Published online Jul 24, 2014. doi: 10.5410/wjcu.v3.i2.127
Revised: March 4, 2014
Accepted: May 8, 2014
Published online: July 24, 2014
Processing time: 213 Days and 21.9 Hours
AIM: To compare a modified technique preserving brain circulation during cardiopulmonary by-pass (CPB) for radical nephrectomy and caval thrombectomy, to the standard technique.
METHODS: Retrospective evaluation of an institutional database that collects the data of patients submitted to nephrectomy and removal of caval thrombosis with CPB since 1998. In period between 1998 and 2007, CPB followed a standard technique (group sCPB); then, since 2008, a variation in the perfusional technique was introduced, allowing the anterograde perfusion of brain circulation during circulatory arrest (group CPB + BP) with the aim to reduce the risk of ischemic damage to the brain and also the need of deeper hypothermia. Patients (age, gender, comorbidity) and tumor characteristics (side, histology, staging, level of thrombosis), as well as parameters of CPB (times of CPB, aortic clamping and circulatory arrest, minimum temperature reached during hypothermia), intra- and perioperative morbidity (complications in general, bleeding, renal and hepatic failure) and mortality were analyzed and compared between 2 groups (sCPB vs CPB + BP)
RESULTS: The data of 24 patients, respectively 9 in sCPB group and 15 in CPB + BP group, have been reviewed. No differences in the characteristics of patients and tumors were observed. Only 1 (11.1%) and 4 (26.0%) of sCPB and CPB + BP patients, respectively, didn’t experience any event of complication. In sCPB group were observed 15 events of complication (5 of which Clavien ≥ 3, 33% of the events), for a mean of 1.66 events/patient; 29 events (10 Clavien ≥ 3, 30.3%), in the CPB + BP group, for a mean of 2.1 events/patient. 1 (11.1%) and 2 (14.2%) deaths occurred, respectively. For patients submitted to CPB + BP, the minimum temperature reached was significantly higher (29.9 °C vs 26.4 °C, P = 0.001), the time of circulatory arrest was longer (17.4 min vs 13.7 min, NS), but the overall time of CPB shorter (76.1 min vs 92.5 min, NS), albeit these latter differences were not statistically significant. No differences in terms of bleeding, impairment of renal function (post-operative Cr > 2.0 mg/dL respectively in 44.4% vs 35.7% of cases, in the two groups, NS) or hepatic insufficiency (post-operative GOT or GPT > 50 U/L respectively in 44.4% and 66.7% of patients, NS) were noted. Average follow-up was 51 mo in patients undergoing a sCPB and 12 mo in the CPB + BP group of patients; at the last follow-up, 7 patients had died of progression of the condition (4 in the first group and 3 in the second group, respectively), 7 were alive in progression and 10 had no evidence of the disease.
CONCLUSION: The perfusional technique that maintains brain perfusion during circulatory arrest limits hypothermia and lowers time of CPB, without rising the risk of renal and hepatic injury.
Core tip: Surgery for renal cell carcinoma with caval thrombosis extended to the diaphragm or right atrium is burdened by a high risk of complications. The adoption of a modified technique of cardiopulmonary by-pass that maintans the perfusion of brain circulation, doesn’t add morbidity to the procedure and can be in principle of benefit, since it shortens the duration of surgery and requires a less deep hypothermia.
- Citation: Antonelli A, Bisleri G, Mittino I, Moggi A, Muneretto C, Cunico SC, Simeone C. Cardiopulmonary bypass with brain perfusion for renal cell carcinoma with caval thrombosis. World J Clin Urol 2014; 3(2): 127-133
- URL: https://www.wjgnet.com/2219-2816/full/v3/i2/127.htm
- DOI: https://dx.doi.org/10.5410/wjcu.v3.i2.127
Renal carcinoma (RCC) is extremely angiotropic and may extend into the venous circulation, from the renal vein to the right sections of the heart[1]. Lacking an effective medical treatment, surgery is still the only available treatment, leading to 5-year cancer-specific survival rates of up to 70%[2,3].
When the thrombosis reaches the diaphragm, the surgical treatment requires a combination of abdominal and thoracic approaches in order to achieve an extensive removal of the thrombus within the inferior vena cava and the right atrium by means of cardiopulmonary bypass (CPB) and circulatory arrest. Even if other strategies have been also suggested to avoid circulatory arrest or even CPB (i.e., CPB under mild hypothermia without cardiac arrest, veno-venous by-pass by means of cavo-atrial shunt and “milking” manoeuvre below the major hepatic veins without CPB[4]), CBP with circulatory arrest is probably the most widely accepted surgical strategy for these patients.
This procedure itself is burdened by a high risk of bleeding, which is in part due to the need of blood heparinization during the exanguination of the patient, but also to the coagulation disorders caused by deep hypothermia, used in order to minimise the potential parenchymal damage (in particular to the brain) caused by the circulatory arrest.
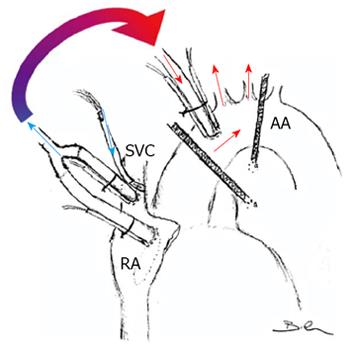
In an attempt to further improve patients’ clinical outcomes, at our institution since 2007 a novel CPB technique has been adopted which allows for antegrade cerebral perfusion during circulatory arrest in mild hypothermia. The purpose of this study was therefore to review the results achieved by means of this novel technique (cardiopulmonary bypass with cerebral perfusion-CPB + BP, Figure 1) and compare it with the conventional technique (standard cardiopulmonary bypass without cerebral perfusion-sCPB), with respect to intra- and post-operative outcomes.
This study included all patients undergoing a procedure including nephrectomy and removal of thrombosis with CPB at our Institution since 1998, because since that year a specific database to store all the surgical data of these patients was generated.
The indication for the removal of thrombosis with the aid of CPB was done for all those cases in which the preoperative assessments revealed that the upper level of thrombosis reached the right atrium or above. All the patients were studied by electronic computer X-ray tomography technique (CT), magnetic resnane iamge (MRI), trans-esophageal echocardiography and coronarography, in order to evaluate the extent and features of the thrombosis as well to rule out any potential concomitant heart disease.
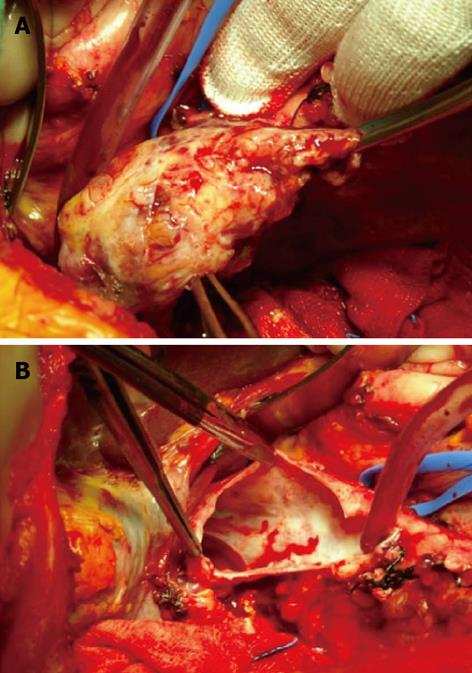
The surgical approach implies a bilateral subcostal incision and a median sternotomy, separated by a short skin bridge, with the aim to improve the healing of the sternal incision by keeping it separate from the abdominal one. Once the abdominal vena cava and aorta have been isolated and the renal artery ligated, the kidney is mobilised while preserving only the renal vein; once the CPB has been instituted, before the cavotomy, the inferior vena cava caudal to the thrombosis and the contralateral renal vein are clamped with tourniquets. Then, once mild hypothermia is achieved, cardioplegia solution is delivered and the general circulation is arrested; finally, the right atrium and the lower abdominal vena cava are opened in order to remove the thrombosis and to complete the nephrectomy.
From 1998 to 2007, CPB has been carried out using a standard central cannulation technique, achieving moderate hypothermia (25 °C) during circulatory arrest (sCPB group).
Instead, since 2007 to date, a variation of such technique has been adopted (CPB + BP group), to maintain cerebral perfusion so that mild hypothermia was sufficient during the circulatory arrest. As we previously described[5], once the pericardium is opened, the aortic arch is prepared as to allow exposure of the supra-aortic vessels; the ascending aorta is cannulated, as well as the right atrium and the superior vena cava. Once moderate-mild hypothermia has been reached (30 °C), the aorta is clamped and a cardioplegic solution is administered; then, an additional clamp is positioned on the aortic arch between the left common carotid artery and the left subclavian artery. Following opening of the right atrium, venous drainage is obtained exclusively via the cannula previously inserted into the superior vena cava: therefore, cerebral perfusion is maintained through the aortic arch while the patient is on systemic circulatory arrest, allowing for a bloodless field both on the cardiac and abdominal sides.
In the present study, the level reached by the thrombosis was classified according to the Mayo Clinic system[6]; co-morbidities were scored according to the Charlson-Romano score[7]; post-operative complications were recorded up to 30 d after surgery according to the Clavien-Dindo system[8].
Discrete variables were analysed by Fisher exact test or χ2 test, while Mann-Whitney test was utilised for continuous variables (SPSS v.13, SPSS Inc, Chicago, IL, United States).
During the period of the study (1998-2013), 1477 patients underwent surgery for renal cancer at our Institution. Overall, 23 patients with venous thrombosis underwent surgery with the aid of CPB, 9 with sCPB, 15 with a CPB + BP technique.
The two groups had comparable characteristics, as listed in Table 1. Even in all the patients at the preoperative evaluation the head of the thrombosis was deemed as inside of the right atrium, in 12 patients at surgical exploration, it was close but outside the atrium, so that they have been down-classified as level 3, again in a similar rate in the two groups.
| Patients and tumors characteristics | sCPB | CPB+BP | P |
| Age (yr) | 64.0 ± 9.2 | 66.2 ± 10.2 | NS |
| Gender | |||
| Males | 7/9 (77.8%) | 9/15 (60%) | NS |
| Females | 2/9 (22.2%) | 6/15 (40%) | |
| Pre-operative ejection fraction | 59.7% ± 0.8% | 57.6% ± 4.6% | NS |
| Comorbidity | |||
| Charlson score 0 | 2/9 (22.2%) | 6/15 (40%) | NS |
| Charlson score ≥ 1 | 7/9 (77.8%) | 9/15 (60%) | |
| Tumor side | |||
| Right | 7/9 (77.8%) | 10/15 (66.7%) | NS |
| Left | 2/9 (22.2%) | 5/15 (33.3%) | |
| Tumor diameter (cm) | 9.6 ± 2.5 | 9.6 ± 2.9 | NS |
| Level of thrombosis | |||
| 3 | 5/9 (56.6%) | 8/15 (53.3%) | NS |
| 4 | 4/9 (44.4%) | 7/15 (46.6%) | |
| Histology | |||
| Clear Cell renal carcinoma | 7/9 (77.8%) | 13/15 (86.6%) | NS |
| Other | 2/9 (22.2%) | 2/15 (13.3%) | |
| Infiltration of perirenal tissues | 7 (77.8%) | 10 (66.7%) | NS |
| Infiltration of venous wall | 3 (33.3%) | 4 (26.6%) | NS |
| N+ | 1 (11.1%) | 2 (13.3%) | NS |
| M+ | 2 (22.2%) | 5 (33.3%) | NS |
Only 1 (11.1%) and 4 (26.0%) patients in the sCPB and in the CPB+BP group, respectively, did not experienced any postoperative complications; 15 complications (5 of which were grade ≥ 3, equal to 33% of the events) happened in the sCPB group, which means on average 1.66 events per patient; 29 complications (10 of which were grade ≥ 3, equal to 30.3% of the events) in the CPB + BP group, which means on average 2.1 events per patient (Table 2).
| Clavien grade | sCPB | CPB + BP |
| 1 | 4 acute renal failures | 5 acute renal failures |
| 2 | 3 transfusions | 7 transfusions |
| 3 atrial fibrillations | 7 atrial fibrillations | |
| 3a | 1 sternal wound dehiscence | |
| 3b | 1 bleeding requiring re-laparotomy | 1 bleeding requiring re-laparotomy |
| 1 ligature of the contralateral ureter, requiring ureteral stenting | ||
| 4a | 2 = respiratory failures | 1 brain stroke |
| 1 pulmonary embolism | ||
| 3 respiratory failures | ||
| 4b | - | 1 multi-organ failure |
| 5 | 1 (1st post-operative day) | 2 (3rd and 25th post-operative day) |
Table 3 summarizes the comparison of CPB parameters and indicators of morbidity. For the patients of the CPB+BP group was noted a significantly less deep hypothermia and, even without statistical significance, a prolonged time of circulatory arrest (CPB + BP 17.4 min vs sCPB 13.7 min), but a shorter overall CPB time (CPB + BP 76.1 min vs sCPB 92.5 min) due to the faster cooling and rewarming of the patient. Finally, no differences in terms of indicators of hepatic, renal, brain and coagulative impairment were noted, with a shorter overall length of stay for the CPB + BP group.
| Intra- and post-operative variables | sCPB | CPB+BP | P |
| CPB time (min) | 92.5 ± 35.7 | 76.1 ± 18.5 | NS |
| Aortic Clamp time (min) | 30.8 ± 15.8 | 26.5 ± 19.6 | NS |
| Circulatory arrest time (min) | 13.7 ± 8.9 | 17.4 ± 5.3 | NS |
| Minimum temperature (°C) | 26.4 ± 2.5 | 29.9 ± 1.9 | 0.001 |
| Intraoperative blood units transfused (no.) | 12 (4-12) | 13.2 (6-20) | NS |
| ICU stay (in days) | 2 (2-2) | 2.7 (1-3) | NS |
| Hospital stay (in days) | 27 (22-57) | 21 (10-25) | NS |
| Post-operative Cr > 2 mg/dL | 4/9 (44.4%) | 5/15 (33.3%) | NS |
| Post-operative GOT or GPT > 50 U/L | 4/9 (44.4%) | 8/15 (53.3%) | NS |
| Post-operative bleeding | 5/9 (55.6%) | 8/15 (53.3%) | NS |
| Peri-operative mortality | 1/11 (11.1%) | 2/15 (13.3%) | NS |
Average follow-up was 51 mo in patients undergoing a sCPB and 12 mo in the CPB + BP group of patients; at the last follow-up, 7 patients had died of progression of the condition (4 in the first group and 3 in the second group, respectively), 7 were alive in progression and 10 had no evidence of the disease.
Renal cancer is extremely angiotropic, which may result in a macroscopic invasion of the large venous vessels in up to 10% of cases[9]. While a regression with targeted therapies has been occasionally reported[10,11], only radical surgery can effectively treat patients albeit with variable 5-year survival rates, ranging between 34% and 72%[2,3]: such outcomes may be influenced mostly by unfavourable prognostic factors which are frequently associated with the occurrence of neoplastic thrombosis rather than the cranial extension of the thrombosis itself[12].
Surgery of caval thrombosis is technically complex and has high morbidity and mortality rates, up to 22% in a recent series[11].
In patients in which the thrombosis has extended over the diaphragm, the use of a CPB with circulatory arrest has been widely utilised in order to allow for a better control of the cranial end of the thrombosis through an atriotomy as well as to achieve a bloodless surgical field once the inferior vena cava has been opened (Figures 2, 3). To reduce the metabolic requirements of the tissues and thus increase the resistance to ischemic damage during the circulatory arrest, deep hypothermia (< 20 °C) has been routinely used[13]. In particular, the brain yields an higher risk of ischemic damage and its metabolism during circulatory arrest must be therefore significantly reduced by means of hypothermia, with an ischemic tolerance lasting up to 5 min at 37 °C, 15 min at 25 °C, 24 min at 20 °C, and 45 min at 10 °C[14-17].
There is a high risk of bleeding during CPB, which is related to the heparin infused when blood is diverted into the reservoir and the patient is exanguinated, and then antagonised by protamin when the physiologic circulation is restored, but also to hypothermia itself that could impair the platelet function and the production of coagulation factors.
The evidence that hypothermia may exert a negative impact is debated and recent publications, on the contrary, advocate its adoption on the basis of a better clinical outcome[18,19]. At the same time a diffuse concern exists, since several authors suggested alternative techniques to avoid the circulatory arrest[20,21], rather accepting a higher risk of a bloody surgical field, embolisms and tears to the caval wall due to the lack of a direct control over the cranial end of the thrombosis[22].
CPB with antegrade cerebral perfusion has been widely utilised for the surgery of the aortic arch[23], and it has also been reported in the treatment of thrombosis from renal carcinoma by our and other groups[5,24]. By the antegrade perfusion of the brain, hypothermia can be limited, thus reducing the theoretical risk of hypothermia-induced coagulation failure as well as the sure waste of time required to cool down and warm up the patient, but still providing the same bloodless operative field offered by a conventional deep hypothermic circulatory arrest.
The present study reviews the experience of a single academic institution with 23 consecutive patients treated in the last 15 years, using a CPB for caval thrombosis over the level of diaphragm. The number of patients, limited in absolute terms, is comparable to the main reports that have been published so far; in addition, for the present study the data collection has been planned for the specific purpose of estimating the morbidity of the procedure.
It has been confirmed that extensive caval thrombosis is associated with other unfavourable pathologic prognostic factors (invasion of peri-renal tissues, lymphnodes and distant metastasis), which may account for the poor prognosis[1,5,11]: in this study, the 5-year cancer-specific survival rate was 35%, but reached 62% in patients without lymphnodes or distant metastasis, thus confirming that in such cases surgery may promote a prolonged survival.
In the 9 cases treated in the first period of this study (sCPB), patients were cooled down to an average temperature of approximately 26 °C during the circulatory arrest, while in the 15 cases treated in the second period (CBP + BP), changing the technique of perfusion resulted in a remarkably lesser hypothermia, with an average minimum temperature of approximately 30 °C. Such level of hypothermia was maintained for a more prolonged time of circulatory arrest (CPB + BP 17.4 min vs sCPB 13.7 min), but within a shorter overall CPB time (CPB + BP 76.1 min vs sCPB 92.5 min) due to the less time needed to cool and rewarm the patient.
No differences were found between the two groups in terms of pre-operative co-morbidity or characteristics of tumors. Post-operative complications, systematically recorded, were very frequent, with at least one event in 83% of cases and a 30-d perioperative mortality rate of 12.5%, as shown in Table 3. The number of events of complications and the rate of major complications were similar between the 2 groups, as the mortality rate. However the length of stay was slightly shorter in CPB + BP group, suggesting a less detrimental effect in these patients from the events of complication. More interestingly, the number of renal and liver failure events turned out to be comparable, confirming that these parenchyma may tolerate temperatures above 20 °C-25 °C, at least for the time of circulatory arrest that such kind of surgery requires. At the same time, from our results nor advantages neither disadvantages in terms of bleeding or neurologic sequelae cannot be proved, as the only neurologic event happened just in the CPB + BP group.
So, the present study shows that the CPB + BP technique is not inferior to a standard CPB in terms of radicality of surgery and overall complications, while gives an advangtage in terms of duration of surgery. Surely, these conclusions should be taken with caution, because the study suffers from some limitations. First, the retrospective design, in spite of the perspective manner in which data has been collected: even if it is reasonable that the maintenance of cerebral circulation could add an advantage on neurological functions, the study fails to offer sure evidences of this, lacking of an established indicator that could measure cerebral metabolism prior, during and after the intervention. Second, the limited number of patients, enrolled in a long timeframe, that lowered the validity of statistical comparisons between groups; however, RCC with caval thrombosis treated with CPB is a rare condition, so that a perspective study probably will never be designed, even with a multicentric data collection, since different institutions usually adopt a personal approach.
The variation of the technique of perfusion proposed limits the need for hypothermia to moderate levels (30 °C), with the theoretical benefits on coagulation function and a sure advantages in terms of duration of surgery, without affecting the radicality of surgery or provoking a higher number of sequelae than a CPB with deeper hypothermia.
Surgery is the only option to cure some of the patients affected by a renal cancer that involves the inferior vena cava, However, this surgery suffers from high risks of intra and postoperative morbidity, which mainly depend on the cranial extension of the thrombus. Indeed, morbidity is higher for thrombosis extended up to the retroepatic vena cava or the right atrium, since in such conditions cardiopulmonary by-pass (CPB).
The exsanguination by CPB is required to extract of caval thrombosis extended up to the diaphragm or above in a bloodless field after the vena cava and/or the atrium are opened. To permit CPB, deep hypothermia is required, so that the organs - and in particular the brain - will suffer in a less extent from ischemia. Hypothermia can provoke an impairment of coagulation and prolongs the duration of the operation, worsening the morbidity of the procedure. Many authors investigated means alternative to CPB to reduce the morbidity of surgery in renal cancer with extended thrombosis. These procedures avoid at all the CPB, adopting an exclusive abdominal approach, by the complete mobilization of the liver and the exposition of the retrohepatic vena cava, or by a veno-venous bypass that diverts the venous flow from the vena cava but maintaining the cardiac activity and the arterial perfusion. There are, however, risks of incomplete radicality, if the thrombosis infiltrates a portion of the caval wall out which is not visible from the abdominal access, of embolism due to the detachment of part of the thrombus without the upper control through atriotomy, and of bleeding, related to the backflow from the lumbar veins.
The CPB with brain perfusion (CPB + BP) is a technique developed by cardiac surgeons with the intent to preserve cerebral perfusion during aortic arch replacement, showing a lower morbidity in respect to a standard CPB, in principle related to the less deep hypothermia required and to the maintenance of cerebral perfusion. At authors’ institution this technique has been applied to the surgery of renal cancer with extended venous thrombosis. At now only a very few cases have been reported, while this study reported a larger number of patients, comparing the results with an homogeneous historical group in which a standard CPB was adopted
The tecnhique can be suggested to the institutions actually treating these patients by a standard CPB, since the authors showed a non-inferiority of this modified technique in terms of renal and hepatic impairment, as of morbidity in general, with a less deep hypothermia and shorter operative times. The study can be the basis for future studies to investigate the impact on cerebral metabolism of this technique.
Cardiopulmonary by-pass: a procedure to convey blood from normal circulation to a machine that oxygenates blood.
The article is a well-written manuscript comparing two techniques of cardiopulmonary bypass for excision of renal tumours with vena caval extension.
P- Reviewers: Raja SG, Taheri S S- Editor: Song XX L- Editor: A E- Editor: Lu YJ
| 1. | Blute ML, Leibovich BC, Lohse CM, Cheville JC, Zincke H. The Mayo Clinic experience with surgical management, complications and outcome for patients with renal cell carcinoma and venous tumour thrombus. BJU Int. 2004;94:33-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 389] [Cited by in RCA: 443] [Article Influence: 21.1] [Reference Citation Analysis (0)] |
| 2. | Glazer AA, Novick AC. Long-term followup after surgical treatment for renal cell carcinoma extending into the right atrium. J Urol. 1996;155:448-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 118] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 3. | Ciancio G, Manoharan M, Katkoori D, De Los Santos R, Soloway MS. Long-term survival in patients undergoing radical nephrectomy and inferior vena cava thrombectomy: single-center experience. Eur Urol. 2010;57:667-672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 117] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 4. | Vaidya A, Ciancio G, Soloway M. Surgical techniques for treating a renal neoplasm invading the inferior vena cava. J Urol. 2003;169:435-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 60] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 5. | Bisleri G, Piccoli P, Cunico SC, Muneretto C. Modified perfusion technique for patients with renal cell carcinoma infiltrating the inferior vena cava. J Thorac Cardiovasc Surg. 2009;137:e42-e44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 6. | Neves RJ, Zincke H. Surgical treatment of renal cancer with vena cava extension. Br J Urol. 1987;59:390-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 354] [Cited by in RCA: 361] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 7. | Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32099] [Cited by in RCA: 38001] [Article Influence: 1000.0] [Reference Citation Analysis (0)] |
| 8. | Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18532] [Cited by in RCA: 24590] [Article Influence: 1171.0] [Reference Citation Analysis (0)] |
| 9. | Haferkamp A, Bastian PJ, Jakobi H, Pritsch M, Pfitzenmaier J, Albers P, Hallscheidt P, Müller SC, Hohenfellner M. Renal cell carcinoma with tumor thrombus extension into the vena cava: prospective long-term followup. J Urol. 2007;177:1703-1708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 129] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 10. | Karakiewicz PI, Suardi N, Jeldres C, Audet P, Ghosn P, Patard JJ, Perrotte P. Neoadjuvant sutent induction therapy may effectively down-stage renal cell carcinoma atrial thrombi. Eur Urol. 2008;53:845-848. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 100] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 11. | Shuch B, Riggs SB, LaRochelle JC, Kabbinavar FF, Avakian R, Pantuck AJ, Patard JJ, Belldegrun AS. Neoadjuvant targeted therapy and advanced kidney cancer: observations and implications for a new treatment paradigm. BJU Int. 2008;102:692-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 133] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 12. | Novara G, Ficarra V, Antonelli A, Artibani W, Bertini R, Carini M, Cosciani Cunico S, Imbimbo C, Longo N, Martignoni G. Validation of the 2009 TNM version in a large multi-institutional cohort of patients treated for renal cell carcinoma: are further improvements needed? Eur Urol. 2010;58:588-595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 168] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 13. | Vaislic C, Puel P, Grondin P, Vargas A. Surgical resection of neoplastic thrombosis in the inferior vena cava by neoplasms of renal-adrenal tract. Vasc Surg. 1983;September-October:322. [RCA] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Ehrlich MP, McCullough JN, Zhang N, Weisz DJ, Juvonen T, Bodian CA, Griepp RB. Effect of hypothermia on cerebral blood flow and metabolism in the pig. Ann Thorac Surg. 2002;73:191-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 166] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 15. | McCullough JN, Zhang N, Reich DL, Juvonen TS, Klein JJ, Spielvogel D, Ergin MA, Griepp RB. Cerebral metabolic suppression during hypothermic circulatory arrest in humans. Ann Thorac Surg. 1999;67:1895-1899; discussion 1895-1899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 279] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 16. | Reich DL, Uysal S, Sliwinski M, Ergin MA, Kahn RA, Konstadt SN, McCullough J, Hibbard MR, Gordon WA, Griepp RB. Neuropsychologic outcome after deep hypothermic circulatory arrest in adults. J Thorac Cardiovasc Surg. 1999;117:156-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 158] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 17. | Griepp RB, Di Luozzo G. Hypothermia for aortic surgery. J Thorac Cardiovasc Surg. 2013;145:S56-S58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 18. | Shuch B, Crispen PL, Leibovich BC, Larochelle JC, Pouliot F, Pantuck AJ, Liu W, Crepel M, Schuckman A, Rigaud J. Cardiopulmonary bypass and renal cell carcinoma with level IV tumour thrombus: can deep hypothermic circulatory arrest limit perioperative mortality? BJU Int. 2011;107:724-728. [PubMed] |
| 19. | Dominik J, Moravek P, Zacek P, Vojacek J, Brtko M, Podhola M, Pacovsky J, Harrer J. Long-term survival after radical surgery for renal cell carcinoma with tumour thrombus extension into the right atrium. BJU Int. 2013;111:E59-E64. [PubMed] |
| 20. | Ciancio G, Shirodkar SP, Soloway MS, Livingstone AS, Barron M, Salerno TA. Renal carcinoma with supradiaphragmatic tumor thrombus: avoiding sternotomy and cardiopulmonary bypass. Ann Thorac Surg. 2010;89:505-510. [PubMed] |
| 21. | Weiss AJ, Lin HM, Bischoff MS, Scheumann J, Lazala R, Griepp RB, Di Luozzo G. A propensity score-matched comparison of deep versus mild hypothermia during thoracoabdominal aortic surgery. J Thorac Cardiovasc Surg. 2012;143:186-193. [PubMed] |
| 22. | Onorati F, Santini F, Telesca M, Veraldi GF, Faggian G, Mazzucco A. Avoiding sternotomy and cardiopulmonary bypass in type IV renal carcinoma: is it really worth it? Ann Thorac Surg. 2011;91:640-641; author reply 640-641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Zierer A, El-Sayed Ahmad A, Papadopoulos N, Moritz A, Diegeler A, Urbanski PP. Selective antegrade cerebral perfusion and mild (28°C-30°C) systemic hypothermic circulatory arrest for aortic arch replacement: results from 1002 patients. J Thorac Cardiovasc Surg. 2012;144:1042-1049. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 111] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 24. | Mazzola A, Gregorini R, Villani C, Colantonio LB, Giancola R, Gravina GL, Vicentini C. Cavoatrial tumor thrombectomy with systemic circulatory arrest and antegrade cerebral perfusion. Ann Thorac Surg. 2007;83:1564-1565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |