Published online Mar 9, 2024. doi: 10.5409/wjcp.v13.i1.86693
Peer-review started: August 26, 2023
First decision: December 11, 2023
Revised: January 2, 2024
Accepted: February 2, 2024
Article in press: February 2, 2024
Published online: March 9, 2024
Processing time: 194 Days and 1.2 Hours
Vitamin D deficiency is a common problem in exclusively breastfed infants, with supplementation recommended by various international medical organizations. However, in Thailand, no advice for routine vitamin D supplementation is available. Thus, this study investigated the prevalence of vitamin D deficiency and its associated factors in exclusively breastfed infants in Bangkok, Thailand.
To investigated the prevalence of vitamin D deficiency and its associated factors in exclusively breastfed infants in Bangkok, Thailand.
This descriptive observational cross-sectional study assessed 109 4-month-old infants at Charoenkrung Pracharak Hospital from May 2020 to April 2021. The 25-OH vitamin D level of the infants was measured using an electrochemiluminescence binding assay. Vitamin D deficiency was defined as 25-OH level < 20 ng/mL, with vitamin D insufficiency 20-30 ng/mL. The sun index and maternal vitamin D supplementation data were collected and analyzed using the inde
The prevalences of vitamin D deficiency and vitamin D insufficiency were 35.78% and 33.03%, respectively with mean serum 25-OH vitamin D levels in these two groups 14.37 ± 3.36 and 24.44 ± 3.29 ng/mL. Multivariate logistic regression showed that the main factors associated with vitamin D status were maternal vitamin D supplementation and birth weight, with crude odds ratios 0.26 (0.08–0.82) and 0.08 (0.01–0.45), respectively. The sun index showed no correlation with the 25-OH vitamin D level in exclusively breastfed infants (r = −0.002, P = 0.984).
Two-thirds of healthy exclusively breastfed infants had hypovitaminosis D. Vitamin D supplementation prevented this condition and was recommended for both lactating women and their babies.
Core Tip: Vitamin D deficiency is a common problem in exclusively breastfed infants, so vitamin D supplementation was recommended by various international organizations but it has not been established in Thailand because of the limitation of study. This study showed high prevalence of vitamin D deficiency at 35.78% in exclusively breastfed infants at Charoenkrung Pracharak Hospital and its main associated factor was maternal vitamin D supplementation while the sun index in infants showed no correlation with the 25-OH vitamin D level. So, routine Vitamin D supplementation was recommended for both lactating women and their babies to prevent vitamin D deficiency.
- Citation: Suksantilerd S, Thawatchai R, Rungrojjananon N. Prevalence of vitamin D deficiency in exclusively breastfed infants at Charoenkrung Pracharak Hospital. World J Clin Pediatr 2024; 13(1): 86693
- URL: https://www.wjgnet.com/2219-2808/full/v13/i1/86693.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v13.i1.86693
Vitamin D3 is produced in human skin, whereas vitamin D2 is produced in plants and fungi from ergosterol[1]. This is subsequently metabolized by 25-hydroxylase in the liver and converted to 25-OH vitamin D, its storage form. 25-OH vitamin D is then catalyzed by 1-hydroxylase in the kidneys and converted to its hormonally active form, 1,25-dihydroxyvitamin D[2]. 25-OH vitamin D and other metabolites play a crucial role in maintaining calcium and phosphate homeostasis. Active vitamin D stimulates calcium absorption in the intestines and directly influences bones and growth plates as well as extraskeletal organs[2,3]. Vitamin D receptors and vitamin D metabolic enzymes are broadly expressed in the body. Several studies have shown that vitamin D has an effect on various organs and the immune system. Vitamin D deficiency causes osteopenia and rickets in infants and is associated with nonskeletal diseases such as allergies and autoimmune diseases, diabetes, cardiovascular disease, and cancer[3-5]. Lack of exposure to ultraviolet light is a risk factor for vitamin D deficiency, which is defined as 25-OH vitamin D levels of < 20 ng/mL[4]. However, several sunshine-rich countries, including Thailand, continue to report vitamin D deficiency cases despite the presence of abundant sunshine. Inadequate consumption of dairy products and low calcium intake are also causes of vitamin D deficiency[5]. Therefore, adequate ultraviolet light exposure and consumption of vitamin D-rich foods are crucial factors in maintaining normal vitamin D levels. Rickets, the most prevalent disease resulting from vitamin D deficiency, frequently occurs in children less than 2 years old. In 3-month-old infants, vitamin D is supplied through transplacental crossing, with the peak prevalence of rickets occurring in children aged 3–18 months[5,6]. Exclusively breastfed infants develop vitamin D deficiency rickets owing to inadequate sun exposure and low vitamin D content in breast milk (approximately 20 IU/Liter). The American Academy of Pediatrics has recommended that all breastfed infants should also be supplemented with 400 IU/d of vitamin D[5,7].
In Thailand, routine vitamin D supplementation guidelines for lactating mothers or infants have not been established, while in South East Asia, the amount of sun exposure required to maintain normal vitamin D levels in infants has not been quantified. A literature search recommended that infants wearing only a diaper should be exposed to sunlight for up to 30 min per week, while those fully clothed with no hat should be exposed to sunlight for up to 2 h per week[7].
This study investigated the prevalence of vitamin D deficiency and its associated factors in exclusively breastfed infants in Bangkok.
This descriptive observational cross-sectional study was conducted at Charoenkrung Pracharak Hospital, a tertiary and breastfeeding-friendly hospital in Bangkok, from May 2020 to April 2021. During this period, 510 4-month-old infants visited the well-baby clinic in Charoenkrung Pracharak Hospital. The study was approved by the Bangkok Metropolitan Administration Human Research Ethics Committee (S008h/63) on April 20, 2020.
The sample size of the study was calculated using the equation below: The expected proportion was estimated at 93.3% to give the largest sample size with a 5% degree of precision. The alpha error was accepted at 0.05, and the calculated sample size was 97, with 109 chosen after allowing for a 10% dropout rate.
A 10% value of the degree of precision was chosen due to financial and time limitations.
Four-month-old infants who were exclusively breastfed at the well-baby clinic in Charoenkrung Pracharak Hospital were included in the study. All the infants were born at 37-42 wk of gestation, weighed 2500-4000 g, and were of Thai descent. Infants who had received vitamin D supplementation and medications, had started using complementary foods, had been previously admitted to a neonatal intensive care unit, or those with other medical conditions (renal, gas
After obtaining written informed consent from the mothers, demographic data including gestational age, birth weight, and length were recorded. Maternal demographic data, body mass index (BMI), education level, status of vitamin D supplementation (defined as the mother taking a Obimin-AZ tablet containing 400 IU of vitamin D once daily after delivery until the date of enrollment), and family income were recorded. Vitamin D levels in the breast milk were not measured. The sun index record form was created to calculate the sun index, using hours of sun exposure per week and percentage body surface area exposed to sunlight (full sun is not needed). Directions describing seven consecutive days of sun exposure were provided to the mothers, and the accuracy of the sun index record forms completed by the enrolled mother–infant pairs was validated. All the mothers completed the sun index record form correctly without any errors, ensuring that the case record forms were valid. The completed sun index record forms were collected, and the sun index was calculated using the following formula: Sun index = hours of sun exposure per week × fraction of body surface area exposed to sunlight.
Blood samples were drawn once via venipuncture from the infants to measure the 25-OH vitamin D levels on the day of visiting the well-baby clinic. Other blood chemistry measurements were not assessed. The 25-OH vitamin D serum levels were measured using an electrochemiluminescence binding assay (cobas®; CE number 05894913190). Vitamin D deficiency was defined as 25-OH vitamin D levels of < 20 ng/mL, with vitamin D insufficiency defined as 25-OH vitamin D levels between 20 and 30 ng/mL, and vitamin D sufficiency defined as 25-OH vitamin D levels of ≥ 30 ng/mL. Hypovitaminosis D was defined as the combination of vitamin D deficiency and vitamin D insufficiency[4]. The data were computerized and analyzed using SPSS version 26 (SPSS, IBM Corp., Armonk, NY, United States). Normally distributed data were presented as means ± standard deviation. A univariate analysis was performed to compare and define the differences between the groups, while associations between the significant factors for vitamin D deficiency and other factors including sun index and vitamin D supplementation in mothers were analyzed using multivariate regression. The Chi-square test was used for categorical data, with analysis of variance for quantitative normally distributed data, and the Kruskal-Wallis test for non-normally distributed data. The P value cutoff was set at < 0.05.
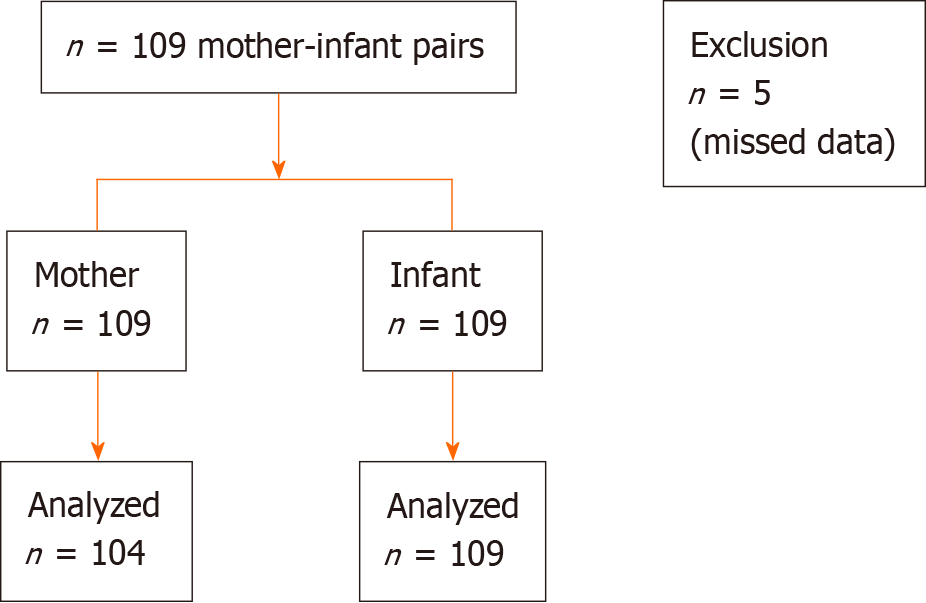
The flow diagram (Figure 1) shows demographic data for the 109 mother-infant pairs enrolled in the study. Incomplete case record forms were identified in five mothers and these were removed, with the remaining 104 maternal case record forms analyzed. Blood samples were drawn from 109 infants to measure 25-OH vitamin D levels, and a follow-up was conducted to collect the sun index record forms for analysis.
