Published online Sep 9, 2022. doi: 10.5409/wjcp.v11.i5.408
Peer-review started: February 26, 2022
First decision: April 17, 2022
Revised: June 1, 2022
Accepted: August 22, 2022
Article in press: August 22, 2022
Published online: September 9, 2022
Processing time: 193 Days and 6 Hours
Children/adolescents with type 1 diabetes (T1D) require holistic approach and continuous care. However, the coronavirus disease 2019 (COVID-19) pandemic has made challenges for the T1D children and their caregivers, professionals, and the healthcare system. This minireview aims to consolidate and discuss the difficulties and solutions of children with type 1 diabetes in the COVID-19 pandemic. T1D has been the most common type of diabetes in children and adolescents and the last decades has seen a rapid increase in the prevalence of T1D in youths worldwide, which deserves a public concern particularly in the COVID-19 pandemic. As reported in previous studies, T1D is a risk factor related to severe cases, while the virus may induce new-onset diabetes and serious complications. Moreover, restriction strategies influence medical availability and lifestyle, impact glycemic control and compilation management, and thus pose stress on families and health providers of youths with T1D, especially on those with certain fragile conditions. Therefore, special treatment plans are required for children provided by caregivers and the local health system. Latest health tools such as improved medical devices and telemedicine service, as well as a combined support may benefit in this period. This minireview emphasises that continued medical access and support are required to prevent deteriorated condition of children and adolescents with diabetes throughout this pandemic. Therefore, strategies are supposed to be formulated to mitigate the difficulties and stress among this group, particularly in the most at-risk population. Proposed solutions in this minireview may help individuals and the health system to overcome these problems and help youths with T1D in better diabetes management during such emergency situations.
Core Tip: There are several reviews in the literature discussing the difficulties or solutions to the life of children with type 1 diabetes (T1D). However, this is the first review to collect and analyse the latest studies on which sub-groups of children with T1D are more likely to be influenced, how the coronavirus disease 2019 pandemic affects the treatment of children with T1D and the life of their caregivers, and what measures are supposed to be applied to deal with these dilemmas.
- Citation: Shi Y, Wu LQ, Wei P, Liao ZH. Children with type 1 diabetes in COVID-19 pandemic: Difficulties and solutions. World J Clin Pediatr 2022; 11(5): 408-418
- URL: https://www.wjgnet.com/2219-2808/full/v11/i5/408.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v11.i5.408
Type 1 diabetes (T1D) is a heterogeneous disorder characterized by destruction of pancreatic beta cells, culminating in absolute insulin deficiency. It accounts for 5- 10% of the total cases of diabetes worldwide corresponding to 21-42 million people, while type 2 diabetes (T2D), characterized by a combination of resistance to insulin action and inadequate compensatory insulin secretory response, is the more prevalent category[1]. Particularly, in children and adolescents, T1D has been the most prevalent type of diabetes and 15%-20% of newly diagnosed patients are under age 5. Children with T1D and their caregivers are faced with challenges from various aspects such as physiology, psychology, and development[2].
The coronavirus disease 2019 (COVID-19) has been regarded as a global pandemic since 2020, leading to strict control policy and interrupted health care services, which contribute to challenges such as disruption in follow-up visits, restricted availability of medicines, and changes in lifestyle, particularly for those with chronic illnesses such as T1D[3,4].
Although there have already been some attempts to help to address these dilemmas, a systematic review on this issue has not been carried out. Since there are a large number of children and adolescents with T1D, who have specific concerns during the ongoing pandemic, we review the existing literature, related websites, and relevant guidelines to form this minireview to help resolve key questions in this area.
T1D is a frequent chronic diseases in infants and the most common endocrinal disease in children and adolescents[5]. To diagnose the diabetes syndrome, both the history and check results are clues: A family history of diabetes is important, while a history of previous early childhood deaths or miscarriages is relevant. Pointers in the examination include evidence of sensorineural hearing loss or vision defects or developmental delay. Useful investigations include autoantibodies to glutamic acid decarboxylase, islet cells, audiogram and visual evoked responses, and fasting insulin and C-peptide. Further specialized checks include an echocardiogram, bone marrow aspirate, skeletal survey, and genetic testing[6].
Diabetes management mandates adherence to insulin, balanced diet, regular physical activity, and self-monitoring of blood glucose to achieve good glycemic control and prevent the development of short-term and long-term complications[7]. Pediatric diabetes management needs continuous parental supervision and confronts the whole family in challenges in the daily life, including regular blood glucose monitoring, insulin application, dietary indications, etc[8]. To achieve a favorable control, it is necessary to monitor blood sugar on a regular basis in a day, while for the patients who have erratic glycemic control or intermittent hypoglycemia, it is recommended to monitor at least 4 times a day and an additional check should be performed when there are signs or symptoms related to hypoglycemia[8]. In addition, children and adolescents with T1D require multiple daily insulin injections: The major organizations recommend one to two basal insulin injections with at least three regular or rapid acting insulin injections[8].
Unsatisfying metabolic control may result in the acute complications of hypoglycemia and ketoacidosis, poor growth, and chronic microvascular and macrovascular complications. Due to the fact that children and adolescents are more sensitive to a lack of insulin than adults, the youths are at higher risk of a rapid and dramatic development of diabetic ketoacidosis. Episodes of severe hypoglycemia or ketoacidosis especially in young children are risk factors for structural brain abnormalities and impaired cognitive function[9].
Risk of contracting COVID-19 in patients with T1D: Diabetes can affect the immune response to pathogens and thus make patients vulnerable to the infections[10,11]. Diabetic patients are exposed to a higher risk of being infected compared to the healthy group and the risk is even greater in T1D children than in those with T2D, which may be attributed to immune dysfunction, micro- and macro-angiopathies induced by hyperglycemia, and more needs for medical interventions in this group[12,13]. Analyses carried out in many countries revealed that people with diabetes hospitalized for COVID-19 have a greater chance to suffer more severe outcomes, including twice the risk of requiring intensive unit care and increased risk of death[14-19]. It can be attributed to free radical overproduction due to viral infection, which can burden the oxidative stress, leading to pulmonary oxidative injury and inflammation[20]. Furthermore, the virus causes glucose metabolism disorders, which may entangle the pre-existing diabetes in complications[21].
Effect of COVID-19 on development of T1D: Viral infections are associated with the development of pancreatic autoantibodies leading to T1D in genetically susceptible children, and coronavirus family was considered to be an incriminating pathogen[22]. Viral infections trigger autoimmune insulitis and pancreatic β-cell destruction by directly damaging β-cells, increasing the risk of autoantibody generation, and activating cytokine release and T cells[23]. According to previous surveys, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV2) binds to angiotensin-converting enzyme 2 receptors in the pancreas, consequently damaging islet cells and reduced insulin release[24]. During the COVID-19 pandemic, similar associations have been made for children[25, 26].
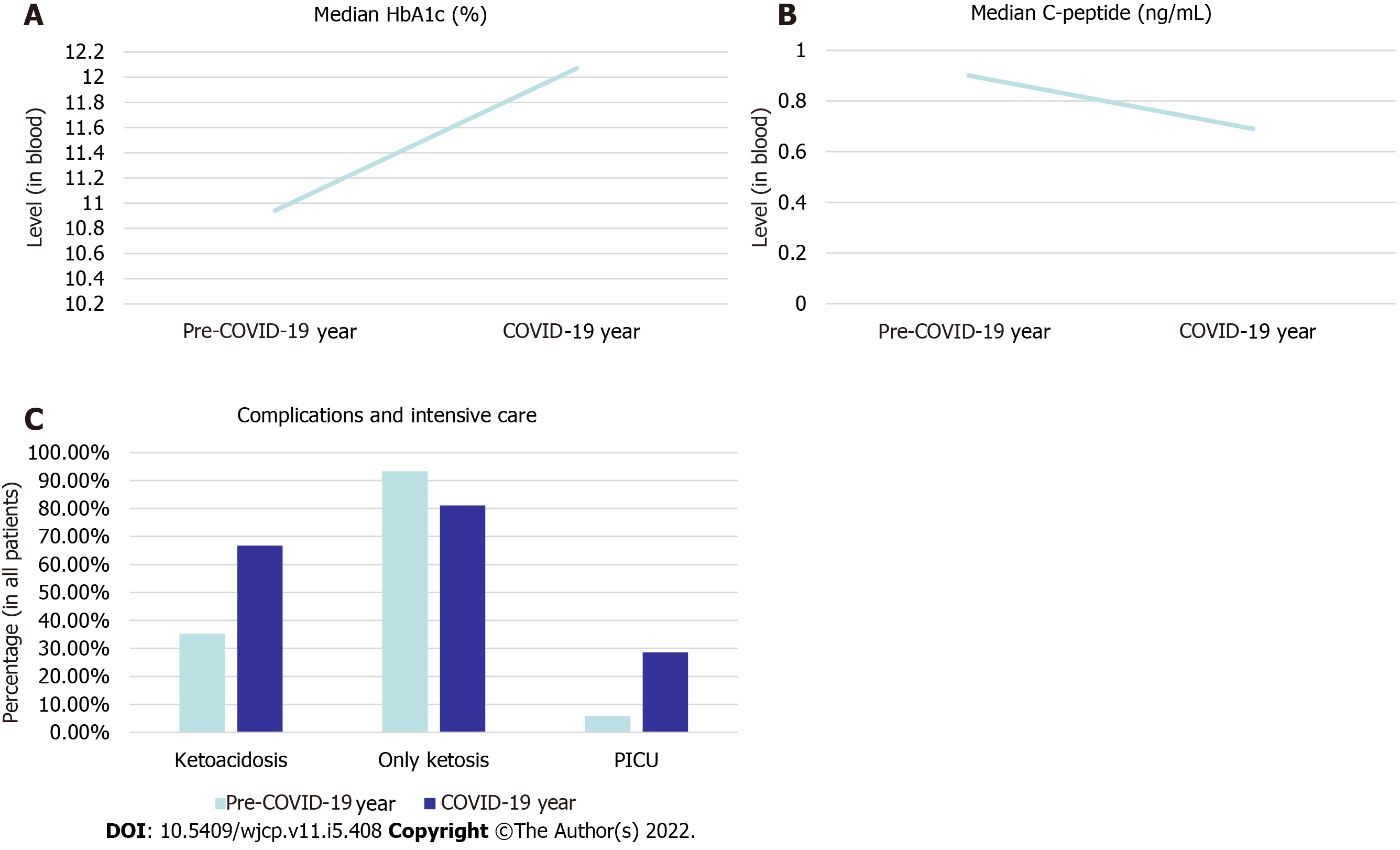
The data in Figure 1 represent the situation in Western Greece. The median ages of the patients are 10.94 years old and 12.07 years old in pre-COVID-19 years and COVID-19 years, respectively.
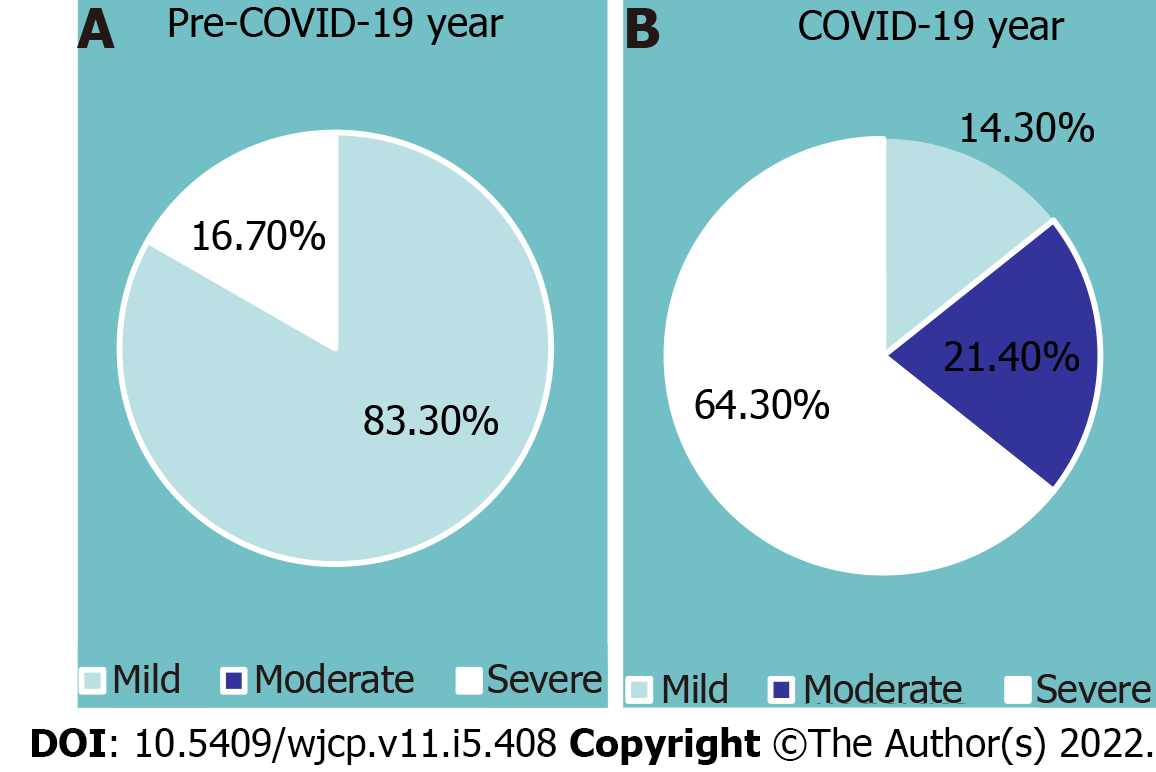
Cautions against COVID-19 on complications of T1D: Chloroquine and hydroxychloroquine are increasingly administered to treat COVID-19. However, these drugs may increase the incidence of hypoglycemia in diabetes patients[27]. Chloroquine stimulates insulin secretion, glucose uptake, and glycogen synthase, while hydroxychloroquine decreases insulin degradation, increases intracellular insulin accumulation, and stimulates insulin-mediated glucose transport[27,28]. All these functions can lead to a low blood glucose level and therefore, patients with T1D who use these agents need should be monitored for hypoglycemia (Figure 2).
Risk of diabetic ketoacidosis: COVID-19 can increase the opportunity of diabetic ketoacidosis (DKA) and hyperosmolar hyperglycaemic state even in people without previously diagnosed diabetes[29]. Meanwhile, patients with T1D are at a greater risk of developing DKA especially in youths, and there are reports of prevalence of severe DKA in COVID children with established T1D[21,30,31]. Moreover, researchers have found that delayed diagnosis of new-onset T1D can lead to severe DKA, which may be due to reduced clinical visit for fear of being infected by SARS-CoV2, less access to emergency departments, closure of non-COVID-19-related hospital services, preoccupied doctors, and potential changes in access to insulin or self-monitoring of blood glucose test strips[32,33]. Certain features of DKA overlap with viral illnesses in youths and pediatricians should pay attention to symptoms including polyuria, polydipsia, weight loss, and Kussmaul breathing, as well as a fruity odour in breath. Ultimately, the standard of care for DKA to apply intravenous insulin may lead to a dilemma in the present pandemic because it often requires ICU admission. However, beds may be occupied for COVID-19 patients[31,34].
Influence of restriction strategies on individual T1D management: Strict isolation measures interrupt access to routine health care and social activities, thus increasing stress and anxiety among children and adolescents with T1D and their caregivers[4]. Since T1D is dominantly affected by alterations in daily routine, isolation measures pose a negative effect in glycemic control. However, interestingly, several researchers have reported contrary results that there was no deterioration or even improvement in glycemic management (Table 1).
| Target group | Methods | Pros | Cons |
| Patients | Routine glycemic management | Provide a more convenient and comfortable alternative | |
| Sick day management | Avoid glycemic fluctuations and subsequent risk of complications | Need regular education and more rigorous adherence | |
| Psychosocial aids | May help to vent out distress | ||
| Physical activities | May help to reduce stress and achieve a healthy BMI | May be hard to perform because of the restriction in outdoor activities | |
| Caregivers | Channels for voice and guidance | Eliminate the sense of overload | |
| Provision of multidisciplinary ways | Provide economically accessible information | ||
| Groups on social media | Share perceptions and help each other | ||
| Medical providers | Collaboration and intervals | Improve patient care equality, provide the learning opportunities to establish a holistic view | |
| Financial and social stressors inquiries | Affect family engagement with healthcare providers | ||
| Persistent efforts | May help to get desired outcomes | ||
| Telemedicine users | May help to get diabetes reviews, self-management support, and timely professional intervention with the minimised risk of virus transmission | Have difficulty to perform a suitable physical examination, lack widespread availability, have obstacles to gain collaboration, cannot replace the in-clinic visits in several circumstances |
Factors that worsen glycemic control: Difficulties in access to medical care was particularly prevalent in families with a lower socio-economic condition[35,36]. The COVID-19 pandemic has led to an economic crisis, and those whose financial stability was already difficult were first to suffer[37]. Researchers found that minority children had a higher glycosylated hemoglobin (HbA1c) level both in the pre-pandemic and the lockdown period than white race[38-40]. Similarly, patients with medical aid had a notably higher HbA1c and increase in HbA1c during the lockdown than those with private insurance[38]. Other publications have also indicated that youth whose families are in a disadvantaged financial condition have poorer glucose control[38-40]. The reason can be ascribed to the fact that many of those are supported by various programs for regular supply of insulin and glucose meterstrips[41]. However, these medicine and devices may be unavailable because of closure of nodal healthcare facilities and local transport facilities during the lockdown. Sequentially, the limited availability and the fear of shortage of medical supply forced these children with T1D to reduce glucose monitoring, which caused more frequent hypo-/hyperglycemic excursions[42]. Moreover, consequent DKA may emerge with unavailability of any type of insulin or technology-related problems such as pump dysfunction[43].
Female gender was a risk factor for unfavorable glycaemic control due to more mental effect[44,45]. Glycemic control interacts with stress, which may directly disturb glucose regulation, or indirectly result in non-adherence to treatment and unhealthy daily routine[46]. Previous epidemiological publications reported that females are at a greater risk for psychological disorders and perceived stress is more prevalent among females compared with males in the lockdown[47]. Interestingly, one study indicated that the glycemic control of males was more adversely affected in this period, which may be ascribed to more changes in almost all aspects of lifestyle among boys compared to girls[36].
Factors that improve glycemic control: Glycemic level in the school age children had significantly improved during the lockdown period, which may be attributed to more supervision of insulin injections and overall health care from their parents[48]. On the contrary, the pubertal adolescents group showed an adverse trend, which may be attributed to a change in independence from the parents during this age and more pressure from peer and themselves[36].
Although children and adolescents performed less physical activity and engaged in more sedentary behavior during the lockdown which impeded glycemic control, the changes in eating habits seemed to play a more essential role in glycemic management[49]. Healthy diet is essential for glycemic control. Evidence revealed that hyperglycemia is a significant predictor of some viral infections including COVID-19 which can exacerbate the complications of diabetes mellitus (DM)[50]. According to the literature review, adequate intake of dietary protein, fiber, essential fatty acids, and some micronutrients especially vitamins D, C, and B12, folate, zinc and selenium are beneficial to the prevention and treatment of COVID-19 in diabetic patients through modulation of innate and adaptive immune responses or direct effects on virus enzymes or cell entrance[50]. Due to home confinement, parents may monitor their children’s behavior throughout the day. Particularly, compared to those with a longer duration of the disease, children with newly diagnosed or less than a year diabetes got more benefit from improvement in eating behaviors, which may be partially ascribed by taking over diabetes control from their caregivers[51]. Furthermore, outside dining and junk food consumption are prone to be limited due to the lockdown, which may have reduced opportunities to adopt or engage in the unhealthy dietary habits or weight control practices that have been frequently observed in youths with diabetes[43,52]. In addition, the isolation measures may have reduced or canceled activities and contexts typically linked to social situation with peers that usually challenge good diabetes management and lead to behaviors negatively influencing glycemic control[53]. However, in certain areas, because of strict lockdown and suspension of food supplies, regular supply of important components of their healthy diet plan may be not available, which obstructs medical nutrition therapy and deserves the concern of government[54].
Hard time for caregivers of T1D children: Before the pandemic, caregivers played a fundamental role in family diabetes control and short or long-term consequence resolving[55]. Pediatric T1D is a very fragile context, in which the pandemic can lead to emotional adaptation disorders[56]. In some families of children and adolescents with T1D, the school nurse provided most of the diabetes care. However, because of the sudden closure of school, parents who needed extra help may have less access to adequate training[38]. The unavailability of medical appointments, the lack of information about the relationship between COVID-19 and T1D, the difficulty in obtaining specialized support, and the inability to provide quality food and supplies for diabetes during the pandemic may generate negative feelings and insecurity in these caregivers[57,58]. Ultimately, the emotional burden of caregivers might not only influence the parents’ mental health, but also negatively affect blood sugar control of their children[59].
Challenges related to the healthcare system: Patients with T1DM require continuous access to healthcare services. However, the lockdown and closure of healthcare centers may deprive these patients of access to medical support for their daily disease management and complication treatment. In addition, emergency issues like hypoglycemia or DKA requiring hospitalization may be precipitated, while infections such as COVID-19 or any other cases, may also lead to glycemic fluctuations and increase the risk of hospitalization[43,60]. How to deal with all the factors mentioned above poses challenges for the healthcare system.
Self-management: Patients with T1DM need to adhere to frequent glucose monitoring, proper dietary behaviors, adequate hydration, and dose titration of glucose-lowering medication. As signified in publications, the up-to-date medical devices and test methods may bring convenience to these procedures. For instance, continuous glucose monitoring (CGM) and fast glucose monitoring systems are proved to be useful[61]. Moreover, percentage time in range and other CGM-derived metrics are the substitutes of HbA1c in the absence of routine laboratory tests related to the pandemic, which are potential to monitor the glycemic control[62]. Meanwhile, transitioning to CGM indicates “fewer finger punctures and less pain” for children and caregivers can constantly monitor the insulin level with the device[63]. In addition, the insulin pump allows T1D patients to achieve a better control as it tracks the glucose level and injects a proper dose of insulin automatically, thus generating a more comfortable alternative compared to multiple daily insulin injections[64].
The importance of management in sick days should be highlighted to avoid glycemic fluctuations and subsequent risk of DKA or hypoglycemia. As mentioned in publications, when children with T1D are under stress and acute infections, less food intake and more stress hormones may affect glycemic control, therefore it should be cautioned about the rising risk of either hyperglycemia or hypoglycemia[65]. Moreover, patients are recommended to take symptomatic therapy to reduce fever[66]. Ultimately, regular education about diabetes-related symptoms may contribute to a faster diagnosis of T1D and reduce the prevalence of DKA in children and adolescents, along with more rigorous adherence to “sick-day rules” which are recommended to diagnosed T1D patients[67].
Mental outcomes of the COVID-19 pandemic should be taken into consideration in the further treatment plan for children and adolescents with T1D[56]. To vent out distress, the most common method was sharing problems with companions[68].
Physical activities: As recommended by the World Health Organization, young people are supposed to practice more than 1 h per day, doing moderate or vigorous intensity physical activity[69]. However, the physical activity level of T1D children was low before the lockdown and further reduced in the pandemic[36]. Therefore, innovative methods such as appropriate indoor exercises may be a potential way to maintain or lift physical activity levels during the restriction of outdoor activities[36]. For instance, taking online physical training which provides various indoor exercise selections could be a beneficial choice for teenagers.
Use of telemedicine: A move towards telemonitoring to provide healthcare services for patients with diabetes has been part of a long-term plan in the management of the disease[70]. Hopefully, the public health emergency of the COVID-19 pandemic has accelerated the process[71]. Telemedicine services means that digital services substitute for the routine care to offer reviews and self-management advice on diabetes[71]. Telemedicine consultation minimizes the risk of virus transmission by maintaining physical distancing, while remote monitoring of electronic data enables health-care workers to provide in-time support in patients with worsening condition based on available data, which may benefit clinical outcomes[72].
However, there are still limitations in telemedicine including unavailability to perform a suitable physical examination, obstacles in wide spread because of difficulty of Internet construction in certain regions and populations, and challenges in establishing harmonious relationship with patients or helping resolve behavior problems or making effective communication and gaining collaboration[73,74]. In addition, it should be emphasized that in-clinic visits are indispensable in some care processes at a certain frequency. Meanwhile, patients with a more acute disease including DKA or hyperosmolar hyperglycemic state should not simply adapt the transition to telemedicine[75]. Moreover, insulin initiation in new-onset T1D is typically required in in-clinic attendance and face-to-face training. Therefore, in the future, telemedicine is not merely about keeping patients away from hospitals, but it is about knowing who should be asked to come to the clinic and when at the same time[71].
Relieving the stress of caregivers: There are several possible strategies that should be used to reduce the mental impact on caregivers[58]. To begin with, channels for these caregivers’ voice and guidance on emotional self-relief should be provided to eliminate the sense of overloading[58]. In addition, the multidisciplinary ways which provide physical, psychological, and nutritional guidance for children and adolescents with T1D should be economically accessible[58]. Nevertheless, creating social media groups to promote peer interaction in communicating their perceptions and helping each other could be beneficial[58].
Responsibility of medical providers: The whole is greater than the sum of its parts. To provide efficient help, local support groups should coordinate with the hospital team for better T1D management[43]. Interdisciplinary collaboration via staff meetings or other forms at a regular basis improves patient care equality, allowing medical providers to learn from others and perform medical service from a more holistic view[74,76]. To connect with individual patients, clinics should ask families about stress on finance and society due to the pandemic, which may influence their coordination with medical providers as well[74].
Furthermore, it was reported that interventions of glycemic management employed during the first two cycles did not produce satisfying outcomes for any target. However, in the 3rd cycle of intervention, the screening and consultation rates increased[74]. Therefore, it should be highlighted that persistent efforts make sense.
The minireview is based on the articles mostly reported in English, which limits the extrapolation of results across the globe. Moreover, in most of the research, assessments of glycemic control were only based on HbA1c instead of the home blood glucose levels due to a variety of reasons. Additionally, albeit the use of self-reported measures administered online overcomes the impossibility of conducting a traditional paper survey during the pandemic, it may lead to imprecise ratings of specific anthropometric and clinical data, and subjective perceptions and behaviors. Similarly, thoughts and feelings may not have been sincerely, accurately, or fully revealed[77]. Notwithstanding the above limitations, all studies provide an invaluable report about the difficulties met by youths with T1D and promising solutions.
T1D is one of the most common endocrine metabolic disorders around the world[78]. Children with T1D are imperiled by psychological issues, owing to the underlying disease and the complex management of diabetes[79]. As discussed in the minireview, children and adolescents with diabetes are vulnerable to the COVID-19 pandemic resulting in worsening healthcare and would need specific medical access in this period for health advice and support. In addition, they are encouraged to keep a healthy lifestyle whenever possible during these difficult times. In addition, emotional overload leads to exhaustion in youths with T1D diabetes and those who are responsible to take care of them. More than ever, the mental well-being of T1D children and adolescents and their caregivers should be prioritized, and coping strategies should be advocated[58]. Moreover, the COVID-19 pandemic is an opportunity for telemedicine development and puts it to the forefront of diabetes management. Besides distant management of diabetes, identifying the at-risk groups to provide in-person consultation and care is also the value of routine telemonitoring[71]. Ultimately, cooperation and continuous effort should be made among medical providers, families with T1D youths, and the whole society.
In summary, we can conclude that youths with T1D require continuous care and attention during the COVID-19 pandemic because of various issues as discussed above. Proposed solutions in this article may assist them to resolve these obstacles in diabetes management to reduce the risk of complications particularly DKA during such emergency situations. Furthermore, proper prospective studies need to be conducted to identify the challenges faced by youths with T1DM during lockdown and their influence on glycemic control and complications, which may help us to come to more precise solutions to improve the welfare of children and adolescents with T1D during such pandemic.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Associate Member of American Association for Cancer Research, 1075629.
Specialty type: Pediatrics
Country/Territory of origin: Singapore
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Abdelbasset WK, Saudi Arabia; Moshref RH, Saudi Arabia; Virarkar M, United States S-Editor: Wang LL L-Editor: Wang TQ P-Editor: Wang LL
| 1. | DiMeglio LA, Evans-Molina C, Oram RA. Type 1 diabetes. Lancet. 2018;16:2449-2462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 595] [Cited by in RCA: 967] [Article Influence: 138.1] [Reference Citation Analysis (0)] |
| 2. | Writing Group for the SEARCH for Diabetes in Youth Study Group. Dabelea D, Bell RA, D'Agostino RB Jr, Imperatore G, Johansen JM, Linder B, Liu LL, Loots B, Marcovina S, Mayer-Davis EJ, Pettitt DJ, Waitzfelder B. Incidence of diabetes in youth in the United States. JAMA. 2007;297:2716-2724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 688] [Cited by in RCA: 686] [Article Influence: 38.1] [Reference Citation Analysis (0)] |
| 3. | WHO. Coronavirus disease 2019 (COVID-19): situation report, 75. [cited 20 April 2022]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. |
| 4. | Kretchy IA, Asiedu-Danso M, Kretchy JP. Medication management and adherence during the COVID-19 pandemic: Perspectives and experiences from low-and middle-income countries. Res Social Adm Pharm. 2021;17:2023-2026. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 152] [Cited by in RCA: 179] [Article Influence: 44.8] [Reference Citation Analysis (0)] |
| 5. | DiMeglio LA, Evans-Molina C, Oram RA. Type 1 diabetes. Lancet. 16:2449-2462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 595] [Cited by in RCA: 967] [Article Influence: 138.1] [Reference Citation Analysis (0)] |
| 6. | Donaghue KC, Marcovecchio ML, Wadwa RP, Chew EY, Wong TY, Calliari LE, Zabeen B, Salem MA, Craig ME. ISPAD Clinical Practice Consensus Guidelines 2018: Microvascular and macrovascular complications in children and adolescents. Pediatr Diabetes. 2018;19 Suppl 27:262-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 195] [Article Influence: 27.9] [Reference Citation Analysis (0)] |
| 7. | Noser AE, Patton SR, Van Allen J, Nelson MB, Clements MA. Evaluating Parents' Self-Efficacy for Diabetes Management in Pediatric Type 1 Diabetes. J Pediatr Psychol. 2017;42:296-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Ferguson SC, Blane A, Wardlaw J, Frier BM, Perros P, McCrimmon RJ, Deary IJ. Influence of an early-onset age of type 1 diabetes on cerebral structure and cognitive function. Diabetes Care. 2005;28:1431-1437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 173] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 9. | Orioli L, Hermans MP, Thissen JP, Maiter D, Vandeleene B, Yombi JC. COVID-19 in diabetic patients: Related risks and specifics of management. Ann Endocrinol (Paris). 2020;81:101-109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 54] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 10. | Knapp S. Diabetes and infection: is there a link? Gerontology. 2013;59:99-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 221] [Article Influence: 17.0] [Reference Citation Analysis (1)] |
| 11. | Carey IM, Critchley JA, DeWilde S, Harris T, Hosking FJ, Cook DG. Risk of Infection in Type 1 and Type 2 Diabetes Compared With the General Population: A Matched Cohort Study. Diabetes Care. 2018;41:513-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 272] [Cited by in RCA: 418] [Article Influence: 59.7] [Reference Citation Analysis (0)] |
| 12. | Casqueiro J, Casqueiro J, Alves C. Infections in patients with diabetes mellitus: A review of pathogenesis. Indian J Endocrinol Metab. 2012;16 Suppl 1:S27-S36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 377] [Cited by in RCA: 515] [Article Influence: 39.6] [Reference Citation Analysis (0)] |
| 13. | Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054-1062. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17476] [Cited by in RCA: 18194] [Article Influence: 3638.8] [Reference Citation Analysis (0)] |
| 14. | Bode B, Garrett V, Messler J, McFarland R, Crowe J, Booth R, Klonoff DC. Glycemic Characteristics and Clinical Outcomes of COVID-19 Patients Hospitalized in the United States. J Diabetes Sci Technol. 2020;14:813-821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 462] [Cited by in RCA: 484] [Article Influence: 96.8] [Reference Citation Analysis (0)] |
| 15. | Chen Y, Yang D, Cheng B, Chen J, Peng A, Yang C, Liu C, Xiong M, Deng A, Zhang Y, Zheng L, Huang K. Clinical Characteristics and Outcomes of Patients With Diabetes and COVID-19 in Association With Glucose-Lowering Medication. Diabetes Care. 2020;43:1399-1407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 276] [Cited by in RCA: 273] [Article Influence: 54.6] [Reference Citation Analysis (0)] |
| 16. | Holman N, Knighton P, Kar P, O'Keefe J, Curley M, Weaver A, Barron E, Bakhai C, Khunti K, Wareham NJ, Sattar N, Young B, Valabhji J. Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study. Lancet Diabetes Endocrinol. 2020;8:823-833. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 620] [Cited by in RCA: 612] [Article Influence: 122.4] [Reference Citation Analysis (0)] |
| 17. | Paternoster G, Sartini C, Pennacchio E, Lisanti F, Landoni G, Cabrini L. Awake pronation with helmet continuous positive airway pressure for COVID-19 acute respiratory distress syndrome patients outside the ICU: A case series. Med Intensiva (Engl Ed). 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 18. | Mantovani A, Byrne CD, Zheng MH, Targher G. Diabetes as a risk factor for greater COVID-19 severity and in-hospital death: A meta-analysis of observational studies. Nutr Metab Cardiovasc Dis. 2020;30:1236-1248. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 208] [Cited by in RCA: 188] [Article Influence: 37.6] [Reference Citation Analysis (0)] |
| 19. | Fadini GP, Morieri ML, Longato E, Avogaro A. Prevalence and impact of diabetes among people infected with SARS-CoV-2. J Endocrinol Invest. 2020;43:867-869. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 294] [Cited by in RCA: 334] [Article Influence: 66.8] [Reference Citation Analysis (0)] |
| 20. | Cuschieri S, Grech S. COVID-19 and diabetes: The why, the what and the how. J Diabetes Complications. 2020;34:107637. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 80] [Cited by in RCA: 80] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 21. | Caruso P, Longo M, Esposito K, Maiorino MI. Type 1 diabetes triggered by covid-19 pandemic: A potential outbreak? Diabetes Res Clin Pract. 2020;164:108219. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 22. | Op de Beeck A, Eizirik DL. Viral infections in type 1 diabetes mellitus--why the β cells? Nat Rev Endocrinol. 2016;12:263-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 209] [Article Influence: 23.2] [Reference Citation Analysis (0)] |
| 23. | Yang WL, Li Q, Sun J, Huat Tan S, Tang YH, Zhao MM, Li YY, Cao X, Zhao JC, Yang JK. Potential drug discovery for COVID-19 treatment targeting Cathepsin L using a deep learning-based strategy. Comput Struct Biotechnol J. 2022;20:2442-2454. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 13] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 24. | Uto H, Matsuoka H, Murata M, Okamoto T, Miyata Y, Hori T, Ido A, Hirono S, Hayashi K, Tsubouchi H. A case of chronic hepatitis C developing insulin-dependent diabetes mellitus associated with various autoantibodies during interferon therapy. Diabetes Res Clin Pract. 2000;49:101-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 25. | Doğan Eİ, Kurt BÖ. New-onset or Exacerbated Occupational Hand Eczema among Healthcare Workers During the COVID-19 Pandemic: A Growing Health Problem. Acta Dermatovenerol Croat. 2021;291:21-29. [PubMed] |
| 26. | Imanova Yaghji N, Kan EK, Akcan S, Colak R, Atmaca A. Hydroxychloroquine Sulfate Related Hypoglycemia In A Non-Diabetic COVİD-19 Patient: A Case Report and Literature Review. Postgrad Med. 2021;133:548-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 27. | Halaby MJ, Kastein BK, Yang DQ. Chloroquine stimulates glucose uptake and glycogen synthase in muscle cells through activation of Akt. Biochem Biophys Res Commun. 2013;435:708-713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 28. | Li J, Wang X, Chen J, Zuo X, Zhang H, Deng A. COVID-19 infection may cause ketosis and ketoacidosis. Diabetes Obes Metab. 2020;22:1935-1941. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 285] [Cited by in RCA: 392] [Article Influence: 78.4] [Reference Citation Analysis (0)] |
| 29. | Smith SM, Boppana A, Traupman JA, Unson E, Maddock DA, Chao K, Dobesh DP, Brufsky A, Connor RI. Impaired glucose metabolism in patients with diabetes, prediabetes, and obesity is associated with severe COVID-19. J Med Virol. 2021;93:409-415. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 89] [Cited by in RCA: 126] [Article Influence: 25.2] [Reference Citation Analysis (0)] |
| 30. | Ho J, Rosolowsky E, Pacaud D, Huang C, Lemay JA, Brockman N, Rath M, Doulla M. Diabetic ketoacidosis at type 1 diabetes diagnosis in children during the COVID-19 pandemic. Pediatr Diabetes. 2021;22:552-557. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 74] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 31. | Cherubini V, Gohil A, Addala A, Zanfardino A, Iafusco D, Hannon T, Maahs DM. Unintended Consequences of Coronavirus Disease-2019: Remember General Pediatrics. J Pediatr. 2020;223:197-198. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 65] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 32. | Croft A, Bucca A, Jansen JH, Motzkus C, Herbert A, Wang A, Hunter BR. First-time Diabetic Ketoacidosis in Type 2 Diabetics With COVID-19 Infection: A Novel Case Series. J Emerg Med. 2020;59:e193-e197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 33. | Dżygało K, Nowaczyk J, Szwilling A, Kowalska A. Increased frequency of severe diabetic ketoacidosis at type 1 diabetes onset among children during COVID-19 pandemic lockdown: an observational cohort study. Pediatr Endocrinol Diabetes Metab. 2020;26:167-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 57] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 34. | Kostopoulou E, Eliopoulou MI, Rojas Gil AP, Chrysis D. Impact of COVID-19 on new-onset type 1 diabetes mellitus - A one-year prospective study. Eur Rev Med Pharmacol Sci. 2021;25:5928-5935. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 35. | Cheng HP, Wong JSL, Selveindran NM, Hong JYH. Impact of COVID-19 lockdown on glycaemic control and lifestyle changes in children and adolescents with type 1 and type 2 diabetes mellitus. Endocrine. 2021;73:499-506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 36. | Nicola M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, Iosifidis C, Agha M, Agha R. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int J Surg. 2020;78:185-193. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2872] [Cited by in RCA: 2681] [Article Influence: 536.2] [Reference Citation Analysis (0)] |
| 37. | Gayoso M, Lim WY, Mulekar MS, Kaulfers AD. Effect of COVID-19 quarantine on diabetes Care in Children. Clin Diabetes Endocrinol. 2021;7:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 38. | Johns C, Faulkner MS, Quinn L. Characteristics of adolescents with type 1 diabetes who exhibit adverse outcomes. Diabetes Educ. 2008;34:874-885. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 39. | Borschuk AP, Everhart RS. Health disparities among youth with type 1 diabetes: A systematic review of the current literature. Fam Syst Health. 2015;33:297-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 61] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 40. | Kumar KM, Saboo B, Rao PV, Sarda A, Viswanathan V, Kalra S, Sethi B, Shah N, Srikanta SS, Jain SM, Raghupathy P, Shukla R, Jhingan A, Chowdhury S, Jabbar PK, Kanungo A, Joshi R, Kumar S, Tandon N, Khadilkar V, Chadha M. Type 1 diabetes: Awareness, management and challenges: Current scenario in India. Indian J Endocrinol Metab. 2015;19:S6-S8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 41. | Odeh R, Gharaibeh L, Daher A, Kussad S, Alassaf A. Caring for a child with type 1 diabetes during COVID-19 lockdown in a developing country: Challenges and parents' perspectives on the use of telemedicine. Diabetes Res Clin Pract. 2020;168:108393. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 42] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 42. | Jethwani P, Saboo B, Jethwani L, Kesavadev J, Kalra S, Sahay R, Agarwal S, Hasnani D. Management of children and adolescents having type 1 diabetes during COVID-19 pandemic in India: challenges and solutions. Int J Diabetes Dev Ctries. 2020;1-5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 43. | Gerstl EM, Rabl W, Rosenbauer J, Gröbe H, Hofer SE, Krause U, Holl RW. Metabolic control as reflected by HbA1c in children, adolescents and young adults with type-1 diabetes mellitus: combined longitudinal analysis including 27,035 patients from 207 centers in Germany and Austria during the last decade. Eur J Pediatr. 2008;167:447-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 161] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 44. | Springer D, Dziura J, Tamborlane WV, Steffen AT, Ahern JH, Vincent M, Weinzimer SA. Optimal control of type 1 diabetes mellitus in youth receiving intensive treatment. J Pediatr. 2006;149:227-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 69] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 45. | Agarwal N, Harikar M, Shukla R, Bajpai A. COVID-19 pandemic: a double trouble for Indian adolescents and young adults living with type 1 diabetes. Int J Diabetes Dev Ctries. 2020;40:346-352. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 46. | Özdin S, Bayrak Özdin Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. Int J Soc Psychiatry. 2020;66:504-511. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 854] [Cited by in RCA: 708] [Article Influence: 141.6] [Reference Citation Analysis (0)] |
| 47. | Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S, Wang Y, Fu H, Dai J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One. 2020;15:e0231924. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1367] [Cited by in RCA: 1297] [Article Influence: 259.4] [Reference Citation Analysis (0)] |
| 48. | Dunton GF, Do B, Wang SD. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health. 2020;20:1351. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 603] [Cited by in RCA: 513] [Article Influence: 102.6] [Reference Citation Analysis (0)] |
| 49. | Marigliano M, Maffeis C. Glycemic control of children and adolescents with type 1 diabetes improved after COVID-19 lockdown in Italy. Acta Diabetol. 2021;58:661-664. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 50. | Elhenawy YI, Eltonbary KY. Glycemic control among children and adolescents with type 1 diabetes during COVID-19 pandemic in Egypt: a pilot study. Int J Diabetes Dev Ctries. 2021;41:389-395. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 51. | Howe CJ, Jawad AF, Kelly SD, Lipman TH. Weight-related concerns and behaviors in children and adolescents with type 1 diabetes. J Am Psychiatr Nurses Assoc. 2008;13:376-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 52. | Palladino DK, Helgeson VS. Friends or foes? J Pediatr Psychol. 2012;37:591-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 73] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 53. | Smart CE, Annan F, Higgins LA, Jelleryd E, Lopez M, Acerini CL. ISPAD Clinical Practice Consensus Guidelines 2018: Nutritional management in children and adolescents with diabetes. Pediatr Diabetes. 2018;19 Suppl 27:136-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 127] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 54. | Harrington KR, Boyle CT, Miller KM, Hilliard ME, Anderson BJ, Van Name M, DiMeglio LA, Laffel LM; T1D Exchange Clinic Network. Management and Family Burdens Endorsed by Parents of Youth <7 Years Old With Type 1 Diabetes. J Diabetes Sci Technol. 2017;11:980-987. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 39] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 55. | Carducci C, Rapini N, Deodati A, Pampanini V, Cianfarani S, Schiaffini R. Post-traumatic stress disorder (PTSD) in parents of children with type 1 diabetes during COVID-19 pandemic. Ital J Pediatr. 2021;47:176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 56. | Commissariat PV, Harrington KR, Whitehouse AL, Miller KM, Hilliard ME, Van Name M, DeSalvo DJ, Tamborlane WV, Anderson BJ, DiMeglio LA, Laffel LM. "I'm essentially his pancreas": Parent perceptions of diabetes burden and opportunities to reduce burden in the care of children <8 years old with type 1 diabetes. Pediatr Diabetes. 2020;21:377-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 63] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 57. | Alessi J, de Oliveira GB, Erthal IN, Teixeira JB, Morello MS, Ribeiro RJE, de Carvalho TR, Jaeger EH, Schaan BD, Telo GH. "Not having a minute of self-distancing during the social distancing is exhausting": a qualitative study on the perspective of caregivers of youth with type 1 diabetes during the COVID-19 pandemic. Acta Diabetol. 2021;58:1533-1540. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 58. | Van Gampelaere C, Luyckx K, Van Ryckeghem DML, van der Straaten S, Laridaen J, Goethals ER, Casteels K, Vanbesien J, den Brinker M, Cools M, Goubert L. Mindfulness, Worries, and Parenting in Parents of Children With Type 1 Diabetes. J Pediatr Psychol. 2019;44:499-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 59. | Brink S, Joel D, Laffel L, Lee WW, Olsen B, Phelan H, Hanas R; International Society for Pediatric and Adolescent Diabetes. ISPAD Clinical Practice Consensus Guidelines 2014. Sick day management in children and adolescents with diabetes. Pediatr Diabetes. 2014;15 Suppl 20:193-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 60. | Caballero AE, Ceriello A, Misra A, Aschner P, McDonnell ME, Hassanein M, Ji L, Mbanya JC, Fonseca VA. COVID-19 in people living with diabetes: An international consensus. J Diabetes Complications. 2020;34:107671. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 96] [Cited by in RCA: 82] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 61. | Danne T, Nimri R, Battelino T, Bergenstal RM, Close KL, DeVries JH, Garg S, Heinemann L, Hirsch I, Amiel SA, Beck R, Bosi E, Buckingham B, Cobelli C, Dassau E, Doyle FJ 3rd, Heller S, Hovorka R, Jia W, Jones T, Kordonouri O, Kovatchev B, Kowalski A, Laffel L, Maahs D, Murphy HR, Nørgaard K, Parkin CG, Renard E, Saboo B, Scharf M, Tamborlane WV, Weinzimer SA, Phillip M. International Consensus on Use of Continuous Glucose Monitoring. Diabetes Care. 2017;40:1631-1640. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1375] [Cited by in RCA: 1377] [Article Influence: 172.1] [Reference Citation Analysis (0)] |
| 62. | Şahinol, M. , Başkavak, G. Contested Daily Routines, Contested Care. Children with Type 1 Diabetes in COVID-19 Times. Childhood Vulnerability. 2021;3:23-40. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 63. | Bergenstal RM, Tamborlane WV, Ahmann A, Buse JB, Dailey G, Davis SN, Joyce C, Peoples T, Perkins BA, Welsh JB, Willi SM, Wood MA; STAR 3 Study Group. Effectiveness of sensor-augmented insulin-pump therapy in type 1 diabetes. N Engl J Med. 2010;363:311-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 670] [Cited by in RCA: 605] [Article Influence: 40.3] [Reference Citation Analysis (0)] |
| 64. | Chiang JL, Maahs DM, Garvey KC, Hood KK, Laffel LM, Weinzimer SA, Wolfsdorf JI, Schatz D. Type 1 Diabetes in Children and Adolescents: A Position Statement by the American Diabetes Association. Diabetes Care. 2018;41:2026-2044. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 295] [Cited by in RCA: 290] [Article Influence: 41.4] [Reference Citation Analysis (0)] |
| 65. | Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL, Boehm B, Amiel S, Holt RI, Skyler JS, DeVries JH, Renard E, Eckel RH, Zimmet P, Alberti KG, Vidal J, Geloneze B, Chan JC, Ji L, Ludwig B. Practical recommendations for the management of diabetes in patients with COVID-19. Lancet Diabetes Endocrinol. 2020;8:546-550. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 535] [Cited by in RCA: 562] [Article Influence: 112.4] [Reference Citation Analysis (0)] |
| 66. | Lee AA, Piette JD, Heisler M, Rosland AM. Diabetes Distress and Glycemic Control: The Buffering Effect of Autonomy Support From Important Family Members and Friends. Diabetes Care. 2018;41:1157-1163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 72] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 67. | Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, Carty C, Chaput JP, Chastin S, Chou R, Dempsey PC, DiPietro L, Ekelund U, Firth J, Friedenreich CM, Garcia L, Gichu M, Jago R, Katzmarzyk PT, Lambert E, Leitzmann M, Milton K, Ortega FB, Ranasinghe C, Stamatakis E, Tiedemann A, Troiano RP, van der Ploeg HP, Wari V, Willumsen JF. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54:1451-1462. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4541] [Cited by in RCA: 5364] [Article Influence: 1072.8] [Reference Citation Analysis (1)] |
| 68. | Bain SC, Czernichow S, Bøgelund M, Madsen ME, Yssing C, McMillan AC, Hvid C, Hettiarachchige N, Panton UH. Costs of COVID-19 pandemic associated with diabetes in Europe: a health care cost model. Curr Med Res Opin. 2021;37:27-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 69. | Danne T, Limbert C, Puig Domingo M, Del Prato S, Renard E, Choudhary P, Seibold A. Telemonitoring, Telemedicine and Time in Range During the Pandemic: Paradigm Change for Diabetes Risk Management in the Post-COVID Future. Diabetes Ther. 2021;12:2289-2310. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 27] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 70. | Castle JR, Rocha L, Ahmann A. How COVID-19 Rapidly Transformed Clinical Practice at the Harold Schnitzer Diabetes Health Center Now and for the Future. J Diabetes Sci Technol. 2020;14:721-722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 71. | Espinoza J, Shah P, Raymond J. Integrating Continuous Glucose Monitor Data Directly into the Electronic Health Record: Proof of Concept. Diabetes Technol Ther. 2020;22:570-576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 72. | Brodar KE, Hong N, Liddle M, Hernandez L, Waks J, Sanchez J, Delamater A, Davis E. Transitioning to Telehealth Services in a Pediatric Diabetes Clinic During COVID-19: An Interdisciplinary Quality Improvement Initiative. J Clin Psychol Med Settings. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 73. | Choudhary P, Wilmot EG, Owen K, Patel DC, Mills L, Rayman G, Winocour P, Ayman G, Patel R, Hambling C, Nagi DK. A roadmap to recovery: ABCD recommendations on risk stratification of adult patients with diabetes in the post-COVID-19 era. Diabet Med. 2021;38:e14462. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 74. | Powell PW, Corathers SD, Raymond J, Streisand R. New approaches to providing individualized diabetes care in the 21st century. Curr Diabetes Rev. 2015;11:222-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 42] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 75. | Troncone A, Chianese A, Zanfardino A, Cascella C, Piscopo A, Borriello A, Rollato S, Casaburo F, Testa V, Iafusco D. Disordered eating behaviors in youths with type 1 diabetes during COVID-19 lockdown: an exploratory study. J Eat Disord. 2020;8:76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 76. | Tuomilehto J. The emerging global epidemic of type 1 diabetes. Curr Diab Rep. 2013;13:795-804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 190] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 77. | Rubin RR, Peyrot M. Psychological issues and treatments for people with diabetes. J Clin Psychol. 2001;57:457-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 173] [Article Influence: 7.2] [Reference Citation Analysis (0)] |