Published online Nov 28, 2015. doi: 10.5319/wjo.v5.i4.105
Peer-review started: June 26, 2015
First decision: August 16, 2015
Revised: August 23, 2015
Accepted: October 12, 2015
Article in press: October 13, 2015
Published online: November 28, 2015
Processing time: 167 Days and 9.4 Hours
AIM: To examine the presentation, diagnosis and outcomes of patients with laryngeal cleft.
METHODS: An 18 mo (from mid-2012 to 2013) prospective longitudinal study was performed at the Barts Children’s and Royal London Hospital, a tertiary referral centre. Chart review was performed for all patients including data extraction of demographics, outpatient clinic review documentation, speech therapy findings, medication list, operative findings alongside technique and follow up. A systematic review of contemporary English medical literature was also reviewed to compare series. The study was approved and registered by the hospital clinical governance and audit board. Biostatistician review was not required.
RESULTS: Twenty-two children aged 1 to 72 mo (mean age 23.5 mo) with a 7:4 male-female ratio. Twenty had Benjamin-Evans type 1 clefts and 2 had a type 2 cleft. All were symptomatic despite medical management including anti-reflux therapy. Patients presented with dyspnoea (81%), feeding difficulty (63%), stridor (54%) and recurrent pneumonia (36%). Several patients had concomitant aerodigestive abnormalities including 7 with laryngomalacia, 4 subglottic stenosis, 2 subglottic webs and 1 tracheo-oesophageal fistula. To date, 18 patients have undergone endoscopic repair, all of whom have shown radiological and/or clinical signs of improvement. All endoscopic repairs were performed with the novel use of a Negus knot pusher, with Baby Benjamin rigid suspension, to more reliably and easily suture at depth.
CONCLUSION: This is a significant single unit series demonstrating the strong association of laryngeal cleft with combined aerodigestive symptoms and other laryngeal abnormalities. Endoscopic management of type 1 and 2 laryngeal clefts is successful. We recommend the use of a Negus knot pusher to facilitate endoscopic repair.
Core tip: Laryngeal cleft is a rare laryngo-tracheal wall abnormality. Patients may present with laryngeal or respiratory symptoms. A high index of suspicion is required. A multi-disciplinary team, including speech therapy and otorhinolaryngology, is required to manage these patients. Endoscopic surgical repair is increasingly the gold standard for symptomatic patients. We propose the use of the Negus knot pusher to facilitate endoscopic repair procedures.
- Citation: Yalamachili S, Virk JS, Bajaj Y. Diagnosis and management of laryngeal cleft: A single centre experience and a novel endoscopic technique. World J Otorhinolaryngol 2015; 5(4): 105-109
- URL: https://www.wjgnet.com/2218-6247/full/v5/i4/105.htm
- DOI: https://dx.doi.org/10.5319/wjo.v5.i4.105
Laryngeal cleft is a congenital malformation that results in an abnormal communication between the oesophagus and larynotracheal complex. It is a rare disease, slightly more common in males, affecting approximately 1:10000 live births, constituting 1% of congenital laryngeal malformations[1-3]. However, there has been an increased prevalence in more recent literature due, in part, to increased diagnosis of latent and asymptomatic cases[4-8].
Laryngeal clefts occur due to an absence of fusion of the posterior cricoid lamina and in some cases, the tracheoesophageal septum. Histopathological investigations suggest deformities of the posterior cricoid lamina and alterations in muscle differentiation of the inter- and crico-arytentoid muscles. As a result, laryngeal cleft is typically associated with other malformations, particularly those of the digestive tract[2-4,6,9].
There are a number of classification systems but the most commonly employed is that which Benjamin et al[10] described in 1989, with Type 1-4 clefts depending on their length. Symptoms correlate with the extent of the cleft and may be laryngeal, in the form of stridor, swallowing difficulties, aspiration, cough or hoarse cry, or respiratory, such as dyspnoea, cyanosis and recurrent lower respiratory tract infections. There are also known associations with reflux disease and syndromes including CHARGE, Pallister Hall, VACTERL and OPTIZ G[3].
The aim of this study was to present and analyse a prospective series of laryngeal cleft patients at a single tertiary referral centre.
An 18 mo (mid-2012 to 2013) prospective longitudinal study was performed at the Barts Children’s and Royal London Hospital. Chart review was performed for all patients. A systematic review of contemporary English medical literature was also reviewed to compare series (Table 1). The study was approved and registered by the hospital clinical governance and audit board. Biostatistician review was not required.
| Ref. | Year | Number1 | Grading of laryngeal cleft | Type of repair | Prospective | Level of evidence |
| Yalamachili et al | 2015 | 18 (22) | 16 grade 1; 2 grade 2 | 18 endoscopic | Yes | IV |
| Ojha[2] | 2014 | 27 (42) | 27 grade 1 | 27 endoscopic | No | IV |
| Thiel et al[6] | 2011 | 12 | 6 grade 1; 5 grade 2; 1 grade 3 | 3 endoscopic; 2 open | No | IV |
| Cohen et al[19] | 2011 | 16 | 16 grade 1 | 16 injection laryngoplasty | No | IV |
| Broomfield et al[7] | 2011 | 7 | 3 grade 2; 4 grade 3 | 7 endoscopic | No | IV |
| Rahbar et al[18] | 2009 | 49 (74) | 28 grade 1; 21 grade 2 | 49 endoscopic | No | IV |
| Rahbar et al[17] | 2006 | 22 | 3 grade 1; 10 grade 2; 9 grade 3 | 6 endoscopic; 16 open | No | IV |
| Chien et al[8] | 2006 | 16 (20) | 16 grade 1 | 16 endoscopic | Yes | IV |
| Kubba et al[16] | 2005 | 35 | 35 grade 1-3 | Variable | No | IV |
| Watters et al[21] | 2003 | 8 (12) | 8 grade 1 | 8 endoscopic | No | IV |
| Kennedy et al[15] | 2000 | 8 | 8 grade 1 | 8 gelfoam | No | IV |
| Glossop et al[22] | 1984 | 6 (10) | 6 grade 2-4 | Variable | No | IV |
Twenty-two patients were identified with an age range of 1 to 72 mo (mean 23.5 mo) and 7:4 male to female ratio. All patients were symptomatic despite full medical management including anti-reflux therapy. Twenty patients had type 1 clefts with the remaining 2 diagnosed with type 2 laryngeal cleft.
The main referral sources were general or family practitioners (45%) and hospital paediatricians (36%), with the remainder from the paediatric intensive care service. The commonest presenting symptoms were dyspnoea (81%), feeding difficulty (63%), stridor (54%) and recurrent pneumonia (36%). Co-pathologies were noted in 14 patients (64%) including 7 with laryngomalacia (32%), 4 subglottic stenosis (18%), 2 subglottic web (9%), 1 tracheoesophageal fistula (4.5%).
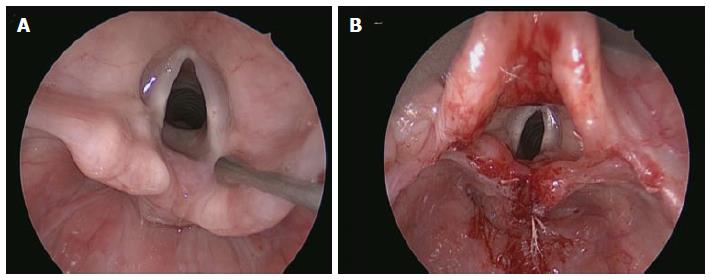
All patients underwent speech and language team assessment with penetration or aspiration demonstrated on video fluoroscopy (n = 18) unless speech therapy deemed the swallow too unsafe to proceed (n = 4). At the time of chart review, 18 children had subsequently undergone surgical endoscopic laryngeal cleft repair (Figure 1).
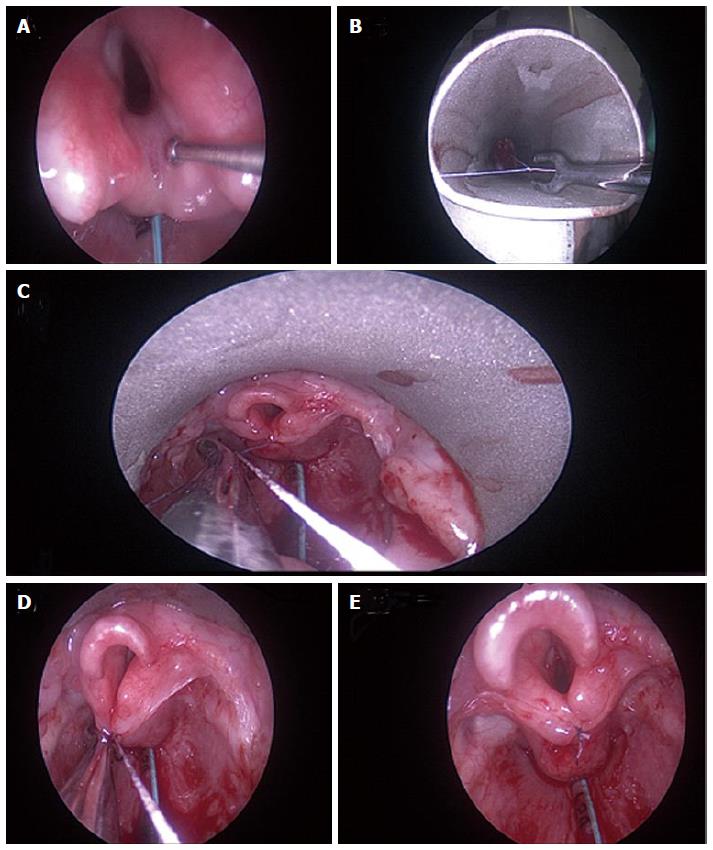
All patients underwent our standard departmental anaesthetic induction with spontaneous ventilation. All endoscopic repairs were performed with Baby Benjamin laryngoscope in suspension. We employed the novel use of a Negus knot pusher with an absorbable suture to facilitate ease and reliability of squaring of knots and closure. This produced excellent intraoperative and postoperative outcomes (Figure 2).
Laryngeal cleft is rare disorder for which a high index of suspicion is required, across a number of specialities from intensivists, family practitioners, paediatricians and otolaryngologists due to wide variety of presenting symptoms, as highlighted by our results[1,8,11]. This is a significant single unit series demonstrating the strong association of laryngeal cleft with combined upper aerodigestive tract symptoms and other laryngeal abnormalities. All patients in this series either underwent or are due to undergo endoscopic cleft repair as they remain symptomatic despite maximal medical and speech therapy including anti-reflux medications.
This series represents one of the largest prospective analyses (Table 1) of laryngeal clefts in recent literature and highlights the importance of the symptom profile of children presenting with this abnormality alongside associated findings and successful endoscopic management. In our series, the proportion of males was less than published in the literature[3]. In addition, the rate of tracheoesophageal fistula in our series (4.5%) was much lower than typically expected (10%-20%) from the literature[2,4,8,12]. This may reflect referral patterns and our local population.
Management options for laryngeal cleft are myriad ranging from conservative/medical management (including reflux treatment, prevention of pulmonary complications, thickened feeds) to early surgery to prevent complications and where conservative therapies have failed. Viable surgical options incorporate endoscopic surgical repair and external approaches, with anterior (or less commonly, lateral) cervical approaches for more significant clefts[1-3]. Other techniques such as injection laryngoplasty, gel foam, laser repair and cartilage grafts have also been attempted[5,6,13-19]. There is however an increasing trend, like in our series, towards endoscopic approaches[1,2,11].
We note a growth in absolute numbers of referrals from paediatric respiratory and intensivist colleagues. This trend may be in part due to a rise in awareness locally but may also reflect a wider trend in greater prevalence due to a greater cohort of premature babies being supported through infancy. This pattern might in turn correspond to the increased prevalence reported in recent literature[1,2,4,8,12,20]. We propose to continue to monitor the growing influx into the paediatric airway service at our centre with particular respect to laryngeal clefts and report further trends in presentation and outcomes in the management of these children.
In conclusion, a high index of suspicion and a multi-disciplinary team, including speech therapy and otolaryngology, is required to manage these patients. Endoscopic surgical repair is increasingly the gold standard for symptomatic patients with laryngeal cleft, particularly of types 1-2. We recommend the use of the Negus knot pusher to facilitate endoscopic repair.
The main objective of this study was to analyse the laryngeal cleft patients at a tertiary referral centre, in terms of presentation, diagnosis, management and outcomes.
This is one of the largest single unit series of laryngeal cleft patients.
This endoscopic repair technique is previously unpublished.
The authors recommend their technique to add to the armamentarium of paediatric otorhinolaryngologists.
This is a paper reporting the diagnosis and management of laryngeal cleft. The subjects for this investigation included 22 children. A novel endoscopic technique is a main point of this paper.
P- Reviewer: Coskun A, Nakashima T S- Editor: Gong ZM L- Editor: A E- Editor: Wu HL
| 1. | Chiang T, McConnell B, Ruiz AG, DeBoer EM, Prager JD. Surgical management of type I and II laryngeal cleft in the pediatric population. Int J Pediatr Otorhinolaryngol. 2014;78:2244-2249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 2. | Ojha S, Ashland JE, Hersh C, Ramakrishna J, Maurer R, Hartnick CJ. Type 1 laryngeal cleft: a multidimensional management algorithm. JAMA Otolaryngol. 2014;140:34-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 3. | Rossi MS, Buhler KE, Ventura GA, Otoch JP, Limongi SC. Laryngeal cleft type I in neonate: case report. Codas. 2014;26:421-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Eriksen C, Zwillenberg D, Robinson N. Diagnosis and management of cleft larynx. Literature review and case report. Ann Otol Rhinol Laryngol. 1990;99:703-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 45] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Watters K, Ferrari L, Rahbar R. Laryngeal cleft. Adv Otorhinolaryngol. 2012;73:95-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Thiel G, Clement WA, Kubba H. The management of laryngeal clefts. Int J Pediatr Otorhinolaryngol. 2011;75:1525-1528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Broomfield SJ, Bruce IA, Rothera MP. Primary endoscopic repair of intermediate laryngeal clefts. J Laryngol Otol. 2011;125:513-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Chien W, Ashland J, Haver K, Hardy SC, Curren P, Hartnick CJ. Type 1 laryngeal cleft: establishing a functional diagnostic and management algorithm. Int J Pediatr Otorhinolaryngol. 2006;70:2073-2079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 84] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 9. | Lim TA, Spanier SS, Kohut RI. Laryngeal clefts: a histopathologic study and review. Ann Otol Rhinol Laryngol. 1979;88:837-845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 42] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Benjamin B, Inglis A. Minor congenital laryngeal clefts: diagnosis and classification. Ann Otol Rhinol Laryngol. 1989;98:417-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 264] [Cited by in RCA: 229] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 11. | Watters K, Ferrari L, Rahbar R. Minimally invasive approach to laryngeal cleft. Laryngoscope. 2013;123:264-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Walner DL, Stern Y, Collins M, Cotton RT, Myer CM. Does the presence of a tracheoesophageal fistula predict the outcome of laryngeal cleft repair? Arch Otolaryngol Head Neck Surg. 1999;125:782-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Froehlich P, Truy E, Stamm D, Morgon A, Floret D, Chappuis JP. Cleft larynx: management and one-stage surgical repair by anterior translaryngotracheal approach in two children. Int J Pediatr Otorhinolaryngol. 1993;27:73-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Prescott CA. Cleft larynx: repair with a posterior cartilage graft. Int J Pediatr Otorhinolaryngol. 1995;31:91-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (1)] |
| 15. | Kennedy CA, Heimbach M, Rimell FL. Diagnosis and determination of the clinical significance of type 1A laryngeal clefts by gelfoam injection. Ann Otol Rhinol Laryngol. 2000;109:991-995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 31] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Kubba H, Gibson D, Bailey M, Hartley B. Techniques and outcomes of laryngeal cleft repair: an update to the Great Ormond Street Hospital series. Ann Otol Rhinol Laryngol. 2005;114:309-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 40] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Rahbar R, Rouillon I, Roger G, Lin A, Nuss RC, Denoyelle F, McGill TJ, Healy GB, Garabedian EN. The presentation and management of laryngeal cleft: a 10-year experience. Arch Otolaryngol Head Neck Surg. 2006;132:1335-1341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 94] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 18. | Rahbar R, Chen JL, Rosen RL, Lowry KC, Simon DM, Perez JA, Buonomo C, Ferrari LR, Katz ES. Endoscopic repair of laryngeal cleft type I and type II: when and why? Laryngoscope. 2009;119:1797-1802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 68] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 19. | Cohen MS, Zhuang L, Simons JP, Chi DH, Maguire RC, Mehta DK. Injection laryngoplasty for type 1 laryngeal cleft in children. Otolaryngol Head Neck Surg. 2011;144:789-793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 20. | Jefferson ND, Carmel E, Cheng AT. Low inter-arytenoid height: a subclassification of type 1 laryngeal cleft diagnosis and management. Int J Pediatr Otorhinolaryngol. 2015;79:31-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Watters K, Russell J. Diagnosis and management of type 1 laryngeal cleft. Int J Pediatr Otorhinolaryngol. 2003;67:591-596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 43] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 22. | Glossop LP, Smith RJ, Evans JN. Posterior laryngeal cleft: an analysis of ten cases. Int J Pediatr Otorhinolaryngol. 1984;7:133-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 0.7] [Reference Citation Analysis (0)] |