Published online May 9, 2021. doi: 10.5409/wjcp.v10.i3.40
Peer-review started: January 5, 2021
First decision: January 25, 2021
Revised: February 4, 2021
Accepted: March 10, 2021
Article in press: March 10, 2021
Published online: May 9, 2021
Processing time: 113 Days and 11.6 Hours
Chilaiditi syndrome is a rare disorder characterized by the hepatodiaphragmatic interposition of the intestine.
Here we report a case of a 12-year-old male who was admitted to the pediatric intensive care unit secondary to abdominal pain and severe respiratory distress. He was treated conservatively but the symptoms persisted requiring a surgical approach. While there have been several cases of Chilaiditi syndrome reported in adults, there is a scarcity of cases reported in the pediatric population. Our review of the literature found only 30 pediatric cases, including our reported case, with Chilaiditi syndrome, 19 (63%) of which were male. The median age of diagnosis was 4.5 years old with an interquartile range of 2.0-10.0 years. In our review, we found that the most common predisposing factors in children are aerophagia (12/30 cases) and constipation (13/30 cases). Ninety percent of the cases presented with complete intestinal interposition, in 100% of which, the colon was involved. Three of the 30 cases were associated with volvulus.
In the pediatric population, conservative (21/30 cases) and surgical (8/30 cases) treatment approaches have produced satisfactory outcomes for all the patients, regardless of approach.
Core Tip: We describe a pediatric case of Chilaiditi syndrome with successful treatment, as well as a literature review of all pediatric case reports of Chilaiditi syndrome. In the pediatric patients, both conservative and surgical approaches in treating Chilaiditi syndrome with treatment of predisposing factors have resulted in satisfactory outcomes.
- Citation: Caicedo L, Wasuwanich P, Rivera A, Lopez MS, Karnsakul W. Chilaiditi syndrome in pediatric patients - Symptomatic hepatodiaphragmatic interposition of colon: A case report and review of literature. World J Clin Pediatr 2021; 10(3): 40-47
- URL: https://www.wjgnet.com/2219-2808/full/v10/i3/40.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v10.i3.40
Chilaiditi syndrome, first described by Viennese radiologist Dr. Chilaiditi[1] in 1910, is noted to be an extremely rare disorder associated with various symptoms including nausea, vomiting, abdominal pain, constipation, and respiratory distress. The condition is recognized radiologically by the presence of the hepatodiaphragmatic interposition of the intestine, called Chilaiditi sign. Chilaiditi sign can be confused radiologically with other conditions such as pneumoperitoneum and subdiaphrag
A 12-year-old male was admitted to the pediatric intensive care unit due to severe respiratory distress.
With this present admission, the patient presented with respiratory distress and right upper quadrant abdominal pain. He was placed on oxygen supplementation via nasal cannula to maintain normal oxygen saturations.
Prior to this admission, he experienced persistent cough, dyspnea, nausea, and chest pain for over two months. He was prescribed antibiotics, nebulizations, and pain medication; however, there were no improvements in his respiratory symptoms. The patient has a history of asthma, gastroesophageal reflux disease, constipation, and a prior diagnosis of Chilaiditi syndrome. The diagnosis of Chilaiditi syndrome was made two years prior to this admission when the patient presented with a one-week history of right upper quadrant pain, nausea, and vomiting. There was no history of recent weight loss. An abdominal computerized tomography (CT) showed cons
No relevant family history.
No relevant physical examination.
Laboratory results from complete blood count, comprehensive metabolic panel, and C-reactive protein were within normal limits.
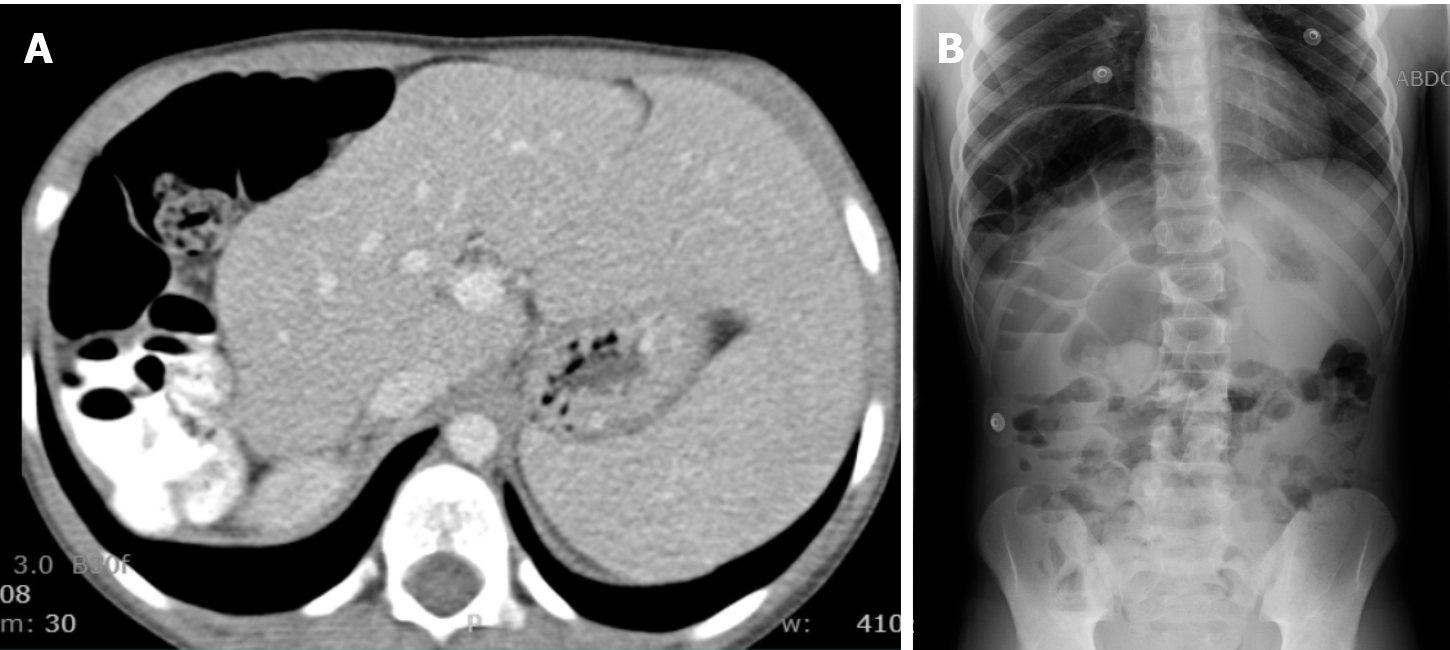
A chest X-ray revealed that the transverse colon was above the liver. On the first hospital admission day, a kidney, ureter, and bladder X-ray (KUB) showed significant amount of fecal material and air-filled colonic loops which were slightly dilated and reaching the right hemidiaphragm (Figure 1).
A final diagnosis of Chilaiditi syndrome was given.
He subsequently received a bowel-cleaning regimen with GoLytely®. A follow-up KUB on the second hospital admission day showed the resolution of fecal retention or constipation. However, the patient continued to complain of tachypnea and right upper quadrant pain. Because of his persistent respiratory and abdominal symptoms, and due to the lack of significant improvement, surgery was consulted. The patient underwent laparoscopic colopexy and peritoneal abrasion of the diaphragm and liver. Significant intraoperative findings included a redundant transverse colon, no evidence of volvulus or adhesions in the upper abdomen, a relatively small right liver lobe (noncirrhotic), and a large gap between the liver and the anterior chest wall and diaphragm.
His respiratory distress and abdominal pain resolved completely post-operatively and the patient was discharged with a maintenance stool softener regimen, colonic stimulant, and adequate dietary fiber. At the one-month follow-up after surgery, the patient reported regular bowel movements and no recurrence of his respiratory distress. He reported some mild intermittent episodes of right upper quadrant abdominal pain but never required emergency care or any interventions since the surgery.
The essential hallmark of Chilaiditi sign in Chilaiditi syndrome is that the air-filled loops of intestine remain unchanged in position of the patients due to its immobi
| Ref. | Sex | Age | Predisposition | Bowel segment | Symptoms | Type of interposition | Dx procedure | Treatment | Type of surgery | Outcome |
| [24] | M | 16 mo | Aerophagia | Colon | Abdominal distention and pain, vomiting | Complete | KUB | Conservative | --- | Resolution |
| [24] | F | 3 yr | Aerophagia | Colon | Abdominal distention and pain, passed flatus | Complete | KUB | Conservative | --- | Resolution |
| [24] | F | 5 yr | Aerophagia, constipation | Colon | Abdominal pain, constipation | Partial | KUB | Conservative | --- | Resolution |
| [24] | F | 4 yr | Aerophagia | Colon | Anorexia, recurrent abdominal pain, vomiting | Complete | KUB | Conservative | --- | Resolution |
| [27] | F | 2 yr | --- | Colon | Marasmus, vomiting, lethargy, inability to walk | Complete | KUB | Surgery (Volvulus) | Laparoscopic colopexy and transverse colectomy | Resolution |
| [26] | M | 6 mo | --- | Colon | Abdominal pain, vomiting | Partial | KUB | Conservative | --- | Resolution |
| [19] | M | 8 yr | Aerophagia | Colon | Abdominal pain, distention | Complete | KUB | Conservative | --- | Resolution |
| [7] | M | 12 yr | --- | Colon | Respiratory distress, pleuritic pain, fever | Complete | CXR, BE | Surgical (Volvulus) | Laparoscopic detorsion | Resolution |
| [22] | M | 17 yr | Mental retardation, constipation, congenital adhesions | Colon | Abdominal distention, vomiting, constipation | Complete | CXR, KUB | Surgical (Volvulus) | Laparoscopic transverse colectomy | Resolution |
| [28] | F | 9 yr | Constipation | Colon | Abdominal pain, nausea, constipation | Complete | CXR, KUB | Conservative | --- | Resolution |
| [9] | F | 11 yr | Constipation | Colon | Abdominal pain, vomiting | Complete | KUB, CT | Surgery | Laparoscopic transverse colectomy | Resolution |
| [23] | F | 9 yr | DE, constipation | Colon | Epigastric pain, constipation, nausea | Complete | CXR, KUB, CT | Conservative | --- | Resolution |
| [23] | M | 1 yr | DE | Colon | Recurrent respiratory distress | Complete | CXR, KUB, CT | Surgery | Correction of diaphragmatic, eventration and elevation of right hemidiaphragm | Resolution |
| [23] | F | 16 mo | DE | Colon | Recurrent respiratory distress | Complete | CXR, KUB, CT | Surgery | Correction of diaphragmatic, eventration and elevation of right hemidiaphragm | Resolution |
| [25] | M | 5 mo | --- | Colon | Recurrent respiratory distress | Complete | CXR, CT | Conservative | --- | Resolution |
| Present study | M | 12 yr | Constipation | Colon | Recurrent respiratory distress, abdominal pain, constipation | Complete | CXR, KUB | Surgical | Laparoscopic colopexy | Resolution |
| [33] | F | 2 yr | Constipation | Colon | Recurrent respiratory distress, abdominal pain, constipation | Complete | CXR | Conservative | --- | Resolution |
| [10] | M | 8 yr | Constipation | Colon | Abdominal pain, constipation | Complete | KUB, CT | Conservative | --- | Resolution |
| [11] | M | 10 d | Constipation | Colon | Abdominal distension, respiratory distress, constipation | Complete | KUB | Conservative | --- | Resolution |
| [12] | F | 3 yr | Constipation | Colon | Recurrent respiratory distress, constipation | Complete | CXR | Conservative | --- | --- |
| [13] | M | 4 yr | Aerophagia | Colon | Respiratory distress | Complete | CXR | Conservative | --- | Resolution |
| [14] | M | 6 yr | --- | Colon | Abdominal pain, emesis, FTT | Complete | CXR | Surgical | Laparoscopic colopexy | Resolution |
| [15] | M | 10 yr | Aerophagia | Colon | Recurrent respiratory distress | Complete | CXR, MRI | Conservative | --- | Resolution |
| [15] | M | 7 yr | Aerophagia | Colon | Recurrent respiratory distress, abdominal distention | Complete | CXR, MRI | Conservative | --- | Resolution |
| [8] | M | 4 yr | Aerophagia, constipation | Colon | Recurrent respiratory distress, abdominal pain, constipation | Complete | CXR, CT | Conservative | --- | Resolution |
| [16] | M | 3 yr | Aerophagia | Colon | Recurrent respiratory distress, abdominal distention | Complete | CXR | Conservative | --- | Resolution |
| [17] | M | 20 yr | Duchenne muscular | Colon | Recurrent respiratory distress | Complete | CT | Conservative | --- | Resolution |
| [18] | M | 19 yr | Dystrophy, aerophagia, constipation | Colon | Chest pain, respiratory distress, abdominal pain | Complete | CXR | Conservative | --- | Resolution |
| [20] | F | 1 yr | Aerophagia | Colon | Respiratory distress | Partial | CXR | Conservative | --- | Resolution |
| [21] | M | 10 yr | Constipation, mental retardation | Colon | Respiratory distress, constipation, failure to thrive, abdominal distention | Complete | CXR | --- | --- | --- |
The etiology of Chilaiditi syndrome has been categorized into (1) Intestinal: megacolon, abnormal colonic motility or redundancy, constipation, and congenital malrotation; (2) Hepatic: cirrhosis, segmental agenesis of the right lobe of the liver, and relaxation of the hepatic suspensory ligament; and (3) Diaphragmatic: phrenic nerve injury and diaphragmatic eventration[15,17]. Several risk and predisposing factors have been associated with this entity including, aerophagia, adhesions, obesity, constipation, mental retardation, pregnancy, muscular dystrophy, and significant weight loss[17,22]. Very rarely, episodes of volvulus have been associated to this syndrome, especially in the elderly population and could be complicated with cecal perforation[4,7,22,29,30]. Chilaiditi syndrome can further be divided in two types, depending on the degree of intestinal interposition and liver displacement: (1) In the complete form, the colon typically lies above the liver, there being contact between the liver and diaphragm, with the liver displaced inferiorly, anteriorly, and medially; and (2) In the incomplete (partial) form, the colon does not typically rise above the liver, but lays lateral or posterior to it[23]. In theory, patients after orthotic liver transplan
In our review of the pediatric literature, we found the most common predisposing factors in children to be aerophagia (12/30 cases) and constipation (13/30 cases). Ninety percent of the cases presented with complete intestinal interposition, in 100% of which the colon was involved. Three of the 30 cases were associated with volvulus. In the case we described here, the predisposing factor was believed to be a combi
The most common clinical presentation of Chilaiditi syndrome is constipation, abdominal pain, nausea, vomiting, abdominal distention, and respiratory distress. On physical examination, it is possible to encounter loss of hepatic dullness on percussion (Joubert sign)[7,8,23,25]. The diagnosis of hepatodiaphragmatic interposition can be demonstrated with radiologic tests such as a plain KUB, a right upper quadrant ultrasound or an abdominal CT scan. Identifying haustra or plicae circularis between the liver and the diaphragm can distinguish pneumoperitoenum from Chilaiditi syndrome.
The majority of the cases with Chilaiditi syndrome require a conservative therapy which includes bed rest in a supine position, daily maintenance bowel regimen with laxatives and normal fiber diet, frequent bowel cleansing, fluid supplementation, and nasogastric decompression[23,25]. In some specific cases emergency surgery may be re
The teaching point of this uncommon but intriguing syndrome is to have a high index of suspicion of this condition in patients who have predisposing factors. In addition, it is essential to exclude pathologic conditions such as pneumoperitoneum, subphrenic abscess, posterior hepatic lesions, and Morgagni hernia, which can mimic Chilaiditi sign on a radiologic film. A subphrenic abscess usually features a compa
Chilaiditi syndrome is a rare condition especially among the pediatric population. It should be suspected when patients present with constipation, abdominal pain (particularly located in the right upper quadrant), nausea, vomiting, abdominal distention, and respiratory distress of unknown cause. In the cases previously reported, there were no data about recurrence or timeline from first symptomatology to diagnosis; given the lack of information, long-term follow-up in these cases is necessary. In the pediatric population, both conservative and surgical approaches in treating Chilaiditi syndrome, with treatment of the predisposing factors, have resulted in satisfactory outcomes.
We would like to thank Dr. Colombani P for performing the surgery on our patient reported in this article.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Raahave D S-Editor: Zhang L L-Editor: A P-Editor: Yuan YY
| 1. | Chilaiditi D. Zur Frage der Hepatoptose und Ptose im allgemeinen im Anschluss an drei Falle von temporarer, partieller Leberverlagerung. Fortcshr Geb Rontgenstr Nuklearmed Erganzongsband. 1910;16:173-208. |
| 2. | Kumar A, Mehta D. Chilaiditi Syndrome. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2021. [PubMed] |
| 3. | Lo BM. Radiographic look-alikes: distinguishing between pneumoperitoneum and pseudopneumoperitoneum. J Emerg Med. 2010;38:36-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Torgersen J. Suprahepatic interposition of the colon and volvulus of the cecum. Am J Roentgenol Radium Ther. 1951;66:747-751. [PubMed] |
| 5. | Murphy JM, Maibaum A, Alexander G, Dixon AK. Chilaiditi’s syndrome and obesity. Clin Anat. 2000;13:181-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Platz TA, Barker M, Carlo J, Lord J. Chilaiditi syndrome--an interesting complication in a bariatric surgery patient. Surg Obes Relat Dis. 2006;2:57-8; discussion 59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Barroso Jornet JM, Balaguer A, Escribano J, Pagone F, Domenech J, del Castillo D. Chilaiditi syndrome associated with transverse colon volvulus: first report in a paediatric patient and review of the literature. Eur J Pediatr Surg. 2003;13:425-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Dogu F, Reisli I, Ikinciogullari A, Fitöz S, Babacan E. Unusual cause of respiratory distress: Chilaiditi syndrome. Pediatr Int. 2004;46:188-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | White JJ, Chavez EP, Souza J. Internal hernia of the transverse colon-Chilaiditi syndrome in a child. J Pediatr Surg. 2002;37:802-804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Evrengül H, Yüksel S, Orpak S, Özhan B, Ağladıoğlu K. Chilaiditi Syndrome. J Pediatr. 2016;173:260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Dutt R, Dutt C. Chilaiditi syndrome: a rare manifestation in newborn. J Clin Neonatol. 2013;2:50-51. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Ghani S, Course CW, Bodla HP. From sign to syndrome: Chilaiditi. Arch Dis Child. 2017;102:1117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Sunejam U, Alharbi O, Karki K, Agyare S. Chilaiditi Syndrome. Consult Pediatr. 2016;15. |
| 14. | Blevins WA, Cafasso DE, Fernandez M, Edwards MJ. Minimally invasive colopexy for pediatric Chilaiditi syndrome. J Pediatr Surg. 2011;46:e33-e35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Erdem SB, Nacaroğlu HT, Karkıner CŞÜ, Alper H, Can D. Chilaiditi Syndrome in Two Cases Presented with Respiratory Distress Symptoms. Turk Thorac J. 2015;16:97-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Hussain S, Hussain S. Chilaiditi Syndrome-What’s Air Doing There? J Emerg Med. 2018;55:e131-e132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Ogasawara M, Ishiyama A, Sugiura A, Segawa K, Nonaka I, Takeshita E, Shimizu-Motohashi Y, Komaki H, Sasaki M. Duchenne muscular dystrophy with platypnea-orthodeoxia from Chilaiditi syndrome. Brain Dev. 2018;40:339-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Inzamam Ali M, El Essawy B, Menakuru S. Undiagnosed Chilaiditi syndrome presenting with pericarditis in a patient with congenital anomalies. BMJ Case Rep. 2018;2018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 19. | Fitzgerald JF, Tronconi R, Morris LD, Nowicki MJ. Clinical quiz. Chilaiditi’s sign. J Pediatr Gastroenterol Nutr. 2000;30:425, 471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Bostancı İ, Üner Ç, Erdoğan D. In the differential diagnosis of wheezy infant, Chilaiditi syndrome caused by empty bottle absorption. J Contemp Med. 2019;9:410-1. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 21. | Sinopidis X, Gkentzi D, Kostopoulou E, Karatza A, Dimitriou G. Upgrade of Chilaiditi Sign to Syndrome: Are There Any Predisposing Factors? J Emerg Med. 2019;57:573-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Flores N, Ingar C, Sánchez J, Fernández J, Lazarte C, Málaga J, Medina M, Herrera R, Morales C. [The Chilaiditi syndrome and associated volvulus of the transverse colon]. Rev Gastroenterol Peru. 2005;25:279-284. [PubMed] |
| 23. | Huang WC, Teng CS, Tseng MH, Lin WJ, Wang CC. Chilaiditi’s syndrome in children. Acta Paediatr Taiwan. 2007;48:77-83. [PubMed] |
| 24. | Jackson AD, Hodson CJ. Interposition of the colon between liver and diaphragm (Chilaiditi’s syndrome) in children. Arch Dis Child. 1957;32:151-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | Keles S, Artac H, Reisli I, Alp H, Koc O. Chilaiditi syndrome as a cause of respiratory distress. Eur J Pediatr. 2006;165:367-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 26. | London D, Sestopal-Epelman M, Lebovici O. Chilaiditi’s syndrome in an infant: bowel loops mimicking mass lesions on sonography. Pediatr Radiol. 1995;25 Suppl 1:S238-S239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 27. | Pintér A, Pilaszanovich I, Bakó M. Chilaiditi’s syndrome--successful surgical correction. Z Kinderchir Grenzgeb. 1980;30:271-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 28. | Teng CS, Lin WJ, Tseng MH, Wang CC. Chilaiditi’s syndrome in a 9-year-old girl with hepato-diaphragmatic interposition of the colon: a short report. Eur J Pediatr. 2005;164:119-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 29. | Aldoss IT, Abuzetun JY, Nusair M, Suker M, Porter J. Chilaiditi syndrome complicated by cecal perforation. South Med J. 2009;102:841-843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 30. | Chinnappan K, Abhyankar A, Jameel Z. Chilaiditi’s syndrome with cecal volvulus and perforation. Am Surg. 2008;74:1220-1222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 31. | Altomare DF, Rinaldi M, Petrolino M, Sallustio PL, Guglielmi A, Pannarale OC. Chilaiditi’s syndrome. Successful surgical correction by colopexy. Tech Coloproctol. 2001;5:173-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 32. | Nakagawa H, Toda N, Taniguchi M, Ibukuro K, Tagawa K. Prevalence and sonographic detection of Chilaiditi’s sign in cirrhotic patients without ascites. AJR Am J Roentgenol. 2006;187:W589-W593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 33. | Correa Jiménez O, Buendía De Ávila M, Parra Montes E, Davidson Córdoba J, De Vivero Camacho R. [Chilaiditi’s sign and syndrome: rare conditions but diagnostically important in pediatrics. Clinical cases]. Rev Chil Pediatr. 2017;88:635-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |