Published online Dec 9, 2023. doi: 10.5409/wjcp.v12.i5.359
Peer-review started: June 6, 2023
First decision: August 30, 2023
Revised: September 9, 2023
Accepted: September 26, 2023
Article in press: September 26, 2023
Published online: December 9, 2023
Processing time: 178 Days and 11.9 Hours
Situs inversus totalis (SIT) may be an incidental finding in asymptomatic children. Patients may not understand the implications of this condition and the impor
We report an asymptomatic seventeen-year-old adolescent with previously-diagnosed SIT who presented for a routine well-child visit. During history taking, he denied any past medical conditions, including cardiovascular conditions. Only when physical exam revealed point of maximal impulse and heart sounds on the right side, did he convey that he had been diagnosed with SIT incidentally at age of 12 years. He was not aware of associated conditions or the potential implications of his diagnosis, nor did he realize it is pertinent medical history to be relayed to healthcare providers. Chest X-ray confirmed dextrocardia and abdo
While SIT is rare and mostly asymptomatic, affected patients may not compre
Core Tip: Situs inversus totalis (SIT) is a rare and mostly asymptomatic condition. This care report describes a previously-diagnosed seventeen-year-old adolescent who presented for a routine healthcare visit. During history taking, he denied any past medical conditions, including cardiovascular issues, until physical exam showed heart sounds on the right. He then revealed that he had been diagnosed with SIT incidentally at age 12, but did not realize that it is a significant condition. Patients with SIT may not understand the importance of the diagnosis and its potential ramifications. Healthcare workers must recognize that this lack of understanding of their diagnosis exists and educate them. Our patient was counseled that his diagnosis, although asymptomatic, should be relayed to healthcare teams.
- Citation: Hayashi LC, Acharya R. Situs inversus totalis in an asymptomatic adolescent - importance of patient education: A case report. World J Clin Pediatr 2023; 12(5): 359-364
- URL: https://www.wjgnet.com/2219-2808/full/v12/i5/359.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v12.i5.359
Situs inversus totalis (SIT) is a rare congenital anomaly in which the abdominal and thoracic organs are transposed across the sagittal midline with complete mirror-image reversal of laterality[1]. Situs solitus totalis is the term used to describe the normal left-right asymmetry with respect to midline in the arrangement of internal organs. Situs ambiguous, also called heterotaxy syndrome, involves a disturbance in the usual left-right distribution of the thoraco-abdominal organs which does not entirely correspond to the complete mirror image, unlike in SIT[2]. An example would be isolated dextrocardia, in which the heart has reverse orientation without concomitant laterality shift of thoracoabdominal organs. In some of these ambiguous cases, normally asymmetric structures like the lung (2 left lobes vs 3 right) and kidneys (different vascular branching patterns) tend toward symmetry[2]. SIT refers to complete, 180 degree reversal of left-to-right orientation, such that the heart, stomach and spleen are located on the right side, liver on the left side, and the paired lungs and kidneys also display reversal of left-right characteristics[1]. However, given that most of these cases are discovered incidentally during the work-up for another condition and are mostly asymptomatic, patients and their families may not realize the importance of this condition. Here, we report such a lack of awareness in a 17-year-old male with SIT who presented for a routine health care examination visit in a primary care provider’s office.
Patient is a 17-year-old male who presents to the adolescent clinic in the southeastern United States for a sports physical examination and well-child visit.
Patient is accompanied by his mother, who is from South America and does not speak English. Patient and mother report that he is “completely healthy with no medical conditions.” He exercises regularly for 90 min daily, encompassing both strength training and cardiovascular fitness.
The patient initially reports no medical history, including when directly asked about cardiac conditions or symptoms of chest pain, shortness of breath, dyspnea at rest or on exertion, palpitations, ascites, or leg edema. However, when physical exam revealed right-sided heart sounds, the patient revealed that he had been diagnosed incidentally at the age of 12 years following an X-ray performed for unrelated abdominal pain. He subsequently had two appointments with a cardiologist in South America with no reported symptoms or complications. Since moving to the United States two years ago, he has not had medical care. He denies history of sinopulmonary infections or decreased olfaction. When asked why the patient and mother did not disclose this diagnosis when queried about cardiac conditions, their answer was that it was not important information since he is healthy and SIT does not affect him; their understanding was that he did not have a disease, just a mirror-image flip and was essentially normal. The patient and his mother were surprised by these questions and were unaware that this condition may be associated with other syndromes or that there may be potential ramifications for his medical treatment in the future.
The patient’s personal and family history were otherwise unremarkable for cardiovascular conditions or sudden deaths.
Physical examination revealed stable vital signs with manual blood pressure 120/74 mmHg (< 95th percentile for age, height and gender), pulse 86 beats per minute, temperature 96.2° F, and body mass index of 24.5 kg/m2. Cardiovascular examination was significant for point of maximal impulse palpated on the right at the 5th intercostal space at the midclavicular line. Rate and rhythm were regular with no murmurs, rubs or gallops. Skin had two benign-appearing dark nevi with well-defined borders (approximately 2-3 mm) along posterior axillary line bilaterally. There were no surgical scars detected. Abdominal examination was significant for inferior border of liver palpated 2 cm beneath left costal margin. There were normal bowel sounds with no rebound or guarding.
Investigations showed borderline decreased high-density cholesterol of 27 mg/dL (23-92 mg/dL), and otherwise unremarkable lipid studies. Complete blood count showed hemoglobin of 16 g/dL. Renal and hepatic function was normal.
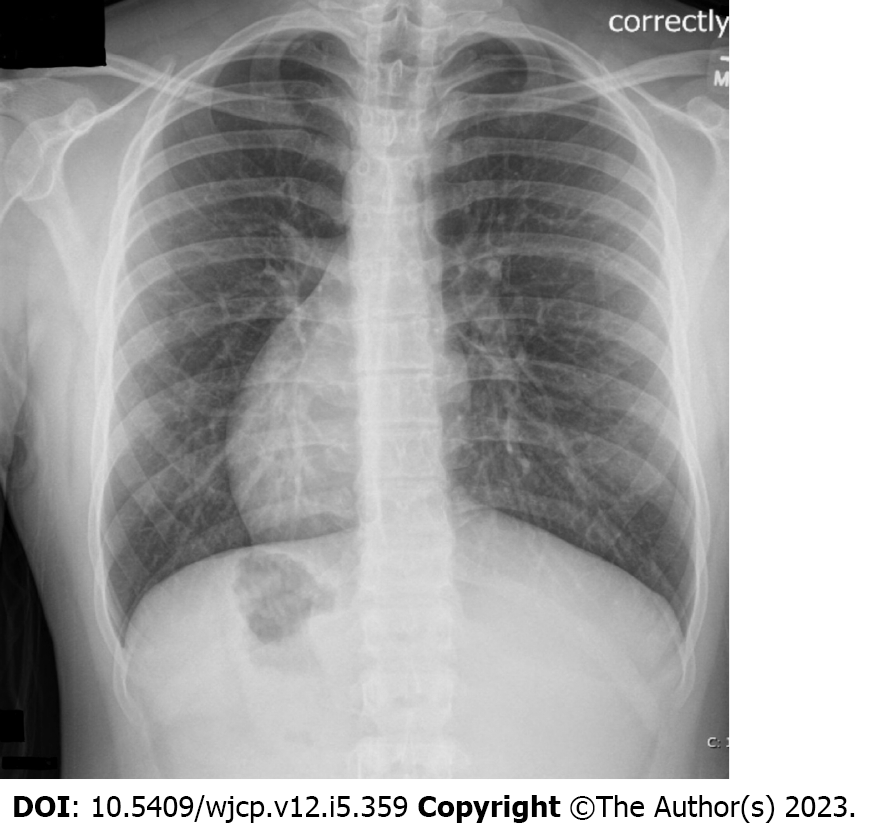
Chest X-ray showed dextrocardia with situs inversus (Figure 1). Abdominal radiograph showed stomach on the right upper quadrant (Figure 2). Transthoracic echocardiogram showed heart located in the right chest with cardiac apex pointing to the right. There was atrial situs inversus with atrio-ventricular concordance and ventriculo-arterial concordance. The pulmonary veins drained normally to the right sided morphologic left atrium. The superior and inferior vena cava drained normally to the left sided morphologic right atrium. There was normal valvular structure and function. Abdominal sonogram report from South America mentioned liver on the left, spleen on the right, and mirror image configuration of aorta and inferior vena cava.
The final diagnosis was SIT with dextrocardia.
No specific treatment for this condition was necessary.
Given that the patient was asymptomatic with otherwise stable chest X-ray and normal echocardiogram, no further workup was deemed necessary. The main intervention consisted of counseling the patient and his mother about SIT, including how it is a medical condition that should be included when relaying his history. The patient was asked to follow up at next well-child visit for routine check-up. It was suggested that no scheduled follow up with cardiology is necessary unless symptoms arise.
In this report, we describe an asymptomatic adolescent male with a history of incidentally found SIT who, upon relaying his medical history, initially denied cardiac conditions, including when directly asked about congenital heart conditions. The patient was unaware that SIT is a diagnosis that should be communicated to his providers as part of his history. It was only when heart sounds were auscultated on his right side that he mentioned his diagnosis. He explained that from his understanding, SIT would not impact his health. He was unaware that it may be associated with other syndromes and was thus confused when further questioned about symptoms that could be associated with SIT. It is critical to educate these patients about their condition and potential implications. This case report is the first to our knowledge to highlight the lack of patient understanding of their SIT diagnosis and to focus upon the importance of patient education.
Reverse orientation of thoracoabdominal organs was first documented in human beings in the 17th century[3]. In 1888, the condition was documented with illustrations of physical exam findings. Finally, in 1897, Vehsemeyer was the first to demonstrate transposition by X-ray, which in addition to ultrasound has since been the diagnostic method of choice[4]. The incidence of SIT has been reported to be 1:6500 to 1:25000[1].
Laterality is established in utero around day 22 when embryological cardiac tubes rotate rightward, known as looping[5]. The apex of the heart migrates to the left thorax over the following two weeks, such that the heart is located on the left side of the chest[6]. Dextrocardia is a heart with the apex directed to the right[7]. When the abnormal rotation of the cardiac tubes leftward is also accompanied by a similar rotation of the lungs and visceral organs, SIT results. The embryological cascade which dictates laterality is believed to involve over a hundred genes, including those coding for signaling, cell adhesion and motor peptides. While most cases of abnormal laterality are sporadic, there are also hereditary cases[8].
It is important to note that SIT may occur with other anomalies or as a part of broader syndromes. The most common is primary ciliary dyskinesia, also known as immotile cilia or Kartagener syndrome, which can involve a triad of situs inversus, bronchiectasis and sinusitis. About half of the individuals with a diagnosis of Kartagener’s syndrome have SIT. The underlying dysmotility in cilia and flagella results in recurrent sinopulmonary infections, anosmia and infertility in males[9].
Rates of congenital heart disease increase with left-right malformation. Cardiac anomalies occur in 3%-9% of patients with SIT and 80% with situs ambiguous, compared to 0.6% without a laterality condition[10]. Up to 25% of patients with situs ambiguous may not be diagnosed until adulthood, especially those with mild cardiac abnormalities[1]. Caval vein disorders are also common, which may lead to higher rates of deep vein thrombosis[11]. When situs ambiguous disrupts splenic development, it can cause either asplenia (double right-side anatomy or right isomerism) or polysplenia (double left-side anatomy or left isomerism)[12]. Asplenia is associated with severe cardiac and pulmonary abnormalities, leading to a mortality rate up to 80% in the first year[13,14]. It is important to take a careful history about syndromic or congenital heart disease symptoms and following up the abnormal physical examination findings with imaging to differentiate among these laterality diagnoses.
Our patient falls into the majority of SIT patients who are asymptomatic with an incidental diagnosis. Even though he was previously diagnosed, he did not realize this information is pertinent medical history and was unaware that his presentation could be part of a broader syndrome.
An understanding of their disease is of especial importance in pediatric adolescent patients as they transition to adult care. Of the handful of studies that address this topic in adolescents with congenital heart conditions, participants have shown a poor understanding of their disease. One study in adolescents (median 13 years of age) with a wide spectrum of heart disease (not including SIT), illustrated that 78% of participants did not know the medical name of their condition and 36% had a poor understanding or wrong concept about their disease. There was no association between under
Having an understanding of SIT and communicating the diagnosis is of particular importance in emergent settings such as acute abdomen, since SIT patients may have atypical symptom locations[17]. Patients who present with left sided abdominal pain in the setting of appendicitis are more likely to have delayed diagnosis and treatment[18]. One report described a 46-year-old with a family history of SIT who presented with left upper quadrant pain[19]. Because the patient volunteered the SIT family history, clinical suspicion for SIT was high and thus atypical differential diagnoses were considered. Indeed, the work-up revealed both a new SIT diagnosis and acute cholecystitis, which might have otherwise been misdiagnosed and mistreated as gastritis. Another report described a patient who was diagnosed incidentally during exploratory laparotomy in the setting of trauma[20]. Visceral surgery in SIT patients poses a unique challenge; the common guidance for surgery in SIT patients includes diligent preoperative planning and selection of experienced surgeons who can adapt to technical modifications for the reverse anatomy[21].
Our case report illustrates a poor understanding of SIT in a previously-diagnosed adolescent. Given the patient was a new international patient to our clinic, his previous medical records from South America were unavailable. We were thus relying on his and his mother’s history, in which they failed to convey his SIT diagnosis until it was revealed by physical exam. He subsequently showed a lack of knowledge about the disease or its potential implications. After our patient had a stable X-ray and echocardiography to rule out congenital abnormalities, he was deemed clear for sports and counseled about his condition. This surprise diagnosis in an outpatient setting had little health consequence, but could have added confusion and costly time to diagnosis or surgical challenges in the context of urgent care or trauma.
The main limitation of this case is that the patient had an incentive to present himself as a healthy individual with no medical conditions, since he was seeking medical clearance for high school sports. It is possible this led him to downplay his diagnosis; yet it is also possible that he truly had an inaccurate understanding of his disease. If this misperception is genuine, it may be that his previous cardiologist’s reassurances that SIT is not immediately life-threatening led to this patient’s idea that it is not a medical disease. To fully understand the extent of incomplete comprehension about SIT within asymptomatic patients, more research is needed in pediatric patients outside of the medical-clearance context.
Because SIT is so rare and most physicians will encounter only a few cases in their careers[4], the medical profession has not recognized this lack of awareness within adolescent SIT patients, let alone SIT patients in general. There are currently no guidelines about how to counsel patients with this condition. This case report highlights a knowledge gap within the medical literature on the extent to which patients with SIT understand their disease. Further research on this topic may help guide clinical practice in counseling patients with SIT and enable patients, especially adolescents, to safeguard their health.
SIT is a congenital anomaly with potential health implications. This case report highlights the poor understanding of the disease in a previously diagnosed adolescent and the importance of patient education. For an adolescent approaching adulthood, it is of particular importance that he comprehend and can communicate his own medical history, especially with a diagnosis of SIT. This understanding can help avert diagnostic and therapeutic confusion, especially in the setting of trauma or emergent surgeries, where a thorough review of past medical records is not always feasible. The patient was counseled that his SIT diagnosis, although asymptomatic, must be relayed to future healthcare teams as it could affect his medical care.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Pediatrics
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: MD XM, China S-Editor: Lin C L-Editor: A P-Editor: Yuan YY
| 1. | Eitler K, Bibok A, Telkes G. Situs Inversus Totalis: A Clinical Review. Int J Gen Med. 2022;15:2437-2449. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 101] [Article Influence: 33.7] [Reference Citation Analysis (0)] |
| 2. | Spoon JM. Situs inversus totalis. Neonatal Netw. 2001;20:59-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 31] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Wood GO, Blalock A. Situs inversus totalis and disease of biliary tract: survey of literature and report of case. Arch Surg. 1940;40:885-896. [RCA] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Blegen HM. Surgery in Situs Inversus. Ann Surg. 1949;129:244-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 95] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 5. | Splitt MP, Burn J, Goodship J. Defects in the determination of left-right asymmetry. J Med Genet. 1996;33:498-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 55] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 6. | Izpisúa Belmonte JC. How the body tells left from right. Sci Am. 1999;280:46-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Evans WN, Acherman RJ, Collazos JC, Castillo WJ, Rollins RC, Kip KT, Restrepo H. Dextrocardia: practical clinical points and comments on terminology. Pediatr Cardiol. 2010;31:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 34] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Peeters H, Devriendt K. Human laterality disorders. Eur J Med Genet. 49:349-362. [RCA] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 126] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 9. | Popatia R, Haver K, Casey A. Primary Ciliary Dyskinesia: An Update on New Diagnostic Modalities and Review of the Literature. Pediatr Allergy Immunol Pulmonol. 2014;27:51-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Merklin RJ, Varano NR. Situs inversus and cardiac defects. A study of 111 cases of reversed asymmetry. J Thorac Cardiovasc Surg. 1963;45:334-342. [PubMed] |
| 11. | Batouty NM, Sobh DM, Gadelhak B, Sobh HM, Mahmoud W, Tawfik AM. Left superior vena cava: cross-sectional imaging overview. Radiol Med. 2020;125:237-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 12. | Asplenia, Polysplenia Syndromes. In: Baert AL editors. Encyclopedia of Diagnostic Imaging. Berlin: Springer, 2008 . [DOI] [Full Text] |
| 13. | Maldjian PD, Saric M. Approach to dextrocardia in adults: review. AJR Am J Roentgenol. 2007;188:S39-49; quiz S35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 76] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 14. | Applegate KE, Goske MJ, Pierce G, Murphy D. Situs revisited: imaging of the heterotaxy syndrome. Radiographics. 1999;19:837-52; discussion 853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 178] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 15. | Veldtman GR, Matley SL, Kendall L, Quirk J, Gibbs JL, Parsons JM, Hewison J. Illness understanding in children and adolescents with heart disease. Heart. 2000;84:395-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 66] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 16. | Van Deyk K, Pelgrims E, Troost E, Goossens E, Budts W, Gewillig M, Moons P. Adolescents' understanding of their congenital heart disease on transfer to adult-focused care. Am J Cardiol. 2010;106:1803-1807. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 86] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 17. | Oh JS, Kim KW, Cho HJ. Left-sided appendicitis in a patient with situs inversus totalis. J Korean Surg Soc. 2012;83:175-178. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Akbulut S, Ulku A, Senol A, Tas M, Yagmur Y. Left-sided appendicitis: review of 95 published cases and a case report. World J Gastroenterol. 2010;16:5598-5602. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 71] [Cited by in RCA: 67] [Article Influence: 4.5] [Reference Citation Analysis (1)] |
| 19. | Herrera Ortiz AF, Lacouture JC, Sandoval Medina D, Gómez Meléndez LJ, Uscategui R. Acute Cholecystitis in a Patient With Situs Inversus Totalis: An Unexpected Finding. Cureus. 2021;13:e15799. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Olasehinde O, Owojuyigbe AM, Adisa AO, Awowole IO. Incidental finding of complete situs inversus in a polytraumatized adult. Afr J Med Med Sci. 2014;43:183-186. [PubMed] |
| 21. | Enciu O, Toma EA, Tulin A, Georgescu DE, Miron A. Look beyond the Mirror: Laparoscopic Cholecystectomy in Situs Inversus Totalis-A Systematic Review and Meta-Analysis (and Report of New Technique). Diagnostics (Basel). 2022;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |