Published online May 8, 2016. doi: 10.5409/wjcp.v5.i2.223
Peer-review started: January 30, 2016
First decision: February 29, 2016
Revised: March 4, 2016
Accepted: March 24, 2016
Article in press: March 25, 2016
Published online: May 8, 2016
Processing time: 94 Days and 1.4 Hours
AIM: To investigate the diagnostic and therapeutic assessment in children with adenomyomatosis of the gallbladder (AMG).
METHODS: AMG is a degenerative disease characterized by a proliferation of the mucosal epithelium which deeply invaginates and extends into the thickened muscular layer of the gallbladder, causing intramural diverticula. Although AMG is found in up to 5% of cholecystectomy specimens in adult populations, this condition in childhood is extremely uncommon. Authors provide a detailed systematic review of the pediatric literature according to PRISMA guidelines, focusing on diagnostic and therapeutic assessment. An additional case of AMG is also presented.
RESULTS: Five studies were finally enclosed, encompassing 5 children with AMG. Analysis was extended to our additional 11-year-old patient, who presented diffuse AMG and pancreatic acinar metaplasia of the gallbladder mucosa and was successfully managed with laparoscopic cholecystectomy. Mean age at presentation was 7.2 years. Unspecific abdominal pain was the commonest symptom. Abdominal ultrasound was performed on all patients, with a diagnostic accuracy of 100%. Five patients underwent cholecystectomy, and at follow-up were asymptomatic. In the remaining patient, completely asymptomatic at diagnosis, a conservative approach with monthly monitoring via ultrasonography was undertaken.
CONCLUSION: Considering the remote but possible degeneration leading to cancer and the feasibility of laparoscopic cholecystectomy even in small children, evidence suggests that elective laparoscopic cholecystectomy represent the treatment of choice. Pre-operative evaluation of the extrahepatic biliary tree anatomy with cholangio-MRI is strongly recommended.
Core tip: Adenomyomatosis of the gallbladder (AMG) in childhood is an extremely rare condition, with only few cases reported so far. We provided a detailed systematic review on diagnostic and therapeutic assessment of children with AMG.
- Citation: Parolini F, Indolfi G, Magne MG, Salemme M, Cheli M, Boroni G, Alberti D. Adenomyomatosis of the gallbladder in childhood: A systematic review of the literature and an additional case report. World J Clin Pediatr 2016; 5(2): 223-227
- URL: https://www.wjgnet.com/2219-2808/full/v5/i2/223.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v5.i2.223
Adenomyomatosis of the gallbladder (AMG) is a degenerative and acquired disease characterized by a localized or diffuse proliferation of the mucosal epithelium which deeply invaginates and extends into the thickened muscular layer of the gallbladder[1-3]. Although AMG is found in up to 5% of cholecystectomy specimens in adult populations, this condition in childhood is extremely rare, with only few cases reported so far. Clinical presentation of AMG in childhood is non-specific, with most patients complaining of abdominal pain. The diagnosis is generally based on imaging and the suspicion of AMG is usually raised by ultrasounds (US). Focusing on diagnostic and therapeutic assessment, a detailed systematic review of AMG in child populations is also provided. We present an additional case of diffuse AMG and pancreatic acinar metaplasia (PAM) of the gallbladder mucosa in an 11-year-old boy, successfully managed with laparoscopic cholecystectomy.
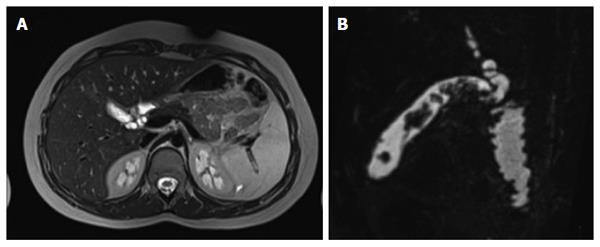
An 11-year-old boy was referred to our Emergnecy department with a one-year history of sporadic post-prandial abdominal pain, non-bilious vomiting and nausea. HCV-related hepatitis and pancreatic adenocarcinoma occurred respectively in the child’s father and grandfather. Physical examination upon admission was unremarkable. Blood tests only showed augmentation (2 ×n) of seric gamma-glutamyl transferase (GGT). Abdominal US revealed diffuse thickening of the gallbladder, with multiple anechogenic nodular areas mainly localized in the fundus and in the body, highly suspected for adenomyomatosis. Magnetic resonance imaging (MRI) confirmed the thickening of the gallbladder and the presence of multiple endoluminal irregular filling-defects (the largest over 13 mm) with enhancement using a contrast dye. A tortuous cystic duct with an increased calibre (5 mm) was also evident (Figure 1). Standard laparoscopic cholecystectomy was programmed. Whilst waiting for surgery, ursodeoxycholic acid was administered orally at a dosage of 15 mg/kg per day. Full informant consent was obtained from the child’s parents before all stages of the procedures. The laparoscopic cholecystectomy procedure went smoothly. The excised gallbladder measured 7 cm × 2 cm. Pathological examination confirmed the diagnosis of chronic hyperplastic cholecystitis with diffuse adenomyomatosis and foci of PAM (Figure 2). The postoperative recovery was uneventful. At a 28-mo follow-up the child is doing well and is completely asymptomatic.
This systematic review was performed according to preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines[4]. The PubMed database was searched for original studies on AMG published since 1990, involving patients younger than 18 years of age. Eligible study designs were case report, case series and review. We omitted reports in which abstracts indicated that they were on adult population (> 18 years) and they not reported the methods of diagnosis and treatment. We then evaluated the full text of the selecte articles. The date of the last search was January 2016. For each study, data were extracted for sex and age at presentation, clinical presentation, diagnostic assessment, treatment, pathological examination and outcome.
The PubMed search yielded 5 potentially relevant studies[1-3,5,6], involving a total of 5 children with AMG (Table 1). All selected studies were case reports (class of evidence III and rating scale of evidence E)[4].
| Ref. | Age | Sex | Clinical presentation | US findings | Additional imaging | Type | Treatment |
| Alberti et al[1] | 5 yr | Male | Unspecific abdominal pain | Echogenic nodule next to the neck of gallbladder | Technetium 99m HIDA, PTC | Localized | Laparoscopic cholecystectomy |
| Cetinkursun et al[2] | 6 yr | Male | Acute abdominal pain, fever and bilious vomiting | Small and multiseptated gallbladder with thickened wall | MRI | Diffuse | Open cholecystectomy |
| Zani et al[6] | 5 yr | Male | Unspecific abdominal pain | Multiseptated gallbladder within the lumen | NA | Segmental (annular type) | Open cholecystectomy |
| Akçam et al[3] | 9 yr | Female | Unspecific abdominal pain | Thickening of the wall of the gallbladder with echogenic areas parallel to the wall of gallbladder | MRI | Diffuse (honeycomb) | Open cholecystectomy |
| Zarate et al[5] | 4 mo | Female | Incidental finding in Beckwith-Wiedemanns | Echoic foci within gallbladder wall | None | Localized | Observation |
| Our case | 11 yr | Male | Acute abdominal pain, nausea, non-bilious vomiting | Thickening of the wall, multiple polypoid formations | MRI | Diffuse | Laparoscopic cholecystectomy |
Analysis was extended to our additional patient. The condition was more common in boys (67%), with a mean and median age at presentation of 7.2 years (SD + 3.1) and 6.0 years (range 4 mo-11 years), respectively (Table 1). Unspecific abdominal pain was the commonest symptom, occurring in 3 patients, while acute abdominal pain was reported in 2 patients. The remaining patient was an asymptomatic 4-mo-old girl with Beckwith-Wiedemann syndrome in whom AMG was accidentally discovered during abdominal US[5]. Besides abdominal pain, vomiting was present in 2 out of the 6 patients. Abdominal US was performed on all patients, with a diagnostic accuracy of 100%. None of the patients of the series presented gallstones or biliary sludge. Additional diagnostic examinations were performed on 4 patients, including MRI (3 patients), percutaneous trans-hepatic cholecystocholangiograhy (PTC) (1 patient), and Technetium 99m HIDA scan in (1 patient). Five out of the six patients underwent cholecystectomy (open procedure in 3 and laparoscopic in 2). AMG was diffuse in three patients, localized in 2 and segmental (annular) in the remaining child. At follow-up, all patients who underwent surgery were asymptomatic. In the remaining patient, completely asymptomatic at diagnosis, a conservative approach with monthly monitoring via ultrasonography was undertaken.
Hyperplastic cholecystosis includes two types of mucosal abnormalities of the gallbladder which are usually clinical accidental findings at the time of a cholecystectomy: Cholesterolosis and adenomyomatosis[1-3]. Cholesterolosis is defined by mucosal villous hyperplasia, accumulation of cholesterol within epithelial layer; AMG is a hyperplastic lesion characterized by thickening of the muscle wall, overgrowth of the mucosa, and multiple intramural mucosal diverticula[7]. Although AMG is found in up to 5% of cholecystectomy specimens in adult populations[8], its occurrence in pediatric setting is extremely uncommon, and only five cases have been previously reported. The widespread and early use of US in pediatrics, either for recurrent or chronic abdominal pain or for other reasons, most probably will lead to emergent diagnosis, reinforcing the theory that implies that most patients with AMG might not be diagnosed until adulthood due to the absence or presence of only unspecific symptoms prior to the development of gallstones and/or cholecystitis[1-3].
The etiology of AMG still remains unclear: Co-morbidities that increase the formation of gallstones, such as congenital abnormalities of the biliary tract, hemolytic disease, total parenteral nutrition, chronic inflammatory bowel disease and obesity have been reported in adult AMG patients[1-3,8]. However, these conditions were not observed in this pediatric series. Nowadays AMG is considered a degenerative disease rather than a congenital malformation[1-3,8]. The first noticeable stage of the disease is most probably related to increased gallbladder intraluminal pressure caused by abnormalities of muscle contraction or to excessive mural absorption of bile, leading to hyperproliferation of the epithelial cells of the gallbladder mucosa and to hyperplasia of the smooth muscle[9]. As a consequence of this excessive proliferation, the epithelia invaginates into the hypertrophic muscular layer of the gallbladder forming intramural diverticula known as Rokitanski-Ashoff sinuses, that may fill with bile, biliary sludge and/or gallstone[9]. This condition is morphologically classified into three types: Generalized (or diffuse), localized (usually a single nodule in the fundus that projects into the lumen showing a polyp image at US, called “adenomyoma”) and segmental (annular type with an “hourglass” configuration of the gallbladder, due to the transverse congenital septum in the body of gallbladder)[1-4,8].
In the past, attention has been drawn to the potential malignant degeneration of AMG, as different adult series have described an incidence of up to 6.4% of gallbladder cancer developing in patients with segmental AMG[2,10,11]. Nevertheless, the question whether AMG should be considered a pre-malignant lesion is still unanswered, and the risk of gallbladder cancer in patients with adenomyomatosis has not been clearly understood[3,8,11]. Also, the presence of PAM in the gallbladder, as observed in our patient, should be considered as an accidental finding unrelated to clinical or histological abnormalities, as PAM is commonly reported in other sites (gastroesophageal junction, stomach) with no clinical significance[12].
Clinical signs and symptoms, when present, are similar to those of chronic gallbladder disease, which in childhood usually appear with a variety of atypical symptoms differing from the typical right upper quadrant pain[1-3,5,6,8,13]. Interestingly, if AMG in adults is associated with gallstones in up to 91.7% of the cases, gallstones or biliary sludge were not reported in this series[11]. Radiological diagnosis of AMG is easy and US is considered the most sensitive and specific imaging method for diagnosis[1]. AMG US findings include: Rokitansky-Aschoff sinuses, which can be found either as anechogenic (bile filled) or as echogenic foci (biliary sludge or gallstone filled), gallbladder wall thickening, US findings of ring down artifacts (Comet Tail) as a result of reverberation between the sinuses themselves, intrasinus papillary projections and polypoidal projections of at least 10 mm length[1,6]. Due to variation in morphology, adenomyomatosis can appear as diffuse gallbladder wall thickening or as focal lesions, simulating gallbladder carcinoma[2]. Additional diagnostic assessment with cholangio-RMN should be performed before surgery in order to obtain a detailed map of the extrahepatic biliary tract, as major variations and anomalies of the biliary tree have been found in up to 18% of cases and these anomalies must be identified to prevent severe lesions to the common bile duct[14]. In particular, MRI T2-weighted sequences are reported to be superior to other sequences in order to visualize the Rokitansky-Aschoff sinuses[8,9]. Diffuse-type AMG typically shows an early mucosal enhancement with subsequent serosal enhancement. On the contrary, localized AMG exhibits homogeneous enhancement, showing continuity with the surrounding gallbladder epithelium[8,9]. Furthermore, cholangio-MRI can detect stones into the choledocus[1,2,6].
The evidence regarding current management of AMG in children is poor. Whilst, in case of symptomatic patients, the need for surgery is obvious, management of asymptomatic children is still debated[5]. Considering the remote but possible degeneration leading to cancer and the feasibility of laparoscopic cholecystectomy even in small children[1,11], conservative treatment and ultrasonographic monitoring should be reserved only to patient subsets with clear contraindications to surgery. In contrast, evidence suggest that elective laparoscopic cholecystectomy represents the treatment of choice for children as well as adults. Pre-operative evaluation of the extrahepatic biliary tree anatomy with cholangio-MRI is strongly recommended.
Adenomyomatosis of the gallbladder (AMG) is a degenerative disease characterized by a proliferation of the mucosal epithelium which deeply invaginates and extends into the thickened muscular layer of the gallbladder, causing intramural diverticula. Although AMG is found in up to 5% of cholecystectomy specimens in adult populations, this condition in childhood is extremely rare, with only few cases reported so far.
Although AMG is found in up to 5% of cholecystectomy specimens in adult populations, this condition in childhood is extremely rare, with only few cases reported so far.
Authors provide a detailed systematic review of the pediatric literature on AMG. An additional case of AMG is also presented.
This systematical review focus on diagnostic and therapeutic assessment of AMG in childhood.
Hyperplastic cholecystosis includes two types of mucosal abnormalities of the gallbladder which are usually clinical accidental findings at the time of a cholecystectomy: Cholesterolosis and adenomyomatosis. Cholesterolosis is characterized by mucosal villous hyperplasia with accumulation of cholesterol esters within epithelial macrophages, while AMG is a hyperplastic lesion characterized by overgrowth of the mucosa, thickening of the muscle wall and intramural mucosal diverticula formation.
AMG in children is a very rare disease. This paper introduced a case report and a systemic review, which had a clinical guading influence.
P- Reviewer: Lee KG, Shu JA, Xu Z S- Editor: Ji FF L- Editor: A E- Editor: Wang CH
| 1. | Alberti D, Callea F, Camoni G, Falchetti D, Rigamonti W, Caccia G. Adenomyomatosis of the gallbladder in childhood. J Pediatr Surg. 1998;33:1411-1412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Cetinkursun S, Surer I, Deveci S, Demirbag S, Saglam M, Atabek C, Ozturk H. Adenomyomatosis of the gallbladder in a child. Dig Dis Sci. 2003;48:733-736. [PubMed] |
| 3. | Akçam M, Buyukyavuz I, Ciriş M, Eriş N. Adenomyomatosis of the gallbladder resembling honeycomb in a child. Eur J Pediatr. 2008;167:1079-1081. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9207] [Cited by in RCA: 8050] [Article Influence: 536.7] [Reference Citation Analysis (2)] |
| 5. | Zarate YA, Bosanko KA, Jarasvaraparn C, Vengoechea J, McDonough EM. Description of the first case of adenomyomatosis of the gallbladder in an infant. Case Rep Pediatr. 2014;2014:248369. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Zani A, Pacilli M, Conforti A, Casati A, Bosco S, Cozzi DA. Adenomyomatosis of the gallbladder in childhood: report of a case and review of the literature. Pediatr Dev Pathol. 2005;8:577-580. [PubMed] |
| 7. | Owen CC, Bilhartz LE. Gallbladder polyps, cholesterolosis, adenomyomatosis, and acute acalculous cholecystitis. Semin Gastrointest Dis. 2003;14:178-188. [PubMed] |
| 8. | Yoshimitsu K, Honda H, Aibe H, Shinozaki K, Kuroiwa T, Irie H, Asayama Y, Masuda K. Radiologic diagnosis of adenomyomatosis of the gallbladder: comparative study among MRI, helical CT, and transabdominal US. J Comput Assist Tomogr. 2001;25:843-850. [PubMed] |
| 9. | Pellino G, Sciaudone G, Candilio G, Perna G, Santoriello A, Canonico S, Selvaggi F. Stepwise approach and surgery for gallbladder adenomyomatosis: a mini-review. Hepatobiliary Pancreat Dis Int. 2013;12:136-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Mariani PJ, Hsue A. Adenomyomatosis of the gallbladder: the “good omen” comet. J Emerg Med. 2011;40:415-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Aldridge MC, Gruffaz F, Castaing D, Bismuth H. Adenomyomatosis of the gallbladder. A premalignant lesion? Surgery. 1991;109:107-110. [PubMed] |
| 12. | Schneider NI, Plieschnegger W, Geppert M, Wigginghaus B, Höss GM, Eherer A, Wolf EM, Rehak P, Vieth M, Langner C. Pancreatic acinar cells--a normal finding at the gastroesophageal junction? Data from a prospective Central European multicenter study. Virchows Arch. 2013;463:643-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Svensson J, Makin E. Gallstone disease in children. Semin Pediatr Surg. 2012;21:255-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 51] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 14. | Choi JW, Kim TK, Kim KW, Kim AY, Kim PN, Ha HK, Lee MG. Anatomic variation in intrahepatic bile ducts: an analysis of intraoperative cholangiograms in 300 consecutive donors for living donor liver transplantation. Korean J Radiol. 2003;4:85-90. [PubMed] |