Published online Sep 9, 2022. doi: 10.5492/wjccm.v11.i5.311
Peer-review started: April 11, 2022
First decision: April 28, 2022
Revised: May 3, 2022
Accepted: July 16, 2022
Article in press: July 16, 2022
Published online: September 9, 2022
Processing time: 148 Days and 22.3 Hours
In this editorial, we comment on the current development and deployment of data science in intensive care units (ICUs). Data in ICUs can be classified into quali
Core Tip: Data in intensive care units (ICUs) can be classified into qualitative and quantitative data with different technologies needed to translate and interpret them. Data science, in the form of artificial intelligence (AI), should find the right interaction between physicians, data and algorithm to maximize the utility. AI deployment in the ICUs should be emphasized more to facilitate AI development. Individual-level applications such as disease prediction, and ICU-level potentials such as resource allocation are both of paramount importance.
- Citation: Luo MH, Huang DL, Luo JC, Su Y, Li JK, Tu GW, Luo Z. Data science in the intensive care unit. World J Crit Care Med 2022; 11(5): 311-316
- URL: https://www.wjgnet.com/2220-3141/full/v11/i5/311.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v11.i5.311
The intensive care unit (ICU) is a data-rich setting where the right decision can mean the difference between life and death. This gives the ICU the perfect opportunity to explore the impact of data science combined with artificial intelligence (AI) to maximize the utility and benefits. However, challenges remain because the interpretation of an incredibly huge amount of data is still a black hole with many questions unanswered. Although many models have been created, their clinical applications are limited. Attention is mostly paid to individual-level decision making such as diagnosing and predicting the prognosis of a specific disease, while potentials at a more macroscopic level such as ICU resource allocation, are largely omitted.
Generally speaking, data in the ICU can be classified into qualitative and quantitative data. Qualitative data include graphical data such as waves on the ventilation machine, and radiological data such as x-rays or computed tomography scans. Such data need to be translated first before being further calculated. Recently, we have seen a substantial number of researches focusing on such a translation process[1-4]. Quantitative data in the form of numbers such as physiological parameters, laboratory results, dosage of medication and ICU bed capacity, are common to intensivists. This kind of data has the advantage of being readily available for statistical analyses without the necessity for further proc
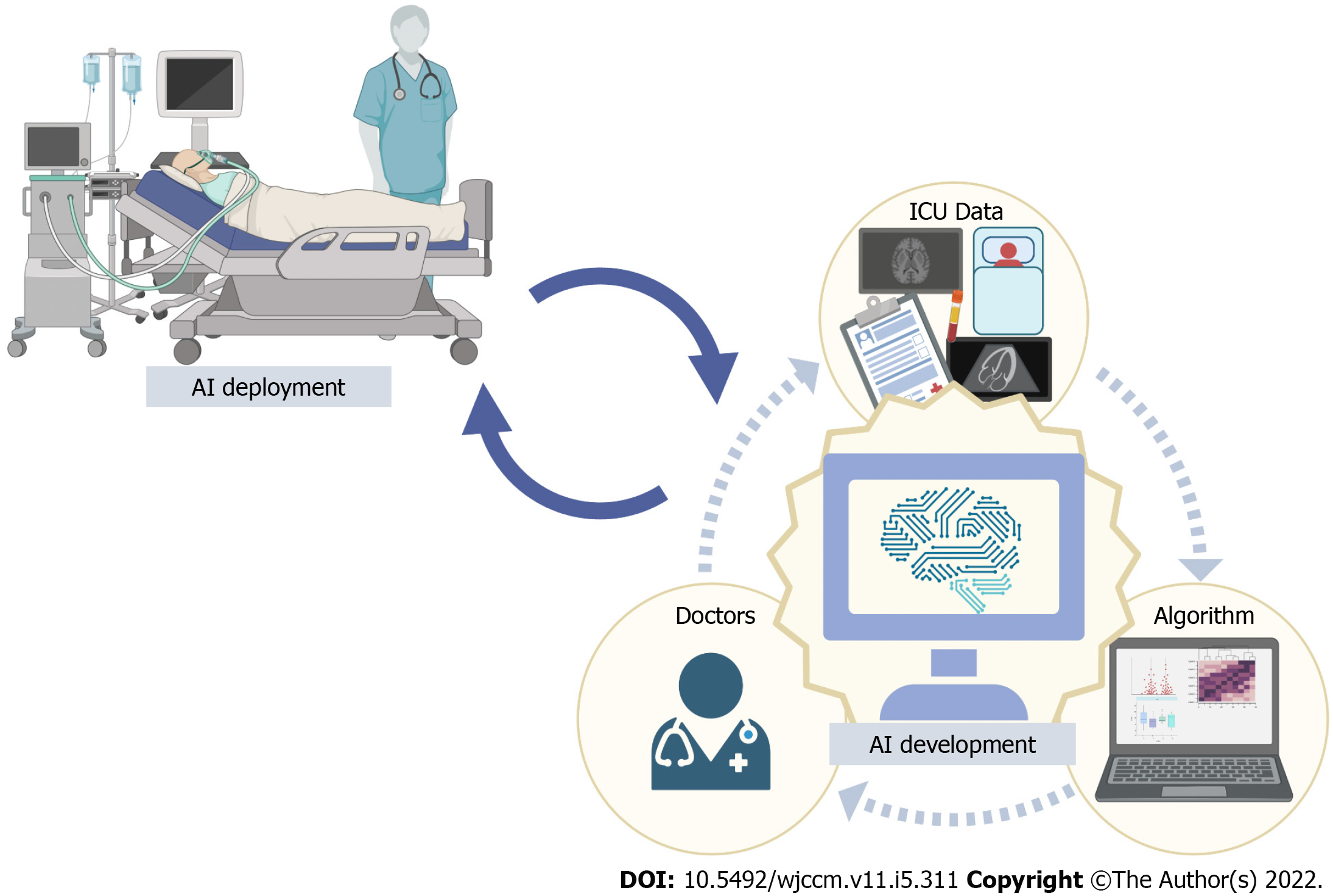
The key to making full use of data in ICUs is to find the right interaction between three roles: physi
Two examples where predictive models are supported by AI in decision making in ICUs are sepsis and mechanical ventilation. Sepsis is a leading cause of morbidity and mortality in critically ill patients. AI models have been studied in different stages such as the detection, prediction, risk stratification and management of sepsis. Goh et al[5] developed an algorithm with independent clinical notes and achieved high predictive accuracy 12 h before the onset of sepsis (Area under curve 0.94). It also has great potential for improving the early identification of patients who may benefit from the administration of antibiotics. Moreover, it can discover new phenotypes for sepsis potentially transforming sepsis treatment and offering a more tailored strategy for patients with sepsis[6], such as the use of glucocorticoids[7]. Clinicians hold a positive view in letting AI take a more active role when managing patients with sepsis[8].
Mechanical ventilation is another common situation in ICUs. Machine learning can predict the need for intubation in critically ill patients using commonly collected bedside clinical parameters and laboratory results[9]. AI has the potential to identify treatable phenotypes, optimize ventilation strat
Such an exciting trend should be viewed with caution. Current AI prediction models to diagnose sepsis are at a major risk of bias when the diagnostic criteria vary. The generalizability of these models is poor due to overfitting and the lack of standardized protocols. Similar conditions occur for mecha
Mamdani and Slutsky summarized three themes in applied AI in medicine: (1) Enabling data; (2) AI development; and (3) AI deployment. We believe that AI development and AI deployment should be combined to revise current models and offer tangible benefits derived from current researches. A vast majority of developed ICU-AI models remain within the testing and prototyping environment and only a handful have been actually evaluated in clinical practice[12] which implies the lack of enough evid
Machine learning and algorithm have been widely used to manage resource allocation. Machine learning has been studied for predictive scheduling and resource allocation in large-scale manufacturing systems and resource allocation strategies in vehicular networks using machine learning have been extensively explored[13,14]. These settings are similar to ICUs in that both need to capture the value from big data processing and extract useful insights to optimize production and protect resources.
