Published online May 8, 2014. doi: 10.5409/wjcp.v3.i2.14
Revised: February 21, 2014
Accepted: March 13, 2014
Published online: May 8, 2014
Processing time: 154 Days and 9.8 Hours
AIM: To determine the utility of X-ray in identifying non-metallic foreign body (FB) and assess inter-radiologist agreement in identifying non-metal FB.
METHODS: Focus groups of nurses, fellows, and attending physicians were conducted to determine commonly ingested objects suitable for inclusion. Twelve potentially ingested objects (clay, plastic bead, crayon, plastic ring, plastic army figure, glass bead, paperclip, drywall anchor, eraser, Lego™, plastic triangle toy, and barrette) were embedded in a gelatin slab placed on top of a water-equivalent phantom to simulate density of a child’s abdomen. The items were selected due to wide availability and appropriate size for accidental pediatric ingestion. Plain radiography of the embedded FBs was obtained. Five experienced radiologists blinded to number and types of objects were asked to identify the FBs. The radiologist was first asked to count the number of items that were visible then to identify the shape of each item and describe it to a study investigator who recorded all responses. Overall inter-rater reliability was analyzed using percent agreement and κ coefficient. We calculated P value to assess the probability of error involved in accepting the κ value.
RESULTS: Fourteen objects were radiographed including 12 original objects and 2 duplicates. The model’s validity was supported by clear identification of a radiolucent paperclip as a positive control, and lack of identification of plastic beads (negative control) despite repeated inclusion. Each radiologist identified 7-9 of the 14 objects (mean 8, 67%). Six unique objects (50%) were identified by all radiologists and four unique objects (33%) were not identified by any radiologist (plastic bead, Lego™, plastic triangle toy, and barrette). Identification of objects that were not present, false-positives, occurred 1-2 times per radiologist (mean 1.4). An additional 17% of unique objects were identified by less than half of the radiologists. Agreement between radiologists was considered almost perfect (kappa 0.86 ± 0.08, P < 0.0001).
CONCLUSION: We demonstrate potential non-identification of commonly ingested non-metal FBs in children. A registry for radiographic visibility of ingested objects should be created to improve clinical decision-making.
Core tip: Foreign body (FB) ingestion is very common in children and results in numerous visits for acute medical evaluation. X-ray identification of FB location and retention is used to guide management decisions including performance of additional imaging studies or FB retrieval. We investigated whether non-metal FB were visible on X-ray using a radiographic phantom. Our results show that expert radiologists are potentially unable to identify ingested non-metal foreign bodies. Creation of a database to catalogue X-ray characteristics of ingested non-metal objects would enable clinicians to improve quality of care by reduction of false-negative tests and prevention of unnecessary procedures.
- Citation: Saps M, Rosen JM, Ecanow J. X-ray detection of ingested non-metallic foreign bodies. World J Clin Pediatr 2014; 3(2): 14-18
- URL: https://www.wjgnet.com/2219-2808/full/v3/i2/14.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v3.i2.14
Foreign body (FB) ingestion in children was reported to United States poison control approximately 100000 times in 2010[1]. In children, the ingestion of FB is frequently not witnessed[2]. Unwitnessed FB ingestion poses a diagnostic challenge with important therapeutic implications[3,4]. Children are often too young or frightened to provide a reliable history. Children can remain asymptomatic despite ingestion of a potentially harmful FB. Even in the asymptomatic child, retention of an ingested FB may necessitate removal depending on type, location, or size. To solve this diagnostic and therapeutic challenge, physicians usually obtain X-ray studies (XR)[5]. XR is instrumental in cases of metal objects, however its utility is limited in cases of non-metal objects of unknown visibility. Despite limitations, XR is widely recommended as an initial diagnostic tool due to disadvantages of other imaging techniques (magnetic resonance imaging, computed tomography, and ultrasound) including cost, radiation exposure, and expertise/equipment required for performance and interpretation.
Although button batteries[6] and magnets[7] appropriately receive attention in the media and scientific literature because of harmful, sometimes fatal, ingestions, other objects also present significant risks. Case reports identify ingested non-metal materials including a plastic toy[8], pencil[9], tape[10], bottle cap diaphragm[11], ballpoint pen[12,13], toothbrush[14], eel vertebrae[15], twig[16] and other unusual objects[17,18] that may not be readily identifiable with routine XR. Ingestion of plastic toys can lead to intestinal obstruction[19] or other toxic effects of chronic retention due to plastic constituents[20]. Intestinal perforation also may result from ingestion of non-metal objects[21,22].
Confronted with the uncertainty of a possible FB, providers cannot make an informed and efficient decision. The provider may opt to rely on an XR result that provides false reassurance and potentially leads to otherwise preventable morbidity. Alternatively, the practitioner may distrust XR results and perform unnecessary diagnostic tests (i.e., endoscopy) with increased risk to the child. Instruction of parents to screen or strain the child’s stools for FB passage is inconvenient and may raise parental and child anxiety.
Despite high frequency of FB ingestion and importance of diagnostic radiography in guiding therapy, there are only case reports describing ability of XR to detect specific non-metallic FBs. Increased understanding of XR utility in diagnosis of non-metallic FBs is an initial step to improve clinical care. We conducted a study assessing non-metallic FB identification by XR.
The primary aims of our descriptive study were to assess the ability of radiologists to detect non-metallic FBs through radiography and to determine the inter-rater agreement of detection. A secondary aim of our study was to create an easily reproducible model to assess visibility of ingested FB in children. Phantoms are frequently used for calibration and testing of imaging devices in radiology departments. For the purpose of this study we custom designed a water-equivalent phantom (WEP) to model the density of the child’s body. WEPs are composite materials that allow simulation and testing of radiographic techniques without human radiation exposure. To encase foreign bodies, a 2 cm thick gelatin-in-water mold was prepared by dissolving 28 g of gelatin in 1 quart of tap water (Knox Gelatin, Kraft Foods, Inc., Tarrytown, NY). The gelatin slab was placed on top of a standard WEP (Gammex Solid Water, Laco, Inc., Chesterland, OH) to create a composite (gelatin/WEP) phantom.
Twelve unique items, some with “choking hazard” warnings, and two copies of one item were encased in the gelatin slab (clay, plastic bead, crayon, plastic ring, plastic army figure, glass bead, paperclip, drywall anchor, eraser, Lego™, plastic triangle toy, and barrette). Potential items for inclusion were determined by conducting focus groups with nurses, gastroenterology fellows, and attending physicians. The items included were selected due to wide availability and appropriate size for accidental pediatric ingestion. Copies of one item, a plastic bead, were used to evaluate reliability of our model. A metallic paperclip was used as a positive control. The slab with encased objects was placed on an 18 cm thick WEP to create a 20 cm thick composite phantom representative of a 20 cm thick child. A single XR was obtained of the composite phantom with encased objects (Axiom Multix M, Siemens United States Corp., Washington, DC, United States, 70 kVP, 39 mAs, phototimer technique, table-top Bucky grid).
Five board certified radiologists, each with ten years or greater experience, and blinded to the number and identity of the items in the gelatin slab, were shown a single radiograph. The radiologist was first asked to count the number of items that were visible on the radiographic image. After recording the number of items identified, each radiologist was asked to identify the shape of each item and describe it to a study investigator who recorded all responses.
Overall inter-rater reliability was analyzed using percent agreement and κ coefficient. κ coefficient values < 0 indicate poor, 0-0.2 slight, 0.21-0.4 fair, 0.41-0.6 moderate, 0.61-0.8 substantial, and 0.81-1 almost perfect agreement, respectively. We calculated P value to assess the probability of error involved in accepting the κ value. This study was performed without the use of human or animal subjects.
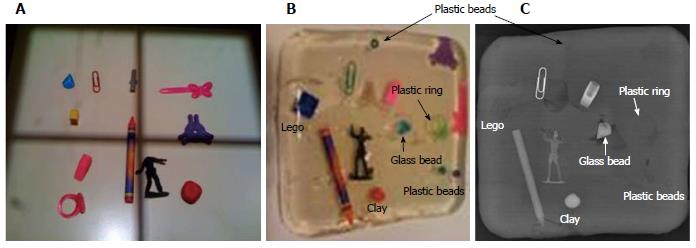
Fourteen objects had color photographs taken before and after embedding in gelatin, and plain X-ray taken after embedding (Figure 1). Each radiologist identified 7-9 of the 14 objects (mean 8, 67%). Six unique objects (50%) were identified by all radiologists and four unique objects (33%) were not identified by any radiologist (round plastic bead, Lego™, pink barrette, and purple triangle). Identification of objects that were not present, false-positives, occurred 1-2 times per radiologist (mean 1.4). An additional 17% of unique objects were identified by less than half of the radiologists. Agreement between radiologists was considered almost perfect (kappa 0.86 ± 0.08, P < 0.0001) (Table 1).
| No. | Rad 1 | Rad 2 | Rad 3 | Rad 4 | Rad 5 | Object |
| 1 | + | + | + | + | + | Army figure |
| 2 | + | + | + | + | + | Clay lump |
| 3 | + | + | + | + | + | Crayon |
| 4 | + | + | + | + | + | Eraser |
| 5 | + | + | + | + | + | Glass diamond bead |
| 6 | + | + | + | + | + | Paperclip |
| 7 | - | + | - | - | + | Ring |
| 8 | + | - | - | - | - | Drywall anchor |
| 9 | - | - | - | - | - | Lego |
| 10 | - | - | - | - | - | Pink barrette |
| 11 | - | - | - | - | - | Plastic bead |
| 12 | - | - | - | - | - | Plastic bead 2 |
| 13 | - | - | - | - | - | Plastic bead 3 |
| 14 | - | - | - | - | - | Triangle purple plastic |
| x | + | “Half violin” | ||||
| x | + | “Irregular elongated rectangle” | ||||
| x | + | “Irregular opacity” | ||||
| x | + | “Irregular opacity” | ||||
| x | + | “Linear lucency” | ||||
| x | + | “Irregular lucency” | ||||
| x | + | “Irregular opacity” |
This is the first published study assessing visibility of non-metallic objects using an inexpensive, simple, easily reproducible model that represents a child’s body density. Gelatin slabs have variable distribution of embedded air bubbles that may help simulate the presence of fat in the child’s body. The excellent agreement found in our study among experienced radiologists validates (face value) the model. If the accuracy and utility of our model is confirmed in larger studies, it could potentially be used to predict the visibility of FB in children. The fact that some objects could not be seen by any radiologist suggests that such an object may not be visible if ingested by children. More than half of the items were either not detected or detected inconsistently, raising the potential for unnecessary diagnostic XR or missed opportunity for intervention in patients. Toy ingestions represent almost 7% of all phone calls to poison control in children less than 5 years of age in the United States[1]. Some of the most popular toys used by children such as Legos™ could not be visualized by any radiologist. Regardless of whether a given ingested object presents significant risk, parental (and primary care provider) anxiety often leads to repeated patient evaluation.
The results of our study underscore the need for an easily accessible FB registry denoting XR visibility. The creation of such a registry could be instrumental in helping radiologists and emergency room physicians in diagnosis and management. Enhancing confidence in diagnosing the presence of an ingested FB could facilitate the physician’s medical plan and alleviate parental anxiety. The European Registry on Upper Aerodigestive Tract Foreign Body Injuries in Children (Susy Safe)[23] serves as a successful model with data input at the point of care by all member institutions. Susy Safe data has demonstrated the need for ongoing collection of information to identify modifiable risk factors in toy design[24] as well as the ongoing necessity of integrative preventative strategies[25,26]. Our proposed registry should be internet-accessible and include standardized data fields for radiographic characteristics of FB that are lacking in the Susy Safe registry.
