Copyright
©2014 Baishideng Publishing Group Inc.
World J Clin Urol. Jul 24, 2014; 3(2): 96-112
Published online Jul 24, 2014. doi: 10.5410/wjcu.v3.i2.96
Published online Jul 24, 2014. doi: 10.5410/wjcu.v3.i2.96
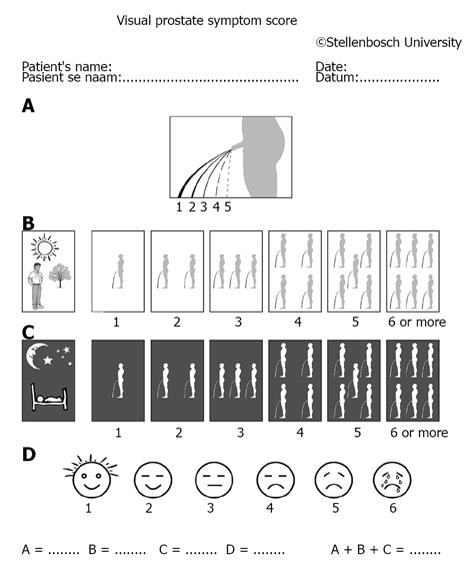
Figure 1 Visual prostate symptom score consisting of pictograms to evaluate (A) force of the urinary stream, (B) daytime frequency, (C) nocturia, and (D) quality of life[9].
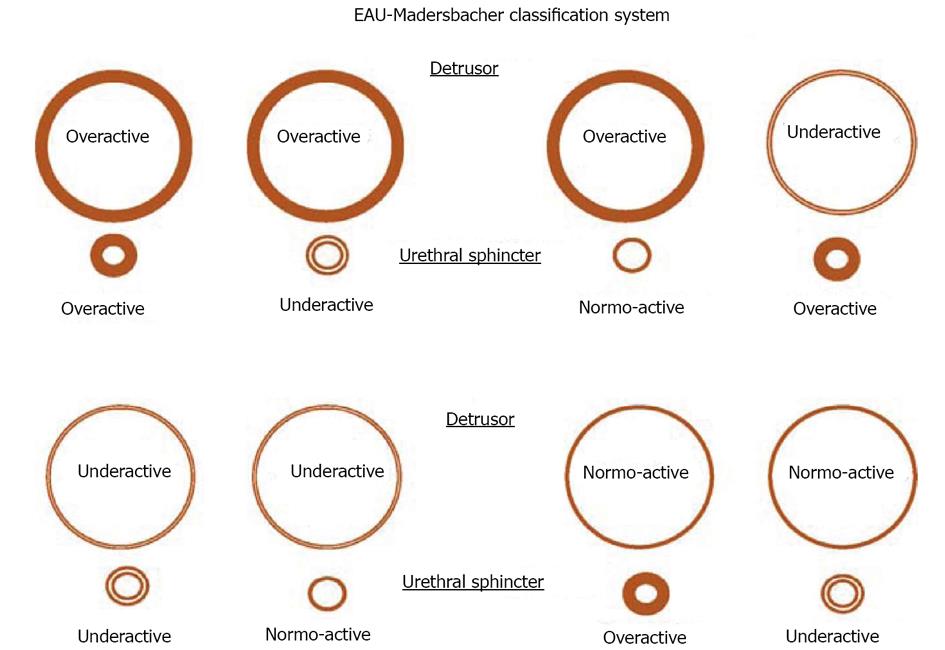
Figure 2 The European Association of Urology-Madersbacher classification system[15].
EAU: European Association of Urology.
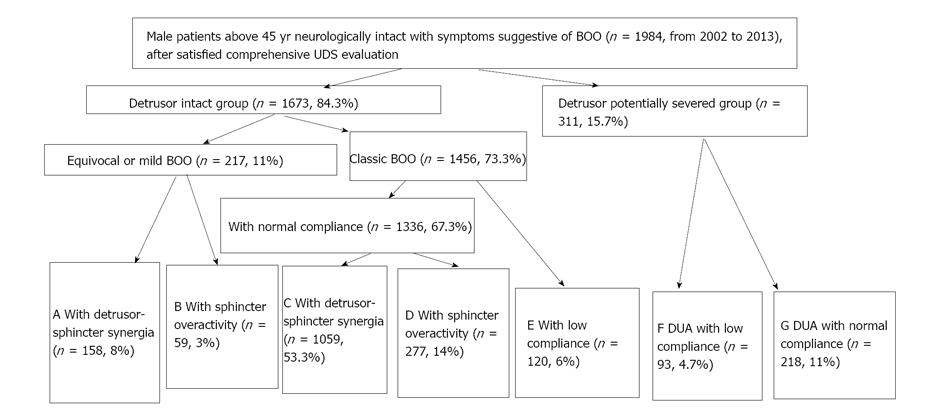
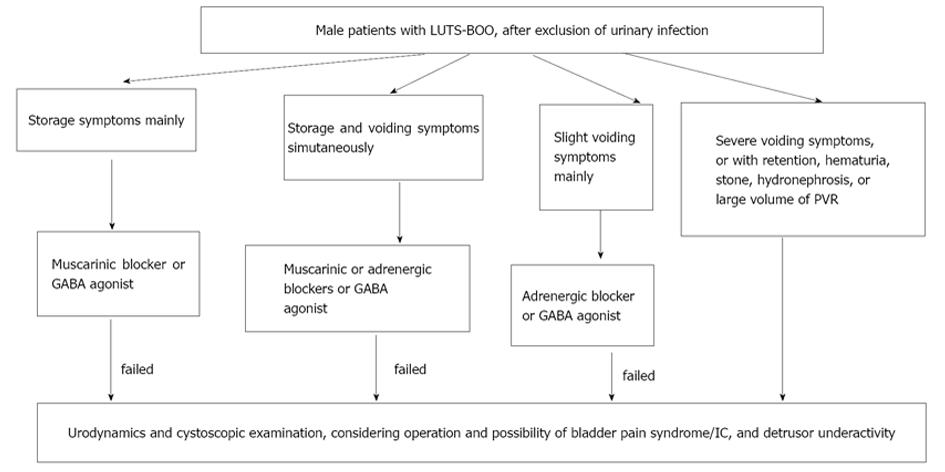
Figure 3 Study design, flow diagram and final outcome of male patients above 45 years neurologically intact with symptoms suggestive of male symptoms of lower urinary tract and bladder outlet obstruction[17].
UDS: Urodynamics; DUA: Detrusor underactivity; BOO: Bladder outlet obstruction.
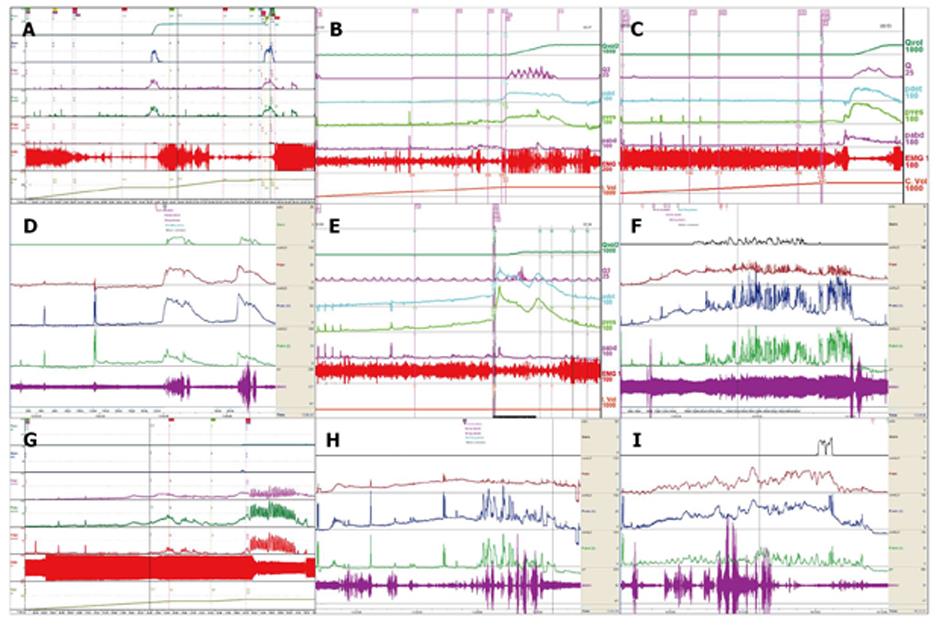
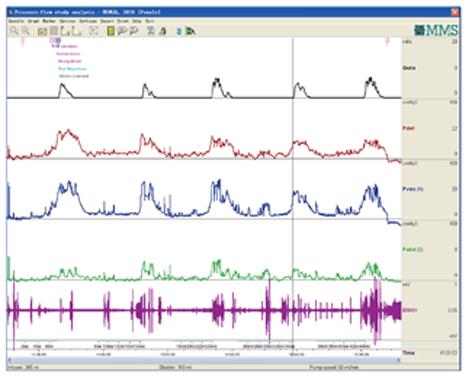
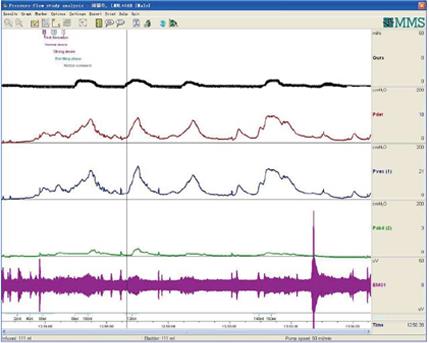
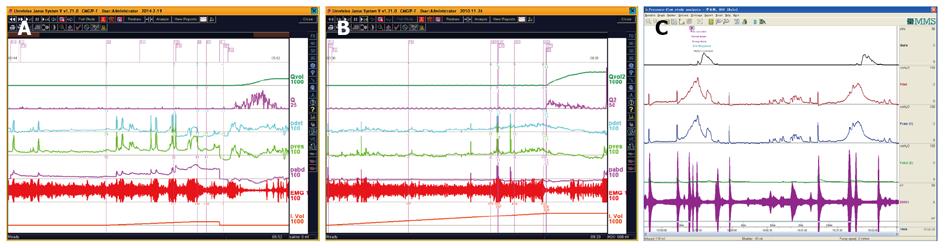
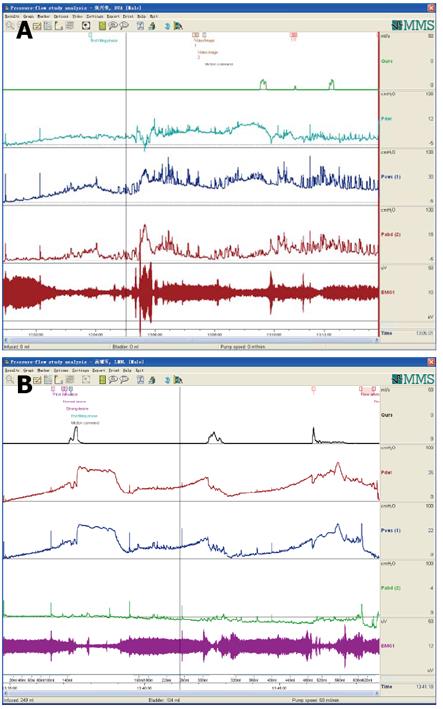
Figure 4 Urodynamic patterns of male patients older than 45 years neurologically intact with symptoms of lower urinary tract/bladder outlet obstruction[17].
A: Pattern A [equivocal or mild bladder outlet obstruction (BOO) with sphincter synergia with or without idiopathic detrusor overactivity]; B: Pattern B (equivocal or mild BOO with idiopathic sphincter overactivity); C: Pattern C (classic BOO with sphincter synergia); D: Pattern D (classic BOO with idiopathic sphincter overactivity); E: Pattern E (BOO with only detrusor low compliance); F: Pattern F (BOO with both detrusor underactivity and low compliance); G: Pattern G (equivocal BOO with detrusor underactivity); H: Urodynamic study of a patient with pattern F; I: The same patient with pattern F as in H after 4 wk urinary draining, whose detrusor contraction recovered and urodynamic study pattern was transformed into pattern E.
Figure 5 A proposed supplement to the guideline of male symptoms of lower urinary tract/bladder outlet obstruction[17].
BOO: Bladder outlet obstruction ; LUTS: Symptoms of the lower urinary tract.
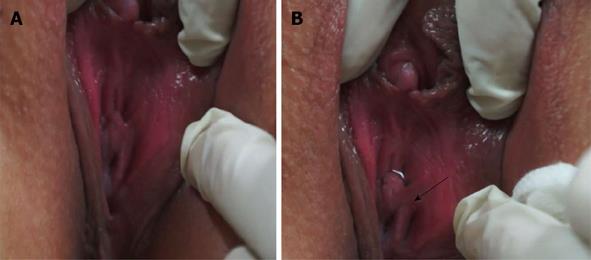
Figure 6 Perineal view of a female patient with urethral external sphincter agenesis before urodynamic evaluation.
A: Urethral orifice and hymen as the urethral orifice was dried with gauze; B: Urine expelled out as solid arrow indicated.
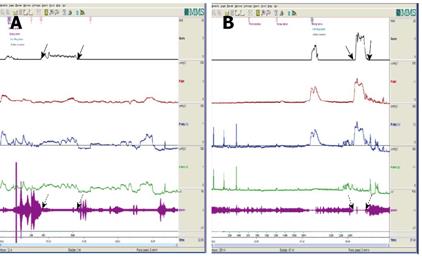
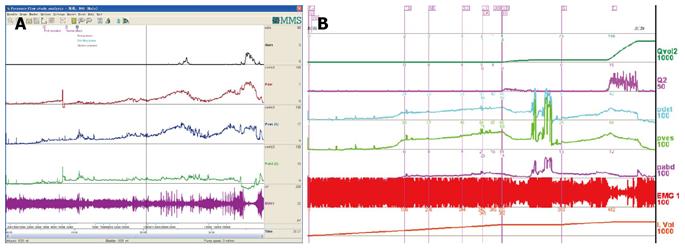
Figure 7 Comprehensive urodynamic evaluation of a patient with urethral sphincter agenesis.
A: As saline was infused into the bladder, saline and her urine were expelled steadily (solid arrows) in the initial examination, however, during this phase, anal sphincter electromyogram showed synergia (as dotted arrows indicated); B: The storage and voiding function was recovered to normal and incontinence cured 4 mo after sphincteroplasty.
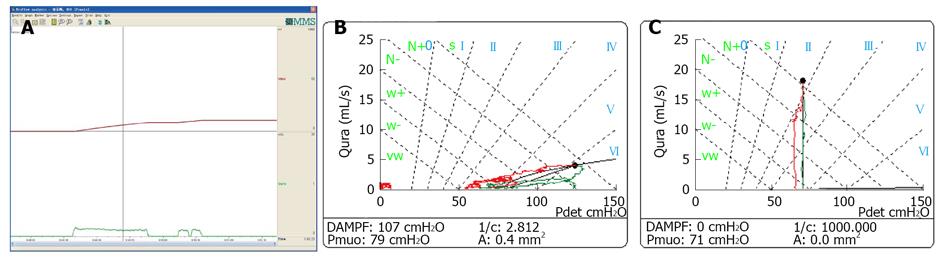
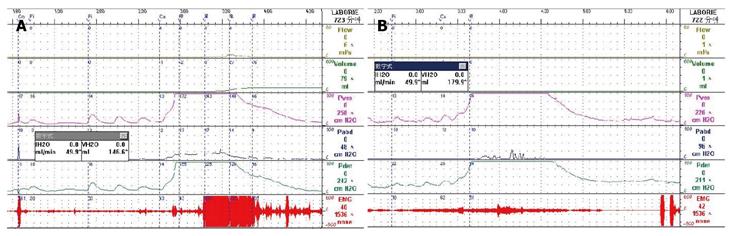
Figure 8 Low-smooth uroflowmetry curve in a female patient confirmed with urethral stricture, constrictive bladder outlet obstruction and compressive bladder outlet obstruction.
A: Low-smooth uroflowmetry curve in a female patient confirmed with urethral stricture; B: Constrictive bladder outlet obstruction (BOO) produces a decreased slope of the passive urethral resistance relation (PURR) curve and a normal minimal opening pressure (Pmuo); C: Compressive BOO produces a steep slope of PURR curve and a higher Pmuo[25].
Figure 9 Repeated urodynamic curve of a female patient aged 69 years with urinary urgency and frequency for more than 20 years, proved as idiopathic sphincter overactivity with a functional bladder capacity of 80 mL and cured by baclofen 10 mg, tid.
The characteristic findings of idiopathic sphincter overactivity were equivocal in the first and fourth urodynamic evaluations and obvious in the remaining ones.
Figure 10 Repeated urodynamic curve of a male patient aged 80 years with urinary urgency and incontinence associated with acute myelitis for more than 11 years, proved as NDO, which had full response to administration of muscarinic blocker.
Figure 11 Repeated urodynamic curve of a male patient aged 37 years with urinary retention after lumbar tumor resection for one month, proved as neurogenic detrusor overactivity (i.
e., neurogenic detrusor hyperreflexia) and non-sympathetic overactivity (i.e., detrusor-external sphincter dyssynergia).
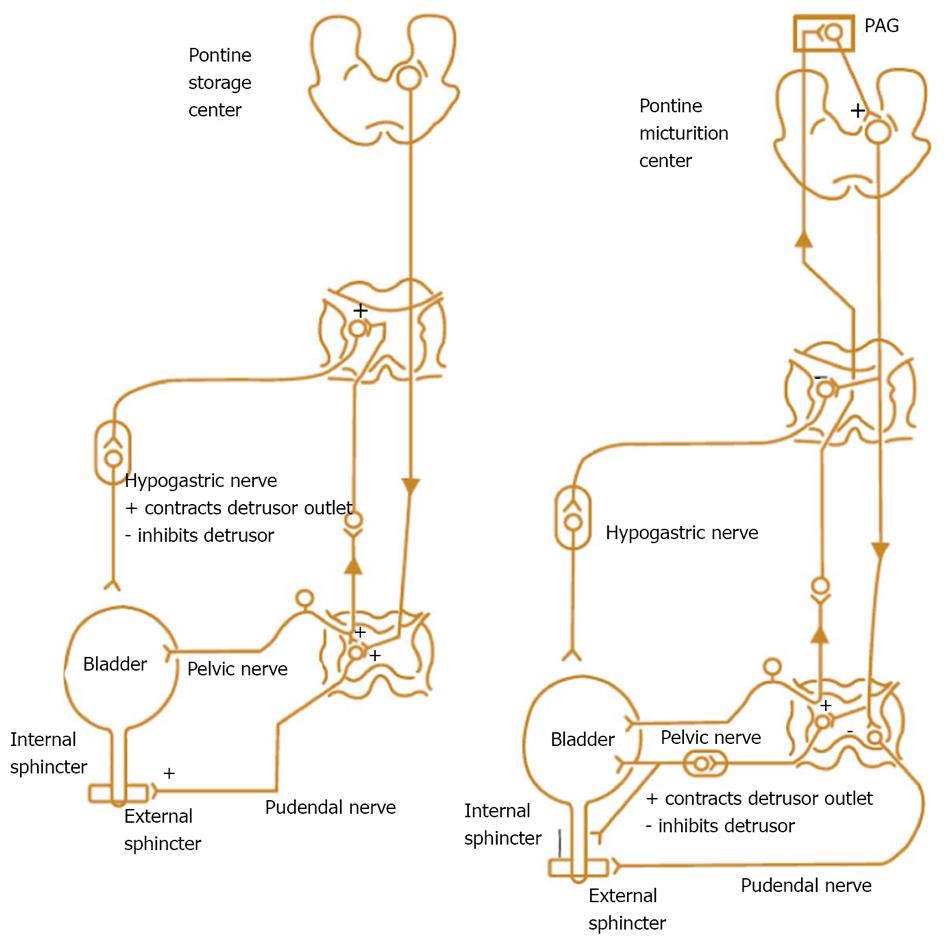
Figure 12 Nerve supply to the bladder and urethra and nerve signal transduction during storage and emptying phase[36].
PAG: Periaqueductal gray.
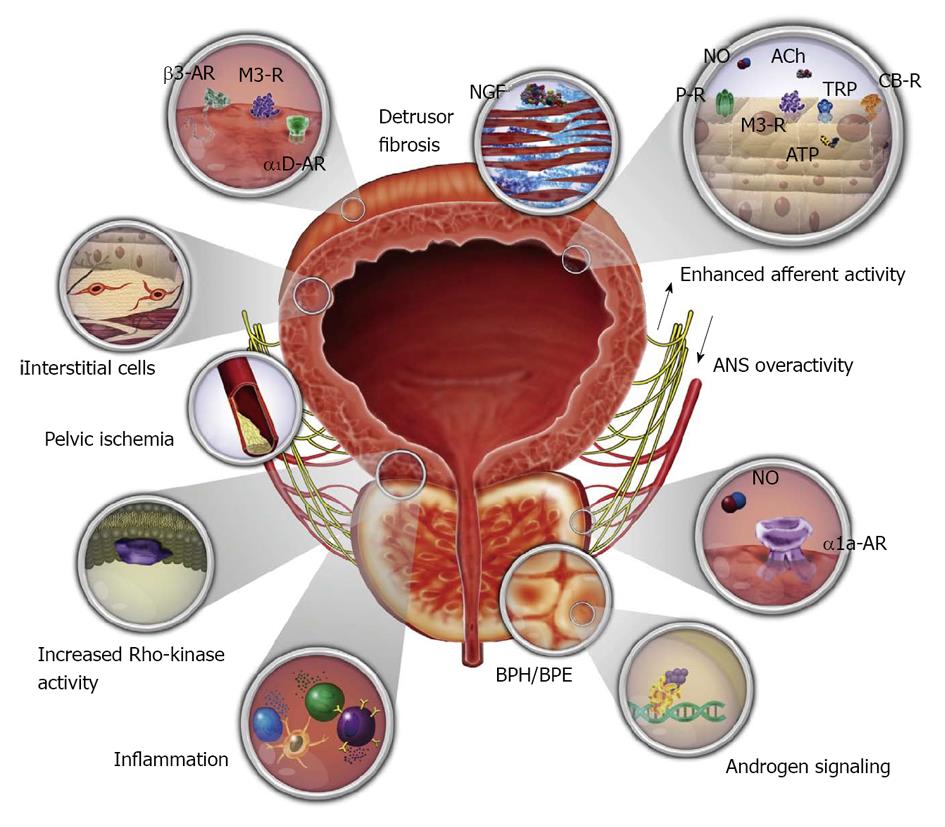
Figure 13 Various autonomic receptors of the bladder and urethra associated with pharmacotherapy for male symptoms of the lower urinary tract[37].
Figure 14 Severe urge incontinence caused by idiopathic sphincter overactivity was cured with baclofen.
A: A 39-year-old woman presented with urge incontinence for 10 year. Urodynamics (UDS) showed that she had idiopathic sphincter overactivity (ISO); B: The ISO improved obviously after administration of baclofen for 2 wk; C: Six weeks after the first consultation, her ISO appearance disappeared absolutely.
Figure 15 Refractory idiopathic sphincter overactivity-induced bladder outlet obstruction for 18 years cured with baclofen within three weeks.
A: Urodynamic (UDS) curve of the woman aged 26 years whose complaints were poor-weak flow and voiding difficulty, undertaken before consultation; B: UDS curve undertaken four years ago.
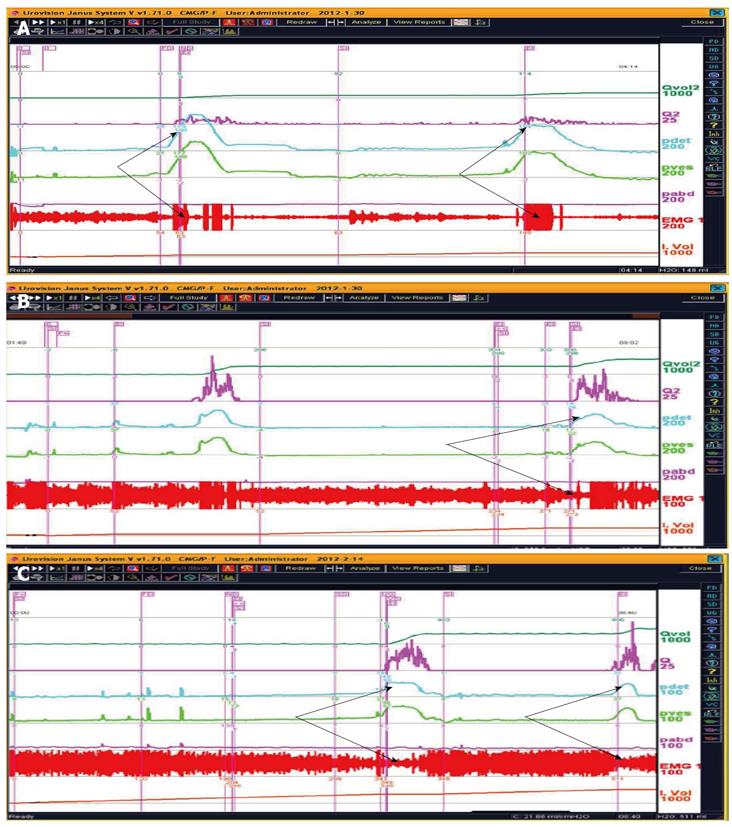
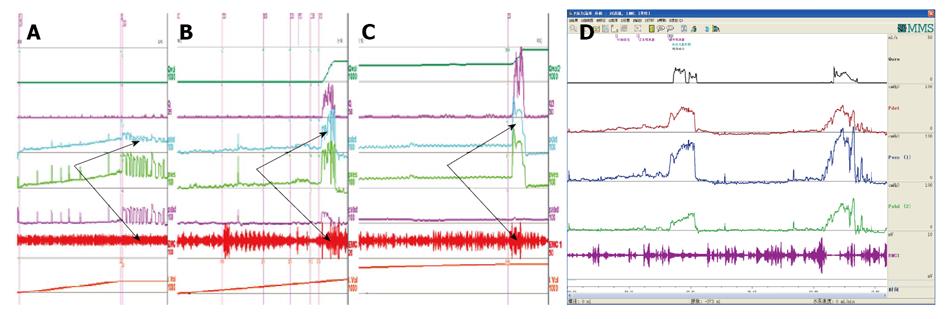
Figure 16 Various detrusor underactivity manifestations coupled with idiopathic sphincter overactivity and abdominal straining.
A: A woman complaining of urinary incontinence was confirmed with detrusor underactivity (DUA) and idiopathic sphincter overactivity (ISO); B: A male patient aged 86 years complaining of poor-weak flow after benign prostatic hyperplasia (BPH) operation was confirmed with DUA and abdominal straining with detrusor-sphincter synergia; C: A female patient suffering from bladder overdistention was confirmed with DUA and ISO; D: A female aged 55 years suffering from incontinence was proved with DUA, ISO and nearly normal Qmax.
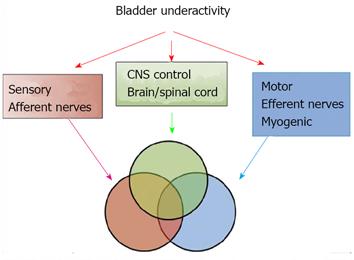
Figure 17 Mechanisms involved in bladder underactivity[42].
CNS: Central nervous system.
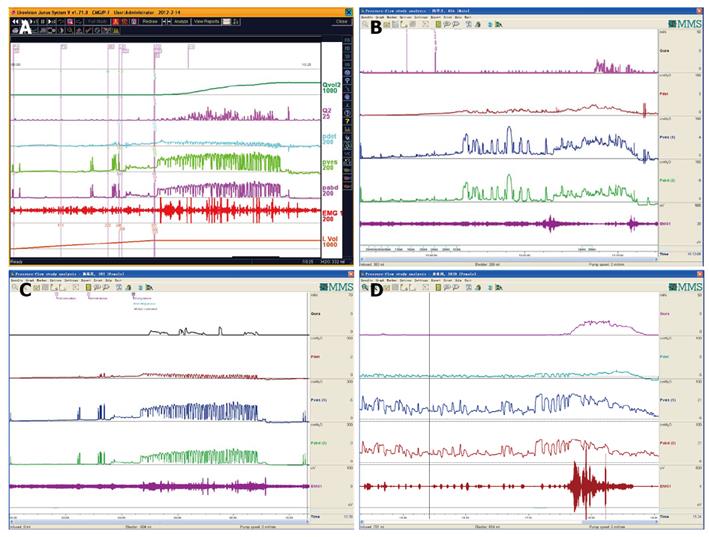
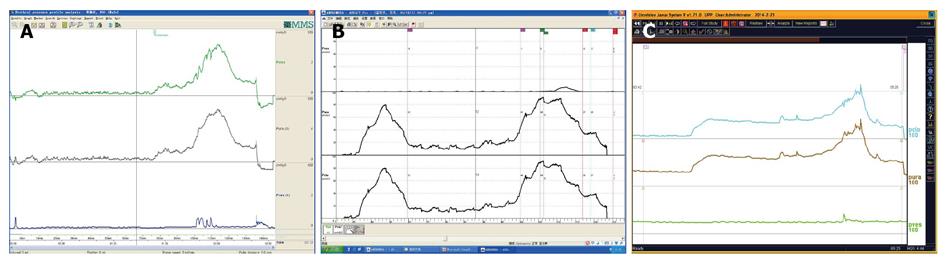
Figure 18 By means of efficient relaxation of the sphincter, satisfactory micturition fulfilled even without detrusor contraction in patients with symptoms of the lower urinary tract or neurogenic symptoms of the lower urinary tract.
A: A female patient suffering from stress urinary incontinence had a satisfactory pressure-flow study; B: A woman passed urine fluently without action of the detrusor; C: A male patient with detrusor underactivity and low compliance voided by efficient sphincter relaxation.
Figure 19 Bilateral hydroureteronephrosis due to bladder low compliance associated with diabetes insipidus and pituitary disorder.
A: A male patient aged 42 years complaining of polyuria had low compliance and intact detrusor and sphincter. The residual urine reached 1550 mL after 700 mL saline voided out; B: A male patient aged 23 years had low compliance and no detrusor underactivity or detrusor-external sphincter dyssynergia. His detrusor could contract violently based on raised detrusor pressure and void 900 mL urine.
Figure 20 Effective neuroanastomosis resulting in recovery of micturition reflex and the patients getting rid of catheter-dependent state.
A female patient aged 46 years had her new reflex succeeded 5 and 9 years after the anastomosis (B and C) as compared with preoperation (A); D: A male patient aged 39 years gained satisfying lower urinary tract function 2 years after the anastomosis, especially with detrusor-sphincter synergia now.
Figure 21 Typical urethral pressure profilometry curves in male patients suffering from benign prostatic hyperplasia.
A: Classic urethral pressure profilometry (UPP) curve of male patients with benign prostatic hyperplasia induced bladder outlet obstruction; B: Bimodal UPP curve of patients with enlarged middle lobe; C: Severely big prostate possesses a long functional profile length.
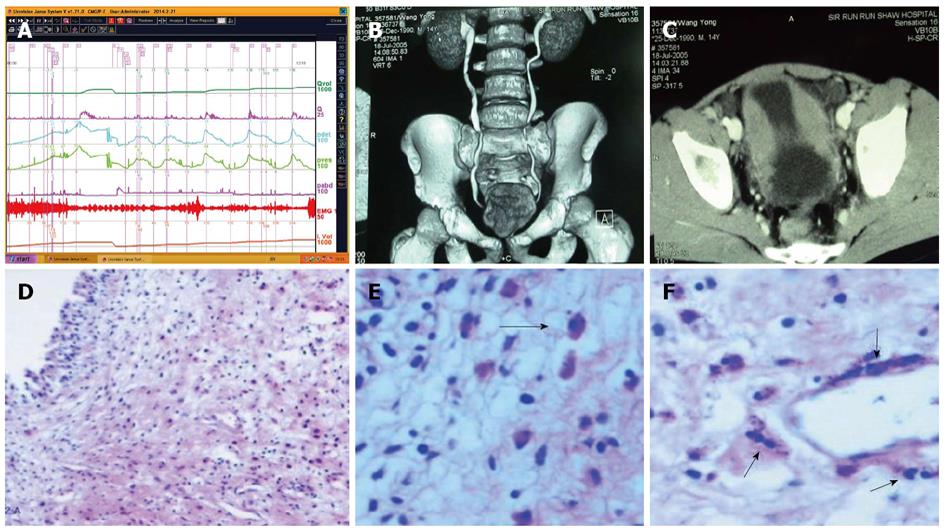
Figure 22 Acidophilic cystitis resulting in poor-weak flow and vomiting in a 15-year-boy was proved as normal detrusor and sphincter function, low compliance, and cured with steroid[50].
A: Although there was neither bladder outlet obstruction (BOO) nor idiopathic sphincter overactivity (ISO), his compliance was low; B: Bladder computed tomography (CT); C: Bladder CT with 3D imaging; D-F: Bladder biopsy specimen: eosinophilic cell suffusion infiltration and proliferation of spindle cells (HE staining).
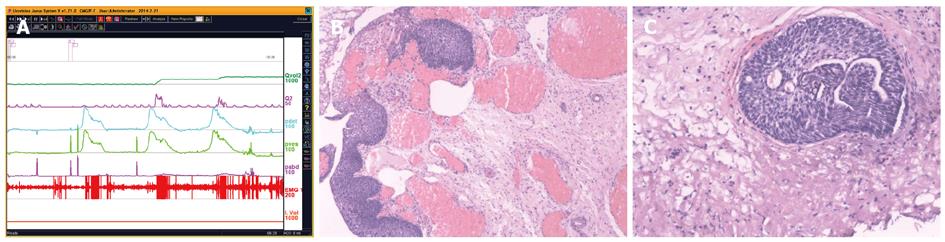
Figure 23 Squamous metaplasia or glandular cystitis of the bladder neck may be caused by longstanding idiopathic sphincter overactivity and produces bladder outlet obstruction-like symptoms.
A: A 58-year-old woman presented with urinary obstruction and idiopathic sphincter overactivity and transurethral resection of bladder neck was performed with satisfactory results; B: The bladder transitional epithelium had entered the process of metaplasia, and Brunn nest was forming; C: A Brunn’s nest was evident and cavity was in the nest core.
Figure 24 Extra or intra-lower urinary tract symptoms and urodynamic findings in some cases precede pathological abnormality.
This phenomenon makes us be convinced of the present medical state. A: A 60-year-old male patient complaining of poor-weak flow and nocturia was proved as having detrusor underactivity (DUA) and low compliance, not responding to TURP, and was proved as having multiple system atrophy 2 years after the first consultation; B: A 52-year-old male patient having received bilateral nephrostomy because of hydronephrosis, was proved as having DUA and low compliance. He could void by efficient sphincter relaxation. However, no abnormal image sign was found at time of consultation.
- Citation: Qu CY, Xu DF. Comprehensive urodynamics: Being devoted to clinical urologic practice. World J Clin Urol 2014; 3(2): 96-112
- URL: https://www.wjgnet.com/2219-2816/full/v3/i2/96.htm
- DOI: https://dx.doi.org/10.5410/wjcu.v3.i2.96