Published online Nov 28, 2013. doi: 10.5412/wjsp.v3.i3.41
Revised: July 10, 2013
Accepted: August 4, 2013
Published online: November 28, 2013
Processing time: 209 Days and 7.1 Hours
AIM: To investigate the accuracy of preoperative examinations in follicular type tumors, we re-evaluate results of our operative cases.
METHODS: Cases are follicular neoplasms in 36 patients, which are more than 30 mm in diameter and underwent surgery in our hospital in 2005-2006. These cases had been suspected of malignancy on one or more of the preoperative examinations, including ultrasound (US), thallium-technecium (Tl-Tc) scinitigram, computed tomography (CT), or fine needle aspiration biopsy (FNA) examinations. Concern about operative procedure, lobectomy plus sentinel lymph node biopsy (SNB) was performed in all 36 follicular tumors at the first surgery. Because we can diagnose a suspected follicular tumor as carcinoma and can change the operative procedure intra-operatively, when the metastasis of lymph nodes, outside of the thyroid, is found. The operative procedure was changed from lobectomy to total thyroidectomy plus lymph nodes dissection (central component), when the SNB has metastasis. All thirty six cases were obtained to track the prognosis until 2012, for 6-7 years follow up periods.
RESULTS: The final pathological results are 3 cases of follicular carcinoma, 6 cases of papillary carcinoma, 1 case of papillary carcinoma follicular type, 1 case of malignant lymphoma, 16 cases of follicular adenoma, and 9 cases of adenomatous goiter. The malignant tumor were observed in 11/36 (30.6%) cases. All six papillary carcinomas were less than 20 mm, and present with follicular adenoma and adenomatous goiter, which have more than 40 mm diameter. In physical examination, tumor size of 36 cases of follicular neoplasm is more than 30 mm all at the time of surgery. The tumors were palpable somewhat stiff, such as no cystic component in 34 cases. Occasional dyspnea, dysphagia, and cough was accompanied in all 36 cases. The true ratio of correct diagnosis of preoperative US, Tl-Tc scinitigram, CT, and FNA were 17/36 (47.2%), 16/36 (44.4%), 24/36 (66.7%), 21/36 (58.3%), respectively. In 11 malignant cases, there was one SNB positive case (one lymph node metastasis in 3 SNB: 1/3). This case was changed the operative procedure from lobectomy to total thyroidectomy plus lymph node dissection (central component). There is other lymph nodes metastasis in dissected lymph nodes (4/15). For the remaining malignant 10 cases, the observations were selected without additional resection, because surgical margins and SN were negative in postoperative pathology results at the first operation. No recurrence and metastasis are allowed in 11 malignant cases, up to 7 years after post-operation. Over all, the more than 30 mm in diameter follicular neoplasms, which were suspected the malignancy in the one and more preoperative examinations, are present the malignancy by pathological diagnosis in 11/36 (30.6%) cases after surgery. The non SNB metastasis cases had no symptoms of lymph nodes metastasis up to 7 years after post-operation.
CONCLUSION: We think that more than 30 mm in diameter follicular neoplasms are considered as candidates of surgery from our results.
Core tip: To know the accuracy of preoperative examinations, we investigated the operated 36 follicular type tumors, according to the postoperative final pathological diagnosis. We also re-evaluate the operative indication and operative procedure. The true ratio of correct diagnosis of preoperative ultrasound, thallium-technecium scinitigram, computed tomography, or fine needle aspiration biopsy were 17/36 (47.2%), 16/36 (44.4%), 24/36 (66.7%), 21/36 (58.3%), respectively, and there were no statically differences between the accuracy of these preoperative diagnoses. The more than 30 mm in diameter tumors, which were suspected the malignancy in the one and more preoperative examinations, are present the malignancy in 11/36 (30.6%) cases by final pathological diagnosis.
- Citation: Takeyama H, Tabei I, Kato K, Kamio M, Nogi H, Toriumi Y, Kinoshita S, Akiba T, Uchida K, Morikawa T. Operative indications of follicular type tumors, based on Japanese clinical guidelines. World J Surg Proced 2013; 3(3): 41-46
- URL: https://www.wjgnet.com/2219-2832/full/v3/i3/41.htm
- DOI: https://dx.doi.org/10.5412/wjsp.v3.i3.41
The diagnostic accuracy of papillary carcinoma is over 90% by preoperative examinations. On the other hand, the diagnostic accuracy of follicular type tumors is only 20%-40%.
For example, the accuracy of fine needle aspiration biopsy (FNA) is more than 90% in papillary carcinoma, because the morphology of papillary cell has some distinctive features, such as intra-nuclear inclusion or notching of nuclei. In contrast, there are no differences between follicular malignant tumors and benign follicular tumors morphologically by FNA. For the preoperative diagnosis of thyroid tumor, ultrasound (US) examination, thallium-technecium (Tl-Tc) scinitigram, computed tomography (CT), and fine needle aspiration biopsy (FNA) are usually recommended. We decided the operative indication and resected area with these results.
Recently, some physical signs and radiological imagings are indicated as the detection tools of malignant follicular type tumor by the new Japanese guide line of thyroid tumor, published in 2010[1].
In this study, we re-evaluate the results of preoperative examinations of follicular type tumors according to the guide line, using the pathologically final diagnosed cases, and re-consider the operative indications.
Cases are follicular neoplasms in 36 patients, which are more than 30 mm in diameter and underwent surgery in our hospital in 2005-2006. These cases had been suspected of malignancy by the one or more of preoperative examinations, including US, Tl-Tc scinitigram, CT, or FNA examinations.
Usually, the operation of follicular type tumor performs tumor-side lobectomy, as the differential diagnosis is difficult in preoperative examinations.
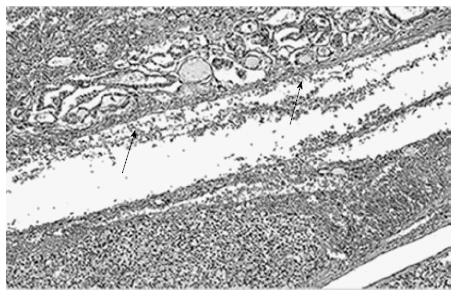
In the Japanese thyroid cancer treatment protocol in 2005 Edition[2], follicular carcinoma diagnostic criteria are determined as follows: (1) membrane invasion of the tumor cells; (2) lymphatic or vessel duct invasion of the tumor cell; and (3) metastasis outside of the thyroid gland being able to confirm one of either of these histological examinations.
In this study, we tried the lobectomy plus sentinel nodes biopsy (SNB) as a first operation. Because we can diagnose a follicular tumor as carcinoma and can change the operative procedure intra-operatively, when the metastasis of lymph nodes, outside of the thyroid, is found.
The final diagnosis of tumor was determined by formalin-fixed, Hematoxylin-Eosin (HE) stained specimen after surgery. SNB was evaluated by HE stained frozen section intra-operatively, and reevaluated by formalin-fixed specimen after surgery.
The final pathological diagnosis and the results of preoperative examinations were summarized in Tables 1 and 2. The pathological diagnoses are 3 cases of follicular carcinoma (diameter 40-54 mm), 6 cases of papillary carcinoma (5-14 mm), 1 case of papillary carcinoma follicular variant type (30 mm), 1 case of malignant lymphoma (45 mm), 16 cases of follicular adenoma (30-80 mm), 9 cases of adenomatous goiter (43-170 mm). The malignant tumors were observed in 11/36 (30.6%) cases.
| Pathological diagnosis | Cases | Tumor size (mm) |
| Malignant lesion | ||
| Papillary carcinoma | 7 | 5-30 |
| Follicular carcinoma | 3 | 40-54 |
| Malignant lymphoma | 1 | 45 |
| Benign lesion | ||
| Follicular adenoma | 16 | 33-80 |
| Adenomatous goiter | 9 | 43-170 |
| US | Tl-Tc scinitigram | CT | FNA | |
| True positive: TP (malignant) | 2 (18.2) | 9 (81.8) | 2 (18.2) | 6 (54.5) |
| True negative: TN (benign) | 15 (40.0) | 7 (28.0) | 22 (88.0) | 15 (60.0) |
| TP + TN (accuracy) | 17 (47.2) | 16 (44.2) | 24 (66.7) | 21 (58.3) |
About seven papillary carcinomas including follicular variant type, 6 papillary carcinomas were present with adenoma and adenomatous goiter that have more than 40 mm diameter (Figure 1).
In 36 patients performed SNB intraoperative, there was one positive metastasis case of papillary carcinoma follicular variant type (1/36, 2.7%).
Physical examination: Tumor size of 36 cases is more than 30 mm all at the time of surgery. The tumors were palpable somewhat stiff, such as no cystic component in 34 cases. Occasional dyspnea, dysphagia, and cough was accompanied in all 36 cases, but was not accompanied lymph node swelling, paralysis of the vocal cords.
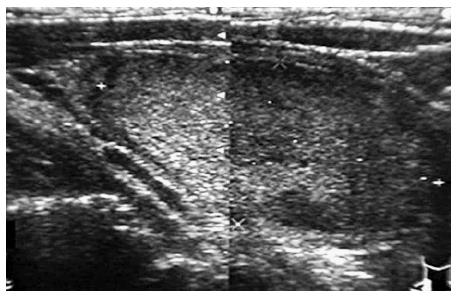
US: US examination diagnosed 24 cases as benign tumors including adenoma, adenomatous goiter, and 12 cases as suspicion of malignant or malignant tumor. The true positive ratio (TP) was 2/11 (18.2%), the true negative ratio (TN) 15/25 (60.0%), the false-positive ratio (FP) 10/25 (40.0%), the false negative ratio (FN) 9/11 (81.8%), respectively. The true ratio (TR) of correct diagnosis (TP + TN/Total cases) by US was 17/36 (47.2%). The malignant tumor suspected by US, were indicated in Figure 2.
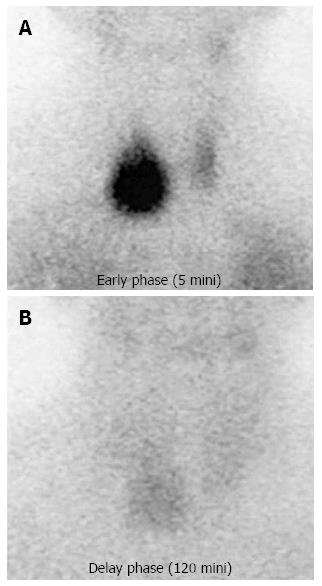
Scintigraphy (Tl-Tc scinitigram): Tl-Tc scinitigram examination diagnosed 9 cases as benign tumor, and 27 cases as suspicion of malignant or malignant tumor. TP was 9/11 (81.8%), TN7/25 (28.0%), FP18/25 (72.0%), FN 9/11 (81.8%), respectively. TR by Tl-Tc scinitigram was 16/36 (44.4%). The malignant tumor suspected by scintigraphy was suggested in Figure 3.
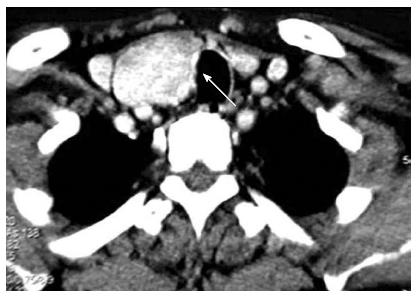
CT: CT examination diagnosed 31 cases as benign tumor, and 5 cases as suspicion of malignant or malignant tumor (Figure 4).
TP was 2/11 (18.2%), TN 22/25 (88.0%), FP 3/25 (12.0%), FN 9/11 (81.8%), respectively. TR by CT was 24/36 (66.7%).
FNA: Twenty cases were benign, and 16 cases were suspicion of malignancy by FNA examination. TP was 6/11 (54.5%), TN 15/25 (60.0%), FP 10/25 (40.0%), and FN 5/11 (45.5%), respectively. TR by FNA was also 21/36 (58.3%).
Operation: Lobectomy plus SNB was performed in all 36 follicular tumors at the first surgery.
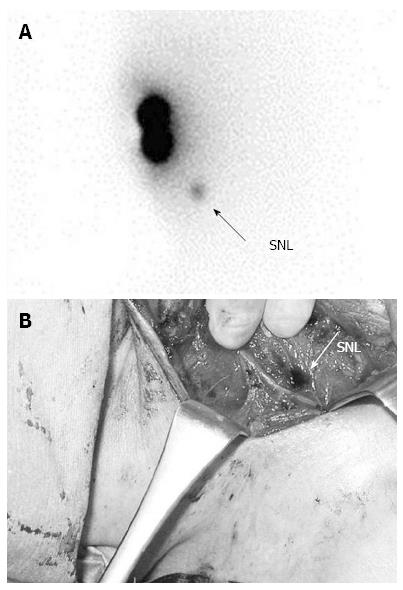
Figure 5A is a statue of SN identification using Tc- physic acid for the 40 mm diameter follicular neoplasm of the right lobe.
Figure 5B is the photo of SN stained by the dye at the time of surgery of the same case. The stained SN was acknowledged in the central component lymph nodes near the right recurrent nerve. The SN was counted the accumulation of isotope, excised, and submitted to the intraoperative pathologic examination to confirm the presence or absence of lymph node metastasis. In 36 patients, there was one positive lymph nodes metastasis case (SNB: 1/3). The surgical procedure was changed to total thyroidectomy plus lymph node dissection (central component) during surgery in this case. There is other lymph nodes metastasis in dissected lymph nodes (4/15).
For the remaining malignant 10 cases, the observations were selected without additional resection, because surgical margins and SN were negative in postoperative pathological diagnosis.
The recurrence or metastasis has not been recognized in these 11 cases of malignant tumor from 2005 to 2012, more than five years after surgeries.
In clinical question (CQ) 6 of the 2010 Thyroid Tumor Treatment Guidelines created by Japan Endocrine Surgery Society/Japan Thyroid Surgery Society, US, Tl-Tc scintigraphy, CT, and fluoro-deoxyglucose positron emission tomography are given as diagnostic imaging methods in the diagnosis of malignant tumors as grade B recommendations[1,3-5]. Among these, US is recommended as the most useful modality[1,6-8].
In this follicular tumor study, correct diagnostic rates of FNA and CT were relative high with 50%-60% on the preoperative examinations.
When we compared these 2 examinations, true positive rate, both true negative rates were more than 50% together in FNA examination. On the other hand, the CT test identified true positive rate 18.2%, and true negative rates 88.0%.
So, we think that FNA is a reliable examination for distinguish malignant and benign follicular tumor than CT study, although there is thought to be room for improvement, as many reports mentioned that diagnosis of follicular malignant neoplasm was more difficult than diagnosis of papillary carcinoma[1,5-8].
CQ 5 of the guidelines state that “physical findings that increase the possibility of malignant neoplasm in thyroid tumors include adhesion to tissues surrounding nodes, lymph node enlargement, vocal cord paralysis (hoarseness), dyspnea, dysphagia, coughing” and “especially in tumor size alone, nodes of ≥ 40 mm are a significant independent factor suggestive of malignancy”[1,9-14]. In addition, when a tumor is follicular carcinoma, tumor size ≥ 40 mm become stage III in the tumor node metastasis classification of Union for International Cancer Control, and the chance of remote metastasis will be increased.
Surgery is thought to be indicated in that reason for the follicular tumors ≥ 40 mm, which can not deny the malignancy[15,16].
In our results, only 3 of 28 follicular tumors ≥ 40 mm in diameter were follicular carcinoma (10.7%), and 5 of 36 follicular tumors ≥ 30 mm that were suspected the malignancy by several preoperative examinations, were malignant tumors (13.9%). Concerning about papillary carcinoma, although the size of papillary carcinoma were less than 20 mm, 6 cases coexisted with follicular adenoma and adenomatous goiter ≥ 40 mm that were benign on postoperative pathological diagnosis.
As described above, the malignancy rate of follicular tumors ≥ 40 mm was not high. However, considering coexisting lesions such as papillary carcinoma with benign follicular tumors ≥ 40 mm, the malignant region was present in a total of 12 of 36 suspected tumor (33.3%). So, we concluded that surgery is thought to be indicated as stated in the guidelines.
For SNB, such as follicular variant of papillary carcinoma that have a fairly high frequency of lymph node metastasis, the surgical procedure can be changed depending on lymph node metastasis status during surgery. So, SNB is thought to have a high likelihood of being useful[15,17].
It is a tiny and one facility study, we think that follicular neoplasms ≥ 40 mm in diameter, which had been suspected of malignancy on one or more of the preoperative examination are considered as candidates of surgery, as suggested in the Treatment of Thyroid Tumor--Japanese Clinical Guidelines[1].
The diagnostic accuracy of papillary carcinoma is over 90% by preoperative examinations. On the other hand, the diagnostic accuracy of follicular type tumors is only 20%-40%.
Recently, some physical signs and radiological imagings are indicated as the detection tools of malignant follicular type tumor by the new Japanese guide line of thyroid tumor, published in 2010. In this study, they re-evaluate the results of preoperative examinations of follicular type tumors according to the guide line, using the pathologically final diagnosed cases, and re-consider the operative indications.
In their results, only 3 of 28 follicular tumors ≥ 40 mm in diameter were follicular carcinoma (10.7%), and 5 of 36 follicular tumors ≥ 30 mm that were suspected the malignancy by several preoperative examinations, were malignant tumors (13.9%). Concerning about papillary carcinoma, although the size of papillary carcinoma were less than 20 mm, 6 cases coexisted with follicular adenoma and adenomatous goiter ≥ 40 mm that were benign on postoperative pathological diagnosis. As described above, the malignancy rate of follicular tumors ≥ 40 mm was not high. However, considering coexisting lesions such as papillary carcinoma with benign follicular tumors ≥ 40 mm, the malignant region was present in a total of 12 of 36 suspected tumor (33.3%). So, the authors concluded that surgery is thought to be indicated as stated in the guidelines.
Authors think that follicular neoplasms ≥ 40 mm in diameter, which had been suspected of malignancy on one or more of the preoperative examination are considered as candidates of surgery, as suggested in the Treatment of Thyroid Tumor-Japanese Clinical Guidelines.
This is a very interested topic for the readers. It shows the guidelines of the Japanese Society of Endocrine Surgery.
P- Reviewer: Rodriguez DC S- Editor: Gou SX L- Editor: A E- Editor: Liu XM
| 1. | Takami H, Yoshida A, Okamoto T, editors . Treatment of Thyroid Tumor--Japanese Clinical Guidelines. Tokyo: KANEHARA Publishing 2010; 33-39. |
| 2. | Miyauchi A, Sakamoto A, Kakudo K, editors . General rules for description of thyroid cancer by the Japanese society of thyroid surgery. 6th ed. Tokyo: KANEHARA Publishing 2006; 13-16. |
| 3. | Ishigaki S, Shimamoto K, Satake H, Sawaki A, Itoh S, Ikeda M, Ishigaki T, Imai T. Multi-slice CT of thyroid nodules: comparison with ultrasonography. Radiat Med. 2004;22:346-353. [PubMed] |
| 4. | Tamizu A, Okumura Y, Sato S, Takeda Y, Maki K, Hiraki T, Akaki S, Kuroda M, Kanazawa S, Hiraki Y. The usefulness of serum thyroglobulin levels and Tl-201 scintigraphy in differentiating between benign and malignant thyroid follicular lesions. Ann Nucl Med. 2002;16:95-101. [PubMed] |
| 5. | de Geus-Oei LF, Pieters GF, Bonenkamp JJ, Mudde AH, Bleeker-Rovers CP, Corstens FH, Oyen WJ. 18F-FDG PET reduces unnecessary hemithyroidectomies for thyroid nodules with inconclusive cytologic results. J Nucl Med. 2006;47:770-775. [PubMed] |
| 6. | Ota H, Ito Y, Matsuzuka F, Kuma S, Fukata S, Morita S, Kobayashi K, Nakamura Y, Kakudo K, Amino N. Usefulness of ultrasonography for diagnosis of malignant lymphoma of the thyroid. Thyroid. 2006;16:983-987. [PubMed] |
| 7. | Fish SA, Langer JE, Mandel SJ. Sonographic imaging of thyroid nodules and cervical lymph nodes. Endocrinol Metab Clin North Am. 2008;37:401-417, ix. [PubMed] |
| 8. | Kabaker AS, Tublin ME, Nikiforov YE, Armstrong MJ, Hodak SP, Stang MT, McCoy KL, Carty SE, Yip L. Suspicious ultrasound characteristics predict BRAF V600E-positive papillary thyroid carcinoma. Thyroid. 2012;22:585-589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 9. | Atli M, Akgul M, Saryal M, Daglar G, Yasti AC, Kama NA. Thyroid incidentalomas: prediction of malignancy and management. Int Surg. 2006;91:237-244. [PubMed] |
| 10. | Mitchell JC, Grant F, Evenson AR, Parker JA, Hasselgren PO, Parangi S. Preoperative evaluation of thyroid nodules with 18FDG-PET/CT. Surgery. 2005;138:1166-1174; discussion 1174-1175. [PubMed] |
| 11. | Lawrence W, Kaplan BJ. Diagnosis and management of patients with thyroid nodules. J Surg Oncol. 2002;80:157-170. [PubMed] |
| 12. | Datta RV, Petrelli NJ, Ramzy J. Evaluation and management of incidentally discovered thyroid nodules. Surg Oncol. 2006;15:33-42. [PubMed] |
| 13. | Chan WF, Lo CY, Lam KY, Wan KY. Recurrent laryngeal nerve palsy in well-differentiated thyroid carcinoma: clinicopathologic features and outcome study. World J Surg. 2004;28:1093-1098. [PubMed] |
| 14. | Lansford CD, Teknos TN. Evaluation of the thyroid nodule. Cancer Control. 2006;13:89-98. [PubMed] |
| 15. | Stang MT, Carty SE. Recent developments in predicting thyroid malignancy. Curr Opin Oncol. 2009;21:11-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | McCaffrey TV. Evaluation of the thyroid nodule. Cancer Control. 2000;7:223-228. [PubMed] |
| 17. | Takeyama H, Tabei I, Uchida K, Morikawa T. Sentinel node biopsy for follicular tumours of the thyroid gland. Br J Surg. 2009;96:490-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |