Published online May 28, 2015. doi: 10.5319/wjo.v5.i2.53
Peer-review started: November 11, 2014
First decision: January 8, 2015
Revised: January 23, 2015
Accepted: February 10, 2015
Article in press: February 12, 2015
Published online: May 28, 2015
Processing time: 192 Days and 11.9 Hours
Otitis media is a frequent problem in preschool children and one of the most common reasons for treatment with antibiotics in children. The exact diagnosis is important for proper management. The diagnosis of otitis media is often difficult. Pneumatic otoscopy, otomicroscopy, and tympanometry can improve the diagnostic quality by indicating fluid or no fluid in the middle ear and thus improve the quality of treatment. The aim of this review is to explain why and how tympanometry can improve the diagnostic quality in otitis media, and to identify some barriers and difficulties encountered when using tympanometry in daily practice. The current literature on tympanometry and own experiences during 38 years are used to elucidate the aim. Tympanometry is difficult to understand and use, when the procedure is not properly trained. The problems are both of a technical nature, and it is difficult to understand and use the information from the curve and the figures on the display. If the use of tympanometry in general practice is increased, the diagnostic quality will improve and hopefully antibiotics will be prescribed on more appropriate indications and less frequently. More demand on tympanometry will hopefully reduce the price of the tympanometer, making it more accessible for GPs. First in that situation the use will be nearly as common as the use of the otoscope.
Core tip: The aim of this review is to explain why and how tympanometry can improve the diagnostic quality in otitis media, and to identify some barriers and difficulties in using tympanometry in daily practice.
- Citation: Lous J. Why use tympanometry in general practice: A review. World J Otorhinolaryngol 2015; 5(2): 53-57
- URL: https://www.wjgnet.com/2218-6247/full/v5/i2/53.htm
- DOI: https://dx.doi.org/10.5319/wjo.v5.i2.53
Otitis media (OM) is a common disease in children. More than 80% of children have had OM before the age of two years[1]. The presentation of otitis media can have two different forms: either acute otitis media (AOM) or otitis media with effusion (OME), also called secretory otitis media. The two forms are closely related. We often see a development from OME to AOM and from AOM to OME, as well as stages in between often challenging the physicians.
AOM is an acute inflammatory disease in the middle ear with acute symptoms like ear pain, ear tugging, vomiting, sleeping problems and often fever, the tympanic membrane is changed in structure (opaque) and color (erythema) and often bulging out, and the middle ear cavity contains fluid (purulent)[2]. The tympanic membrane has in children with AOM no or impaired mobility. When culturing, more than ¾ are found to have bacteria in the middle ear fluid. In Denmark, before the era of antibiotics AOM was a serious disease among children with a mortality of about 6%[3]. Even today 127 relevant papers on complications and sequelae have been published between January 2007 and June 2011[4].
OME often has no or minor symptoms like a small hearing loss, some ear discomfort or pain and sleeping problems[5]. The tympanic membrane can be transparent and amber colored or sometimes grey with visible fluid levels or air bubbles behind the tympanic membrane, and the mobility is impaired[6,7]. Or the tympanic membrane can be opaque (not transparent), dull or sometimes edematous. In OME the fluid normally is without living bacteria.
In otitis media a correct diagnosis is fundamental to proper management. AOM must be differentiated from OME to avoid unnecessary antimicrobial use[2,7]. Diagnosing AOM requires a history of acute onset in sign and symptoms, and presence of middle ear effusion, and signs of middle ear inflammation[2], whereas OME just is fluid in the middle ear without signs or symptoms of acute ear infection[7].
The diagnosis of OM can be difficult in a crying child with fever in the out-of-hours service in the late evening. Also the differentiation between AOM and OME can be difficult with a normal otoscope, especially in children, because of a narrow and angled ear canal with hair and cerumen. Is the tympanic membrane normal (gray, translucent, with light reflex)? Is the tympanic membrane translucent or with changed color (erythema or amber)? Is it possible to see fluid level or air bubbles behind the tympanic membrane? etc.
Three important tools can improve our clinical examination. Pneumatic otoscopy improves the diagnostic quality by giving information of the mobility of the tympanic membrane, thus providing an indication about presence or absence of fluid in the middle ear and thereby improving the quality of treatment. Pneumatic otoscopy is recommended in the United States guidelines on OME with the best balanced sensitivity 94% (95%CI: 91%-96%) and specificity of 80% (75%-86%)[7]. The equipment for doing pneumatic otoscopy is not expensive, but the problem is that it is difficult to learn and is therefore seldom used in general practice[8].
Another tool is otomicroscope with better light and bioccular magnification. It can easily be combined with pneumatic examination. A sensitivity of up to 94% and specificity of 94% have been found[9,10]. The otomicroscope requires a lot of space in the surgery, is difficult to move, and is expensive. Therefore it is not recommended for use in normal general practice clinics.
A third technique to improve the diagnostic quality in ear patients is tympanometry (electroacoustic impedance audiometry). Tympanometry is in the guidelines recommended as an alternative or supplement to pneumatic otoscopy[7]. Tympanometry measures the “stiffness” of the tympanic membrane (and middle ear and ear canal). The use can be learned in a few hours course, including understanding of the test results displayed on the screen[11]. The tympanometer is still relatively expensive, but more demand will hopefully reduce the price.
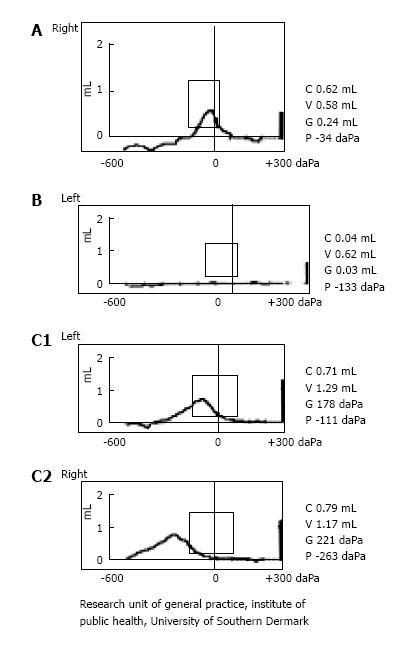
As mentioned, tympanometry is an electroacoustic impedance measurement of the tympanic membrane and related structures[12]. A generated sound of 220 Hz is sent into the ear canal, and a microphone measures the reflection of sound energy from the tympanic membrane during a pressure change in the ear canal from +200 to -400 daPa (dekapascal nearly equal to mm water pressure). That means the tympanic membrane will be pressed inwards in the beginning, then gradually become more relaxed, when the pressure in the ear canal is the same as in the middle ear and finally more tense or stiff when the negative pressure in the ear canal sucks the tympanic membrane outwards. During this pressure change the impedance (or actually the admittance) is recorded and displayed on the screen of the tympanometer (low - > high - > low) - normally as a bell-shaped curve called a tympanogram, with a top between +50 and - 99 daPa. This curve is called type A tympanogram according to Jerger/Fiellau-Nikolajsen’s modification[13,14]. In ears with negative pressure the curve has the same shape, but is displaced to the left, the negative side of the X-axis. When the pressure is between -100 and -199 daPa it is called a type C1 curve and when between -200 and -400 a type C2 curve. In middle ears filled with fluid the tympanic membrane will act more stiffly, i.e., more sound is reflected (less admittance) and the curve will be very low or flat (a type B tympanogram) (Figure 1). Type B tympanogram has a high predictive value for fluid in the middle ear (97%-93%), and a type A tympanogram signifies a middle ear without fluid[15,16]. The C tympanograms are in a stage between normal and not normal. Often C1 is classified as normal, and often C2 means negative pressure with a mix of fluid and air in the middle ear[15].
The effect of using tympanometry was studied in a group of 40 GPs in the of Region Southern Denmark[17]. They performed otoscopy and made a diagnosis on the basis of history and examination. Subsequently they performed tympanometry successfully in 88% of the children, and in 26% the diagnosis was changed. Their findings indicated that tympanometry and training of the GPs resulted in more relevant cases being referred for treatment by ENT[17]. In another Danish study 20 GPs were randomized to use tympanometry and 20 to usual management. Children under 16 years of age were included when the GP found indication for otoscopy[18]. They found 8.4% with acute otitis in the control group and 2.6% in the tympanometry group. OME was found in 14.2% in the control group and in 25% in the tympanometry group. Antibiotics were prescribed in 7.6% in the control group and in 4.1% in the tympanometry group[18].
We asked a group of GPs and practice nurses attending courses on otitis media and tympanometry what problems they had[11]. Of the 197 participants 142 completed the questionnaire (72%), 48 (34%) had not used tympanometry before, and 94 (62%; 95%CI: 52-71) of the participants with experience in tympanometry had frequently one or more problems when performing tympanometry (Table 1). The total number of frequent problems was 172. None of the 94 experienced participants were without problems when performing tympanometry.
| Type of frequent problems in 94 participants with some experience in tympanometry | Before the coursen (%) | Six weeks after the coursen (%) | Absolute improvement (95%CI) |
| Technical problems | |||
| Getting a reliable curve written | 38/93 (40.9) | 10/94 (10.6) | 30.20% (18 to 41) |
| Getting airtight sealing | 32/92 (34.8) | 9/93 (9.7) | 25.10% (13 to 36) |
| Problems handling the tympanometer | 21/91 (23.1) | 5/92 (5.4) | 17.60% (8 to 28) |
| Getting the children to cooperate | 11/91 (12.1) | 4/93 (4.3) | 7.80% (0 to 17) |
| Understanding the results | |||
| Understanding the meaning of the displayed figures and using them as quality assurance of the measurement | 41/93 (44.1) | 6/94 (6.4) | 37.70% (26 to 48) |
| Understanding what the curves mean for the clinical decision | 29/93 (31.2) | 2/94 (2.1) | 29.10% (19 to 39) |
The problems were often technical: how to get airtight sealing, or a reliable written curve, and how to handle the tympanometer. The other half of the problems was how to understand the curves and the written figures on the display and how to use the information in the clinical situation[11]. Table 2 gives more detailed answers to these questions. After the course, the number of frequent problems was reduced significantly (Table 1).
| Airtight sealing between the tip of the tympanometer and the ear canal is important. If there are problems with sealing use a little water or cream on the tip, and more pressure towards the ear canal and at the same time pull the external ear up and backwards to stretch the ear canal. Alternatively use a bigger and more solid tip |
| In order to perform valid tympanometry the sound signal and air pressure have to pass through the ear canal. That means there must be no earwax blockade and the probe has to point in the direction of the ear canal. Partly ear wax occlusion does not disturb the measurement |
| The result of the tympanometry is a curve, called a tympanogram. The curve is characterized by the height of the curve (compliance), the flatness of the curve (gradient), and location of the peak on the x-axis (pressure). These three characteristics will be given as figures on the screen of the tympanometer, together with the curve (Figure 1) |
| The fourth value measured by the tympanometer is the ear canal volume. It is important to compare the volumes of left and right ear canal. Normally they will be nearly the same, if the same size of tip is used in both ears. A very small ear canal volume measurement can occur because of ear wax blockade or because the tip is pointing towards the wall of the ear canal. A high ear canal volume is seen in ears with perforation of the tympanic membrane or ventilation tube (grommet) in function. A blocked grommet gives a normal ear canal volume |
| The appearance of the curve and the figures has to fit (quality assurance) |
| Any not-normal curve should be repeated to exclude any artefacts |
| The curves are often classified according to Jerger/Fiellau-Nikolajsen in Type A = normal peaked curve with pressure between +50 and -99 daPa (decaPascal), Type B is a flat curve without peak, and Type C1 peak curve with negative pressure (-100 to -199), and Type C2 a peaked curve with negative pressure of -200 daPa or less (Figure 1) |
| Other curve types are also described. Type D is a very high curve (high compliance), meaning a very flexible tympanic membrane, often because of atrophy. Type P is a peaked tympanogram with positive pressure above +50 daPa, often because of acute otitis media with a bulging tympanic membrane |
| The tympanogram has to be compared with the history and objective findings |
| A flat tympanogram (Type B) means a stiff tympanic membrane and predicts fluid in the middle ear (a positive predictive value of more than 90%) |
| A normal tympanogram (Type A) means a middle ear without fluid and an intact tympanic membrane (a negative predictive value of more than 95%) |
| Types C1 and C2 tympanograms are often seen in children with a runny nose. These types are a stage “in between”, i.e., they can develop into a Type B or A tympanogram. In daily clinical practice C1 is often classified as normal. Some of the ears with Type C2 tympanograms have a mixture of air and effusion in the middle ear |
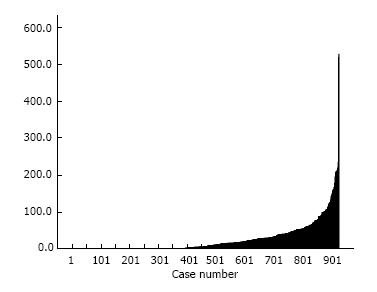
The problems in using tympanometry is reflected in a surprisingly skewed use, with many not using at all, a majority using it seldom, and a very few using it more than once daily[11,19] (Figure 2).
Clinic type does not matter. Single-handed GPs in smaller clinics have the same use (mean 24.4, 95%CI: 20.2-28.8) of tympanometry per year as GP in clinics with several GPs (mean 26.3, 95%CI: 22.3-30.4), (ANOVA, F = 0.4, P = 0.53)[19]. We found no relation to sex and age in the use of tympanometry. We found a difference in use between three regions, representing about half of Danish population, with about 900 clinics and more than 1700 GPs. A total of about 60% (95%CI: 57-63) used tympanometry, even since 2006 it has been reimbursed with about 14 € per examination, and the increase was slow from 56% in 2007 to 60% in 2009. Tympanometry was significantly more used in the Region of Southern Denmark (68%) (64 to 73), than in the North Denmark Region (61%) (54 to 68) and Region Zealand (48%) (42 to 53). Maybe the explanation for this difference is related to early research using tympanometry in both the Region of Southern Denmark[17,18] and the North Denmark Region[20] with participation of several trendsetting GPs in the regions.
Nobody knows. In the clinics doing tympanometry the median value was 28 tympanometry tests per year (interquartile range 13 to 53) per GP. The increase in the use of tympanometry was only between 1% and 4% per year. The variation in the use of tympanometry was surprisingly high, from none, to a maximum of more than 500 tympanometric examinations per GP per year. There may be several reasons for this variation. Education seems to be important.
No official recommendation on when to perform tympanometry has been made in Denmark, but a reasonable use could be whenever you are in doubt of the otoscopic findings, and that is very common. The 5% most frequent users of tympanometry seem to use it in about 2%-3% of their consultations, just the same number of ear diseases in most registrations in general practice[21]. This means that the tympanometer should be used more than 100 times per GP per year and in order to do that, a tympanometer within arm’s reach is required in the clinic.
Multi-frequency and multicomponent tympanometry added useful extensions to simple low-frequency tympanometry. They permitted the clinician to use probe tones that were higher in frequency than 226 Hz. This addition to the simple tympanometry proved useful for neonates and for any patient who did not produce obvious low-frequency tympanograms. Only a few of tympanometers used in general practice in Denmark can change probe tone to a higher frequency[22].
The next technical step is wideband tympanometry measurements provide a view of the acoustic response properties of the middle ear over a broad range of frequencies and ear-canal pressures. More research is need before the clinical implication of this technic can be outlined[23]. The price of the wideband acoustic immittance equipment of about 15000 € is a barrier for use in general practice.
An increased use of tympanometry in general practice will improve the diagnostic quality in children with middle ear problems and also improve the use of antibiotics, resulting in more appropriate antibiotic prescribing. More demand for tympanometry will hopefully reduce the price of the tympanometer, making it more accessible to GPs. That means that the use of tympanometry will be nearly as common as the use of otoscopy.
P- Reviewer: Lee DH, Xu Z S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Paradise JL, Rockette HE, Colborn DK, Bernard BS, Smith CG, Kurs-Lasky M, Janosky JE. Otitis media in 2253 Pittsburgh-area infants: prevalence and risk factors during the first two years of life. Pediatrics. 1997;99:318-333. [PubMed] |
| 2. | Lieberthal AS, Carroll AE, Chonmaitree T, Ganiats TG, Hoberman A, Jackson MA, Joffe MD, Miller DT, Rosenfeld RM, Sevilla XD. The diagnosis and management of acute otitis media. Pediatrics. 2013;131:e964-e999. [PubMed] |
| 3. | Sparrevohn UR. Acute suppurative otitis media in infants. Acta Otolaryngol. 1945;33:162. [PubMed] |
| 4. | Jung TT, Alper CM, Hellstrom SO, Hunter LL, Casselbrant ML, Groth A, Kemaloglu YK, Kim SG, Lim D, Nittrouer S. Panel 8: Complications and sequelae. Otolaryngol Head Neck Surg. 2013;148:E122-E143. [PubMed] |
| 5. | Lous J, Burton MJ, Felding JU, Ovesen T, Rovers MM, Williamson I. Grommets (ventilation tubes) for hearing loss associated with otitis media with effusion in children. Cochrane Database Syst Rev. 2005;CD001801. [PubMed] |
| 6. | Lous J, Fiellau-Nikolajsen M. Epidemiology and middle ear effusion and tubal dysfunction. A one-year prospective study comprising monthly tympanometry in 387 non-selected 7-year-old children. Int J Pediatr Otorhinolaryngol. 1981;3:303-317. [PubMed] |
| 7. | Rosenfeld RM, Culpepper L, Doyle KJ, Grundfast KM, Hoberman A, Kenna MA, Lieberthal AS, Mahoney M, Wahl RA, Woods CR. Clinical practice guideline: Otitis media with effusion. Otolaryngol Head Neck Surg. 2004;130:S95-118. [PubMed] |
| 8. | Jensen PM, Lous J. Criteria, performance and diagnostic problems in diagnosing acute otitis media. Fam Pract. 1999;16:262-268. [PubMed] |
| 9. | Young DE, Ten Cate WJ, Ahmad Z, Morton RP. The accuracy of otomicroscopy for the diagnosis of paediatric middle ear effusions. Int J Pediatr Otorhinolaryngol. 2009;73:825-828. [PubMed] |
| 10. | Rogers DJ, Boseley ME, Adams MT, Makowski RL, Hohman MH. Prospective comparison of handheld pneumatic otoscopy, binocular microscopy, and tympanometry in identifying middle ear effusions in children. Int J Pediatr Otorhinolaryngol. 2010;74:1140-1143. [PubMed] |
| 11. | Lous J, Ryborg CT, Damsgaard JJ, Munck AP. Tympanometry in general practice: use, problems and solutions. Fam Pract. 2012;29:726-732. [PubMed] |
| 12. | Lous J, Hansen JG, Felding JU. [Tympanometry]. Ugeskr Laeger. 2000;162:1908-1911. [PubMed] |
| 13. | Jerger J. Clinical experience with impedance audiometry. Arch Otolaryngol. 1970;92:311-324. [PubMed] |
| 14. | Fiellau-Nikolajsen M, Lous J. Prospective tympanometry in 3-year-old children. A study of the spontaneous course of tympanometry types in a nonselected population. Arch Otolaryngol. 1979;105:461-466. [PubMed] |
| 15. | Fiellau-Nikolajsen M, Falbe-Hansen J, Knudstrup P. Tympanometry in three-year-old children. III. Correlation between tympanometry and findings at paracentesis in a prospectively followed population of otherwise healthy children aged 3--4 years. Scand Audiol. 1980;9:49-54. [PubMed] |
| 16. | Palmu A, Puhakka H, Rahko T, Takala AK. Diagnostic value of tympanometry in infants in clinical practice. Int J Pediatr Otorhinolaryngol. 1999;49:207-213. [PubMed] |
| 17. | Johansen EC, Lildholdt T, Damsbo N, Eriksen EW. Tympanometry for diagnosis and treatment of otitis media in general practice. Fam Pract. 2000;17:317-322. [PubMed] |
| 18. | Lildholdt T, Felding JU, Eriksen EW, Pedersen LV. [Diagnosis and treatment of ear diseases in general practice. A controlled trial of the effect of the introduction of middle ear measurement (tympanometry)]. Ugeskr Laeger. 1991;153:3004-3007. [PubMed] |
| 19. | Lous J. Use of tympanometry in general practice in Denmark. Int J Pediatr Otorhinolaryngol. 2014;78:124-127. [PubMed] |
| 20. | Hansen JG, Schmidt H. [Measurement of the middle ear pressure in preventive examinations of children]. Ugeskr Laeger. 1991;153:186-188. [PubMed] |
| 21. | Moth G, Olesen F, Vedsted P. Reasons for encounter and disease patterns in Danish primary care: changes over 16 years. Scand J Prim Health Care. 2012;30:70-75. [PubMed] |