Published online Aug 9, 2023. doi: 10.5410/wjcu.v12.i2.10
Peer-review started: April 16, 2023
First decision: June 12, 2023
Revised: June 21, 2023
Accepted: July 7, 2023
Article in press: July 7, 2023
Published online: August 9, 2023
Processing time: 112 Days and 20.9 Hours
Urethral stricture is the abnormal narrowing of the urethra due to spongiofibrosis. The established aetiological factors for urethral stricture abound in our environ
This is the case of a 10-year-old boy who presented with a history of nocturnal urinary incontinence since birth and lower urinary tract symptoms (LUTS) for 3 years culminating in chronic urinary retention. He maintained a normal urge to micturate and continent of urine during the daytime before the onset of LUTS. He had an antecedent longstanding history of tying a rubber band to the penile shaft mostly before going to the bed at night to prevent enuresis due to his peer stigmatization. He was acutely ill-looking, with distended suprapubic region. The phallus and scrotum were enlarged and oedematous with a circumferential proximal penile shaft scar and ventral penile shaft urethrocutaneous fistula. He was diagnosed to have complete short segment bulbopenile stricture and right ectopic ureter. He subsequent had augmented anastomotic urethroplasty and bilateral non-refluxing ureteroneocystostomy at different sitting.
The adherence to surgical principles of urethral stricture and enuresis management where surgically correctable in a child is associated with the resolution of enuresis and social reintegration.
Core Tip: Enuresis is a psycho-socially challenging and emotionally traumatic condition. This paper brings to light the management of secondary nocturnal enuresis in a 10-year-old male child with an attendant urethral stricture. A complication resulting from the longstanding application of rubber band to the penile shaft to prevent enuresis and stigmatization by his peers. The clinical presentation of this case is clouded by the clinical features of the dual pathology. Hence, a step-wise application of the surgical principle of clinical evaluation, laboratory and imaging investigations and surgical treatment is associated with resolution of enuresis and patient satisfaction.
- Citation: Khalid A, Nasiru M, Abdulwahab-Ahmed A, Muhammad AS, Agwu NP, Lukong CS. Phallic rubber band application to prevent enuresis unusual cause of urethral stricture in a child: A case report. World J Clin Urol 2023; 12(2): 10-16
- URL: https://www.wjgnet.com/2219-2816/full/v12/i2/10.htm
- DOI: https://dx.doi.org/10.5410/wjcu.v12.i2.10
Urethra stricture disease is a very common urologic condition in our environment[1]. It is the abnormal narrowing of the urethra due to spongiofibrosis[2]. It is the fourth most commonly diagnosed annual new urologic disease seen in our clinical setting among male adults[3]. Post-inflammatory aetiology mainly from post-gonococcal urethritis closely followed by posttraumatic causes due to road traffic accidents or falling astride is encountered frequently[1,3]. In our setting, urethral stricture disease is a less common condition among the paediatric population when compared to the adult population. Urethral stricture when seen in children is often idiopathic or as an iatrogenic consequence commonly resulting from urethral catheterization or hypospadias surgery, especially in younger children usually involving the anterior urethra[4]. In older children, traumatic aetiologies from pelvic injury predominate and commonly affect the posterior urethra[4]. Other reported causes though rare in older children include post-infective urethritis and from lichen sclerosis[4]. The phenomenon of phallic strangulation by a wide variety of objects ranging from nonmetallic to metallic objects has been reported commonly among adults that may result in urethral stricture though rarely encountered in children[5]. Several reasons adduced for this include presence of psychiatric conditions, induction or enhancement of erection for those with erectile dysfunction, and avoidance of coitus were advanced to explain why adults strangulate phallus[5]. In children, however, the actual reason may differ from adults and attempt at controlling enuresis may be a possible reason. The peer ridicule, stigmatization influence may be a strong motivator in children. The application of phallic rubber to prevent enuresis is not a familiar practice among children with enuresis in our environment, let alone urethral stricture as its complication. The application of constricting devices particularly when prolonged initially causes phallic tissue ischemia, urethral erosion and fistulation. If complicated by urinary tract infection or urethritis, the subsequent healing by fibrosis may results in urethra stricture formation. The key investigative modalities for urethral stricture diagnosis according to American Urological Association (AUA) guidelines are urethrocystoscopy, retrograde urethrography, voiding cystourethrography, or ultrasound urethrography[6]. The management of urethra stricture should be guided by the strict application of its surgical principles.
Enuresis is a psychosocially challenging and emotionally traumatic condition. According to the American Pediatric Academy, it refers to the involuntary wetting of clothes or bedding by urine during the daytime or nighttime for a period of at least 3 consecutive months in children older than 5 years of age[7,8]. The nighttime bed wetting or nocturnal enuresis occurs more frequently and tends to be multifactorial, and affects mostly girls[8]. Family history is a strong risk factor[8]. It can be primary, being the most common type in which there is no period of 6 consecutive months of nighttime urinary control[8]. The secondary type of enuresis is associated with organic or psychological aetiologies and in this variety; the children have a periods of 6 consecutive months of nighttime urinary control before the onset of incontinence[8]. In girls primary enuresis is a common occurrence while secondary enuresis predominates in boy with ectopic ureter being a culprit[8-10]. The management of enuresis involves clinical evaluation, relevant laboratory investigations such as urinalysis and urine culture, and urinary tract imaging investigations: Namely ultrasound scan, radiography, computerized tomography scanning, and magnetic resonance imaging as may be necessary. Its treatment ranges from nonsurgical and nonpharmacological options such as urotherapy, limitation of fluid intake, and bedwetting alarm to pharmacological agents such as desmopressin, imipramine, and Oxybutynin among other agents and rarely surgery where a definite amenable cause is found[8]. Other treatment options worth mentioning are Transcutaneous Parasacral Electrical Nerve Stimulation and Functional Magnetic Stimulation[8].
The clinical entity of urethra stricture arising from a rare aetiology such as phallic rubber band application as an attempt at self-treatment of enuresis in a child is scarce in the literature. To the best of our knowledge, this is the first reported case of its kind. We report this unusual cause of urethral stricture in a male child with enuresis and its holistic management. The aim of this paper is to highlight the psychosocial impact and management challenges of a child with enuresis (nocturnal urinary incontinence).
This is the case of a 10-year-old boy who presented with a history of nocturnal urinary incontinence since birth and lower urinary tract symptoms (LUTS) for 3 years.
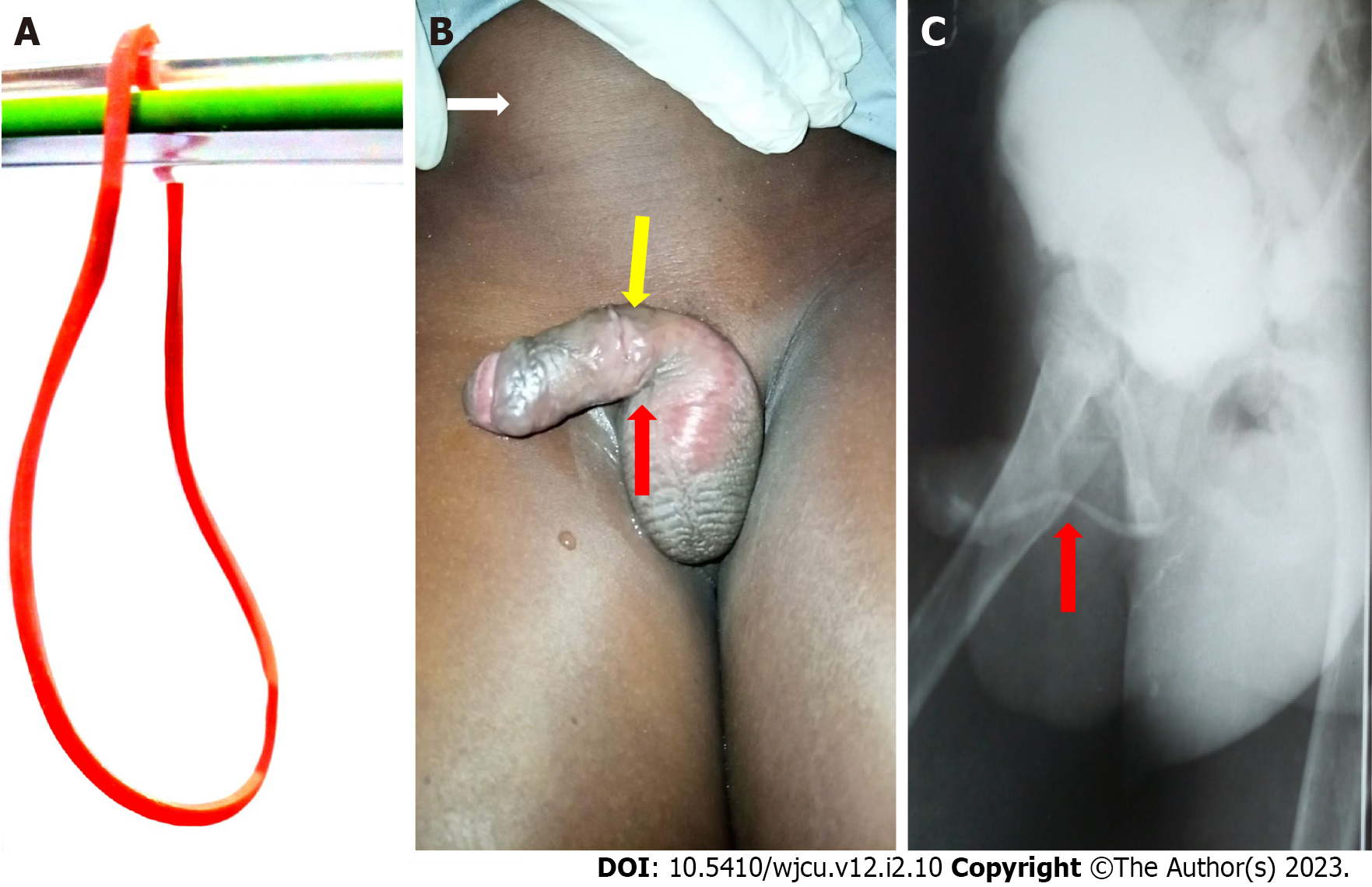
He was noticed by parent to be having nocturnal urinary incontinence beyond the age of achieving urinary continence. Three years before presentation, he had voiding and storage LUTS associated with leakage of urine from the ventral surface of the penile shaft. The symptoms progressively worsened over time culminating in chronic urinary retention. Before onset of LUTS, he maintained a normal urge to micturate and the continence of urine during the daytime. The attempt at urethral catheterization at presentation to our facility was unsuccessful warranting open suprapubic cystostomy. There was an associated history of recurrent fever, anorexia, nausea, and penile swelling for which he was treated on several occasions for urinary tract infections at the referral health facility. He had an antecedent longstanding history of tying a rubber band to the penile shaft mostly before going to the bed at night to prevent enuresis due to his peer stigmatization (Figure 1A and B).
There was no remarkable past medical or surgical history.
There was no associated history of psychiatric illnesses, family history of enuresis, or other remarkable histories.
He was acutely ill-looking, not in painful or respiratory distress, afebrile, pale, and dehydrated but not jaundiced with ammoniacal odour. His temperature, respiratory rate, pulse rate, and blood pressure were 36.1 °C, 24 cycles/min, 102 beats/min, and 100/60 mmHg respectively. The abdomen was full and moved with respiration. The suprapubic region was distended and stony dull to percussion. The phallus and scrotum were enlarged and oedematous with a circumferential proximal penile shaft scar and ventral penile shaft urethrocutaneous fistulous exit at the scar site (Figure 1B). The digital rectal and other systemic examinations were unremarkable.
The complete blood cell count was 7.4 × 109/L and pretransfusion and posttransfusion packed cell volumes of 24% and 30.6% respectively. The serum urea was 18.1 mmol/L, creatinine 2.7 mg/dL, and electrolytes: Na+ 132 mmol/L, K+ 3.6 mmol/L, HCO3- 18 mmol/L and Cl- 96 mmol/L. The urinalysis was positive for nitrites, leukocytes, blood, and protein. The urine culture yielded growth of Staphylococcus aureus sensitive to cefotaxime among others.
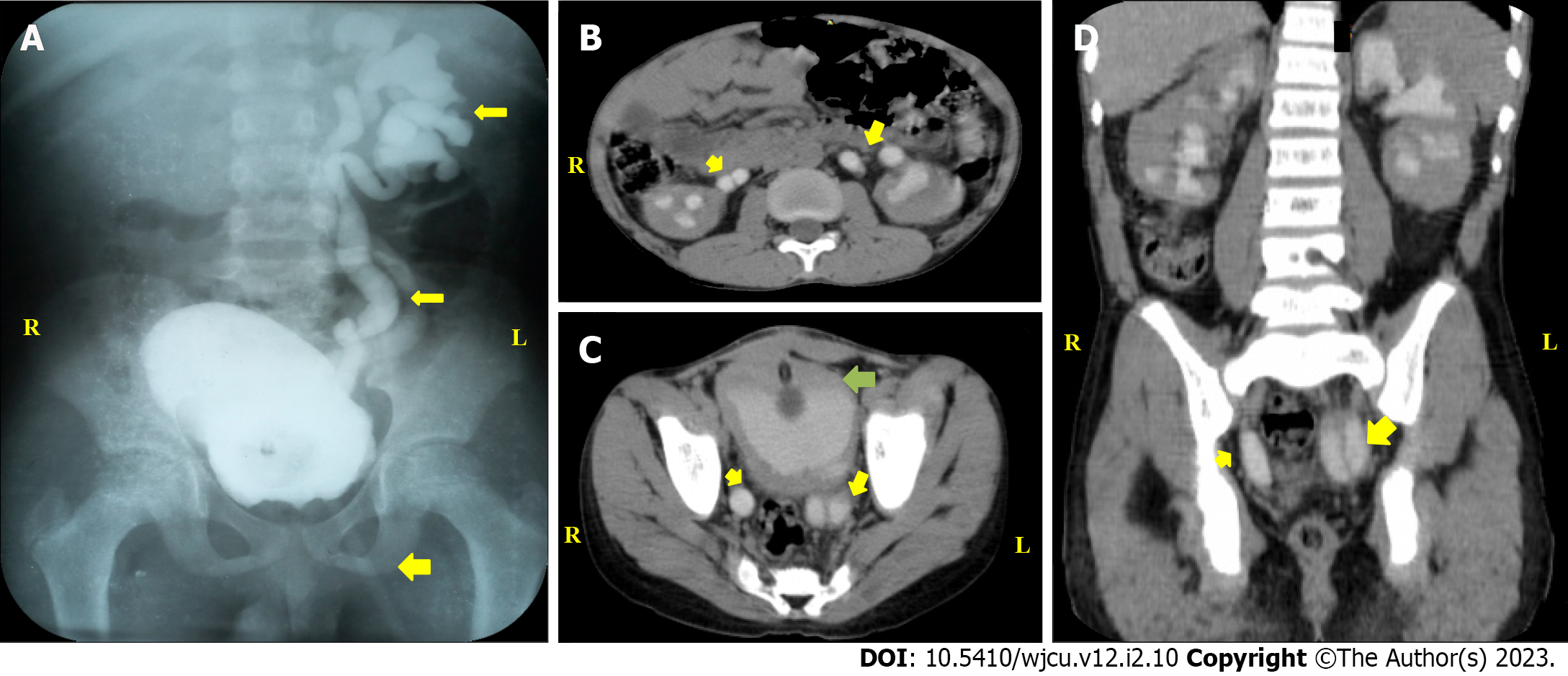
Abdominal Ultrasound scan showed a grossly distended bladder with bilateral moderate to severe hydronephrosis with bilateral hydroureters. The combined retrograde urethrogram and voiding cystourethrogram done later showed normal anterior and posterior urethra with an area of stricture in evolution but the contrast was noticed to be exiting the phallus ventrally at the site of application of the rubber band (Figure 1B and C), dilated bladder and left duplex system with grade IV vesicoureteral reflux into the duplex system (Figure 2A). There was no demonstrable reflux or visualization of the right ureter (Figure 2A).
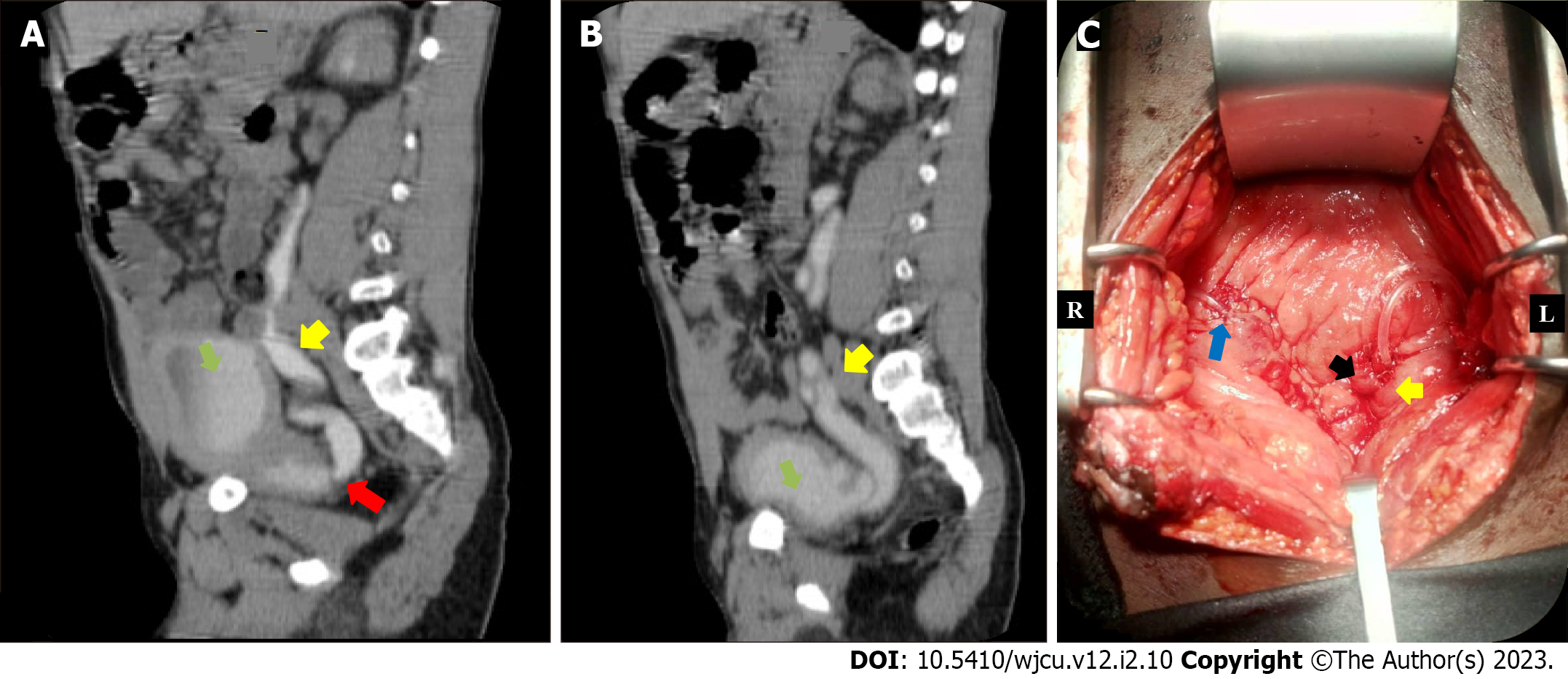
The abdominal computerized tomography scan revealed bilaterally functioning kidneys with a partial and complete duplex (double ureters and collecting system) on the right and left respectively (Figure 2B-D), and the right lower ureter insertion into the region of the prostatic urethra and left duplex ureters insertion into the bladder (Figure 3A and B).
At this point, a diagnosis of enuresis secondary to the right ectopic ureter was made (Figure 3A) with a grade IV left duplex or double ureter reflux (Figure 3B).
He had intravenous fluid, parenteral antibiotics, and a unit of blood transfusion. An initial suprapubic cystostomy was performed which drained urine of 1000 mL. He was discharged home on continuous bladder drainage and monthly suprapubic catheter (14fr) replacement until 8-mo later when Augmented Anastomotic Urethroplasty was performed. The intraoperative findings were a complete short-segment bulbopenile urethral stricture about 1.5 cm long with a fistulous tract arising adjacent to the proximal part of the stricture and ending blindly into the ventral penile shaft skin.
Thereafter, the caregiver was counseled and educated on conservative management of enuresis essentially involving lifestyle modifications with some improvement. However, enuresis persisted despite these measures leading to further imaging investigation (Figure 3A and B).
The parents were counseled and he had exploratory laparotomy with non-refluxing right ureteroneocystostomy and non-refluxing left duplex system ureteroneocystostomy (as common sheath reimplantation) with improvised (feeding tubes) as external ureteric stents, Figure 3C. He had silicon urethral catheter drainage for three weeks. Both stents and catheter were removed at 3-wk postoperative day. He did well postoperative and was discharged home on the 14th postoperative day.
He was 2 years on the follow-up visits after last surgery; the enuresis stopped, and was well-integrated among his peers.
This case report brings to light an uncommon aetiology of urethral stricture in a child with enuresis. The clinical presentation of this dual pathology in a child presents the clinician with a herculean task due to the clouded picture of symptoms. In the index patient, although the history of nocturnal enuresis dated to birth, the thought of an organic cause was not clear at the time of presentation. Therefore, the application of surgical principles in the management of this dual pathology comes in handy. The urethral stricture was diagnosed using the combination of retrograde urethrogram and voiding cystourethrogram, and had urethroplasty, one of the diagnostic investigations and treatments respectively recommended by AUA guidelines[6]. After this treatment, he had the non-pharmacological treatment of enuresis including urotherapy and limitation of fluid intake, which is often the first line of treatment with good outcome in the majority of patients with primary nocturnal enuresis[8]. He had some symptomatic improvement. However, the improvement was short-lived as symptoms persisted later. This led to the reconsideration of our initial thoughts of primary nocturnal enuresis.
At this point, it became pertinent to consider secondary nocturnal enuresis in which organic or psychological aetiologies may be present[8]. Moreso, primary nocturnal enuresis is commonly seen in girls and family history is a strong factor[8]. The index patient is a male child and had no family history of nocturnal enuresis. Also during evaluation for the urethra stricture, the findings of the left refluxing duplex ureter a congenital anomaly, and non-visualization or reflux in the right ureter (Figure 2A) in a patient with infravesical obstruction is not consistent with the commonly observed bilateral vesicoureteral reflux and thus raised our suspicion of a possible congenital etiology or secondary nocturnal enuresis. This informed the decision to request for computerized tomography scan of the abdomen which confirmed the diagnosis of the right ectopic ureter and left duplex ureter (Figure 3A and B).
The right ectopic ureter is inserted into the region of the prostatic urethra (Figure 3A) bypassing the internal sphincter mechanisms, one of the male continence factors. This means the urine from the right kidney can only be controlled by the voluntary external sphincter. As such, in the daytime when the child is awake, he can maintain continence throughout the day but when deeply asleep at night he loses the voluntary external sphincter urine control resulting in secondary nocturnal enuresis. However, the patient maintained the urge to micturate despite enuresis because the duplex left ureter was inserted normally into the bladder (Figure 3B). Hence, urine from the left kidney enters the bladder under both internal and external sphincteric control. It is noteworthy that up to half the cases of male ectopic ureters inserts into the posterior urethra as observed in the index case aside from other rare locations[9]. As such urinary incontinence due to ectopic ureter is an uncommon presentation in male as observed in this case due the protective role of the external sphincter. Conversely, female ectopic ureter inserts often into the female genital organs such as vagina which makes incontinence a prominent feature[10].
The index patient was managed based on surgical principles. This involves initial management of the urethra stricture followed by the nocturnal enuresis. Hence the initial emphasis here was to divert the urinary retention to aid control of infection and preservation of renal function. The patient presented with clinical and laboratory features of infection and renal impairments. Thereafter, he was investigated for the cause of urinary retention before the definitive urethroplasty for the complete short segment bulbopenile urethral stricture. Then, the parent was counseled on the nonpharmacological modality for the treatment of enuresis which led to a short-lived symptomatic improvement. The persistence of enuresis led to further investigation that confirms the diagnosis of the right ectopic ureter and left duplex ureter warranting bilateral non-refluxing ureteroneocystostomy (Figure 3C). This surgical treatment resolved the secondary nocturnal enuresis. The surgery has dual benefits. Firstly, it corrected the secondary nocturnal enuresis caused by the right ectopic ureter and secondly prevented the reflux of the left duplex system that is capable of compromising the renal function in the long term from recurrent urinary tract infection. Apart from open surgical treatment offered in this case, report of laparascopic treatment amongst other operative techniques for managing patient with duplex ureter are available in the literature[11].
This paper aims to highlight the psychosocial impact and management challenges of a child with enuresis (nocturnal urinary incontinence). Urethral stricture following applications of the rubber band to the phallus is an uncommon presentation in children. Once urethral stricture is established, management should be guided by general principles of management of urethral stricture resulting from other aetiologies. Where failed conservative treatment of primary nocturnal enuresis occurs, secondary nocturnal enuresis should be considered and further investigations should be tailored toward unraveling the aetiology. The surgical treatment of enuresis is rewarding where the aetiology is known and associated with the complete resolution of the enuresis and social reintegration of the patient. This case management was challenging and we recommend the early use of imaging investigations in the evaluation of enuresis where symptoms persist despite conservative treatment.
We sincerely thank all the hospital staffs who assisted financially or in kinds during the patient treatment.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: American College of Surgeons, No. 3355571.
Specialty type: Medicine, research and experimental
Country/Territory of origin: Nigeria
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Han J, China; Taskovska M, Slovenia S-Editor: Fan JR L-Editor: A P-Editor: Zhao S
| 1. | Mbibu NH, Nwofor AM, Khalid L. Spectrum of urologic disease in the West African sub-region. Ann Afr Med. 2002;1:44-52. |
| 2. | Latini JM, McAninch JW, Brandes SB, Chung JY, Rosenstein D. SIU/ICUD Consultation On Urethral Strictures: Epidemiology, etiology, anatomy, and nomenclature of urethral stenoses, strictures, and pelvic fracture urethral disruption injuries. Urology. 2014;83:S1-S7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 117] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 3. | Mungadi IA, Khalid A. Spectrum of urological cases in a West African Tertiary Hospital. Ann Afr Med. 2021;20:14-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Ansari MS, Yadav P, Srivastava A, Kapoor R, Ashwin Shekar P. Etiology and characteristics of pediatric urethral strictures in a developing country in the 21st century. J Pediatr Urol. 2019;15:403.e1-403.e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Kyei MY, Asante EK, Mensah JE, Klufio GO, Paintsil A, Gepi-Atee S, Morton B, Ampadu K, Toboh B. Penile Strangulation by self-Placement of Metallic Nut. Ghana Med J. 2015;49:57-59. [PubMed] |
| 6. | Bayne DB, Gaither TW, Awad MA, Murphy GP, Osterberg EC, Breyer BN. Guidelines of guidelines: a review of urethral stricture evaluation, management, and follow-up. Transl Androl Urol. 2017;6:288-294. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | Nevéus T, von Gontard A, Hoebeke P, Hjälmås K, Bauer S, Bower W, Jørgensen TM, Rittig S, Walle JV, Yeung CK, Djurhuus JC. The standardization of terminology of lower urinary tract function in children and adolescents: report from the Standardisation Committee of the International Children's Continence Society. J Urol. 2006;176:314-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 928] [Cited by in RCA: 874] [Article Influence: 46.0] [Reference Citation Analysis (0)] |
| 8. | Arda E, Cakiroglu B, Thomas DT. Primary Nocturnal Enuresis: A Review. Nephrourol Mon. 2016;8:e35809. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 9. | Milicevic S, Bijelic R, Krivokuca V, Jakovljevic B. Duplex System with Ectopic Ureter Opens into the Posterior Urethra: Case Report. Med Arch. 2018;72:145-147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Krishnan A, Baskin LS. Identification of ectopic ureter in incontinent girl using magnetic resonance imaging. Urology. 2005;65:1002. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Wang SB, Wan L, Wang Y, Yi ZJ, Xiao C, Cao JZ, Liu XY, Tang RP, Luo Y. Laparoscopic treatment of bilateral duplex kidney and ectopic ureter: A case report. World J Clin Cases. 2022;10:8344-8351. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |