suggests that the correction of hypernatremia is best achieved through the intravenous administration of a hypotonic solution such as D5W and safest as long as the etiology of hypernatremia is hypertonic sodium gain and treatment can be initiated at ≤ 12 h from the onset of the cause[8]. Since this patient’s free water deficit was 29 L, effective fluid resuscitation required D5W, Ringer’s lactate, and enteral free water for prompt change. The rate of sodium correction should be based on the type of fluid used. Although the blood glucose level was unusually high (300 mg/dL) to initiate D5W, we planned to perform fluid resuscitation with Ringer's lactate and D5W, which resulted in a slower decrease in serum sodium when compared to other isotonic or hypotonic fluids alone. In addition, we started giving free fluid via NG tube. According to de Vos and van der Voort[9], treating patients with ICU-induced hypernatremia with enteral free water did not result in a clinically significant decrease in serum sodium levels[9]. However, we noticed improving sodium as we combined desmopressin to conserve free water by its antidiuretic effects. After 24 h, we were able to achieve the desired decline in sodium level, improvement in both serum creatinine and urine output, improvement in urine and serum osmolarity (Figure 1A), and improvement in the mental status of the patient, suggesting the altered mental status was driven primarily by the hypernatremia.
This case report highlights three vital considerations when treating patients with hypernatremia in the DKA-HHS overlap disease state. First, the decision to treat hyperglycemia more aggressively than hypernatremia due to the intrinsic life-threatening risks. Second, at the initial stage, choosing a combination of hypotonic and isotonic fluid that contains sodium close to the lower limit of normal serum sodium allows glucose to decrease first, at the same time maintaining serum sodium at steady-state and not increasing. Third, giving water via oral, NG, or orogastric tube in combination with desmopressin to improve free water deficit and to prevent excessive hypotonic and/or isotonic fluid induced complications such as peripheral edema and pulmonary edema. This case report highlights the importance of understanding the management approach required for hypernatremia in DKA-HHS to prevent complications associated with these two conditions.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Critical care medicine
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Papadopoulos VP, Greece; Yahaya TO, Nigeria S-Editor: Wei ZH L-Editor: A P-Editor: Wei ZH
| 1. | Shima S, Umino S, Kitamura M, Ushijima K, Yatsuga S. Severe Hypernatremia in Combined Diabetic Ketoacidosis and Hyperglycemic Hyperosmolar State: A Case Report of Two Japanese Children. Cureus. 2020;12:e9672. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (1)] |
| 2. | Sakamoto A, Hoshino T, Boku K, Hiraya D, Inoue Y. Fatal acute hypernatremia resulting from a massive intake of seasoning soy sauce. Acute Med Surg. 2020;7:e555. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (1)] |
| 3. | Qian Q. Hypernatremia. Clin J Am Soc Nephrol. 2019;14:432-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 4. | Ibarra G, Majmundar MM, Pacheco E, Zala H, Chaudhari S. Hypernatremia in Diabetic Ketoacidosis: Rare Presentation and a Cautionary Tale. Cureus. 2020;12:e11841. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Estifan E, Nanavati SM, Kumar V, Gibiezaite S, Michael P. Salty diabetes: a case series of hypernatremia presenting with diabetic ketoacidosis. AME Case Rep. 2019;3:27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Sohal RJ, Joshi S. Salty, Sweet and Difficult to Treat: A Case of Profound Hypernatremia in the Setting of Hyperosmotic Hyperglycemic State. Cureus. 2020;12:e7278. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 7. | Choo SJ, Lee HG, Kim CJ, Yang EM. Severe hypernatremia in soft drink ketoacidosis and hyperglycemic hyperosmolar state at the onset of type 2 diabetes mellitus: a case series of three adolescents. Clin Pediatr Endocrinol. 2022;31:81-86. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Goshima T, Terasawa T, Iwata M, Matsushima A, Hattori T, Sasano H. Treatment of acute hypernatremia caused by sodium overload in adults: A systematic review. Medicine (Baltimore). 2022;101:e28945. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | de Vos EAJ, van der Voort PHJ. ICU acquired hypernatremia treated by enteral free water - A retrospective cohort study. J Crit Care. 2021;62:72-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |