Published online Jul 15, 2022. doi: 10.5412/wjsp.v12.i1.8
Peer-review started: February 3, 2022
First decision: March 12, 2022
Revised: March 27, 2022
Accepted: April 8, 2022
Article in press: April 8, 2022
Published online: July 15, 2022
Processing time: 159 Days and 15.9 Hours
Thyroid storm is an uncommon condition manifesting in severe thyrotoxicosis with a high mortality rate. The concurrence of peptic ulcer disease and hyper
A 53-year-old male chronic smoker, with no previous medical history, presented with severe generalized abdominal pain and vomiting for one day duration. Further history revealed weight loss, diarrhea, and anxiety over the past three months. On clinical examination, patient was febrile with temperature of 38.6 Degrees Celsius and tachycardic at 130-140 beats per minute, his blood pressure was low at 90/50mmHg. His abdomen was tender with generalized peritonism. In view of his clinical history, a thyroid screen was ordered which showed raised thyroxine (T4) levels of 90.3 pmol/L and low thyroxine stimulating hormone (TSH) levels of 0.005 μU/mL. Chest X-ray showed no sub-diaphragmatic free air, but contrasted CT scan revealed pneumoperitoneum with large amount of intraabdominal free fluid. The working diagnosis was perforated peptic ulcer complicated by thyroid storm. An urgent endocrinologist consult was made, and patient was started on beta blocker and intravenous steroids pre-operatively. The patient underwent emergency laparotomy with washout and patch repair of the perforated gastric ulcer. Patient was monitored post-operatively in intensive care unit and required IV hydrocortisone and Lugol’s iodine. Histology of the ulcer edges showed no malignancy. On post-operative day seven, T4 decreased to 20.4 pmol/L, TSH was 0.005 mLU/L. His thyroid function test subsequently normalized 3 mo post-operatively with T4 18.1 pmol/L, TSH 1.91 mLU/L. Patient’s recovery was otherwise uneventful. Thyroid receptor antibody subsequently was positive, and patient was managed for Grave’s disease by the endocrinologist.
This case highlights the rare but life-threatening clinical emergency of peptic ulcer perforation complicated by thyroid storm. Multidisciplinary perioperative management is crucial to optimize patient for surgery and damage control principles should be taken for an acute surgical patient with concurrent endocrine crisis.
Core Tip: Concurrent peptic ulcer perforation and thyroid storm is a rare but life-threatening surgical emergency. Multidisciplinary perioperative management is crucial to optimize patient for surgery, and damage control principles should be taken for an acute surgical patient with concurrent endocrine crisis.
- Citation: Wang JX, Soh LS, Mahendran DCJ, Woon CY, Chia CLK. Rare case of perforated giant gastric ulcer with concurrent thyroid storm: A case report. World J Surg Proced 2022; 12(1): 8-12
- URL: https://www.wjgnet.com/2219-2832/full/v12/i1/8.htm
- DOI: https://dx.doi.org/10.5412/wjsp.v12.i1.8
Thyroid storm is an acute, life-threatening, hypermetabolic state manifesting in severe thyrotoxicosis. This condition is uncommon and associated with a high mortality rate. The concurrence of peptic ulcer disease and hyperthyroidism is rare and the association between these two conditions is unusual. Few reports of perforated peptic ulcer complicated by thyroid storm have been reported, and these patients underwent trial of conservative management to optimize thyroid status before some required delayed surgical repair to control sepsis. We present a patient with perforated giant gastric ulcer with concurrent thyroid storm who was peritonitic and underwent damage control surgery with patch repair with falciform ligament and recovered uneventfully.
A 53-year-old male chronic smoker, with no past medical history presented to the emergency department with severe generalized abdominal pain and vomiting for one day duration.
Patient’s symptoms started acutely one day ago. A history of weight loss, diarrhea and, anxiety over the preceding three months was also elicited from the patient.
The patient had no past medical history.
The patient had no significant personal and family history.
Clinically, patient was febrile with temperature of 38.6 Degrees Celsius and tachycardic at 130-140 beats per minute, blood pressure was 90/50 mmHg. On examination, his abdomen was tender with generalized peritonism. There was no goiter.
A thyroid screen was performed in view of patient’s history, which revealed a markedly raised thyroxine (T4) levels (90.3 pmol/L) and low levels of thyroid stimulating hormone (TSH) (0.005 μU/mL) that suggested primary hyperthyroidism.
Chest X-ray showed no sub-diaphragmatic free air. A contrasted CT scan was performed and revealed pneumoperitoneum with large amount of intraabdominal free fluid.
In view of the suspicion of a concurrent acute thyroid storm in this patient with perforated viscus, a multidisciplinary consult was made with endocrinologist and pharmacist and patient was started on beta blocker and intravenous steroids pre-operatively.
The patient underwent emergency laparotomy, and a perforated giant gastric ulcer was found.
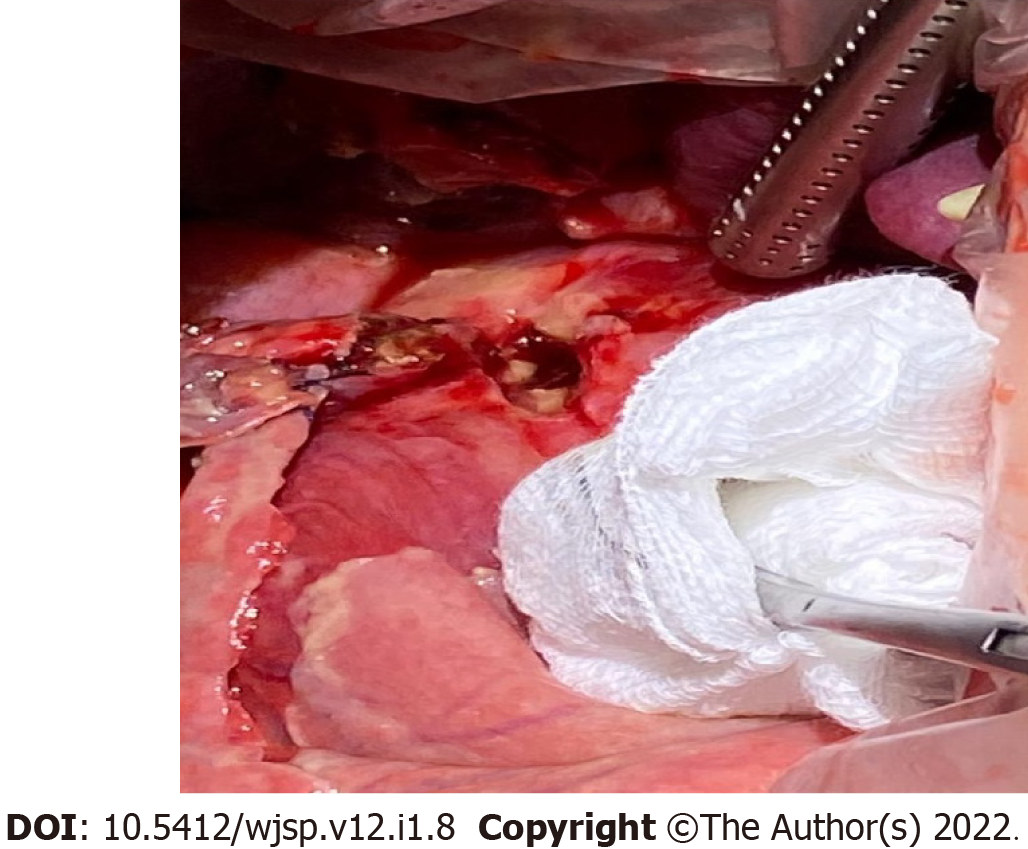
Patient was optimized pre-operatively with beta blocker and intravenous steroids pre-operatively. Intra-operatively, there was gross soilage with a perforated 2.5cm gastric antral ulcer (Figure 1). Damage control surgery was performed, comprising washout and patch repair using a tongue of falciform ligament. Post-operatively, he required IV hydrocortisone and Lugol’s iodine with monitoring in intensive care unit (ICU). Hydrocortisone was weaned off after 48 h and patient was started on propylthiouracil (PTU) with sips of water. Feeds were commenced after 3 days and PTU was subsequently changed to oral carbimazole (30 mg/d) on discharge. On post-operative day seven, T4 decreased to 20.4 pmol/L, TSH was 0.005 mLU/L. His thyroid function test subsequently normalized 3 mo post-operatively with T4 at 18.1 pmol/L, TSH 1.91 mLU/L. Ulcer edge histopathology showed organizing fibrosis with no malignancy. Thyroid receptor antibody returned as positive, and he was managed by the endocrinologist for Grave’s disease.
The patient had an uneventful postoperative clinical course and was discharged one week post-operatively. He is on follow-up with the endocrinologist for Grave’s disease in the outpatient clinic.
Although causes for peptic ulcer disease (PUD) are well described, the association between hyperthyroidism and PUD is unusual due to differences in the autonomic activity behind these two disorders. PUD exhibits a parasympathetic predominance whereas sympathetic activity predominates in hyperthyroidism[1] with Ebert et al[2] showing that acid secretion is reduced in hyperthyroidism. These findings underscore the rarity of concurrent PUD with hyperthyroidism.
There are 3 cases of perforated peptic ulcer[3-5] complicated by thyroid storm reported in literature. All were treated conservatively till thyroid function improved prior to ulcer repair. While the Burch-Wartofsky score is routinely used as a diagnostic tool for thyroid storm, we note that there are conflicting factors in its calculation due to concurrent sepsis driving tachycardia and fever. However, the clinical history with markedly elevated T4 Levels and suppressed TSH levels suggested underlying untreated hyperthyroidism rather than an acute stress response.
Our patient was clinically septic and had generalized peritonism. IV beta-blockers and steroids were for rapid control of metabolic effects of thyrotoxicosis. Oral PTU was not used as in view of the perforation and requirements to be fasted. The alternative is rectal PTU prepared by the in-house pharmacist, but this requires 3-4 h of lead time. PTU takes days to manifest its anti-thyroid effects. Due to sepsis and peritonism, medical therapy and delay to further optimize him was inappropriate. Therefore, decision was made for emergency laparotomy.
Options for a giant gastric ulcer (defined as ulcer diameter > 2 cm) can be broadly divided into primary repair or resection surgery. The principles of damage control surgery in a severely physiologically challenged patient are central to the decision regarding the type of surgery. The aim is expeditious control of contamination and bringing the patient back to ICU for further resuscitation and restoration of physiology. Hence, a patch repair was chosen instead of a prolonged major resection. However, the lack of omentum in this thin patient made a patch repair challenging. As such an alternative using the falciform ligament which lies across the first part of the duodenum was chosen and easily mobilized for a tension-free patch repair. This case also highlights the utility of falciform ligament pedicle flap[6] as an alternative approach to repair perforated giant gastric ulcers and an attempt should be made to preserve the falciform ligament as a backup during initial midline laparotomy for a perforated viscus rather than routinely ligating and dividing it. Another alternative option to a damage control patch repair for large gastric ulcer perforation would be an ulcerectomy with/without pyloroplasty if a patch repair is deemed insufficient.
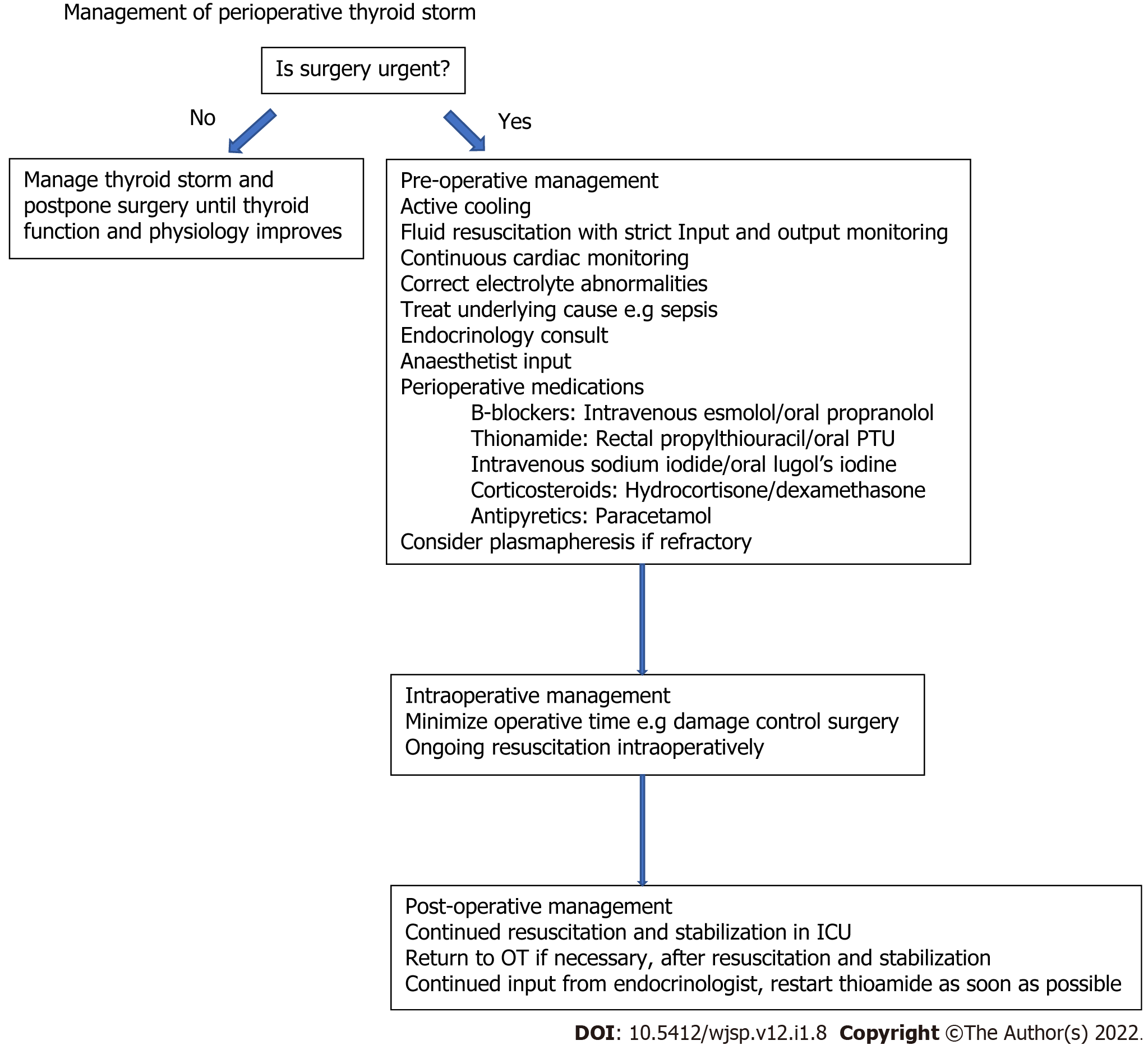
Postoperatively, the patient was transferred to ICU. The key principles of post-operative critical care management in this patient include aggressive resuscitation with fluids and empirical antibiotics, correction of thyroid dysfunction and nutritional support. Multidisciplinary collaboration involving the surgeon, intensivist and endocrinologist is key to good outcomes in an acute surgical patient with concurrent thyroid storm. A flowchart illustrating the principles of management is summarized in Figure 2.
Concurrent peptic ulcer perforation with thyroid storm is a rare but life-threatening surgical emergency. Multidisciplinary perioperative management and damage control surgery are critical to control sepsis, restore physiology and correct thyroid dysfunction in an expeditious fashion.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Singapore
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Awad AK, Egypt; Gao L, China; Luo XZ, China S-Editor: Wang LL L-Editor: A P-Editor: Wang LL
| 1. | Gill AM, Walton FW. Hyperthyroidism and peptic ulcer. Lancet. 1952;1:693-694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (1)] |
| 2. | Ebert EC. The Thyroid and the Gut. J Clin Gastroenterol. 2010;44:402-406. [RCA] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 88] [Article Influence: 5.9] [Reference Citation Analysis (1)] |
| 3. | Ogiso S, Inamoto S, Hata H, Yamaguchi T, Otani T, Koizumi K. Successful treatment of gastric perforation with thyrotoxic crisis. Am J Emerg Med. 2008;26:1065.e3-1065.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Zweig SB, Schlosser JR, Thomas SA, Levy CJ, Fleckman AM. Rectal administration of propylthiouracil in suppository form in patients with thyrotoxicosis and critical illness: case report and review of literature. Endocr Pract. 2006;12:43-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Alfadhli E, Gianoukakis AG. Management of severe thyrotoxicosis when the gastrointestinal tract is compromised. Thyroid. 2011;21:215-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Boshnaq M, Thakrar A, Martini I, Doughan S. Utilisation of the falciform ligament pedicle flap as an alternative approach for the repair of a perforated gastric ulcer. BMJ Case Rep. 2016;2016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |