Peer-review started: September 25, 2018
First decision: November 20, 2018
Revised: November 22, 2018
Accepted: January 21, 2019
Article in press: January 22, 2019
Published online: March 12, 2019
Processing time: 169 Days and 10.1 Hours
Trans-urethral resection of prostate (TURP) is one of the most commonly performed operations in urology to treat bladder outflow obstruction (BOO) in men. TURP surgery is also a key for endo-urological training in the British National Health Service (NHS) for training junior urologists. The working hypothesis is that prostate resection speed (PRS) in the context of bipolar TURP surgery, is not a key factor in major complication rates or broad patient outcomes at 3 mo after surgery, and therefore supervising consultants should not focus primarily on resection speed when teaching TURP.
To investigate objective differences in consultants vs trainees PRS and whether PRS affected complication rates/outcomes after TURP.
Retrospective descriptive study analyzing patient case-notes, operative and electronic records, study undertaken at Burton Queen’s Hospital NHS Foundation Trust, United Kingdom, a secondary care centre in the public sector of the NHS. Participants included: all Bipolar TURPs undertaken between 13/04/2016 and 27/06/2017. Exclusions: patients undergoing concomitant operations or where intra-operative equipment problems occurred. Resected prostate (g), operative time, post-operative complications and outcomes at 3-mo were obtained from electronic records. Clavien-Dindo Grade II complications or above considered significant. Binary successful yes/no outcome at 3-mo after surgery included both patients who reported moderate to significant symptom improvement, or being catheter-free for those catheterized before TURP.
157 patients were identified. After exclusion a total of 125 patients were included from analysis. The mean PRS for trainees (0.34 g/min) was found to be lower than the mean PRS for consultants (0.41 g/min). The operating urologist’s PRS was not observed to be related to the number of TURPs that they performed during the period of the study. The trainee vs consultant means post-operative success rates (86.5% vs 90.5%) were comparable. The Trainees’ patients did not suffer any significant complications as defined by the study. There was no clear relationship observed between PRS and the rate of significant post-operative complications or patients’ 3-mo binary successful outcome. PRS was noted to increase with increasing intra-operative experience for both Trainees 1 and 2 when comparing the first half of their TURPs to their latter half.
Consultants have a higher PRS in comparison to trainees. There is no trend between PRS and significant post-operative complication rates or 3-mo outcomes.
Core tip: Transurethral resection of prostate (TURP) is a common operation for treating bladder outflow obstruction. Prolonged intra-operative resection time is reported to increase complication rates. This study aimed to assess for objective differences in consultants vs trainees prostate resection speed (PRS) and whether differences in PRS affected complication rates and broad patient outcomes after TURP. The study found higher PRS for consultants however no difference in serious complications or broad patient outcomes. The authors therefore recommend that consultant urologists should not primarily focus on their trainee’s PRS when training them in TURP surgery.
- Citation: Donati-Bourne J, Nour S, Angova E, Delves G. Prostate resection speed: A key factor for training and broad outcomes? World J Clin Urol 2019; 8(1): 1-8
- URL: https://www.wjgnet.com/2219-2816/full/v8/i1/1.htm
- DOI: https://dx.doi.org/10.5410/wjcu.v8.i1.1
Trans-urethral resection of prostate (TURP) is one of the most commonly performed operations in urology to treat bladder outflow obstruction (BOO) in men.
Increasing the operative time of TURP surgery is reported to adversely impact patient factors such as fluid shifts, post-operative bleeding and thrombo-embolic events[1] and indeed experts suggest urologists should limit their TURP resection time to 60 min[2].
The operating urologist’s prostate resection speed (PRS) must therefore balance a speed sufficiently high to create an open cavity within the available indicated operative time, without jeopardizing patient safety and increasing risk of iatrogenic injuries.
There is however no defined PRS which a urologist should aim to operate at[1], furthermore studies have demonstrated that greater degrees of prostatic resection have not resulted in significant variations in long-term improvements in BOO symptoms after surgery[3,4].
TURP surgery is also key for endo-urological training in the British National Health Service (NHS), allowing the junior urologist to improve their cystoscopic skills, gain confidence with endoscopic equipment and familiarize themselves with genito-urinary anatomy[5].
United Kingdom trainee urologists are currently required to perform at least 120 TURPs to achieve their Certificate of Completion of Training, and therefore in the NHS TURP is often performed by trainees under consultant supervision[6]. Many trainees will recall their consultant during their training urging them to increase their PRS[7], however most surgeons would agree that the perception of the passage of time in theatre differs when observing surgery compared to performing it[8].
This study aimed to evaluate whether there was an objective difference in consultants vs trainees PRS and whether any such differences in PRS affected complication rates and outcomes after TURP. The study also aimed to use the findings to discuss the true merit of urology trainers evaluating their trainees by their PRS.
The study was undertaken retrospectively and is descriptive. All Bipolar TURPs performed in a single center of 5 urology consultants and 2 United Kingdom nationally appointed urology trainees between 13/04/2016 and 27/06/2017 were included in the study. The dates of the study were selected to allow for a representative number of TURPs to be performed by each surgeon for analysis.
Both trainees were in their third year of a 5-year higher urological training pathway, had performed fewer than 30 TURP operations independently prior to the start of the study and all their operations within the study were undertaken independently with un-scrubbed consultant supervision. The trainees had not received any simulated training prior to the study.
Patients undergoing concomitant operations at the time of TURP (e.g., circumcision or cystolitholapaxy) or where unexpected intra-operative equipment problems occurred were excluded.
Mass of resected prostate tissue in grams, operative time in minutes, occurrence of post-operative complications and outcomes at 3-mo after surgery were obtained from electronic records.
Clavien-Dindo Grade II complications or above only were considered significant for the study and therefore included in the analysis.
Patients that were defined as suffering post-operative bleeding complication included any who needed: continuous bladder irrigation and manual washout for 3 d or more post-TURP, and/or; a blood transfusion, and/or; return to theatre for formal bladder washout
Post-operative sepsis events were recorded as those diagnosed and treated by the attending doctor, with or without the subsequent confirmation of a positive blood culture.
A binary rather than qualitative outcome patient evaluation tool was used to record successful versus unsuccessful outcomes at 3-mo after TURP surgery.
For those already catheterized prior to TURP a binary successful outcome was deemed as achieving catheter-free status at 3 mo after surgery.
For non-catheterized patients, binary successful outcome was a subjective patient-reported moderate or significant improvement in Lower Urinary Tract Symptoms (LUTS) on direct enquiry at the 3 mo follow up clinic appointment with the operating consultant. Mild or no improvement in patient-reported LUTS at 3 mo after TURP was deemed unsuccessful outcome.
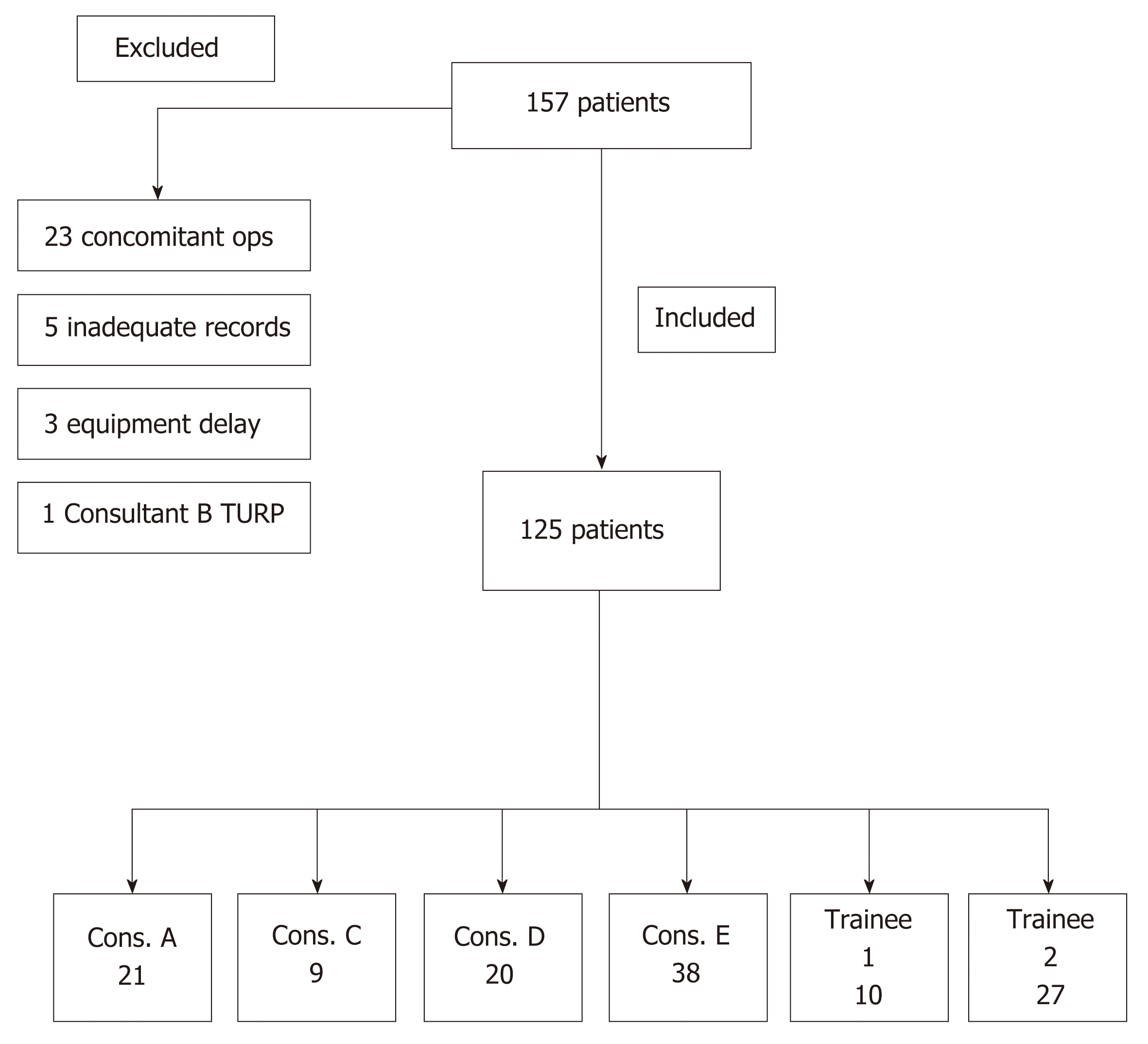
One hundred and fifty seven patients underwent Bipolar TURP surgery during the timeframe of the study. All cases were done electively in the same operating theatre of the hospital.
The following patients were excluded from analysis: (1) 23 had concomitant operations (14 cystolitholapaxy, 3 urethral dilatation, 2 optical urethrotomy, 2 circumcision, 2 bladder biopsy); (2) 5 inadequate electronic records/results for analysis; and (3) 3 intra-operative equipment problems that prolonged operative time,
Consultant B had supervised Trainee 1 and 2 undertaking TURPs but personally performed only 1 TURP during the study timeframe and therefore their patient were not included in analysis.
All cases performed by trainees were performed under consultant supervision, scrubbed or unscrubbed in theatre. 125 patients were included for analysis. The breakdown of operations performed is illustrated in Figure 1.
Results for individual operating surgeons including caseload, PRS, Clavien-Dindo Grade II or above complication rate and binary successful outcome rates are illustrated in Table 1.
| Operating Surgeon | No. TURP performed | Mean PRS (g/min) | % Clavien-Dindo ≥ Grade II | % Successful outcome at 3 mo |
| Consultant A | 21 | 0.59 | 14 | 95 |
| Consultant C | 9 | 0.40 | 11 | 100 |
| Consultant D | 20 | 0.23 | 10 | 85 |
| Consultant E | 38 | 0.43 | 16 | 82 |
| Trainee 1 | 10 | 0.31 | 0 | 80 |
| Trainee 2 | 27 | 0.36 | 0 | 93 |
The mean PRS of trainees was 0.34 g/min (range 0.31 to 0.36) and this was lower than the mean PRS of 0.41 g/min (range 0.23 to 0.59) for consultants.
Mean rates of binary outcome as successful were comparable for trainees at 86.5% (range 80–93) and consultants at 90.5% (range 82–100).
Details of Clavien-Dindo II or above complications are listed in Table 2. No relationship was observed between increasing PRS and rate of significant post-operative complications. The trainees’ patients did not suffer any significant complications as defined by the study. No fatalities were recorded during the study. Two patients had to be taken back to theatre for a formal bladder washout under general anaesthesia, six suffered post-operative sepsis, one received a blood transfusion and three required prolonged ward-based bladder irrigation and washouts.
| Surgeon | No. of Significant complications/total TURPs | Bleeding | Post-operative sepsis |
| Consultant A | 3/21 | 2 | 1 |
| Consultant C | 1/9 | 0 | 1 |
| Consultant D | 2/20 | 1 | 1 |
| Consultant E | 6/38 | 3 | 3 |
| Trainee 1 | 0/10 | - | - |
| Trainee 2 | 0/27 | - | - |
No relationship was observed between PRS and rate of binary successful outcome at 3 mo. PRS was not observed to be related to number of TURPs performed. PRS increased with increasing experience for Trainees 1 and 2 when comparing the first half of their TURPs (mean 0.28 g/min, range 0.26-0.29) to their latter half (mean 0.41, range 0.33–0.48) (Table 3).
| Mean PRS (g/min) in first half of cases | Mean PRS (g/min) in second half of cases | |
| Trainee 1 | 0.29 | 0.33 |
| Trainee 2 | 0.26 | 0.48 |
For Trainee 1 the mean PRS in the first half of cases was 0.29 g/min and this increased to 0.33 g/min in their latter half, whilst for Trainee 2 the mean PRS was 0.26 g/min in their first half increasing to 0.48 g/min in their latter half.
The study is descriptive and the authors discuss the findings of the first 14 mo of the study accordingly. In the study’s hospital the urology Consultants had higher mean PRS than Trainees during TURP and therefore most probably correctly identified the PRS of their trainee was slower than theirs. The consultants mean PRS of 0.41 g/min is however lower than PRS figures approximating 0.6g/minute quoted in other TURP series[9,10].
Urology trainees will encounter a learning curve during their TURP training. A retrospective review of more than 4000 TURPs performed by a single surgeon over 25 years concluded only 81 operations were needed before the surgeon's skill reaches a plateau in TURP[11]. The United Kingdom requirement of 120 TURPs for Completion Certificate of Training in urology hence appears sufficient number to be deemed competent at performing TURP independently.
The key factor that increases a urologist’s PRS is increasing experience[11,12] as confidence handling cystoscopic equipment, achieving haemostasis and familiarity with anatomy improve. The trainees demonstrated an increase in PRS when comparing the first and latter halves of their cases, hence trainers need not focus primarily on speed as they can expect a natural acquisition of PRS in their trainees that will be achieved as their experience increases.
Furthermore the traditional notion of TURP surgery being a highly time sensitive operation, whereby sufficient prostate must be resected whilst minimizing the time-associated risk of TUR syndrome, has been challenged with bipolar TURP[2]. Simultaneous tissue coagulation during bipolar resection improves visualization thus increasing time proportionally spent resecting, and the substitution of glycine with normal saline as irrigation fluid reduces risk of TUR syndrome[13]. The authors accept that the findings of the study may differ with the use of monopolar TURP.
Other factors that may impact PRS by affecting bleeding include whether or not the patient is pre-operatively on finasteride, the presence of a catheter prior to surgery and intra-operative hypertension[14]. These factors were not controlled in our study and were not assessed as the authors deemed these to be beyond the scope of the study. The consultants however did not allocate cases to trainees based on these factors and no pre-operative case selection was undertaken.
The study’s binary successful outcome tool arguably does not facilitate an in-depth qualitative outcome analysis and therefore is considered a study limitation. Achieving catheter-free status after TURP however is one of the main preoccupations in patients with a catheter prior to surgery, and hence the authors believe that success in catheter removal is a highly relevant outcome. Likewise achieving a subjectively reported moderate or significant improvement in LUTS at 3-mo after surgery can be considered a valid tool for broadly deeming whether TURP was successful or not.
As such mean binary successful outcome rates were comparable for consultants (90.5%) and trainees (86.5%) and no relationship between PRS and successful outcome at 3-mo was demonstrable. For example Consultant C and E had the two closest PRS values (0.40 g/min vs 0.43 g/min) yet one of the greatest differences in successful outcome rates (100% vs 82%).
To the authors’ knowledge no study in the literature directly compares PRS with symptomatic outcome after TURP, however the relationship between mass of prostate resected and post-operative LUTS improvement is weak. In a prospective trial by Hakenberg et al[4] the Qmax, IPSS and residual urine of 138 patients were documented prior to TURP and re-evaluated 3 and 6 mo after surgery, and the resected tissue weight (RTW) was recorded for each. No statistically significant relationship was found between RTW and IPSS change. Trainers therefore should not primarily focus on trainee’s PRS during TURP training based on symptomatic outcome alone.
Clavien-Dindo Grade I complications were not considered and present another study limitation.
PRS however had no observable relationship with rates of Clavien-Dindo Grade II complications or above after TURP. For example Consultants C and D had closest complication rates (11% vs 10%) but significantly different PRS (0.40 g/min vs 0.23 g/min).
The patients operated on by trainees did not experience Clavien-Dindo Grade II or above complications, however this may be due to pre-operative case selection – higher-risk patients more likely to suffer complications were preemptively operated on by consultants.
No trend was observed between operative time and complication rates – these occurred in cases with mean operative time of 47.5 min (range 34-67), compared to mean operating time for all cases of 47.1 minutes (range 5-116).
The mean PRS for cases suffering complications (0.49 g/min) was greater than mean PRS for all cases (0.39 g/min). This suggests a slower PRS is less likely to yield complications in bipolar TURP, however it is also possible that the urologist who deemed a patient as medically high-risk chose to resect faster in an attempt to minimize operative time. The findings therefore do not suggest trainers should urge their urological trainees to increase their PRS based on rates of post-operative complications alone.
The limitations of the study include its descriptive nature and lack of in-depth qualitative analysis in patient outcomes, the exclusion of Clavien-Dindo I complications and the comparably small numbers of operations performed by Consultants B and C and Trainee 1.
The authors propose further studies compare PRS objectively with changes in IPSS before and after TURP, as well as with other post-operative factors such as length of in-patient stay and incidence of Clavien-Dindo Grade I complications.
In conclusion, the authors propose based on this descriptive study that trainers in urology teaching how to perform TURP surgery should focus primarily on adequate patient selection, sound surgical techniques and optimizing post-operative care, rather than the PRS of their up-and-coming budding urologists.
Trans-urethral resection of prostate (TURP) is one of the most commonly performed operations in urology to treat bladder outflow obstruction (BOO) in men as well as a key endo-urological training tool in the British National Health Service (NHS) for training junior urologists. The working hypothesis is that prostate resection speed (PRS) in the context of bipolar TURP surgery, is not a key factor in major complication rates or broad patient outcomes at 3 mo after surgery, and therefore supervising consultants should not focus primarily on resection speed when teaching TURP.
The study was motivated to identify whether resection speed during TURP training should be a key factor.
The main objective was to identify whether TURP resection speed affected significant complication and broad outcomes at 3 mo. The study found that resection speed did not correlate with significant complication and broad outcomes at 3 mo. The authors propose that PRS should not be a key factor during TURP training.
Participants included: all Bipolar TURPs undertaken between 13/04/2016 and 27/06/2017. Exclusions: patients undergoing concomitant operations or where intra-operative equipment problems occurred. Patients identified via operative logbooks and case notes retrieved electronically.
The study found that PRS did not correlate with significant complication and broad outcomes at 3 mo. The authors propose a similar study with increased power and qualitative assessment of symptomatic improvement in relation to PRS.
PRS did not correlate with significant complication and broad outcomes at 3 mo. The authors conclude that PRS should not be a key factor during TURP training as increasing experience will lead to natural acquisition of speed. PRS is not a cardinal factor in bipolar TURP surgery for significant complication rates or broad outcomes 3 mo after surgery. In the era of monopolar TURP resection, PRS was highly relevant due to risks of TURP syndrome. In bipolar surgery the use of saline as irrigation fluid minimises this risk. Therefore the authors propose a paradigm shift in training whereby less focus is placed on PRS and greater emphasis on sound safe surgical technique.
The authors propose a paradigm shift in training whereby less focus is placed on PRS and greater emphasis on sound safe surgical technique. The authors propose a similar study with increased power and qualitative assessment of post-operative symptomatic improvement in relation to PRS. Prospective high-powered study with IPSS evaluation pre- and post-TURP and correlation with PRS.
The authors wish to thank Mr Waliul Islam, Mr Shashank Kulkarni, Mr Sikander Khwaja, Mr Anthony Noah and Miss Jyoti Shah.
Manuscript source: Unsolicited manuscript
Specialty type: Urology and nephrology
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Mazaris E S- Editor: Cui LJ L- Editor: A E- Editor: Zhang YL
| 1. | Rassweiler J, Teber D, Kuntz R, Hofmann R. Complications of transurethral resection of the prostate (TURP)--incidence, management, and prevention. Eur Urol. 2006;50:969-979; discussion 980. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 770] [Cited by in RCA: 839] [Article Influence: 44.2] [Reference Citation Analysis (0)] |
| 2. | Issa MM, Young MR, Bullock AR, Bouet R, Petros JA. Dilutional hyponatremia of TURP syndrome: a historical event in the 21st century. Urology. 2004;64:298-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 55] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 3. | Tan AH, Gilling PJ, Kennett KM, Frampton C, Westenberg AM, Fraundorfer MR. A randomized trial comparing holmium laser enucleation of the prostate with transurethral resection of the prostate for the treatment of bladder outlet obstruction secondary to benign prostatic hyperplasia in large glands (40 to 200 grams). J Urol. 2003;170:1270-1274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 236] [Cited by in RCA: 221] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 4. | Hakenberg OW, Helke C, Manseck A, Wirth MP. Is there a relationship between the amount of tissue removed at transurethral resection of the prostate and clinical improvement in benign prostatic hyperplasia. Eur Urol. 2001;39:412-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Sweet RM. Review of trainers for transurethral resection of the prostate skills. J Endourol. 2007;21:280-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Bright E, Vine S, Wilson MR, Masters RS, McGrath JS. Face validity, construct validity and training benefits of a virtual reality TURP simulator. Int J Surg. 2012;10:163-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Issa MM. Technological advances in transurethral resection of the prostate: bipolar versus monopolar TURP. J Endourol. 2008;22:1587-1595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 85] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 8. | MacDonald J, Williams RG, Rogers DA. Self-assessment in simulation-based surgical skills training. Am J Surg. 2003;185:319-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 79] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 9. | Muzzonigro G, Milanese G, Minardi D, Yehia M, Galosi AB, Dellabella M. Safety and efficacy of transurethral resection of prostate glands up to 150 ml: a prospective comparative study with 1 year of followup. J Urol. 2004;172:611-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Berger AP, Wirtenberger W, Bektic J, Steiner H, Spranger R, Bartsch G, Horninger W. Safer transurethral resection of the prostate: coagulating intermittent cutting reduces hemostatic complications. J Urol. 2004;171:289-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Furuya S, Furuya R, Ogura H, Araki T, Arita T. [A study of 4,031 patients of transurethral resection of the prostate performed by one surgeon: learning curve, surgical results and postoperative complications]. Hinyokika Kiyo. 2006;52:609-614. [PubMed] |
| 12. | Yamaçake KG, Nakano ET, Soares IB, Cordeiro P, Srougi M, Antunes AA. Analysis of the learning curve for transurethral resection of the prostate. Is there any influence of musical instrument and video game skills on surgical performance? Turk J Urol. 2015;41:132-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Starkman JS, Santucci RA. Comparison of bipolar transurethral resection of the prostate with standard transurethral prostatectomy: shorter stay, earlier catheter removal and fewer complications. BJU Int. 2005;95:69-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 112] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 14. | Donohue JF, Sharma H, Abraham R, Natalwala S, Thomas DR, Foster MC. Transurethral prostate resection and bleeding: a randomized, placebo controlled trial of role of finasteride for decreasing operative blood loss. J Urol. 2002;168:2024-2026. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 53] [Article Influence: 2.3] [Reference Citation Analysis (0)] |