Published online Nov 8, 2017. doi: 10.5409/wjcp.v6.i4.176
Peer-review started: February 12, 2017
First decision: June 27, 2017
Revised: July 7, 2017
Accepted: September 12, 2017
Article in press: September 12, 2017
Published online: November 8, 2017
Processing time: 277 Days and 23 Hours
Infantile pyknocytosis (IP) is a rare, self-limited neonatal haemolytic anaemia that may require multiple blood transfusions. Only a little more than 50 cases have been reported in the medical literature, and the great majority of them concerns term infants. The etiology of IP is not well understood; most likely it results from a transient extra-corpuscular factor, whose nature is unknown, transmitted from mother to child or, alternatively, from a deficiency of an anti-oxidative agent. We report the case of two preterm twins, one of which suffered from IP and developed severe anaemia at age 2 wk, while the other was unaffected. Although no specific agent was identified as the cause of anaemia and IP, we speculate that the transmission of an agent from mother to child was unlikely, as only twin one suffered from IP. Smelly greenish diarrhoea occurred just before the presentation of IP, suggesting that the same agent led to both the diarrhoea and the oxidative injury. Because IP may remain underdiagnosed, it should be considered in cases of early unexplained severe hemolytic anemia.
Core tip: This manuscript describes the first case of infantile pyknocytosis affecting only one of the twins, and contributes to understand the etiology of infantile pyknocytosis.
- Citation: Berardi A, Balestri E, Bonacorsi G, Chiossi C, Palazzi G, Spaggiari E, Ferrari F. Neonatal pyknocytosis in a preterm dizygotic twin. World J Clin Pediatr 2017; 6(4): 176-179
- URL: https://www.wjgnet.com/2219-2808/full/v6/i4/176.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v6.i4.176
Premature neonates commonly experience a fall in haemoglobin concentration. This has been termed “physiologic” anaemia of prematurity, since it is commonly not associated with any abnormalities in the red blood cells (RBCs). Repeated blood sampling and many diseases of prematurity can worsen this “physiologic” anaemia. However, more rare underlying diseases may mimic anaemia of prematurity or increase its severity.
Infantile pyknocytosis (IP) was first described by Tuffy et al[1] and is characterized by a self-limited neonatal haemolytic anaemia, which may require multiple blood transfusions. The aetiology of IP is unclear. Pyknocytes most likely result from a transient extra-corpuscular factor, whose nature is unknown[2]. An exogenous oxidative agent transmitted from mother to child or a deficiency of an anti-oxidative agent has been hypothesized[3].
We report the case of two Caucasian female preterm twins, one of whom suffered from IP and developed severe anaemia at age 2 wk. We discuss factors possibly associated with IP.
A dizygotic twin pregnancy resulted from an in vitro fertilization-embryo transfer. There was no familial history of unexplained transient neonatal anaemia.
Preterm labour occurred at 32 wk’ gestation, and an emergency caesarean section was required due to breech presentation.
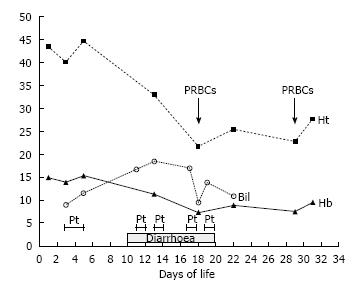
Twin 1 (first born). The Apgar score was 8 and 9 at the 1st and 5th min respectively, birth weight was 1735 g, length was 39 cm and cranial circumference was 25 cm. At birth, the red blood cell count and haemoglobin levels were normal (Figure 1). On day three the neonate suffered from jaundice and required phototherapy. The clinical course was uneventful until day 10, when stools became smelly and the baby required further phototherapy. The fecal occult blood test was positive.
On day 17 she was referred to our neonatal intensive care unit because of jaundice, foul-smelling greenish diarrhoea and worsening anaemia, which required a packed RBC transfusion.
The reticulocyte count was 169 per milliliter. Liver and renal function tests were normal. A direct antiglobulin test and search for irregular agglutinins were negative; haemoglobin electrophoresis as well as glucose-6-phosphate dehydrogenase (G6PD) and pyruvate kinase activity were normal, while lactate dehydrogenase was mildly abnormal (518 U/L). Bacterial cultures were sterile; detailed viral investigations yielded normal results.
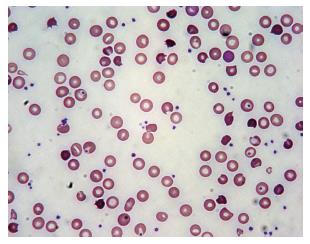
A peripheral blood smear demonstrated high rates (> 25%) of irregularly contracted, bite, and densely stained RBCs (Figure 2). The morphological changes in the RBCs accompanied with normal enzyme activity led us to suspect IP.
The jaundice worsened further on day 19, and additional phototherapy was administered. A further packed RBC transfusion was given on day 28. Subsequently the infant recovered spontaneously, and no further transfusions were given.
At age 5 mo both the haemoglobin level and RBC morphology were normal. G6PD test yielded normal result, confirming overall the initial diagnosis of IP. Twin 2 (second born). The Apgar score was 8 and 9 at the 1st and 5th min respectively.
The birth weight was 1760 g, the length 45 cm and cranial circumference 30 cm. The newborn had mild jaundice (maximum bilirubin levels 90.4 mg/L) on day five. Thereafter her clinical course was uneventful and she never suffered from anaemia. The haemoglobin level was 135 g/L on day 25.
Pyknocytes are small, irregular, distorted erythrocytes, which are densely stained in a peripheral blood smear. A low percentage of pyknocytes is commonly found in healthy full-term neonates (from 0.3% to 1.9%) and preterm neonates (from 0.3% to 5.6%) during the first weeks of life[1].
IP is a transient but often severe neonatal haemolytic anaemia associated with an accentuation of the physiologic presence of pyknocytes. Factors that increase oxidative stress may damage erythrocyte membranes, resulting in the formation of pyknocytes[3]. Since IP was first described, only a little more than 50 cases have been reported in the literature and the great majority of IP cases concern term infants[4]. The rarity of the disease as well as the lack of awareness about this cause of neonatal anaemia may lead to an underestimation.
IP may account for approximately 10% of cases of unexplained neonatal haemolytic anaemia[3]. Most cases present during the first days of life, with neonatal jaundice as the first manifestation; approximately 70% of affected infants develop severe anaemia from the second to the fourth week. Of life, commonly requiring one or more packed RBC transfusions[1,3]. Anaemia resolves spontaneously by the age of 4 to 6 mo[5].
The aetiology of IP is unclear. A transient extra-corpuscolar factor damaging the erythrocyte membrane, rather than an intrinsic factor, has been implicated in the pathogenesis of the disease. Indeed, flow cytometric analysis has shown that morphological changes do not affect reticulocytes, suggesting that erythropoietin treatment could prevent severe anemia[3,6]. Furthermore, among the seven cases of pyknocytosis reported by Ackerman, two showed the same morphologic abnormalities even after exchange transfusion, suggesting that erythrocytes of donor origin may also be affected[2]. There are only 2 reports of IP in twins; in all reported cases both twins were affected[7,8].
Pyknocytes most likely result from a transient extra-corpuscular factor, whose nature is unknown. Causes such as an exogenous oxidative agent or a deficiency of an anti-oxidative agent have been hypothesized[3].
In the current case report, only twin one suffered from IP. Therefore the transmission of an oxidative agent from mother to child, as well as a familial susceptibility or a hereditary factor[8,9] seem unlikely. Even if no specific agent was identified as the cause of the severe anaemia, the occurrence of smelly greenish diarrhoea was just before a decrease in haemoglobin and a rise in bilirubin levels, suggesting that the same cause, most likely an exogenous agent (perhaps infectious), and acquired after birth, led to both the diarrhea and the oxidative injury. Preterm birth possibly contributed to worsening the IP, as premature infants are more susceptible to oxidative stresses[9].
In conclusion, this is first case of IP affecting only one of the twins. The most likely cause of IP was an exogenous oxidative agent associated with diarrhoea and not transmitted from mother to child.
A preterm female twin presented with recurrent jaundice and severe hemolytic anemia at age 2 wk.
The diagnosis was based on jaundice and hemolytic anemia.
Common causes of jaundice and hemolytic anemia were excluded.
Liver, renal tests, viral and bacterial cultures were normal.
A peripheral blood smear demonstrated high rates (> 25%) of irregularly contracted, bite, and densely stained red blood cells (supporting the diagnosis of pyknocytosis).
The newborn underwent blood transfusions and phototherapy.
Infantile pycnocytosis is a transient but often severe neonatal haemolytic anaemia associated with an accentuation of the physiologic presence of pyknocytes.
Infantile pyknocytosis is a rare, self-limited neonatal haemolytic anaemia characterized by high rates of pyknocytes (small, irregular, distorted, densely stained erythrocytes).
Infantile pycnocytosis may remain underdiagnosed; it should be considered in cases of early unexplained severe hemolytic anemia.
The submitted paper by Alberto Berard et al, titled ″Neonatal pyknocytosis in a preterm dizygotic twin″, is very interesting, well structured, with clear presentation.
Manuscript source: Invited manuscript
Specialty type: Pediatrics
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Ivanovski PI S- Editor: Cui LJ L- Editor: A E- Editor: Lu YJ
| 1. | Tuffy P, Brown AK, Zuelzer WW. Infantile pyknocytosis; a common erythrocyte abnormality of the first trimester. AMA J Dis Child. 1959;98:227-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 50] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Ackerman BD. Infantile pyknocytosis in Mexican-American infants. Am J Dis Child. 1969;117:417-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Eyssette-Guerreau S, Bader-Meunier B, Garcon L, Guitton C, Cynober T. Infantile pyknocytosis: a cause of haemolytic anaemia of the newborn. Br J Haematol. 2006;133:439-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Kraus D, Yacobovich J, Hoffer V, Scheuerman O, Tamary H, Garty BZ. Infantile pyknocytosis: a rare form of neonatal anemia. Isr Med Assoc J. 2010;12:188-189. [PubMed] |
| 5. | Dabbous IA, El Bahlawan L. Infantile pyknocytosis: a forgotten or a dead diagnosis? J Pediatr Hematol Oncol. 2002;24:507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Amendola G, Di Concilio R, D’Urzo G, Danise P, Parisi G, della Ragione F, Rossi F, Nobili B, Perrotta S. Erythropoietin treatment can prevent blood transfusion in infantile pyknocytosis. Br J Haematol. 2008;143:593-595. [PubMed] |
| 7. | Lovric VA. Infantile pyknocytosis occurring in dissimilar twins. Med J Aust. 1960;47:579-580. [PubMed] |
| 8. | El Nabouch M, Rakotoharinandrasana I, Ndayikeza A, Picard V, Kayemba-Kay’s S. Infantile pyknocytosis, a rare cause of hemolytic anemia in newborns: report of two cases in twin girls and literature overview. Clin Case Rep. 2015;3:535-538. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Thibeault DW. The precarious antioxidant defenses of the preterm infant. Am J Perinatol. 2000;17:167-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 90] [Article Influence: 3.8] [Reference Citation Analysis (0)] |