INTRODUCTION
There is a famous maxim in the surgical community: “the greater the surgeon, the bigger the incision”, meaning that great surgeons make big incisions and perform complex and challenging operations. However, now we are in the era of “the greater the surgeon, the smaller the incision”. Surgical treatment has been constantly evolving over the last 30 years in the quest for minimal invasiveness irrespective of the complexity and difficulty of the procedure. In 1986, the German surgeon Eric Mühe reported the first cases of laparoscopic cholecystectomy at the Congress of the German Surgical Society, but his concept did not attract much attention. Although his pioneering work was not properly recognized at first, this event represents a epochal paradigm shift from conventional open surgery to minimally invasive surgery. Thereafter, the trend that began with laparoscopic cholecystectomy progressed to include other more technically challenging abdominal procedures[1-5]. Improvements in techniques and instruments now make it feasible to perform complicated surgical procedures in a minimally invasive fashion. Moreover, the principle of minimally invasive surgery eventually reached the next stage in surgical access, natural orifice transluminal endoscopic surgery (NOTES), which does not require any anterior abdominal wall incision.
In the field of colorectal surgery, more than 20 years have passed since the first report of laparoscopic colectomy by Jacobs et al[6] in 1991. Since then, laparoscopic surgery for the management of colorectal diseases has been widely accepted as a prevailing option because of improved short-term outcomes in comparison with open surgery, as prospective randomized trials have demonstrated its safe clinical application for malignant diseases[7-10].
At present, to further the principle of minimally invasive surgery, two new approaches have been developed in the field of colorectal surgery, namely the totally laparoscopic approach and the single-incision approach.
Currently standard procedures of laparoscopic colectomy inevitably involve an additional abdominal incision for delivery of the specimen and preparation for anastomosis. The totally laparoscopic approach dispenses with this incision by combining completely intraperitoneal anastomosis with delivery of the specimen via a natural orifice, which is the anus or the vagina.
The single-incision laparoscopic surgery uses the umbilicus as the sole access to the abdominal cavity, whereas three to six ports are needed in standard laparoscopic surgery. All of the laparoscopic procedures are performed entirely through the umbilicus, in which the surgical scar becomes hidden, achieving virtually scarless surgery.
Undoubtedly, incisionless surgery using the NOTES technique is the most minimally invasive treatment method up to the present. However, NOTES, which faces obvious safety hurdles, is still far from being widely accepted in the standard surgical practice. This article reviews the current status of these two alternative approaches to enhance the advantages of laparoscopic surgery, i.e., the totally laparoscopic and single-incision approaches, and discusses the future of minimally invasive surgery for colorectal diseases.
TOTALLY LAPAROSCOPIC APPROACH
The advent of laparoscopic surgery has brought great changes in the surgical management of colorectal diseases because it involves less postoperative pain, improved cosmetic outcomes, earlier return of bowel function, and shorter hospital stay in comparison with open surgery. Currently most laparoscopic colectomies are performed in a “laparoscopy-assisted” fashion including extracorporeal procedures, such as bowel division and preparation for anastomosis, following laparoscopic mobilization of the bowel and lymph nodes dissection. Therefore, these procedures ineluctably necessitate an additional abdominal incision to the trocar placement sites. There have been many reports of completely intraperitoneal anastomosis combined with delivery of the specimen via a natural orifice, such as the anus or the vagina, which dispenses with a larger abdominal incision other than trocar placement sites[11-15]. Natural orifice specimen extraction (NOSE) has been postulated as an alternative approach to extracting the resected specimen out of the peritoneal cavity through an anatomic passage rather than an additional abdominal incision. Moreover, in the transition period from conventional laparoscopic surgery to true “scarless surgery”, hybrid techniques combining laparoscopic resection and NOSE technique is a convincing alternative in minimally invasive surgery to circumvent the safety hurdles which NOTES faces.
Obviously, extraction of a left-side colon specimen via the anus is not particularly difficult. However, the ensuing completely intraperitoneal anastomosis poses the major challenge in laparoscopic colectomy. In completely intraperitoneal anastomosis using a circular stapling device, in particular, placement and fixation of the anvil are the most difficult steps. For fixation of the anvil in the proximal end of the colon, a procedure using an Endo-loop and a procedure involving a hand-sewn purse-string suture have been two major options[11,13]. These two techniques have their strong and weak points. On the one hand, ligation using an Endo-loop is a very simple technique in itself, whereas it may be less reliable in comparison with a hand-sewn purse-string suture mainly due to difficulty in stabilizing the colonic stump while putting the ligature in place and tightening the loop around the center rod of the anvil. On the other hand, the technique using a hand-sewn purse-string suture is naturally more time-consuming and involves extensive skills in laparoscopic suturing. We have developed a simple and reliable technique for placement of the anvil in the esophageal stump in laparoscopic total gastrectomy using a linear stapling device[16,17]. We have also reported application of this technique to totally laparoscopic sigmoid colectomy[18] and totally laparoscopic low anterior resection[19]. Our technique, named the “efficient purse-string stapling technique”, achieves transection of the colon and placement of the anvil of a circular stapling device on the colonic stump at the same time using a linear stapling device. Our totally laparoscopic procedure using this technique is described in Figures 1-3[18-22].
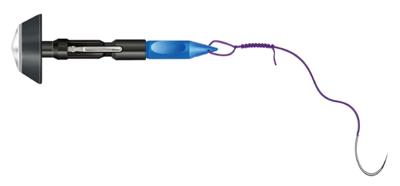
Figure 1 The anvil of a circular stapling device with its center rod secured with a 2-0 monofilament suture at the hole of the tip, is shown.
The suture is tied over 10 times so that the thread that is pulled completely out of the colon does not slip into the intraluminal cavity.
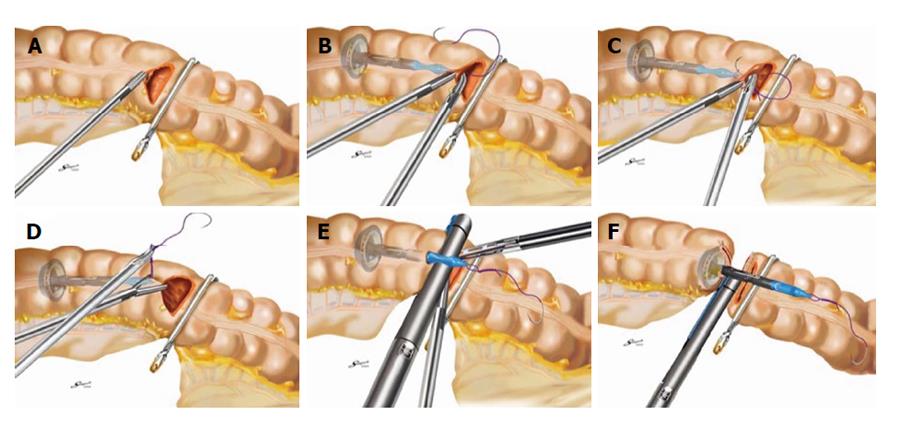
Figure 2 Efficient purse-string stapling technique.
A: A semi-circumferential colotomy is performed at the colonic wall just proximal to the forceps; B: Anvil insertion into the colon via a semi-circumferential colotomy: An anvil with suture is held by a grasper and fully inserted into the proximal colon; C: The accompanying needle is advanced through the anterior colonic wall; D: The suture is pulled out of the colon until all knots are completely exposed; E: While pulling the suture to the right side horizontally, the colon is clamped using a linear stapling device with disposable gastrointestinal cartridge; F: The colon is then transected by firing the instrument to secure the anvil on the colonic stump.
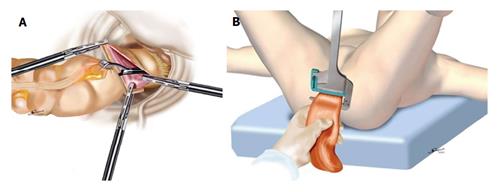
Figure 3 Transanal specimen extraction.
A: In sigmoid colectomy, a grasping forceps is brought through the rectum, and the specimen is extracted through the colotomy made at the distal staple line; B: In low anterior resection, a grasping forceps is inserted under laparoscopic vision from the anus to grasp the staple in the stump, and the distal rectum is everted and pulled transanally outside the body.
Specimen extraction via the anorectal canal is applicable to both male and female patients. However, the application of the transvaginal route is limited only to female patients, whereas it is more complicated due to the necessity of colpotomy in comparison with the transanal route. Moreover, Franklin et al[23] reported that one characteristic complication of transvaginal extraction was accidental damage of the sigmoid colon and rectum, at a rate of 7.7%, because of the narrowness of Douglas’s pouch. On the other hand, regarding the transanal route, there are concerns over intra-abdominal fecal contamination and infectious complications. Leroy et al[24] reported that there was no infectious complications in 16 patients who underwent laparoscopic colectomy with transanal specimen extraction for sigmoid diverticulitis, whereas all peritoneal cultures were positive for polybacterial growth. However, inherent limitations of the transanal route have been pointed out; namely, this route is not applicable to patients with large tumor or narrow anorectal canal[25].
Bernstein et al[26] compared a complete laparoscopic procedure with a conventional laparoscopic procedure and found no statistically significant differences in terms of the hospitalization period or the duration of postoperative ileus. Moreover, a recent systematic review of the current literature concerning left-sided laparoscopic colectomy with transanal specimen extraction pointed out a lack of standardization of techniques and concluded that the level of the evidence supporting laparoscopic colectomy with transanal specimen extraction is low[27].
SINGLE-INCISION APPROACH
Recently, the endeavor to enhance the advantages of laparoscopic surgery has led minimally invasive surgeons to seek to minimize the number and the size of incisions. Especially, the development of single-incision laparoscopic surgery has been attracting increasing attention in the field of minimally invasive surgery. While three to six ports are needed in standard laparoscopic surgery, the single-incision approach uses the umbilicus as the sole access to the abdominal cavity.
The technique of single-incision surgery was first applied to appendectomy, thereafter to cholecystectomy[28]. Pelosi et al[29] reported single-puncture laparoscopic appendectomy in 1992, and in 1997, Navarra et al[30] performed laparoscopic cholecystectomy using only transumbilical trocars. Recently, the single-incision approach has been applied to more complicated procedures including inguinal hernia repair, colectomy, and gastrectomy[31-37]. The authors utilized the umbilicus, which some researchers call an embryologic natural orifice, as the sole access to the abdominal cavity to perform a surgical procedure that will leave a concealed surgical scar, thus achieving an essentially scarless surgical procedure. Unlike NOTES, which requires further development of techinique and the instrument, single-incision transumbilical laparoscopic surgery is ready for widespread implementation. This is because single-incision procedures can be performed using standard laparoscopic instruments, which would enable surgeons to conform to standard surgical principles and techniques. However, conflicts between laparoscopic instruments when used through a narrow single incision often make it infeasible to get adequate retraction and exposure, which necessitates surgeons to have extensive skills in standard laparoscopic surgery.
In the field of colorectal surgery, the first single-access laparoscopic colectomies were reported in 2008. Bucher et al[33,34] have described single-port access laparoscopic right hemicolectomy and left colectomy. They placed two standard laparoscopic ports, a 12-mm umbilical port and a 5-mm port, in a 2-cm umbilical incision, and used a 10-mm laparoscope with a 6-mm working channel. To facilitate dissection, suspension and exposition of the colon was achieved by placing transparietal stitches anchored on the mesentery or the colon wall. Only standard straight laparoscopic instruments were used. The authors pointed out that a low possibility of triangulation and the absence of off-axis vision would make the procedure complex. Remzi et al[35] performed laparoscopic right hemicolectomy using a special multichannel umbilical port and specially designed curved instruments. They emphasized that the flexible steerable laparoscope and instruments helped to reduce the difficulties of dissection due to loss of triangulation. Leroy et al[38] performed sigmoidectomy in a patient with diverticulitis using a multichannel umbilical port that allows the insertion of three laparoscopic instruments concurrently. To facilitate dissection of the mesentery, they used a sigmoidoscope to supplement retraction by means of tip angulation and instrument torque. For placement of the anvil of the circular stapler in the proximal end of the colon, they used an extracorporeal magnet to lock the metal anvil in position. They pointed out that the use of different curved or straight instruments of varying caliber allowed triangulation of the working instruments. They also mentioned the possibility of direct translation of their procedure into a NOTES format. At the same time, they emphasized that their procedure did not allow full mesenteric dissection and therefore was not suitable in its current format for oncological resections. Recently, Takemasa et al[39] reported the technical feasibility and safety of laparoscopic complete mesocolic excision with central vascular ligation for colon cancer.
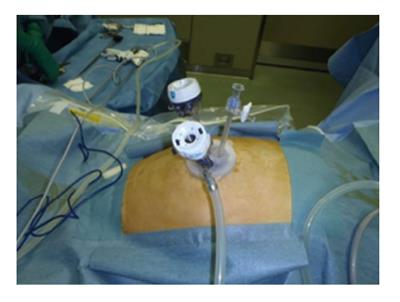
We introduced single-incision laparoscopic colectomy in our institute in 2009. Gradually expanding the indication to include advanced colorectal cancer, single-incision laparoscopic colectomy is now a standard procedure for colorectal cancer from the cecum to the rectosigmoid in our institute. Our typical setting for single-incision laparoscopic colectomy is shown (Figure 4). A 10-mm flexible laparoscope and standard straight laparoscopic instruments are used, of which, in particular, the flexible laparoscope that allows off-axis vision is extremely useful for single-incision laparoscopic surgery. We studied 429 consecutive patients who underwent single-incision laparoscopic colectomy in our institute from 2009 to 2013. The conversion rate to conventional multi-port laparoscopic colectomy was 3.3%. None of the patients was converted to open surgery. The rate of postoperative complications was comparable with those in other reports of multi-port laparoscopic surgery. We also compared two groups of patients: patients with previous abdominal surgery and those with no previous abdominal surgery. There were no significant differences between the two groups in terms of blood loss, operative time, and short-term postoperative outcomes. Therefore, we concluded that single-incision colectomy is safe and feasible even in patients with previous abdominal surgery. Moreover, patients with advanced colorectal cancer were included in this series. Complete mesocolic excision with central vascular ligation can now be performed with our single-incision procedure, corresponding to the standard surgical procedures for advenced colorectal cancer in Japan. This study also showed that the single-incision method was comparable with the multi-port method in terms of resection margin and the number of harvested lymph nodes[40].
Figure 4 Intra-operative view of single-incision laparoscopic colectomy.
We make an 2.5-cm long vertical incision in the umbilicus, and typically use E-Z Access (Hakko Co. Ltd., Nagano, Japan) on the Lap Protector™ (Hakko Co. Ltd., Nagano, Japan) for the insertion of two 5-mm trocars and one 12-mm trocar for a right colectomy, and one 5-mm trocar and two 12-mm trocars for a left colectomy, sigmoidectomy or rectal resection.
After single-incision laparoscopic colectomy for colon cancer was introduced by Remzi et al[35] and Bucher et al[33] in 2008, the feasibility of the procedure was examined in several case-control studies and two randomized controlled trials, which compared short-term outcomes between patients who underwent single-incision laparoscopic colectomy and those who underwent multi-port laparoscopic colectomy. Although single-incision laparoscopic colectomy provides a better cosmetic result and reduces postoperative pain, its impact on the length of hospital stay remains controversial[39,41-45].
DISCUSSION
Totally laparoscopic colectomy with natural orifice specimen extraction has been safely introduced to general surgical practice. Diana et al[46] reviewed 19 studies that reported transanal extraction of the specimen, and they concluded that transanal extraction is a feasible option to minimize incisions in colorectal surgery. At the same time, the concept of single-incision laparoscopic surgery is appealing to surgeons performing minimally invasive procedures and is evolving at a surprisingly rapid rate[29-37].
Undoubtedly, incisionless surgery using the NOTES technique is the final and ultimate goal for minimally invasive surgeons. Furthermore, a survey has shown that patients would prefer NOTES to standard laparoscopic surgery if the risks associated with the two approaches were comparable[47]. However, in spite of the initial enthusiasm after the first advent, NOTES currently remains in the area of experimental surgery mainly due to concerns over the surgical platform, accidental organ injury, and viscerotomy closure.
What is necessary for safe introduction of NOTES in clinical practice, while it takes time for the development of a new surgical platform or reliable techniques for viscerotomy-closure? The optimal transluminal access route for NOTES is now an area of active investigation. Initial work rather focused on transgastric and transvaginal NOTES, and transcolonic NOTES has been the least explored approach because of concerns related to fecal contamination and intra-abdominal infectious complications. Over time, however, transrectal accesss has in fact proved more practical than the former routes[48]. The benefits of transcolonic access include in-line endoscopic visualization, which dispenses with the need for scope retroflection for visualization of upper abdominal organs, more compliance of the anorectum than the esophagus, and suitability for both male and female patients[49]. Moreover, the transanal route has two major advantages over other routes. Firstly, there are reliable surgical platforms: Transanal Endoscopic Microsurgery (TEM) and Transanal Endoscopic Operation (TEO). Since Buess et al[50] introduced TEM in the 1980s, there has been accumulation of extensive human clinical experience with complex transanal surgery. TEO is a modification of TEM. Incorporated with an ordinary laparoscopic imaging system and readily available laparoscopic instruments, TEO allows precice dissection under magnified and high-definition view that is as effective as TEM. Secondly, in the case of rectosigmoid resection, viscerotomy can be removed as part of the specimen or incorporated into the anastomosis. Zhang et al[51] reported the first clinical case of pure transanal NOTES with total mesorectal excision (TME) in 2013. They used a three-channel single-port laparoscopic cannula placed in the procedure of prolapse and hemorrhoids anoscope as the surgical platform, and after removal of the specimen, they made a colorectal anastomosis at the site of the viscerotomy using a circular stapling device. Approximately at the same time, Leroy et al[52] also reported a clinical case of pure transanal NOTES with TME. They used the TEO device as the surgical platform. After the specimen was delivered transanally, a hand-sewn coloanal anastomosis was fashioned so that the viscerotomy was incorporated into the anastomosis. They emphasized the advantages of the transanal route, which include easy accessibility to the anus, reliable surgical platforms like the TEO system, the possibility to eliminate viscerotomy-closure, and the use of currently available laparoscopic instrumentation.
Although two clinical cases of transanal NOTES were successfully carried out, it is unlikely for their procedure to be widely accepted in general practice in the near future. At present, the hybrid NOTES technique seems to be the most pragmatic way to enhance the concept of minimal invasiveness. There are several reports of hybrid NOTES procedures in humans. In all cases, a hybrid laparoscopic technique with one to three transabdominal trocars was used[53-55]. Techniques for totally laparoscopic colectomy with NOSE and single-incision colectomy are well established. Therefore, some of these techniques seem to be feasible and useful even in the hybrid NOTES setting. For example, our technique, i.e., the “efficient purse-string stapling technique”, could be performed in the hybrid NOTES format using standard laparoscopic instruments and stapling devices brought into the peritoneal cavity via the transvaginal port, followed by extraction of the specimen through the vagina[18,19].
The totally laparoscopic approach with NOSE and single-incision approach have been enhanced by both innovative port technology and technical expertise learned by developing NOTES. Conversely, new techniques and technology gained in clinical experience of totally laparoscopic colectomy and single-incision surgery may be ultimately used for NOTES procedures. Therefore, it is of utmost importance that all minimally invasive surgeons constantly keep up with new developments in these two approaches in this rapidly evolving field.
P- Reviewer: Contini S, Kirshtein B, Nash GF, Romeo C
S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