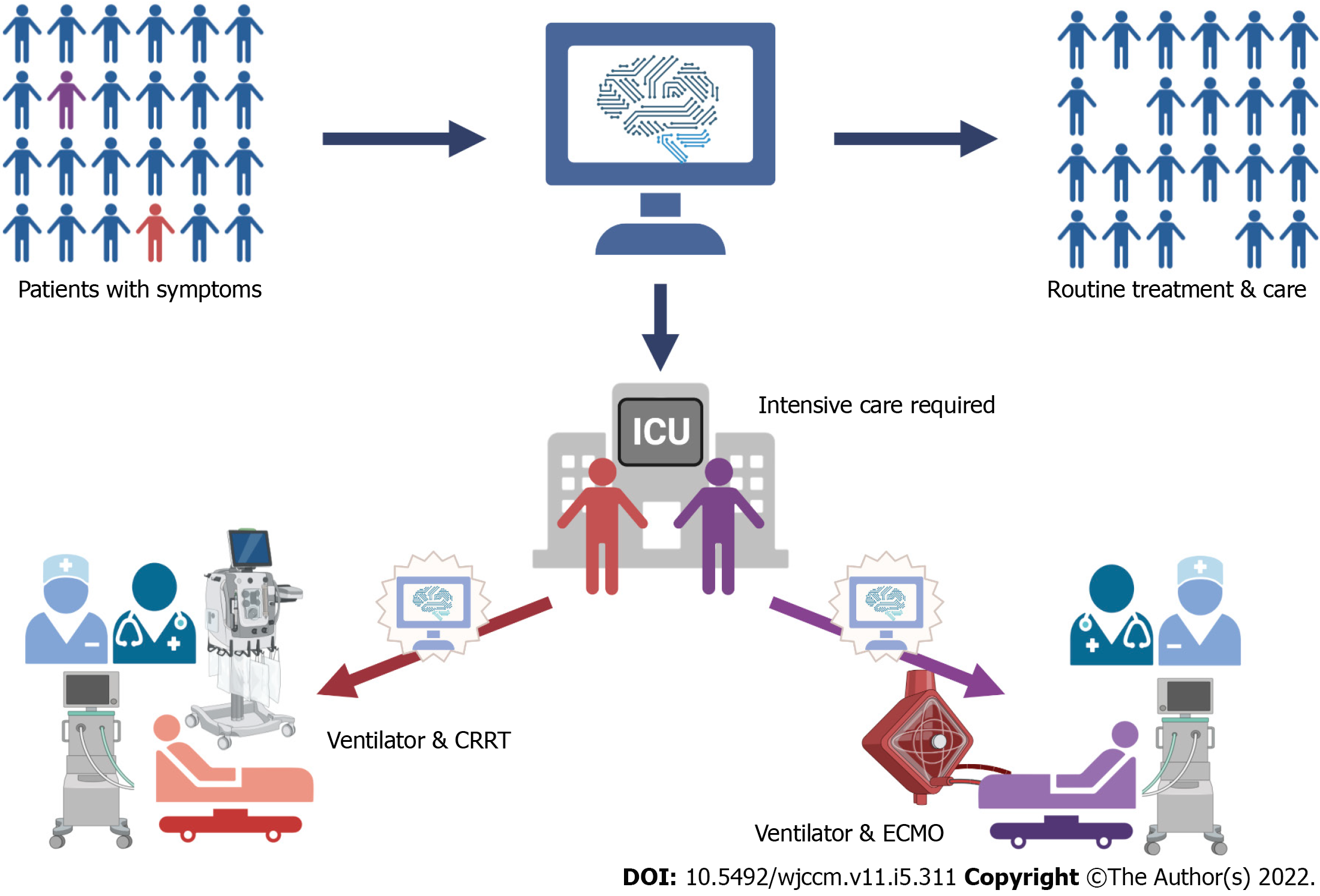
However, in the realm of critical care, where resource can be scarce due to factors such as bed capacity, the applications of machine learning has just shown a glimpse of light (Figure 2). Over the past 2 years, these applications in the context of the coronavirus disease 2019 (COVID-19) ICUs offered more chances to lay emphasis on resource allocation. Cheng et al[15] used machine learning to predict ICU transfer in hospitalized patients with COVID-19 and concluded that it could improve the management of hospital resources and patient-throughput planning. Similar principles were used to predict the use of ICU resources, such as mechanical ventilation, during the COVID-19 pandemic in Denmark[15]. At a healthcare system level, the National Health Service (NHS) in the United Kingdom started trials of a machine-learning system designed to help hospitals in England anticipate the demand on resources caused by COVID-19. COVID-19 Capacity Planning and Analysis System, a machine learning-based system for hospital resource planning, was subsequently developed that could be deployed at individual hospitals and across regions in the United Kingdom in coordination with NHS Digital[16].
Such models can take the application of AI in ICUs to another level. Although its insight into disease prediction, diagnosis and management is extremely important, it gives the chance to make the most use of resources, especially in ICUs where demand and supply frequently mismatch. Prediction in interventions such as mechanical ventilation would mean that the management groups can foresee changes and mobilize resource, such as equipment and staff, to cope with such demands in advance and this is a positive factor for patient outcomes.
Besides efficiency, another aspect that we must pay attention to is how to answer the ethical questions embodied in resource allocation to achieve a healthcare system that values equity and sustainability. This implies that ethical considerations must be included and certain ethical principles must be followed when designing the algorithm. Recently, a set of new studies focused on the ethics of healthcare resource allocation, drawing attentions to patient need, prognosis, equal treatment and cost-effectiveness[17]. Also, numerous comments were made during the COVID-19 pandemic that AI should stick to the ethical standards[18-20]. In a broader setting, the so-called algorithmic fairness highlights specific opportunities where machine learning and public and population health may synergize to achieve health equity[21]. Challenges remain as what ethical principles matter and what priority should be given to each ethical principle and coding them into an algorithm has not been intensively experimented.
AI has become more prevalent in the ICUs. Different kinds of data are collected constantly and should be interpreted in an accurate fashion. The key to maximizing AI in the ICU is to find the right balance between data, algorithms and physicians to ensure that the technical, computational and clinical needs are targeted.
For individuals, sepsis and mechanical ventilation have been two important aspects where AI has been extensively studied. However, major risks of bias, lack of generalizability and poor clinical values imply that AI is far from perfect. AI deployment in ICUs should be more emphasized to facilitate AI development.
More importantly, AI has huge potential in transforming resource allocation in ICUs. The COVID-19 pandemic has given some opportunities to establish such systems and more should be investigated. Ethical concerns must be addressed when designing such AI.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Critical care medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chavan RP, India; Wong YP, Malaysia S-Editor: Wang LL L-Editor: Filipodia P-Editor: Wang LL
| 1. | Homayounieh F, Digumarthy S, Ebrahimian S, Rueckel J, Hoppe BF, Sabel BO, Conjeti S, Ridder K, Sistermanns M, Wang L, Preuhs A, Ghesu F, Mansoor A, Moghbel M, Botwin A, Singh R, Cartmell S, Patti J, Huemmer C, Fieselmann A, Joerger C, Mirshahzadeh N, Muse V, Kalra M. An Artificial Intelligence-Based Chest X-ray Model on Human Nodule Detection Accuracy From a Multicenter Study. JAMA Netw Open. 2021;4:e2141096. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 56] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 2. | Siontis KC, Noseworthy PA, Attia ZI, Friedman PA. Artificial intelligence-enhanced electrocardiography in cardiovascular disease management. Nat Rev Cardiol. 2021;18:465-478. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 114] [Cited by in RCA: 381] [Article Influence: 95.3] [Reference Citation Analysis (0)] |
| 3. | Xu Q, Zhan X, Zhou Z, Li Y, Xie P, Zhang S, Li X, Yu Y, Zhou C, Zhang L, Gevaert O, Lu G. AI-based analysis of CT images for rapid triage of COVID-19 patients. NPJ Digit Med. 2021;4:75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 4. | Su Y, Qiu ZS, Chen J, Ju MJ, Ma GG, He JW, Yu SJ, Liu K, Lure FYM, Tu GW, Zhang YY, Luo Z. Usage of compromised lung volume in monitoring steroid therapy on severe COVID-19. Respir Res. 2022;23:105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Goh KH, Wang L, Yeow AYK, Poh H, Li K, Yeow JJL, Tan GYH. Artificial intelligence in sepsis early prediction and diagnosis using unstructured data in healthcare. Nat Commun. 2021;12:711. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 151] [Article Influence: 37.8] [Reference Citation Analysis (0)] |
| 6. | Seymour CW, Kennedy JN, Wang S, Chang CH, Elliott CF, Xu Z, Berry S, Clermont G, Cooper G, Gomez H, Huang DT, Kellum JA, Mi Q, Opal SM, Talisa V, van der Poll T, Visweswaran S, Vodovotz Y, Weiss JC, Yealy DM, Yende S, Angus DC. Derivation, Validation, and Potential Treatment Implications of Novel Clinical Phenotypes for Sepsis. JAMA. 2019;321:2003-2017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 517] [Cited by in RCA: 834] [Article Influence: 139.0] [Reference Citation Analysis (0)] |
| 7. | Zhang Z, Pan Q, Ge H, Xing L, Hong Y, Chen P. Deep learning-based clustering robustly identified two classes of sepsis with both prognostic and predictive values. EBioMedicine. 2020;62:103081. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 8. | Komorowski M. Clinical management of sepsis can be improved by artificial intelligence: yes. Intensive Care Med. 2020;46:375-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 9. | Siu BMK, Kwak GH, Ling L, Hui P. Predicting the need for intubation in the first 24 h after critical care admission using machine learning approaches. Sci Rep. 2020;10:20931. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 10. | Marshall DC, Komorowski M. Is artificial intelligence ready to solve mechanical ventilation? Br J Anaesth. 2022;128:231-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Zhao QY, Wang H, Luo JC, Luo MH, Liu LP, Yu SJ, Liu K, Zhang YJ, Sun P, Tu GW, Luo Z. Development and Validation of a Machine-Learning Model for Prediction of Extubation Failure in Intensive Care Units. Front Med (Lausanne). 2021;8:676343. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 50] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 12. | van de Sande D, van Genderen ME, Huiskens J, Gommers D, van Bommel J. Moving from bytes to bedside: a systematic review on the use of artificial intelligence in the intensive care unit. Intensive Care Med. 2021;47:750-760. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 101] [Cited by in RCA: 139] [Article Influence: 34.8] [Reference Citation Analysis (0)] |
| 13. | Morariu C, Morariu O, Răileanu S, Borangiu T. Machine learning for predictive scheduling and resource allocation in large scale manufacturing systems. Computers in Industry. 2020;120:103244. [RCA] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 51] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 14. | Nurcahyani I, Lee JW. Role of Machine Learning in Resource Allocation Strategy over Vehicular Networks: A Survey. Sensors (Basel). 2021;21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Cheng FY, Joshi H, Tandon P, Freeman R, Reich DL, Mazumdar M, Kohli-Seth R, Levin M, Timsina P, Kia A. Using Machine Learning to Predict ICU Transfer in Hospitalized COVID-19 Patients. J Clin Med. 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 92] [Cited by in RCA: 104] [Article Influence: 20.8] [Reference Citation Analysis (1)] |
| 16. | Qian Z, Alaa AM, van der Schaar M. CPAS: the UK's national machine learning-based hospital capacity planning system for COVID-19. Mach Learn. 2021;110:15-35. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 17. | Munthe C, Fumagalli D, Malmqvist E. Sustainability principle for the ethics of healthcare resource allocation. J Med Ethics. 2021;47:90-97. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 18. | Cave S, Whittlestone J, Nyrup R, O hEigeartaigh S, Calvo RA. Using AI ethically to tackle covid-19. BMJ. 2021;372:n364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 19. | Leslie D, Mazumder A, Peppin A, Wolters MK, Hagerty A. Does "AI" stand for augmenting inequality in the era of covid-19 healthcare? BMJ. 2021;372:n304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 80] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 20. | Yu M, Tang A, Brown K, Bouchakri R, St-Onge P, Wu S, Reeder J, Mullie L, Chassé M. Integrating artificial intelligence in bedside care for covid-19 and future pandemics. BMJ. 2021;375:e068197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 21. | Mhasawade V, Zhao Y, Chunara R. Machine learning and algorithmic fairness in public and population health. Nature Machine Intelligence. 2021;3:659-666. [RCA] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 69] [Article Influence: 17.3] [Reference Citation Analysis (0)] |