Published online Nov 24, 2016. doi: 10.5410/wjcu.v5.i3.93
Peer-review started: July 21, 2016
First decision: September 5, 2016
Revised: September 21, 2016
Accepted: October 22, 2016
Article in press: October 24, 2016
Published online: November 24, 2016
Processing time: 125 Days and 18.7 Hours
A 61-year-old man with locally advanced prostate cancer was found to have multiple solid intra-abdominal solid lesions during staging investigations. While some were in the pelvis, they were not located in the common landing sites for prostate cancer metastases, and his prostate specific antigen was not significantly elevated to suggest a high burden of metastatic disease. He reported a history of a blunt abdominal trauma due to a motor vehicle accident more than forty years ago which had been conservatively managed. His staging imaging revealed a lack of a discrete spleen in his left upper abdomen and this raised the suspicion that these solid lesions may represent ectopic splenic tissue. Imaging with nuclear medicine scintigraphy confirmed the lesions in his upper abdomen and pelvis to be splenunculi. He proceeded with a combination of androgen deprivation therapy and external beam radiotherapy for locally advanced, non-metastatic prostate cancer. Although it has been described in patients with low risk prostate cancer, this is the first case report of splenunculi mimicking metastases in a patient with locally advanced prostate cancer.
Core tip: The appearance of ectopic splenic tissue in the abdomen and other body cavities can mimic that of solid tissue tumours and metastases. Splenosis may occur following blunt abdominal trauma during which a splenic injury may or may not have been identified and is rarely symptomatic. Being aware of this unusual differential diagnosis may avoid anxiety for patients and allow early diagnosis. Nuclear medicine scintigraphy with Tc-99m is the imaging modality of choice to confirm splenunculi.
- Citation: Foreman D, Plagakis SA. Splenunculi mimicking metastases in a patient with locally advanced prostate cancer. World J Clin Urol 2016; 5(3): 93-96
- URL: https://www.wjgnet.com/2219-2816/full/v5/i3/93.htm
- DOI: https://dx.doi.org/10.5410/wjcu.v5.i3.93
Splenosis is the autotransplantation of splenic tissue and formation of scattered tissue deposits secondary to abdominal trauma or splenectomy. It is a benign condition that is generally asymptomatic with a reported incidence of up to 67% of people who have sustained an abdominal injury[1,2]. Due to increasing rates of abdominal imaging, these cases are now seen more often and the unexpected findings have been mistaken for metastatic disease and hepatoma, as reported in the literature.
We present a case of a 61-year-old man with newly diagnosed locally advanced, high risk prostate cancer, with multiple intra-abdominal masses initially mistaken for metastatic disease. This patient was referred to a Urologist with a prostate specific antigen (PSA) of 6.6 ng/mL. He had no significant medical or family history, apart from being involved in a motor vehicle accident at 18 years of age. The accident involved side impact, and he spent three days in hospital for observation but did not undergo surgery. There was no imaging available from that previous admission.
Digital rectal examination found a generally firm and suspicious feeling prostate gland, and trans-rectal ultrasound (TRUS) showed no hypoechoic lesions. TRUS guided prostate biopsy was performed and revealed a large volume of Gleason 4 + 3 = 7 disease occupying 80%-90% of all cores. The specimen from the right base showed extra-prostatic extension of disease, confirming pathological staging as T3.
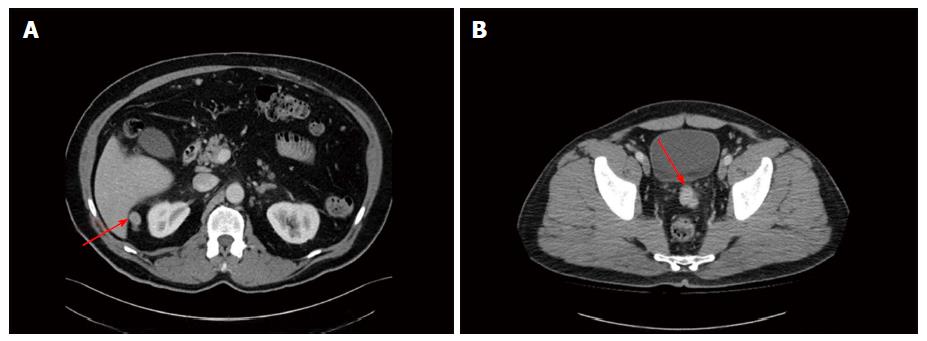
Staging investigations included a computed tomography (CT) scan of the abdomen and pelvis, whole body bone scan (WBBS) and magnetic resonance imaging (MRI) of the pelvis. WBBS did not reveal any bony abnormalities or metastases. CT showed a 2.4 cm lesion between the liver and right kidney and a 3.4 cm lesion between the bladder and rectum, just superior to the seminal vesicles (Figure 1). The lesions were solid and enhanced with intravenous contrast. There was no discrete spleen in the left upper quadrant, however multiple small lesions lay in this region measuring up to 2 cm in diameter each (Figure 2). There was no pelvic or para-aortic lymphadenopathy present. MRI demonstrated disease within the prostate and no gross extraprostatic extension was present. The MRI clearly displayed the pelvic lesion superior to the seminal vesicles, which was not attached to surrounding structures.
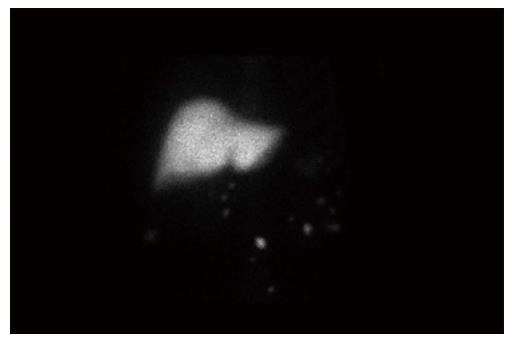
Due to suspicion of ectopic splenic tissue, a heat-damaged radioisotope-labelled red cell scan (99mTc) was performed. All of the lesions seen on CT demonstrated intense tracer uptake and confirmed the presence of multiple intra-abdominal splenunculi (Figure 3), and excluded abdominal metastatic disease.
Following discussion of treatment options for locally advanced, high risk, non metastatic prostate, the patient elected to undergo external beam radiotherapy in combination with 24 mo of androgen deprivation therapy (ADT).
A PSA rise occurred 21 mo after ADT finished, and the patient required intermittent ADT since then. It has been 8 years since diagnosis and the patient is currently off ADT with no metastatic disease on cross sectional imaging and has a PSA of 0.8 ng/mL.
Splenosis is believed to result from the spillage of cells from the splenic pulp during surgical manipulation or following splenic injury. It is reported to develop over an average of 10 years following the insult, and is more common following trauma than iatrogenic causes[3].
The cells can implant in any other location and take their blood supply from surrounding structures; splenosis has been reported as intrathoracic where there is a concomitant diaphragmatic injury or intrahepatic following an emergency splenectomy for trauma[4,5]. The pathogenesis is generally accepted to be mechanical implantation of cells, however there are case reports of intracranial splenic deposits from purported haematological spread[6].
Whilst it is assumed to be functional splenic tissue, splenosis usually does not have the histological appearance of normal spleen, nor does it form a hilum or a mature capsule. Patients are rarely symptomatic and the condition is most often discovered incidentally on abdominal imaging.
This is distinct from an accessory spleen which is congenital and arises from the left side of the dorsal mesogastrium. These deposits are usually found in the region of the gastosplenic ligament or splenopancreatic ligaments, commonly solitary, and if multiple hardly ever exceed six. They are histologically and functionally normal splenic tissue and usually have their own blood supply derived from the splenic artery. They are also usually asymptomatic, but there have been reports of torted accessory spleens and migratory deposits on long vascular pedicles.
The most useful imaging modality by far for investigation of splenosis is nuclear medicine scintigraphy. This can be performed using the agents Technichium-99 sulphur colloid, Technichium-99 heat-damaged erythrocytes or Indium-111 labelled platelets. These agents are widely distributed in the reticuloendothelial system including the liver, bone marrow and spleen. Tc-99m and In-111 labelled platelets are the most sensitive and specific agents for the detection of ectopic splenic tissue[7,8]. If nuclear scintigraphy is not available or conclusive, the option of percutaneous biopsy of the masses can be pursued but this is often challenging given the varying size and location of the masses.
Multiple published case reports describe the initial misdiagnosis of splenosis as solid tumours, metastases or recurrences for breast, renal, colorectal and hepatocellular cancers, to name a few[9-12].
Prostate cancer has been reported once in the literature in this context, in a patient with low grade disease that should not have undergone further imaging according to staging guidelines[13]. This is the first report of splenosis in a patient with high risk prostate cancer.
The presence of splenosis following blunt abdominal trauma is under-recognised and, due to its indolent clinical nature, is usually discovered incidentally years later when it is mistaken for malignant disease. This is the first case report of it appearing in the context of high risk, locally advanced prostate cancer. A heat labelled red cell scan is a sensitive and definitive imaging modality for diagnosis. Early consideration of splenosis and diagnostic confirmation is essential to ensuring appropriate care is instituted in each clinical scenario.
Soft tissue masses in the context of newly diagnosed prostate cancer.
Splenunculi.
Metastatic prostate cancer.
Routine bloods only, no biopsy was required.
Technetium-99 scan confirmed splenunculi.
Ectopic splenic tissue.
Multiple other case reports have indicated this differential diagnosis in the staging of many other cancers, but not locally advanced prostate cancer.
Splenosis is the condition related to ectopic splenic tissue formed as a result of trauma. Accessory spleen is a congenital condition.
One must consider the differential of ectopic splenic tissue in a patient post abdominal trauma, with no discernible spleen, if their soft tissue masses are out of keeping with their expected cancer staging. Technetium-99 scans are the most accurate for assessment of splenic tissue.
This is the first case report of splenunculi mimicking metastases in a patient with locally advanced prostate cancer presented by Foreman D and Plagakis SA. Overall, the case report is quite interesting, well organized and written according to the journal’s style. The language is satisfactory and the figures quite interesting.
Manuscript source: Invited manuscript
Specialty type: Urology and nephrology
Country of origin: Australia
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Gofrit ON, Goluboff ET, Koukourakis GV S- Editor: Ji FF L- Editor: A E- Editor: Li D
| 1. | De Vuysere S, Van Steenbergen W, Aerts R, Van Hauwaert H, Van Beckevoort D, Van Hoe L. Intrahepatic splenosis: imaging features. Abdom Imaging. 2000;25:187-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 46] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 2. | Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 29-1995. A 65-year-old man with mediastinal Hodgkin’s disease and a pelvic mass. N Engl J Med. 1995;333:784-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 37] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Fleming CR, Dickson ER, Harrison EG. Splenosis: autotransplantation of splenic tissue. Am J Med. 1976;61:414-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 133] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 4. | Normand JP, Rioux M, Dumont M, Bouchard G, Letourneau L. Thoracic splenosis after blunt trauma: frequency and imaging findings. AJR Am J Roentgenol. 1993;161:739-741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 72] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Abu Hilal M, Harb A, Zeidan B, Steadman B, Primrose JN, Pearce NW. Hepatic splenosis mimicking HCC in a patient with hepatitis C liver cirrhosis and mildly raised alpha feto protein; the important role of explorative laparoscopy. World J Surg Oncol. 2009;7:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Rickert CH, Maasjosthusmann U, Probst-Cousin S, August C, Gullotta F. A unique case of cerebral spleen. Am J Surg Pathol. 1998;22:894-896. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 55] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Tsitouridis I, Michaelides M, Sotiriadis C, Arvaniti M. CT and MRI of intraperitoneal splenosis. Diagn Interv Radiol. 2010;16:145-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 8. | Dokal IS, Deenmamode M, Lewis SM. Detection and functional assessment of accessory splenic tissue (splenunculi) with radiolabelled heat damaged autologous erythrocytes. Clin Lab Haematol. 1990;12:387-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Froehner M, Leike S, Manseck A, Haase M, Wirth MP. Splenunculus mimicking late local recurrence of renal cell carcinoma. Scand J Urol Nephrol. 1998;32:418-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Basu S, Ray AK, Banerjee S. Splenunculus masquerading as colonic malignancy. Int Surg. 2003;88:181-183. [PubMed] |
| 11. | Foroudi F, Ahern V, Peduto A. Splenosis mimicking metastases from breast carcinoma. Clin Oncol (R Coll Radiol). 1999;11:190-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Liu Y, Ji B, Wang G, Wang Y. Abdominal multiple splenosis mimicking liver and colon tumors: a case report and review of the literature. Int J Med Sci. 2012;9:174-177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 13. | Li H, Snow-Lisy D, Klein EA. Hepatic splenosis diagnosed after inappropriate metastatic evaluation in patient with low-risk prostate cancer. Urology. 2012;79:e73-e74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |