Published online Mar 24, 2016. doi: 10.5410/wjcu.v5.i1.60
Peer-review started: September 10, 2015
First decision: October 27, 2015
Revised: February 10, 2016
Accepted: March 7, 2016
Article in press: March 9, 2016
Published online: March 24, 2016
Processing time: 190 Days and 14.9 Hours
AIM: To evaluate outcomes of robotic-assisted laparoscopic partial nephrectomy performed for posterior renal tumors via a transperitoneal or retroperitoneal approach.
METHODS: Retrospective review was performed for patients who underwent robotic-assisted laparoscopic partial nephrectomy (RALPN) for a posterior renal tumor between 2009-2015. Patient demographic characteristics, operative factors, pathology, oncologic outcomes, renal function, and tumor complexity were obtained. Radius of the tumor, exophytic/endophytic properties of the tumor, nearness of tumor to the collecting system, anterior/posterior position, location relative to the polar line (RENAL) nephrometry scores were calculated. nephrometry scores were calculated. The operative approach was determined by the primary surgeon.
RESULTS: A total of 91 patients were identified who underwent RALPN for a posterior renal tumor. Fifty-four procedures were performed via the retroperitoneal (RP) approach, and 37 via the transperitoneal (TP) approach. There were no significant differences in patient factors (race, sex, age and body mass index), RENAL nephrometry scores, tumor size, conversion rates, or margin status. Among procedures performed on-clamp, there was no significant difference in warm ischemia times. Total operative time (180.7 min for RP vs 227.8 min for TP, P < 0.001), robotic console time (126.9 min for RP vs 164.3 min for TP, P < 0.001), and median estimated blood loss (32.5 mL for RP vs 150 mL for TP, P < 0.001) were significantly lower via the RP approach. Off-clamp RALPN was performed for 31 (57.4%) of RP procedures vs 9 (24.3%) of TP procedures. Oncologic and renal functional outcomes were equivalent.
CONCLUSION: The RP approach to RALPN for posterior renal tumors is superior with regard to operative time and blood loss and the ability to be performed off-clamp.
Core tip: A retrospective review was completed to evaluate perioperative outcomes of robotic-assisted laparoscopic partial nephrectomy (RALPN) performed for posterior renal tumors performed via a transperitoneal or retroperitoneal (RP) approach. Ninety-one patients underwent RALPN for a posterior renal tumor. Fifty-four procedures were performed via the RP approach. Total operative time, robotic console time, and median estimated blood loss were significantly lower via the RP approach. Fifty-seven percent of RP procedures were performed off-clamp. The RP approach to RALPN for posterior renal tumors is superior with regard to operative time and blood loss and the ability to perform the procedure off-clamp.
- Citation: Wetterlin JJ, Blackwell RH, Capodice S, Kliethermes S, Quek ML, Gupta GN. Robotic-assisted laparoscopic partial nephrectomy: A comparison of approaches to the posterior renal mass. World J Clin Urol 2016; 5(1): 60-65
- URL: https://www.wjgnet.com/2219-2816/full/v5/i1/60.htm
- DOI: https://dx.doi.org/10.5410/wjcu.v5.i1.60
Robotic-assisted laparoscopic partial nephrectomy (RALPN) is increasingly utilized as an alternative to laparoscopic or open partial nephrectomy for surgical extirpation of renal masses. RALPN can be performed via a transperitoneal (TP) or retroperitoneal (RP) approach, but the majority of the literature describes the TP approach as it has been more widely adopted and provides a larger working space with more familiar anatomical landmarks[1]. The RP approach, however, has specific advantages including direct access to posterior and lateral tumors without whole kidney mobilization, direct access to the renal artery, and does not require bowel mobilization[1,2]. Additionally, several recent studies have indicated that the RP approach for RALPN is associated with decreased operative time, decreased length of hospital stay, decreased estimated blood loss (EBL), decreased warm ischemia time (WIT), decreased narcotic use, and permitted quicker return of bowel function with comparable oncologic outcomes[1-11].
While the current literature suggests the RP approach to RALPN provides an acceptable alternative to the TP approach, there are no studies that compare these two methods for posteriorly located tumors. The current study evaluates the use of RALPN for posterior renal tumors via the TP and RP approaches in regards to perioperative, renal functional, and oncological outcomes.
A retrospective review was performed in our prospectively-maintained RALPN institutional database to identify patients who underwent RALPN for a posteriorly-located renal tumor from September 2009 to January 2015. Tumor characteristics, including posterior location, were based on radius of the tumor, exophytic/endophytic properties of the tumor, nearness of tumor to the collecting system, anterior/posterior position, location relative to the polar line (RENAL) nephrometry scores. Information regarding patient demographic characteristics, operative factors, renal function, tumor histology, and oncological outcomes were obtained by chart review. Surgical approach was determined by the primary surgeon based on tumor location and characteristics.
The RP approach to RALPN has been previously described, and our technique had little variation[12]. In brief, patients were instructed to hold anticoagulation and antiplatelet agents prior to surgery. No bowel preparation was administered. Patients were placed in a full flank position over a beanbag, secured and appropriately padded, with the table flexed. The flank and abdomen were prepped and bony landmarks identified. An incision was made at the level of the tip of the 12th rib, one centimeter superior to the anterior superior iliac spine. Blunt dissection was then used to enter the retroperitoneum. A balloon trocar was placed to dilate the RP space, after which pneumoretroperitoneum was established. Under direct visualization, two 8 mm robotic ports and a single 12 mm assistant port were placed. The robot was docked over the ipsilateral shoulder at a 15 degree angle towards the spine. Arterial vascular dissection was immediately performed by elevating the kidney off the psoas muscle to identify the renal hilum. For RALPN performed with WIT, only the artery was clamped with bulldog clamps. Intraoperative ultrasound was used to correctly identify the tumor, Gerota’s fat overlying the tumor was removed and sent for pathological analysis, and the tumor was excised using sharp dissection. The decision to perform the procedure with or without clamping of the renal hilum was made by the primary surgeon. Renorrhaphy and placement of hemostatic agents was performed as deemed necessary.
Alternatively, patients undergoing the TP approach were placed in a modified flank position with the table maximally flexed to provide optimal exposure. Insufflation was obtained with the Veress needle. Ports were placed in the supraumbilical area, lateral to the rectus sheath, one 8 mm port superior in the midline, and one inferiorly in the midclavicular line. A 12 mm assistant port was placed inferiorly, and a 5 mm assistant port superiorly. For right-sided procedures, an additional 5 mm assistant port was occasionally placed along the contralateral margin for liver retraction. The robot was docked over the ipsilateral shoulder, after which the kidney and renal hilum were identified in a standard fashion. During the TP approach, the kidney required complete mobilized to facilitate visualization of the posterior tumor.
The patient characteristics that were evaluated included age at time of procedure, gender, race, and body mass index (BMI). Operative factors examined included length of total procedure, robotic console time, conversion to open, EBL and WIT. Renal function was evaluated by comparing preoperative creatinine to postoperative creatinine; postoperative creatinine was measured at an average of 4.5 (1.7-15.3) mo after surgery. Postoperative creatinine levels were routinely measured on postoperative day one, and daily throughout patient’s hospital stay. There was no standardization of postoperative creatinine measurement after patient discharge, and was performed on an individual basis. Tumor characteristics evaluated included RENAL nephrometry scores, tumor histology, size, laterality, and surgical margin status. Patients were followed postoperatively for radiographic evidence of tumor recurrence and or metastasis.
The RENAL nephrometry score is a scoring system to objectively describe anatomic characteristics of renal tumors including tumor radius, amount of tumor that is exophytic, nearness of deepest portion of the tumor to the collecting system or renal sinus, anterior or posterior location, and location relative to the polar line[13].
Standard statistical methods were used to describe characteristics of individuals in both groups. Continuous variables were primarily represented as means and standard deviations, whereas categorical variables were represented as frequencies and percentages. Univariable analyses were conducted to compare differences in patient characteristics, tumor characteristics and operative outcomes between the two groups. Independent t-tests were used for continuous variables and Pearson c2 or Fisher’s exact tests were used for categorical comparisons. Due to the non-normality of WIT and EBL, medians and interquartile ranges were presented and Wilcoxon rank sum tests used.
All procedures were performed by 5 surgeons at a single institution from September 2009 to January 2015. A total of 91 patients underwent RALPN for a posterior renal tumor. Fifty-four procedures were performed via the RP approach, and 37 via the TP approach. There were no significant differences in patient factors including race, sex, age, and BMI (Table 1). The only significant difference with regard to tumor characteristics was laterality of the tumor. A majority of patients with left-sided tumors underwent resection via the TP approach (59.5%), whereas a majority of patients with right-sided tumors were via the RP approach (63%, P = 0.04). There were no significant differences in tumor size or RENAL nephrometry scores, including individual components (Table 2).
| RP (n = 54) | TP (n = 37) | P | |
| Age at time of surgery, mean (SD) | 56.5 (13) | 57.2 (11.6) | 0.801 |
| BMI (SD) | 31.1 (5.8) | 32.1 (7.0) | 0.511 |
| Race | |||
| Asian | 1 (1.9%) | 0 | 0.452 |
| Black | 3 (5.6%) | 3 (8.1%) | |
| Hispanic | 7 (13.0%) | 2 (5.4%) | |
| Other | 0 | 1 (2.7%) | |
| White | 43 (79.6%) | 31 (83.8%) | |
| Sex | |||
| Female | 17 (31.5%) | 17 (46.0%) | 0.163 |
| Male | 37 (68.5%) | 20 (54.1%) | |
| Preoperative creatinine, mean (SD) | 0.95 (0.21) n = 53 | 0.90 (0.17) n = 36 | 0.271 |
| RP (n = 54) | TP (n = 37) | P | |
| Renal location | |||
| Left | 20 (37.0%) | 22 (59.5%) | 0.043 |
| Right | 34 (63.0%) | 15 (40.5%) | |
| Pathologic tumor size (cm), mean (SD) | 3.1 (1.6) n = 53 | 2.9 (1.2) n = 36 | 0.541 |
| Surgical margin | |||
| Negative | 50 (98.0%) | 32 (91.4%) | 0.302 |
| Positive | 1 (2.0%) | 3 (8.6%) | |
| RENAL score, mean (SD) | 6.5 (1.9) | 6.6 (1.8) | 0.711 |
| Radius | |||
| 1 | 42 (77.8%) | 33 (89.2%) | 0.412 |
| 2 | 10 (18.5%) | 4 (10.8%) | |
| 3 | 2 (3.7%) | 0 | |
| Exophytic | |||
| 1 | 29 (53.7%) | 15 (40.5%) | 0.412 |
| 2 | 20 (37.0%) | 19 (51.4%) | |
| 3 | 5 (9.3%) | 3 (8.1%) | |
| Nearness | |||
| 1 | 23 (42.6%) | 15 (40.5%) | 0.943 |
| 2 | 8 (14.8%) | 5 (13.5%) | |
| 3 | 23 (42.6%) | 17 (46.0%) | |
| Location relative to polar line | |||
| 1 | 30 (55.6%) | 19 (51.4%) | 0.513 |
| 2 | 12 (22.2%) | 6 (16.2%) | |
| 3 | 12 (22.2%) | 12 (32.4%) |
Off-clamp RALPN was performed for 57.4% of RP procedures vs 24.3% of TP procedures. Among procedures performed on-clamp, there was no significant difference in warm ischemia times. There were no significant differences in conversion rates or surgical margin status between the two groups. One patient in the RP group had a positive surgical margin vs three in the TP group. Total operative time (180.7 min for RP vs 227.8 min for TP, P < 0.001), robotic console time (126.9 min for RP vs 164.3 min for TP, P < 0.001), and median EBL (32.5 mL for RP vs 150 mL for TP, P < 0.001) were significantly lower via the RP approach (Table 3). There was no significant difference in postoperative renal function between both groups, measured at an average of 4.5 (1.7-15.3) mo postoperatively (Table 4).
| RP (n = 54) | TP (n = 37) | P | |
| Total operative time (SD) | 180.7 (62.3) | 227.8 (59.0) | < 0.0011 |
| Robot console time, mean (SD) | 126.9 (40.0) | 164.3 (51.3) | < 0.0011 |
| WIT, median (IQR)4 | 28.0 (20-31) | 27.0 (21-31) | 0.963 |
| n = 23 | n = 28 | ||
| Conversion | |||
| No | 52 (96.3%) | 32 (86.5%) | 0.122 |
| Yes | 2 (3.7%) | 5 (13.5%) | |
| EBL, median (IQR) | 32.5 (20-100) | 150.0 (50-250) | < 0.0013 |
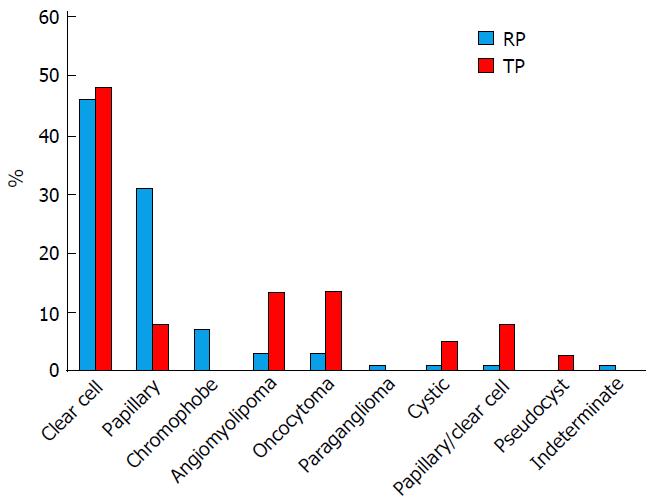
Patients in both groups were followed postoperatively for evidence of radiographic recurrence or metastasis. No patients in either group had evidence of disease recurrence or metastasis after median follow-up of 187 d for the TP group, 104 d for the RP group. Tumor histology was assessed in all patients that underwent RALPN, with the majority of patients in both groups being diagnosed with clear cell renal cell carcinoma (Figure 1).
Minimally invasive techniques and nephron sparing surgery for the management of renal masses are increasingly utilized and have comparable oncologic outcomes to the open approach. Partial nephrectomy remains the standard of care for small renal masses in appropriately selected patients according to current guidelines[14]. Minimally invasive techniques have demonstrated the added advantage of faster postoperative convalescence and shorter hospital stay[7]. In comparison to the TP approach, the RP approach has been less commonly used, even for posteriorly located tumors. This may be attributed to less operative familiarity, a smaller working space, and less familiarity with surgical landmarks[7]. Despite these obstacles, an increasing amount of data supports the use of the RP approach for RALPN. To our knowledge, no prior studies have examined the use of the RP vs TP approach exclusively for posterior renal tumors.
RENAL nephrometry score has been widely used to objectively describe anatomic characteristics of renal tumors including tumor radius, amount of tumor that is exophytic, nearness of the tumor to the collecting system or renal sinus, anterior or posterior location, and location relative to the polar line[13]. Prior studies have evaluated the impact of RENAL nephrometry scores on outcomes of partial nephrectomy and have demonstrated that higher nephrometry scores were associated with more EBL, and longer hospital stay and warm ischemia times[10,13]. Ellison et al[10] found that the nearness of the tumor to the renal sinus had the greatest impact on perioperative outcomes. Hayn et al[13] found that nephrometry score did not impact overall operative times, transfusion rate, complication rate, or pre- and post-operative creatinine clearance. Similarly, our study demonstrated no significant difference in outcomes between RP vs TP approaches with regard to RENAL nephrometry score. In our study, the nephrometry score was only useful to classify the tumor as anterior or posterior.
In a study comparing perioperative outcomes of all renal tumors regardless of anterior or posterior location that underwent RALPN via TP or RP approach, Gin et al[7] found that after adjusting for tumor complexity that less complex tumors based on RENAL nephrometry score were more likely to undergo RP RALPN. They demonstrated that more patients (69%) with posterior renal tumors underwent excision via the RP approach, and this was associated with lower EBL and lower rates of readmission[7].
Further, benefits to the RP approach have been shown with regard to multiple perioperative factors including operative time, EBL, length of hospital stay, and return of bowel function[3,9,15]. A meta-analysis by Ren et al[5], including eight retrospective studies evaluating the use of TP vs RP laparoscopic partial nephrectomy found that RP partial nephrectomy was associated with shorter operative times, lower EBL, and a shorter hospital stay. A similar meta-analysis by Fan et al[2], comparing TP vs RP laparoscopic and robotic partial nephrectomy demonstrated that the RP approach was associated with shorter time to renal hilum control, shorter operative time, shorter length of hospital stay, and a lower overall complication rate.
The RP approach eliminates the need for bowel mobilization thus limiting the potential for injury to abdominal organs and the development of intra-abdominal adhesions and intestinal obstruction[16]. The literature supports the fact that lack of bowel mobilization and faster access to the renal hilum contributes to the shorter operative times and results in earlier return of bowel function postoperatively[9,15]. We also believe that lack of total renal mobilization to access the posterior surface of the kidney contributes to shorter operative times and a lower EBL.
The ability to perform more procedures off-clamp via the RP approach was likely due to the simplicity and speed at which the renal hilum could be identified, thereby also allowing for easy identification of the renal hilum to place a bulldog clamp if necessary during tumor excision. Conversion to an open procedure was performed more commonly during the TP approach at 13.5% vs 3.7% in via the RP group. Although not statistically significant, this is likely due to the ease at which the renal hilum can be accessed and lack of bowel mobilization required for the RP approach. Regarding the differences in laterality of tumors, specifically that a majority of patients with left-sided tumors underwent resection via the TP approach (59.5%), whereas a majority of patients with right-sided tumors were via the RP approach (63%, P = 0.04), remains unclear. This difference is possibly due to anatomical reasons, such that there is no need for liver retraction and placement of an additional port for RALPN for right-sided tumors when performed via the RP approach.
Most patients were discharged on postoperative day one or two after RP or TP RALPN, and therefore length of hospital stay was not evaluated in our study.
Partial nephrectomy remains the standard of care for small renal masses in appropriately selected patients[14]. The RP approach to RALPN has proven an effective approach for posterior renal masses with acceptable oncologic and morbidity outcomes, including preservation of postoperative renal function[6]. In our study, more RP procedures were performed off-clamp. Despite the fact that there was no significant difference in postoperative renal function, we believe in the importance of performing RALPN off-clamp if it is deemed safe and possible, in an attempt to maximally preserve renal function.
The oncological outcomes after RP partial nephrectomy have proven similar to those of competing approaches including rate of recurrence and positive margins. The literature demonstrates positive margin rates of 0%-5.6% for RP RALPN, and recurrence rates of 1.5%-6%. Of note, positive margin rates for open partial nephrectomy and laparoscopic RP partial nephrectomy are similar at 1.3%-1.5% and 2%-7.1%, respectively[6]. Our incidence of positive margins was lower via the RP approach (2%) when compared to the TP approach (8.6%), however this was not statistically significant. We believe that it is important to note the dramatic difference, which may be due to better tumor visualization during excision via the RP approach. Our recurrence rate was low for both approaches, with only one recurrence in the RP group.
Our results support existing literature demonstrating the superiority of the RP approach to RALPN with regard to operative time, blood loss, preservation of renal function, and oncologic outcomes[2,5]. The current study, however, was the first to evaluate outcomes of RP RALPN exclusively for posterior renal masses. With an increasing body of data to support its use, increased familiarity with the RP approach to RALPN may lead to widespread adaptation of this technique, particularly for posterior renal tumors.
The limitations of our study include the retrospective design and lack of randomization. A selection bias likely existed as the surgical approach was determined by the primary surgeon based on the tumor location and characteristics. Patients with posterior renal tumors were more likely to be selected to undergo the RP approach to RALPN. Despite this, however, the findings of decreased total operative time, robotic console time, and EBL remain significant. A prospective, randomized trial is necessary to remedy this selection bias. Randomization should include both right- and left-sided posterior renal tumors performed via the RP and TP approaches. Another limitation includes the short follow-up interval for assessment of postoperative renal function, which was measured at an average of only 4.5 mo. Long-term assessment of oncological outcomes is needed, as our study included radiographic follow-up at an average of less than 1 year postoperatively.
In conclusion, the TP and RP approach to RALPN are feasible approaches for posterior renal masses. The RP approach to RALPN, however, is superior with regard to operative time and blood loss when compared to the more familiar TP approach.
Robotic-assisted laparoscopic partial nephrectomy (RALPN) is increasingly utilized as an alternative to laparoscopic or open partial nephrectomy for surgical extirpation of renal masses, and can be performed via a transperitoneal (TP) or retroperitoneal (RP) approach. The majority of the literature describes the TP approach as it has been more widely adopted, however the RP approach has been shown to have specific advantages. No study has evaluated the use of the RP approach to RALPN specifically for posteriorly located renal tumors.
The literature suggests that the RP approach to RALPN is an acceptable alternative to the TP approach, however no studies have compared these methods specifically for posteriorly located tumors. The current study evaluates the use of RALPN for posterior renal tumors via the TP and RP approaches in regards to perioperative, renal functional, and oncological outcomes.
The RP approach to RALPN has been proven to have specific advantages over the TP approach including direct access to posterior and lateral tumors without whole kidney mobilization, direct access to the renal artery, and lack of need for bowel mobilization. This study was the first study to examine the use of the RP approach to RALPN specifically for posteriorly located renal tumors. The authors concluded that the RP approach to RALPN for posterior renal tumors is associated with decreased total operative time, robotic console time, and estimated blood loss, and is more likely to be performed off-clamp when compared to the TP approach.
This study suggests that the RP approach to RALPN is a safe alternative to the more familiar TP approach for surgical extirpation of posterior renal tumors, and is associated with decreased total operative time, robotic console time, and estimated blood loss. The RP approach to RALPN is also more likely to be performed off-clamp, and is associated with similar oncological outcomes and postoperative renal function. The authors’ findings support the use of the RP approach to RALPN for posteriorly located renal tumors.
The RENAL nephrometry score is a scoring system to objectively describe anatomic characteristics of renal tumors including tumor radius, amount of tumor that is exophytic, nearness of deepest portion of the tumor to the collecting system or renal sinus, anterior or posterior location, and location relative to the polar line.
The study is interesting.
P- Reviewer: Stavroulopoulos A, Taheri S S- Editor: Gong XM L- Editor: A E- Editor: Li D
| 1. | Choo SH, Lee SY, Sung HH, Jeon HG, Jeong BC, Jeon SS, Lee HM, Choi HY, Seo SI. Transperitoneal versus retroperitoneal robotic partial nephrectomy: matched-pair comparisons by nephrometry scores. World J Urol. 2014;32:1523-1529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 47] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 2. | Fan X, Xu K, Lin T, Liu H, Yin Z, Dong W, Huang H, Huang J. Comparison of transperitoneal and retroperitoneal laparoscopic nephrectomy for renal cell carcinoma: a systematic review and meta-analysis. BJU Int. 2013;111:611-621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 86] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 3. | Marszalek M, Chromecki T, Al-Ali BM, Meixl H, Madersbacher S, Jeschke K, Pummer K, Zigeuner R. Laparoscopic partial nephrectomy: a matched-pair comparison of the transperitoneal versus the retroperitoneal approach. Urology. 2011;77:109-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 4. | Benway BM, Bhayani SB, Rogers CG, Dulabon LM, Patel MN, Lipkin M, Wang AJ, Stifelman MD. Robot assisted partial nephrectomy versus laparoscopic partial nephrectomy for renal tumors: a multi-institutional analysis of perioperative outcomes. J Urol. 2009;182:866-872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 374] [Cited by in RCA: 355] [Article Influence: 22.2] [Reference Citation Analysis (0)] |
| 5. | Ren T, Liu Y, Zhao X, Ni S, Zhang C, Guo C, Ren M. Transperitoneal approach versus retroperitoneal approach: a meta-analysis of laparoscopic partial nephrectomy for renal cell carcinoma. PLoS One. 2014;9:e91978. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 6. | Hu JC, Treat E, Filson CP, McLaren I, Xiong S, Stepanian S, Hafez KS, Weizer AZ, Porter J. Technique and outcomes of robot-assisted retroperitoneoscopic partial nephrectomy: a multicenter study. Eur Urol. 2014;66:542-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 50] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 7. | Gin GE, Maschino AC, Spaliviero M, Vertosick EA, Bernstein ML, Coleman JA. Comparison of perioperative outcomes of retroperitoneal and transperitoneal minimally invasive partial nephrectomy after adjusting for tumor complexity. Urology. 2014;84:1355-1360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 8. | Patel M, Porter J. Robotic retroperitoneal partial nephrectomy. World J Urol. 2013;31:1377-1382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Ng CS, Gill IS, Ramani AP, Steinberg AP, Spaliviero M, Abreu SC, Kaouk JH, Desai MM. Transperitoneal versus retroperitoneal laparoscopic partial nephrectomy: patient selection and perioperative outcomes. J Urol. 2005;174:846-849. [PubMed] |
| 10. | Ellison JS, Montgomery JS, Hafez KS, Miller DC, He C, Wolf JS, Weizer AZ. Association of RENAL nephrometry score with outcomes of minimally invasive partial nephrectomy. Int J Urol. 2013;20:564-570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 51] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 11. | Patel M, Porter J. Robotic retroperitoneal surgery: a contemporary review. Curr Opin Urol. 2013;23:51-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Ghani KR, Porter J, Menon M, Rogers C. Robotic retroperitoneal partial nephrectomy: a step-by-step guide. BJU Int. 2014;114:311-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 13. | Hayn MH, Schwaab T, Underwood W, Kim HL. RENAL nephrometry score predicts surgical outcomes of laparoscopic partial nephrectomy. BJU Int. 2011;108:876-881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 43] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 14. | Novick AC, Campbell SC, Belldegrun A, Blute ML, Chow GK, Derweesh IH, Kaouk JH, Leveillee RJ, Matin SF, Russo P. Guideline for Management of the Clinical Stage 1 Renal Mass. American Urological Association Education and Research, Inc. 2009;1-76. |
| 15. | Wright JL, Porter JR. Laparoscopic partial nephrectomy: comparison of transperitoneal and retroperitoneal approaches. J Urol. 2005;174:841-845. [PubMed] |
| 16. | Garg M, Singh V, Sinha RJ, Sharma P. Prospective randomized comparison of transperitoneal vs retroperitoneal laparoscopic simple nephrectomy. Urology. 2014;84:335-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |