Copyright
©2014 Baishideng Publishing Group Inc.
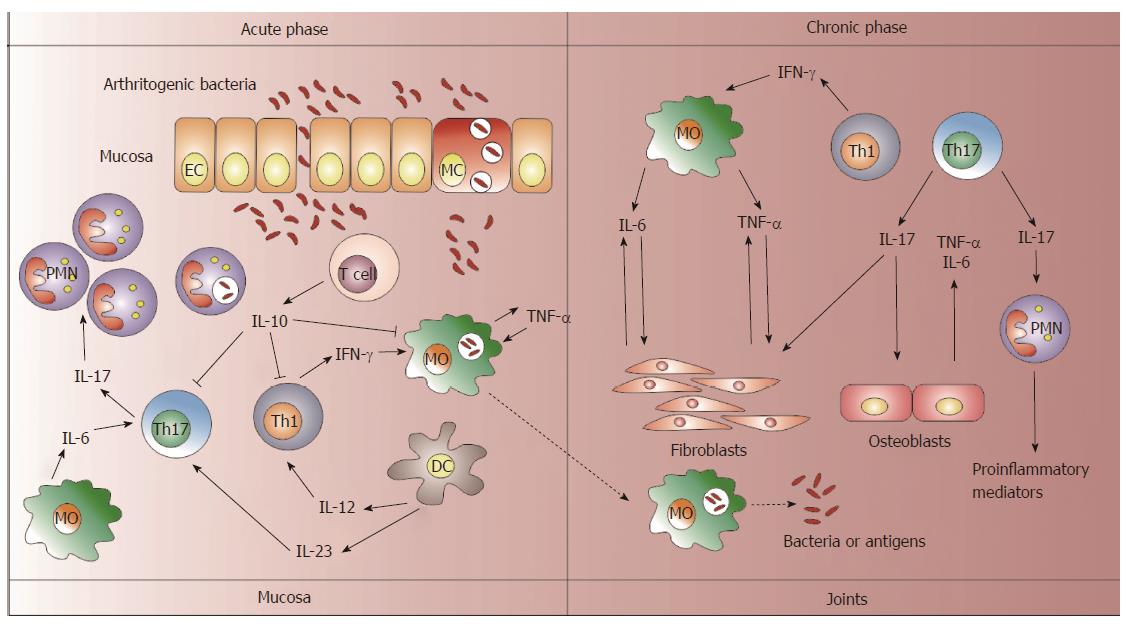
Figure 1 The role of cytokines in reactive arthritis depending on the state of disease.
Arthritogenic bacteria enter through the gastrointestinal or genitourinary mucosa using different strategies (M cells; epithelial cells) and induce an inflammatory response. During the acute stage, interleukin (IL)-12 and IL-23 plus IL-6 promote the development of Th1 and Th17 cells, respectively. These cells are a major source of interferon (IFN)-γ and IL-17, favoring the bacterial clearance. The IFN-γ activates macrophages to kill phagocyted bacteria and secrete tumor necrosis factor (TNF)-α. IL-17 induces the migration of polymorphonuclear cells to the site of infection. However, this effect could be disrupted by the action of regulatory T cells producing IL-10. This regulatory event contributes to the bacterial persistence in the mucosa. Then, the bacteria could reach the joint transported by macrophages. In chronic stages, IL-6, TNF-α, IFN-γ and IL-17 exert pro-inflammatory roles in the joint. These cytokines stimulate articular cells (e.g., fibroblasts, osteoblast) and immune cells to produce more cytokines and pro-inflammatory mediators that contribute to chronic articular inflammation. These effects may be enhanced by the presence of bacteria or bacterial antigens in the joint. EC: Epithelial cell; MC: M cell; MO: Macrophage; PMN: Polymorphonuclear cell; DC: Dendritic cell.
- Citation: Eliçabe RJ, Genaro MSD. Immunopathogenesis of reactive arthritis: Role of the cytokines. World J Immunol 2014; 4(2): 78-87
- URL: https://www.wjgnet.com/2219-2824/full/v4/i2/78.htm
- DOI: https://dx.doi.org/10.5411/wji.v4.i2.78