As shown in Table 1, the prevalences of vitamin D deficiency and insufficiency were 35.78% and 33.03%, respectively. The infants were categorized into three groups: Vitamin D deficiency (n = 39), vitamin D insufficiency (n = 36), and vitamin D sufficiency (n = 34). Among infants in the vitamin D deficiency group, 27 were male, and their mean weight and length were 6,956.92 ± 762.92 g and 62.28 ± 1.81 cm, respectively. Neonatal data showed that mean gestational age, birth weight, and birth length were 38.62 ± 1.09 wk, 3,110.51 ± 338.45 g, and 51.38 ± 2.09 cm, respectively. The demographic data of the infants were not significantly different between the groups, except that the mean birth weight of infants in the vitamin D insufficiency group was slightly lower than for infants in the other two groups (P = 0.008).
| Parametric | Vitamin D deficiency (n = 39) | Vitamin D insufficiency (n = 36) | Vitamin D sufficiency (n = 34) | P value |
| Prevalence, % | 35.78 | 33.03 | 31.19 | 0.326 |
| Season of study | 0.523 | |||
| Summer | 11 (28.20) | 16 (44.44) | 16 (47.05) | |
| Monsoon | 15 (38.46) | 10 (27.78) | 12 (35.29) | |
| Winter | 13 (33.33) | 10 (27.78) | 6 (17.65) | |
| Sun index (median – range) | 1.7-9.04 | 1.37-5.47 | 1.44-10.95 | 0.053 |
| Demographic data of infants | ||||
| Gender | 0.053 | |||
| Male | 27 (69.2) | 19 (52.8) | 14 (41.2) | |
| Female | 12 (30.8) | 17 (47.2) | 20 (58.8) | |
| Weight (g) | 6956.92 ± 762.92 | 6880.28 ± 1036.99 | 6657.53 ± 540.74 | 0.008 |
| Length (cm) | 62.28 ± 1.81 | 62.03 ± 2.24 | 61.15 ± 2 | 0.105 |
| Gestational age (wk) | 38.62 ± 1.09 | 38.64 ± 1.1 | 38.68 ± 1 | 0.930 |
| Birth weight (g) | 3110.51 ± 338.45 | 3093.92 ± 345.04 | 3332.5 ± 362.05 | 0.008 |
| Birth length (cm) | 51.38 ± 2.09 | 51.33 ± 1.67 | 51.35 ± 2.04 | 0.105 |
| Demographic data of mothers | ||||
| Age (yr) | 29.56 ± 7.18 | 27.69 ± 6.6 | 29.10 ± 6.9 | 0.496 |
| Age intervals | 0.754 | |||
| 10-19 (yr) | 5 (12.8) | 4 (11.1) | 3 (8.8) | |
| 19-35 (yr) | 26 (66.7) | 26 (72.2) | 21 (61.8) | |
| ≥ 35 (yr) | 8 (20.5) | 6 (16.7) | 10 (29.4) | |
| Body weight (kg) | 60.03 ± 11.61 | 57.39 ± 9.27 | 57.39 ± 9.25 | 0.496 |
| Height (cm) | 158.24 ± 5.73 | 158.83 ± 5.39 | 160.54 ± 6.25 | 0.274 |
| BMI (kg/m2) | 23.95 ± 4.4 | 22.76 ± 3.54 | 22.48 ± 3.87 | 0.251 |
| Obesity | 9 (26.5) | 8 (22.2) | 10 (25.6) | 0.908 |
| Education | 0.678 | |||
| Elementary school | 3 (8.8) | 2 (5.6) | 3 (7.9) | |
| Junior High School | 10 (29.4) | 6 (16.7) | 6 (15.8) | |
| High School | 13 (38.2) | 16 (44.4) | 14 (36.8) | |
| Bachelor degree or above | 8 (23.5) | 12 (33.3) | 15 (39.5) | |
| Family income (Dollars per month) | 973.09 ± 719.64 | 890.97 ± 511.1 | 1061.92 ± 1445.85 | 0.777 |
| Poverty | 17 (43.58) | 13 (36.11) | 16 (47.05) | 0.635 |
| Not poverty | 22 (56.41) | 23 (63.88) | 18 (52.94) | |
| Vitamin D supplement | 0.001 | |||
| No | 29 (74.35) | 23 (63.88) | 10 (32.30) | |
| Yes | 10 (25.64) | 11 (30) | 21 (67.70) |
Infants in the vitamin D deficiency group were studied in the summer, monsoon, and winter seasons, with 11 (28.20%), 15 (38.46%), and 13 (33.33%) showing vitamin D deficiency, respectively. The sun index score for the vitamin D deficiency group was 1.44-10.95 h/wk and slightly higher than the vitamin D insufficiency and sufficiency groups. For example, the sun index in the vitamin D sufficiency group was 1.70-9.04 h/week. The mean 25-OH vitamin D levels in the vitamin D deficiency, vitamin D insufficiency, and vitamin D sufficiency groups were 14.37 ± 3.36, 24.44 ± 3.29, and 40.33 ± 8.69 ng/mL, respectively.
The demographic data of mothers in the vitamin D deficiency group for mean age, weight, and height were 29.56 ± 7.18 years, 60.03 ± 11.61 kg, and 158.24 ± 5.73 cm, respectively. The mean BMI among mothers in the vitamin D deficiency group was 23.95 ± 4.4, with nine mothers classified as obese (23.07%). Maternal education level and vitamin D status were not significantly different between the groups (P = 0.678 and P = 0.709, respectively). Overall, 42 out of 104 mothers reported that they received Obimin-AZ, and no significant differences were observed between the groups.
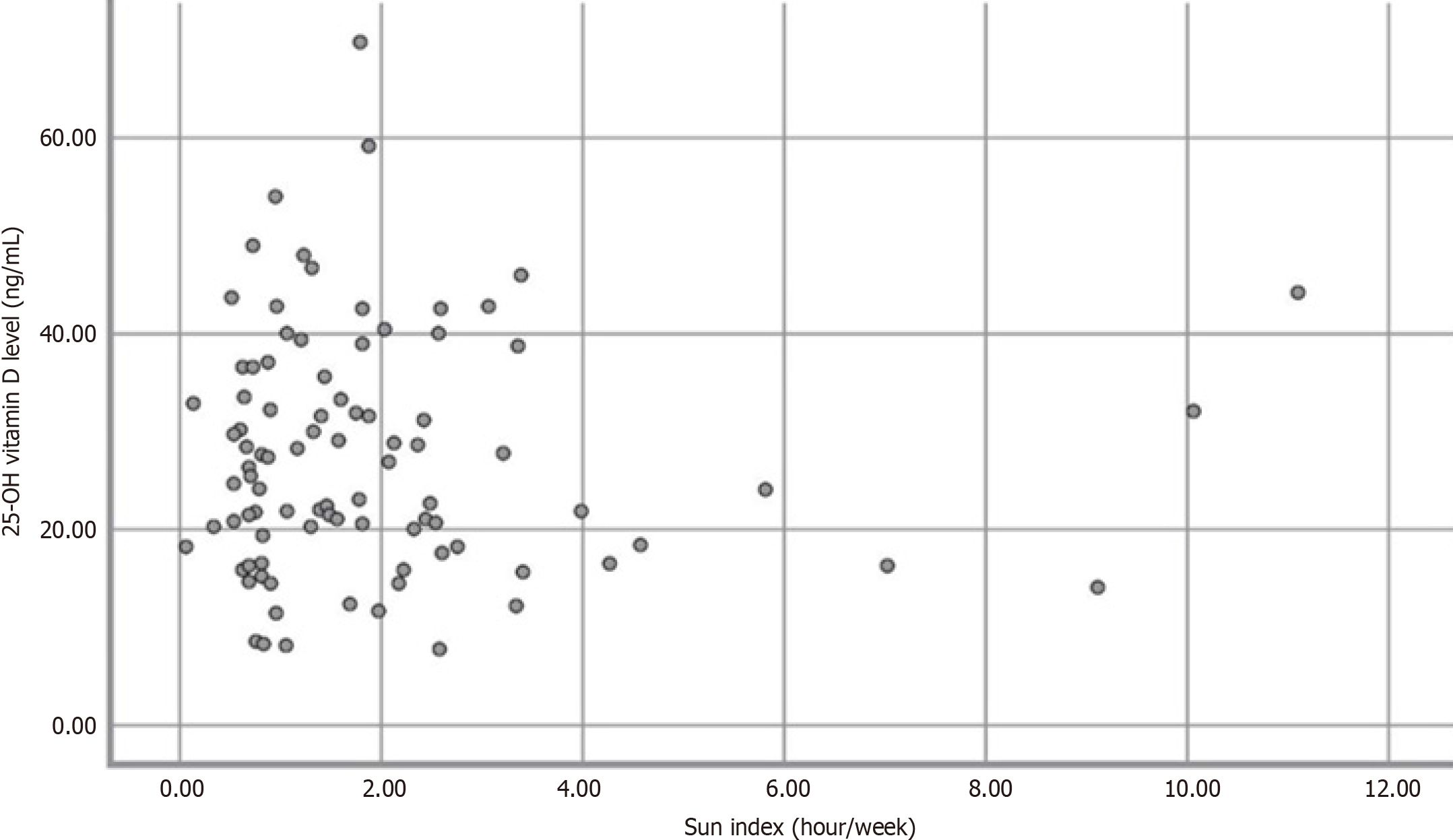
Univariate logistic regression identified male sex and vitamin D supplementation as two factors that were significantly associated with vitamin D status (Table 2), with crude odds ratios (ORs) 2.52 [95% confidence interval (CI): 1.1-5.76] and 0.36 (95%CI: 0.15-0.85), respectively. No significant differences were recorded in sun index scores and birth weights between the groups, with crude ORs 1.12 (95%CI: 0.89-1.39) and 0.46 (95%CI: 0.15-1.4), respectively. Multiple logistic regression analysis revealed that birth weight and vitamin D supplementation in mothers were significantly associated with vitamin D status, with adjusted ORs 0.08 (95%CI: 0.01–0.45) and 0.26 (95%CI 0.08–0.82), respectively. Vitamin D levels were not significantly correlated with the sun index [Pearson R-square = −0.002 (P = 0.984)] (Figure 2).
| Univariate analysis | Hypovitaminosis D | Sufficiency | P value | Crude OR (95%CI) |
| Parametric | ||||
| Infants | ||||
| Male, n | 27 | 33 | 0.028 | 2.52 (1.1-5.76) |
| Birth weight (kg) | 3.11 ± 0.34 | 3.21 ± 0.37 | 0.170 | 0.46 (0.15-1.4) |
| Sun index (h/wk) | 2.28 ± 2.14 | 1.84 ± 1.83 | 0.355 | 1.12 (0.89-1.39) |
| Mothers | ||||
| Vitamin D supplement, n | 10 | 32 | 0.020 | 0.36 (0.15-0.85) |
| Multivariate analysis | ||||
| Parametric | ||||
| Infants | ||||
| Male, n | 0.511 | 1.46 (0.47-4.49) | ||
| Birth weight (kg) | 0.004 | 0.08 (0.01-0.45) | ||
| Mothers | ||||
| Vitamin D supplement, n | 0.109 | 1.28 (0.95-1.73) |
A high prevalence of hypovitaminosis D was recorded in 4-month-old infants whose vitamin D status was slightly confounded by transplacental vitamin D. An age of 2 months is generally considered appropriate for investigating vitamin D levels in infants as they are no longer dependent on their mothers for vitamin D supply[8]. In this study, vitamin D intake from complementary foods did not interfere with the analyses because the infants were exclusively breastfed. We found that two-thirds of healthy exclusively breastfed infants had hypovitaminosis D, concurring with a previous study conducted in Thailand, which reported the incidence of 25-OH vitamin D levels of < 20 ng/mL at 56.8%[9]. Our findings were also consistent with other studies, which found a high prevalence of vitamin D deficiency and insufficiency among exclusively breastfed infants in high-latitude and sunshine-rich countries[9-14]. Notably, the prevalence of vitamin D deficiency reported in this study in Thailand was lower than reported in India (83%)[12], Korea (90.4%)[15], Brazil (80.5%)[11], and the United Arab Emirates (82%)[16]. These differences can be attributed to multiple factors including the latitude of the country, air pollution, season, infant age, and study design. Numerous studies from different countries have reported that breast milk has low vitamin D content[13,17], with several international organizations, including the American Academy of Pediatrics, recommending routine vitamin D supplementation in exclusively breastfed infants[18]. A crucial source of vitamin D in humans is the ultraviolet radiation-dependent cutaneous synthesis of cholecalciferol[19], with the positive effect of sun exposure on vitamin D status previously described[20]. Several studies have shown a lower prevalence of vitamin D deficiency in summer, along with relatively large seasonal fluctuations in circulating vitamin D levels[19-21]. This study is the first report on sun index values in infants in Thailand. Sun exposure can be represented by the sun index, which is calculated from the exposed body surface area and the duration of sun exposure in hours per week. Sun index was expected to be a protective factor; however, the average sun index was low in all participants, and not significantly associated with vitamin D level (r = −0.002, P = 0.984). Sun index was also inversely related to vitamin D status. Low sun exposure was reported in infants living in Bangkok because parents avoided taking their children outside due to air pollution. Our study subjects were 4-month-old infants who spent most of their daytime indoors. Some parents believed that their babies were too young to be exposed to sunlight, and this belief resulted in inadequate sun exposure, which is the major natural source of vitamin D production. Our results showed that seasons were not associated with vitamin D status. Approximately 40% of the infants in the vitamin D deficiency group were studied during the summer season, and their characteristics were similar to those examined during the winter and monsoon seasons. Despite the presence of abundant sunshine throughout the year in South East Asian countries, including Thailand, various studies showed that more than 30% of children and adolescents had vitamin D insufficiency[22]. By contrast, an Indonesian study reported that although Indonesia is located in similar latitudes to other South East Asian countries, the prevalence of vitamin D deficiency was only 16.7%. The authors described a routine cultural practice among Indonesian mothers that involved exposing their newborns (without any cover) directly to the morning sun. This practice may have contributed to cutaneous vitamin D production in these infants[23]. Lactating mothers have increased nutritional demands, including vitamin D delivered from breast milk to their infants. As previously mentioned, vitamin D content in breast milk is low, and lactating women with vitamin D deficiency are more likely to have deficient vitamin D levels in breast milk[24]. Therefore, these mothers should receive supplemental vitamin D to prevent vitamin D deficiency in their infants[25]. Several studies reported a significant correlation between maternal and cord blood vitamin D levels[6,10,26], with maternal vitamin D levels correlating with vitamin D levels in breast milk[17]. Our findings were similar to previous studies[27,28]. In this study, mothers received vitamin D supplementation through Obimin-AZ tablets, which contained 400 IU of vitamin D. An amount of 400 IU/day of vitamin D showed a more protective effect against vitamin D deficiency in mothers than 6,400 IU/d of vitamin D[24]. Despite the lower dosage of vitamin D supplementation in mothers in this study, the occurrence of hypovitaminosis D decreased in infants. Therefore, efforts should be made to identify an optimal dosage of vitamin D supplementation for lactating women.
Female infants showed lower mean serum 25-OH vitamin D levels than male infants[15]. In this study, male sex was found to be associated with poor vitamin D status compared with female sex. However, sex does not influence vitamin D metabolism, and male sex cannot be a clinically significant factor. The birth weight of infants in the vitamin D insufficiency group was lower than in the vitamin D deficiency and vitamin D sufficiency groups and was also associated with hypovitaminosis D. Several studies have shown a correlation between low birth weight and vitamin D deficiency, especially in preterm infants[29-31]. Our study showed that the lowest mean birth weight was reported in the vitamin D insufficiency group. Therefore, other factors should be examined in future studies. We believe that this is the first study to determine the prevalence of vitamin D deficiency in exclusively breastfed infants in Thailand without the effects of transplacental vitamin D or vitamin D from complementary foods. This is also the first study in Thailand to evaluate the sun index, which represents sun exposure. Low vitamin D content in breast milk and inadequate sun exposure in infants are significant risk factors for hypovitaminosis D. This study presented new data from Thailand that can be used to develop guidelines for mothers of infants. Supplementation of vitamin D with a dosage of at least 400 IU/d for infants since birth has also been recommended by the American Academy of Pediatrics. Our findings concur with the Institute of Medicine that vitamin D supplementation should be provided for lactating women[4,32].
This study had certain limitations. First, the vitamin D status of mothers and vitamin D levels in their milk were not measured. Therefore, vitamin D deficiency in mothers was not identified and the correlation between serum vitamin D levels and breast milk was not evaluated. Further studies should explore the association between these factors. Second, the sun index record form was difficult to understand and complete correctly for some mothers, resulting in incomplete reports with missing data. Following enrollment, the mothers were made aware that higher sun exposure resulted in increased vitamin D levels. Due to this knowledge and resulting behavioral changes, the sun index results could be artificially high, leading to bias. Additional studies, including a pilot for the sun index record form, should be conducted. Third, all the infants included in this study lived in Bangkok as an urban location, and the study was conducted in only one hospital. Therefore, the results cannot be considered representative of all Thai babies. Moreover, the air pollution in Bangkok is worse than in other provinces. And parents tend to avoid outside sun exposure for their children. A volunteer bias may also be present as a result of the sample population involved in the study, further limiting the generalizability of the results. Further studies that consider these limitations should be conducted to establish national guidelines.
Our results showed a high prevalence of vitamin D deficiency in exclusively breastfed infants. A 400 IU daily supplement of vitamin D in mothers was found to ameliorate vitamin D deficiency in infants. Sun exposure in infants was inadequate to maintain vitamin D levels and was not correlated with vitamin D status. Thai medical organizations should establish guidelines for routine vitamin D supplementation in exclusively breastfed infants.
Vitamin D deficiency is a common problem in exclusively breastfed infants. Therefore, vitamin D supplementation in infants is suggested by various international medical organizations. Due to limited available data in Thailand, there is no local recommendation for routine vitamin D supplementation. Thus, this study investigated the prevalence of vitamin D deficiency and its associated factors in exclusively breastfed infants.
Due to the limited number of studies on this issue in Thailand, routine vitamin D supplementation for lactating mothers or infants has not been established. In South East Asia, the amount of sun exposure required to maintain normal vitamin D levels in infants remains unknown. Few researchers have recommended that infants wearing only a diaper should be exposed to sunlight for up to 30 min per week and those with full clothes and no hat should be exposed to sunlight for 2 h per week. In addition, Charoenkrung Pracharak Hospital is a tertiary hospital which is a famous friendly breastfeeding hospital in Thailand and has a high rate of delivery. How big of vitamin D deficiency is a valuable thing to figure out in order to set up a proper guideline.
This study aimed to investigate the prevalence of vitamin D deficiency and its associated factors in exclusively breastfed infants in Bangkok. This study could not represent the overall Thai baby because we did a study in Bangkok which is the capital city of Thailand. So, enrolling the participants from all provinces is needed to study in the future in order to make an accurate prevalence of vitamin D deficiency in exclusively breastfed infants in Thailand.
This descriptive observational cross-sectional study assessed 109 4-month-old infants at Charoenkrung Pracharak Hospital from May 2020 to April 2021. The 25-OH vitamin D level of the infants was measured using an electrochemiluminescence binding assay. Vitamin D deficiency was defined as 25-OH level < 20 ng/mL, with vitamin D insufficiency 20-30 ng/mL. This study is the first to report on the sun index in infants in Thailand. Sun exposure is represented by the sun index, which is calculated from the exposed body surface area and the duration of exposure in hours per week. It was expected to be a protective factor. Sun index and maternal vitamin D supplementation data were collected and analyzed using the inde
This study shows the high prevalence of vitamin D deficiency and vitamin D insufficiency (35.78% and 33.03%, respectively). The mean serum 25-OH vitamin D levels in both groups were 14.37 ± 3.36 and 24.44 ± 3.29 ng/mL, respectively. The associated factors were maternal vitamin D supplementation and birth weight. supplementation which were analyzed with multivariate logistic regression and showed crude odds ratios were 0.26 (0.08–0.82) and 0.08 (0.01–0.45), respectively. Sun index did not correlate with the 25-OH vitamin D level in the exclusively breastfed infants (r = −0.002, P = 0.984). In addition, the sun index record form should be revised and recorded for at least 1 wk before collecting the blood to prevent the bias.
Our results showed a high prevalence of vitamin D deficiency in exclusively breastfed infants which is the risk factor of vitamin D deficiency. Daily supplement of vitamin D in mothers was found to ameliorate vitamin D deficiency in infants while sun exposure in infants was inadequate to maintain vitamin D levels and was not correlated with vitamin D status. Although Thailand is rich in sunshine, the prevalence of vitamin D deficiency is high. Therefore, Thai medical organizations should establish guidelines for routine vitamin D supplementation in exclusively breastfed infants.
The correlation of maternal vitamin D level, sun index, the dose of vitamin D supplement and vitamin level in exclusively breastfed infants should be evaluated in order to figure out the associated factors with vitamin D levels in infants. In addition, the vitamin D doses should be explored to set up proper vitamin D doses for prevention and treatment in exclusively breastfed infants who are diagnosed with vitamin D deficiency.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Pediatrics
Country/Territory of origin: Thailand
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Jovandaric MZ, Serbia; Yang LY, China S-Editor: Liu JH L-Editor: A P-Editor: Zhao YQ
| 1. | Bikle D, Christakos S. New aspects of vitamin D metabolism and action - addressing the skin as source and target. Nat Rev Endocrinol. 2020;16:234-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 207] [Article Influence: 41.4] [Reference Citation Analysis (0)] |
| 2. | Saponaro F, Saba A, Zucchi R. An Update on Vitamin D Metabolism. Int J Mol Sci. 2020;21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 153] [Article Influence: 30.6] [Reference Citation Analysis (0)] |
| 3. | Bouillon R, Marcocci C, Carmeliet G, Bikle D, White JH, Dawson-Hughes B, Lips P, Munns CF, Lazaretti-Castro M, Giustina A, Bilezikian J. Skeletal and Extraskeletal Actions of Vitamin D: Current Evidence and Outstanding Questions. Endocr Rev. 2019;40:1109-1151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 514] [Cited by in RCA: 670] [Article Influence: 111.7] [Reference Citation Analysis (0)] |
| 4. | Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Murad MH, Weaver CM; Endocrine Society. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911-1930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6974] [Cited by in RCA: 6844] [Article Influence: 488.9] [Reference Citation Analysis (0)] |
| 5. | Pettifor JM, Thandrayen K, Thacher TD. Vitamin D deficiency and nutritional rickets in children. Vitamin D: Elsevier. 2018;179-201. [DOI] [Full Text] |
| 6. | Niramitmahapanya S, Kaoiean S, Sangtawesin V, Patanaprapan A, Bordeerat NK, Deerochanawong C. Correlation of 25-Hydroxyvitamin D Levels in Serum vs. Breastmilk in Vitamin D-Supplementation Breastfeeding Women during Lactation: Randomized Double Blinded Control Trial. J Med Assoc Thai. 2017;100 Suppl 1:S165-S171. [PubMed] |
| 7. | Bae YJ, Kratzsch J. Vitamin D and calcium in the human breast milk. Best Pract Res Clin Endocrinol Metab. 2018;32:39-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 8. | Munns CF, Shaw N, Kiely M, Specker BL, Thacher TD, Ozono K, Michigami T, Tiosano D, Mughal MZ, Mäkitie O, Ramos-Abad L, Ward L, DiMeglio LA, Atapattu N, Cassinelli H, Braegger C, Pettifor JM, Seth A, Idris HW, Bhatia V, Fu J, Goldberg G, Sävendahl L, Khadgawat R, Pludowski P, Maddock J, Hyppönen E, Oduwole A, Frew E, Aguiar M, Tulchinsky T, Butler G, Högler W. Global Consensus Recommendations on Prevention and Management of Nutritional Rickets. Horm Res Paediatr. 2016;85:83-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 141] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 9. | Ruangkit C, Suwannachat S, Wantanakorn P, Sethaphanich N, Assawawiroonhakarn S, Dumrongwongsiri O. Vitamin D status in full-term exclusively breastfed infants versus full-term breastfed infants receiving vitamin D supplementation in Thailand: a randomized controlled trial. BMC Pediatr. 2021;21:378. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 10. | Marshall I, Mehta R, Ayers C, Dhumal S, Petrova A. Prevalence and risk factors for vitamin D insufficiency and deficiency at birth and associated outcome. BMC Pediatr. 2016;16:208. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | do Prado MR, Oliveira Fde C, Assis KF, Ribeiro SA, do Prado Junior PP, Sant'Ana LF, Priore SE, Franceschini Sdo C. [Prevalence of vitamin D deficiency and associated factors in women and newborns in the immediate postpartum period]. Rev Paul Pediatr. 2015;33:287-294. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Velusamy P, Devarajulu K. Prevalence of vitamin D deficiency in exclusively breastfed infants. Int J Contemp Pediatrics. 2019;6. [DOI] [Full Text] |
| 13. | Jan Mohamed HJ, Rowan A, Fong B, Loy SL. Maternal serum and breast milk vitamin D levels: findings from the Universiti Sains Malaysia Pregnancy Cohort Study. PLoS One. 2014;9:e100705. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 14. | Saraf R, Morton SM, Camargo CA Jr, Grant CC. Global summary of maternal and newborn vitamin D status - a systematic review. Matern Child Nutr. 2016;12:647-668. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 259] [Cited by in RCA: 232] [Article Influence: 25.8] [Reference Citation Analysis (0)] |
| 15. | Choi YJ, Kim MK, Jeong SJ. Vitamin D deficiency in infants aged 1 to 6 months. Korean J Pediatr. 2013;56:205-210. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Dawodu A, Agarwal M, Hossain M, Kochiyil J, Zayed R. Hypovitaminosis D and vitamin D deficiency in exclusively breast-feeding infants and their mothers in summer: a justification for vitamin D supplementation of breast-feeding infants. J Pediatr. 2003;142:169-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 108] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 17. | við Streym S, Højskov CS, Møller UK, Heickendorff L, Vestergaard P, Mosekilde L, Rejnmark L. Vitamin D content in human breast milk: a 9-mo follow-up study. Am J Clin Nutr. 2016;103:107-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 80] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 18. | Wagner CL, Greer FR; American Academy of Pediatrics Section on Breastfeeding; American Academy of Pediatrics Committee on Nutrition. Prevention of rickets and vitamin D deficiency in infants, children, and adolescents. Pediatrics. 2008;122:1142-1152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1031] [Cited by in RCA: 952] [Article Influence: 56.0] [Reference Citation Analysis (0)] |
| 19. | Ferrari D, Lombardi G, Strollo M, Pontillo M, Motta A, Locatelli M. Association between solar ultraviolet doses and vitamin D clinical routine data in European mid-latitude population between 2006 and 2018. Photochem Photobiol Sci. 2019;18:2696-2706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 20. | Barger-Lux MJ, Heaney RP. Effects of above average summer sun exposure on serum 25-hydroxyvitamin D and calcium absorption. J Clin Endocrinol Metab. 2002;87:4952-4956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 213] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 21. | Basile LA, Taylor SN, Wagner CL, Quinones L, Hollis BW. Neonatal vitamin D status at birth at latitude 32 degrees 72': evidence of deficiency. J Perinatol. 2007;27:568-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 47] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 22. | Jaruratanasirikul S. Vitamin D: an essential micronutrient for bone health. PSU Medical Journal. 2021;1:29-37. [DOI] [Full Text] |
| 23. | Oktaria V, Graham SM, Triasih R, Soenarto Y, Bines JE, Ponsonby AL, Clarke MW, Dinari R, Nirwati H, Danchin M. The prevalence and determinants of vitamin D deficiency in Indonesian infants at birth and six months of age. PLoS One. 2020;15:e0239603. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 24. | Hollis BW, Wagner CL, Howard CR, Ebeling M, Shary JR, Smith PG, Taylor SN, Morella K, Lawrence RA, Hulsey TC. Maternal Versus Infant Vitamin D Supplementation During Lactation: A Randomized Controlled Trial. Pediatrics. 2015;136:625-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 155] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 25. | Tan ML, Abrams SA, Osborn DA. Vitamin D supplementation for term breastfed infants to prevent vitamin D deficiency and improve bone health. Cochrane Database Syst Rev. 2020;12:CD013046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 26. | Ariyawatkul K, Lersbuasin P. Prevalence of vitamin D deficiency in cord blood of newborns and the association with maternal vitamin D status. Eur J Pediatr. 2018;177:1541-1545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 27. | Haggerty LL. Maternal supplementation for prevention and treatment of vitamin D deficiency in exclusively breastfed infants. Breastfeed Med. 2011;6:137-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 28. | Thiele DK, Senti JL, Anderson CM. Maternal vitamin D supplementation to meet the needs of the breastfed infant: a systematic review. J Hum Lact. 2013;29:163-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 29. | Matejek T, Navratilova M, Zaloudkova L, Malakova J, Maly J, Skalova S, Palicka V. Vitamin D status of very low birth weight infants at birth and the effects of generally recommended supplementation on their vitamin D levels at discharge. J Matern Fetal Neonatal Med. 2020;33:3784-3790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 30. | Agarwal R, Virmani D, Jaipal ML, Gupta S, Gupta N, Sankar MJ, Bhatia S, Agarwal A, Devgan V, Deorari A, Paul VK; Investigators of LBW Micronutrient Study Group, Departments of Pediatrics and Endocrinology. Vitamin D status of low birth weight infants in Delhi: a comparative study. J Trop Pediatr. 2012;58:446-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 31. | Maugeri A, Barchitta M, Blanco I, Agodi A. Effects of Vitamin D Supplementation During Pregnancy on Birth Size: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients. 2019;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 32. | Rosen CJ, Abrams SA, Aloia JF, Brannon PM, Clinton SK, Durazo-Arvizu RA, Gallagher JC, Gallo RL, Jones G, Kovacs CS, Manson JE, Mayne ST, Ross AC, Shapses SA, Taylor CL. IOM committee members respond to Endocrine Society vitamin D guideline. J Clin Endocrinol Metab. 2012;97:1146-1152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 385] [Cited by in RCA: 422] [Article Influence: 32.5] [Reference Citation Analysis (0)] |