Imaging modalities other than XR for detection and characterization of ingested foreign bodies are rarely used in clinical and research settings. Ultrasonographic techniques show promise and are radiation free[27], but they require a skilled technician at the point of care and specialized equipment. Other modalities including contrast XR, computed tomography[28], and magnetic resonance imaging (MRI) may be helpful in specific circumstances, but involve increased radiation exposure (except MRI), cost, and complexity.
Limitations of this study include the utilization of a model, rather than clinical data, and a small panel of objects subjected to radiographic identification. However, the use of a model simulating the child’s body helps circumvent the ethical considerations of obtaining repeated XR in children.
Our study demonstrates the potential inability to detect ingested non-metallic FBs in children using XR. It also shows that while agreement among radiologists is excellent, some objects are inconsistently or never detected. Some of the objects not detected are common, present in many households and easily accessible to children. We propose a model to assess the visibility of non-metallic FB by XR. Future studies including a larger pool of objects should be conducted to confirm our findings. The creation of an easily accessible FB database should be considered.
Foreign body (FB) ingestion in children is common. X-ray (XR) is a simple diagnostic test that may assist with identification and localization of ingested FB. However, it is not clear whether non-metal objects are radiopaque. This leads to significant difficulty in utilizing XR to guide treatment decisions.
The study proposes a simple, clinically relevant imaging model that could be used to predict FB visibility in children.
Despite high frequency of FB ingestion and importance of diagnostic radiography in guiding therapy, there are only case reports describing ability of XR to detect specific non-metallic FBs. The study assesses non-metallic FB identification by XR.
A similar model can be used at the point of care to predict XR visibility of an ingested foreign body. This could limit unnecessary procedures, or more rapidly and accurately indicate whether endoscopic or surgical retrieval is needed.
The authors studied the utility of XR in identifying non-metallic foreign bodies and inter-radiologist agreement in identifying non-metal foreign body using custom designed water equivalent phantoms, and concluded that the potential inability to detect ingested non-metallic foreign bodies in children using XR. This paper is well-written and has interesting and important findings.
P- Reviewers: Alessandro I, ChoiYH, Viswanatha B, Watanabe T S- Editor: Zhai HH L- Editor: A E- Editor: Wu HL
| 1. | Bronstein AC, Spyker DA, Cantilena LR, Green JL, Rumack BH, Dart RC. 2010 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 28th Annual Report. Clin Toxicol (Phila). 2011;49:910-941. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 298] [Cited by in RCA: 282] [Article Influence: 21.7] [Reference Citation Analysis (0)] |
| 2. | Louie JP, Alpern ER, Windreich RM. Witnessed and unwitnessed esophageal foreign bodies in children. Pediatr Emerg Care. 2005;21:582-585. [PubMed] |
| 3. | Wright CC, Closson FT. Updates in pediatric gastrointestinal foreign bodies. Pediatr Clin North Am. 2013;60:1221-1239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 57] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 4. | Chiu YH, Hou SK, Chen SC, How CK, Lam C, Kao WF, Yen DH, Huang MS. Diagnosis and endoscopic management of upper gastrointestinal foreign bodies. Am J Med Sci. 2012;343:192-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Kay M, Wyllie R. Pediatric foreign bodies and their management. Curr Gastroenterol Rep. 2005;7:212-218. [PubMed] |
| 6. | Takagaki K, Perito ER, Jose FA, Heyman MB. Gastric mucosal damage from ingestion of 3 button cell batteries. J Pediatr Gastroenterol Nutr. 2011;53:222-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Hussain SZ, Bousvaros A, Gilger M, Mamula P, Gupta S, Kramer R, Noel RA. Management of ingested magnets in children. J Pediatr Gastroenterol Nutr. 2012;55:239-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 122] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 8. | Agrawal V, Joshi MK, Jain BK, Gupta A. Plasticobezoar-another new entity for Rapunzel syndrome. Indian J Pediatr. 2009;76:229-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Counsilman CE, van Velzen MF. Subcutaneous emphysema after ingestion of a pencil. Arch Dis Child. 2011;96:147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Fujiwara T, Nishimoto S, Kawai K, Fukuda K, Okuyama H, Kakibuchi M. Exacerbation of oesophageal stenosis by accidental ingestion of tape. J Plast Surg Hand Surg. 2012;46:207-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Glover P, Westmoreland T, Roy R, Sawaya D, Giles H, Nowicki M. Esophageal diverticulum arising from a prolonged retained esophageal foreign body. J Pediatr Surg. 2013;48:e9-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Golffier C, Holguin F, Kobayashi A. Duodenal perforation because of swallowed ballpoint pen and its laparoscopic management: report of a case. J Pediatr Surg. 2009;44:634-636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Rameau A, Anand SM, Nguyen LH. Ballpoint pen ingestion in a 2-year-old child. Ear Nose Throat J. 2011;90:E20-E22. [PubMed] |
| 14. | Gowda D, Familua O, Sathyanarayana N. Toothbrush ingestion leading to laparotomy. Am Surg. 2010;76:E193-E194. [PubMed] |
| 15. | Hon KL, Chu WC, Sung JK. Retropharyngeal abscess in a young child due to ingestion of eel vertebrae. Pediatr Emerg Care. 2010;26:439-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Kappadath SK, Clarke MJ, Stormer E, Steven L, Jaffray B. Primary aortoenteric fistula due to a swallowed twig in a three-year-old child. Eur J Vasc Endovasc Surg. 2010;39:217-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Mahajan M, Gandhi V, Nagral A. An unusual cause of vomiting in a child. BMJ Case Rep. 2011;2011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 18. | Moon JS, Bliss D, Hunter CJ. An unusual case of small bowel obstruction in a child caused by ingestion of water-storing gel beads. J Pediatr Surg. 2012;47:E19-E22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | Zamora IJ, Vu LT, Larimer EL, Olutoye OO. Water-absorbing balls: a “growing” problem. Pediatrics. 2012;130:e1011-e1014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 37] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 20. | Ortmann LA, Jaeger MW, James LP, Schexnayder SM. Coma in a 20-month-old child from an ingestion of a toy containing 1,4-butanediol, a precursor of gamma-hydroxybutyrate. Pediatr Emerg Care. 2009;25:758-760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 21. | Ragazzi M, Delcò F, Rodoni-Cassis P, Brenna M, Lavanchy L, Bianchetti MG. Toothpick ingestion causing duodenal perforation. Pediatr Emerg Care. 2010;26:506-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Stringel G, Parker M, McCoy E. Vinyl glove ingestion in children: a word of caution. J Pediatr Surg. 2012;47:996-998. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Gregori D. The Susy Safe Project. A web-based registry of foreign bodies injuries in children. Int J Pediatr Otorhinolaryngol. 2006;70:1663-1664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | de Koning T, Foltran F, Gregori D. Fostering design for avoiding small parts in commonly used objects. Int J Pediatr Otorhinolaryngol. 2012;76 Suppl 1:S57-S60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 25. | Foltran F, Gregori D, Passàli D, Bellussi L, Caruso G, Passàli FM, Passàli GC. Toys in the upper aerodigestive tract: evidence on their risk as emerging from the ESFBI study. Auris Nasus Larynx. 2011;38:612-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 26. | Foltran F, Passali FM, Berchialla P, Gregori D, Pitkäranta A, Slapak I, Jakubíková J, Franchin L, Ballali S, Passali GC. Toys in the upper aerodigestive tract: new evidence on their risk as emerging from the Susy Safe Study. Int J Pediatr Otorhinolaryngol. 2012;76 Suppl 1:S61-S66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 27. | Piotto L, Gent R, Kirby CP, Morris LL. Preoperative use of ultrasonography to localize an ingested foreign body. Pediatr Radiol. 2009;39:299-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 28. | Luk WH, Fan WC, Chan RY, Chan SW, Tse KH, Chan JC. Foreign body ingestion: comparison of diagnostic accuracy of computed tomography versus endoscopy. J Laryngol Otol. 2009;123:535-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |