Published online Nov 28, 2014. doi: 10.5319/wjo.v4.i4.17
Revised: August 7, 2014
Accepted: September 4, 2014
Published online: November 28, 2014
Processing time: 162 Days and 9.9 Hours
The tympanic (Jacobson’s) nerve is a useful anatomical structure in the middle ear with both practical and physiological functions extending beyond its origin. The paper reviews its clinical anatomy in adults and its surgical significance. English language articles from 5 major databases and Google scholar search engine were used to identify papers outlining the anatomy of the tympanic nerve, associated pathology and surgical relevance. In the majority of cases the tympanic nerve arises from the inferior ganglion of the glossopharyngeal nerve traversing through the tympanic canaliculus into the middle ear. On the promontory it coalesces with sympathetic fibres from the carotid chain forming the tympanic plexus which has individual variability. Functionally, as well as giving off parasympathetic fibres to the parotid gland via the lesser petrosal nerve, it is a useful anatomical landmark for cochlear implantation. The surgical importance of the tympanic nerve is not only restricted to middle ear surgery; it also extends to salivary gland disorders. The tympanic nerve remains clinically relevant to the modern otolaryngologist and as such a detailed understanding of its anatomy is crucial.
Core tip: The tympanic nerve is the first branch arising from the inferior ganglion of the glossopharyngeal nerve. Despite its modest size it has a multitude of functions which are not only limited to the middle ear. In this review we detail the clinical anatomy of the tympanic nerve and its surgical applications in Otolaryngology as they have evolved over the years. We also provide a brief summary of the life and achievements of the indefatigable Ludwig Levin Jacobson, an anatomist and military surgeon, who is credited with the discovery of the tympanic nerve.
- Citation: Kanzara T, Hall A, Virk JS, Leung B, Singh A. Clinical anatomy of the tympanic nerve: A review. World J Otorhinolaryngol 2014; 4(4): 17-22
- URL: https://www.wjgnet.com/2218-6247/full/v4/i4/17.htm
- DOI: https://dx.doi.org/10.5319/wjo.v4.i4.17
This review describes the present evidence outlining the anatomy, function and surgical significance of the tympanic nerve.
The tympanic nerve arises from the inferior ganglion of the glossopharyngeal nerve traversing through the tympanic canaliculus into the middle ear. On the promontory it coalesces with sympathetic fibres from the carotid chain forming the tympanic plexus. Functionally, it provides somatic fibres to the middle ear as well as parasympathetic fibres to the parotid gland via the lesser petrosal nerve.
We have summarised the anatomy from its origin and traced its course through the relevant anatomical segments namely extra tympanic; hypotympanic; and intratympanic. We also elucidate its role in middle ear innervation and secretomotor supply to the parotid. The surgical relevance of the tympanic nerve and the relevant pathological processes are also covered in detail. Further, we have detailed, a historical perspective on the intriguing life of Ludwig Levin Jacobson who is credited with the discovery of the tympanic nerve. For clarity we will use the term tympanic nerve throughout the article although the term “Jacobson’s nerve” is used synonymously throughout the literature.
We conducted a systematic review using Pubmed, Medline, Embase, Google Scholar, Web of Science and the Cochrane library in January 2014. Databases were searched using the term “Jacobson’s/tympanic nerve” before exploring the relevant subheadings. Results were limited to articles published in English. The abstracts were reviewed and most relevant selected for inclusion. Citation links were hand searched to identify further articles of relevance.
Ludwig Levin Jacobson was born in Copenhagen on 10th January 1783 to a family of jewellers[1]. After attending a German school in Stockholm he returned to surgical training in Copenhagen[1,2]. His interests included human anatomy, zoology, chemistry and teaching. He is credited with various anatomical discoveries in animals and most importantly in humans[1,2]. As early as 1809 he discovered a previously undetected vomeronasal organ found in the nasal cavities of mammals only fully understood over a hundred years after his death[2]. In 1813 he would first describe the tympanic nerve outlining its anatomical relations and physiological function[1,2]. Later he also detailed the anatomy and function of Jacobson’s canaliculus (tympanic canaliculus) and “Jacobson anastomosis” plexus (tympanic plexus)[1]. By the time of his death in 1843 he had become a Professor and the King’s personal physician[1].
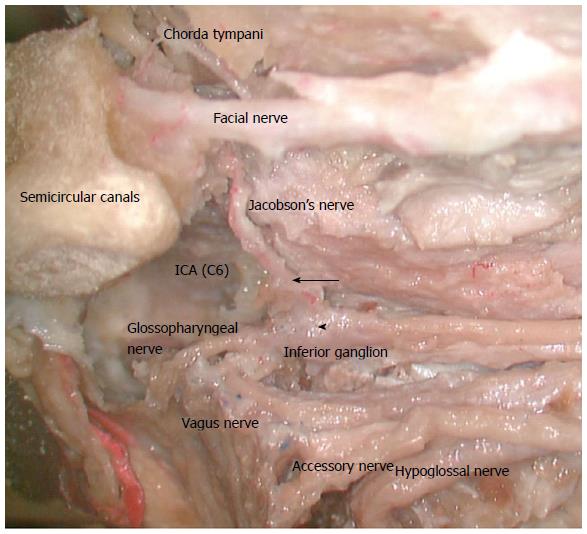
The tympanic nerve is the first branch arising from the inferior ganglion (petrous ganglion) of the glossopharyngeal nerve as it exits the jugular foramen[3-5] (Figure 1). Anatomical variations of its origin are rarely reported. Historically Arnold, cited by Donaldson, noted that the tympanic nerve may occasionally arise at a higher point than the inferior ganglion of the glossopharyngeal nerve and Cuvellier, also cited by Donaldson, suggested that it could arise from contributions from both cranial nerves IX and X[6]. These findings have not been supported by more recent studies.
The anatomical study of the tympanic nerve by Tekdemir et al[7] using ninety-six cadaveric temporal bones states that it arises from the inferior ganglion which is located at a mean distance of 11.3 mm from the genu (knee like bend). It invariably angulates at 90 degrees inferior to the genu en route to the tympanic canaliculus[7].
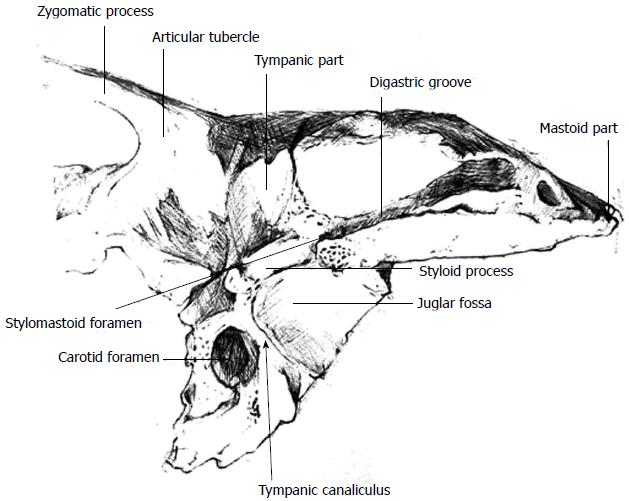
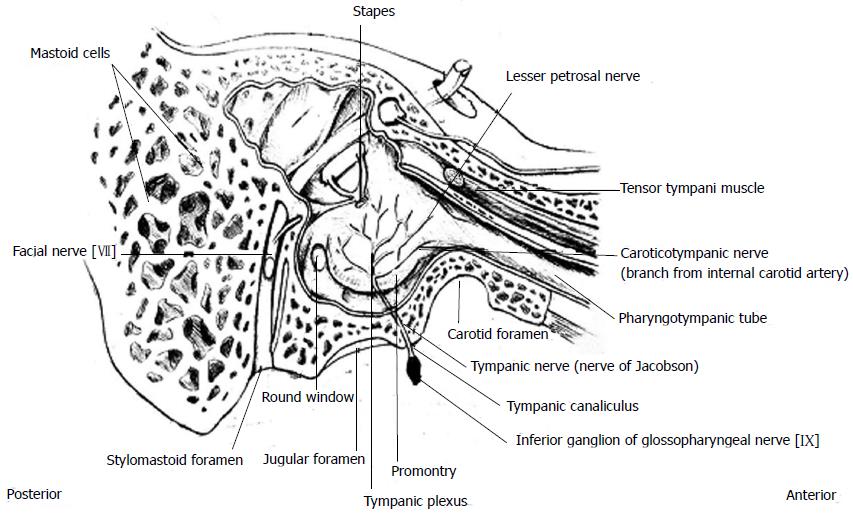
The tympanic nerve and the inferior tympanic artery enter the inferior tympanic canaliculus, a bony septum that lies between the internal carotid foramen medially and the internal jugular foramen laterally[8] (Figure 2). The tympanic canaliculus is located medial to the styloid process and the stylomastoid foramen[9]. In the tympanic canaliculus, the tympanic nerve traverses superiorly on the medial wall of the middle ear onto the cochlea promontory[6]. The auricular branch of the superior ganglion of the vagus nerve (Arnold’s nerve) courses 1-2 mm lateral to the tympanic nerve[9,10].
The mean length of the tympanic canaliculus is 9.5 mm and the inferior 2/3 of the tympanic canaliculus follows a vertical course whilst the superior 1/3 courses anteromedially at an angle between 160 and 170 degrees[7]. In the study by Tekdemir et al[7], the external opening of the tympanic canaliculus was located inside the petrosal fossula, the depression on the inferior surface of the petrous portion of the temporal bone between the jugular fossa and the carotid canal opening in 80% of cases. In the 20% of the cases where the fossula was not identifiable, the opening was found on the anterolateral aspect of the jugular bulb[7].
Porto et al[3] (20 specimens) and Tekdemir et al[7] (96 specimens) both reported findings of the tympanic nerve being covered in bone in its entire course in 5% and 20% of their specimens respectively. Donaldson, in a study of 50 temporal bones, observed that in 6% of the specimens the tympanic nerve ran part or its entire middle ear course deep to the bone of the middle ear and that in these cases there was no hypotympanic branch[6].
An aberrant course of the tympanic nerve where it coursed anteromedially within the bony septum before entering the middle ear anteriorly accompanied by the sympathetic branch from the internal carotid sympathetic plexus was reported in one of the specimens in the same study[6]. Another unusual finding was a unilateral duplication of the tympanic nerve[6].
The tympanic nerve emerges on the promontory of the middle ear, on its medial wall and anterior to the round window[3]. It exits through the internal aperture of the tympanic canaliculus which lies anterior to the inferior half of the round window[7]. The nerve divides on the promontory forming an anterior branch which courses up towards the Eustachian tube and a posterior branch that skirts the rim of the round window[11,12]. The two divisions of the tympanic nerve are often found running parallel to each other on the promontory[13]. On average the distance between Jacobson’s nerve and the lip of round window niche is 2.1 mm with a range of zero to 3.2 mm[14]. A study of 82 temporal bones demonstrated that if the main trunk of the tympanic nerve is visible on the promontory it can be concluded with 95 per cent certainty that it is within 3.3 mm of the lip of the round window niche[14].
Hypotympanic branches are common and therefore an important consideration in surgery of the tympanic nerve. One of the earliest observations on the anatomy of the tympanic nerve suggested that in 40% of cases a hypotympanic branch arises from the main trunk and runs anteriorly and below the promontory to connect to the pharyngotympanic tube recess[15]. Later studies suggests a slightly higher preponderance of a hypotympanic branch of the tympanic nerve, i.e., 50% and 48%, albeit with a variable distribution[3,6]. The hypotympanic branch can have occasional single or double divisions[3,6]. It is reportedly narrower in diameter coursing anterosuperiorly in approximately 45% of cases and posteriorly in 5%[3]. The presence of a hypotympanic branch correlates strongly with the main trunk of the tympanic nerve being covered by promontory bone for the majority of its course, only surfacing on the promontory for 1-2 mm[3]. Interestingly, two canaliculi with nerves passing over the promontory have been reported[6].
On the promontory, the tympanic nerve coalesces with the superior and inferior caroticotympanic nerves which branch from the carotid plexus to form the tympanic plexus[16-18] (Figure 3).
Even though the tympanic nerve and plexus can be found in open grooves (submucosally) on the promontory, in approximately 20% of cases its branches are hidden in bony canals of varying depth making it difficult to locate[18]. Additionally, the nerve and plexus exhibit a multitude of variations as to course, branching and anastomoses. In fact there is no bilateral symmetry; each plexus is unique[18].
The tympanic nerve has a close anatomical relationship with the cochlea; it extends superiorly directly underneath the cochleariform process[19]. Furthermore, it acts as a useful marker in identifying the anterior and posterior parts of the basal segment of the scala tympani of particular relevance in cochlear implantation[8,14,20]. Both segments are in close relation to the hypotympanic cells, infralabyrinthine cell tracts and the jugular bulb[8,14]. The preganglionic parasympathetic fibres reconstitute posteriorly to the cochleariform process, eventually lying medial to it coursing superiorly across the promontory towards the geniculate ganglion of the facial nerve[8].
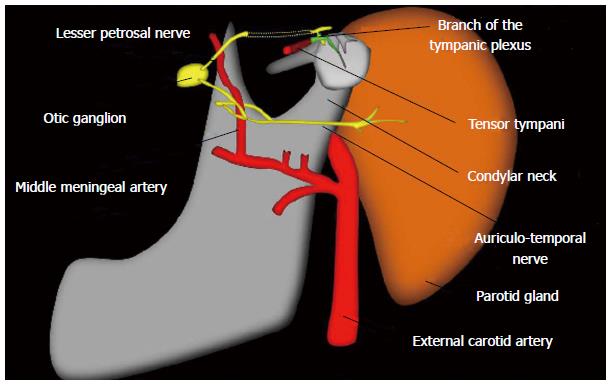
The tympanic nerve exits the middle ear through its own canal below the tensor tympani muscle or through the canal for the tensor tympani muscle as the lesser superficial petrosal nerve[20]. From the anterior surface of the temporal bone the lesser superficial petrosal nerve exits the middle cranial fossa via foramen ovale or the emissary sphenoidal foramen (canal of Vesalius) en route to the otic ganglion conveying presynaptic parasympathetic fibres[21]. The post ganglionic fibres travel with the auriculotemporal nerve, a sensory branch of the mandibular division of the trigeminal nerve to provide the parasympathetic innervation of the parotid gland[11] (Figure 4).
In addition to conveying parasympathetic fibres to the parotid, the tympanic nerve provides somatic fibres to the tympanic cavity: the medial wall of the tympanic membrane, mastoid air cells and the Eustachian tube[8,22]. Animal studies suggest that the tympanic nerve plays an important role in the regulation of middle ear pressure[23,24]. Eden et al[23,24] demonstrated the existence of a neural pathway between the tympanic plexus and the pons and the presence of efferent fibres connecting the pons and the Eustachian tube. The deduction from these studies was that the glomus bodies located along the tympanic nerve, in concert with other structures, sense changes in middle ear pressure[24]. These changes are in turn conducted to the pons via the tympanic nerve resulting in a feedback loop thereby regulating middle ear pressure[23,24]. Songu et al[25] in an attempt to replicate these findings in humans demonstrated, albeit inconclusively, that the tympanic plexus might play a more significant role in the regulation of middle ear pressure via the Eustachian tube than had been previously thought. Such findings are encouraging and more studies of this nature are required given that Eustachian tube dysfunction and its sequelae remains a difficult condition to manage within otolaryngology.
The tympanic nerve is covered in bone for most of its course and is unlikely to be damaged in trauma; injury would indicate severe force[26]. The nerve can be involved in non-traumatic pathological processes along its course, particularly within the foramen[9]. Glomus jugulare tumours, which tend to be slow growing in nature, are the commonest tumour found in the jugular foramen[9]. They have a preponderance to form along the tympanic and Arnold’s nerves as well as in the adventitia of the internal jugular vein[9,27]. In advanced stages they tend to be multidirectional in growth and owing to the narrowness of the jugular foramen may expand and erode to into cranial nerves IX to XII[9].
Tympanic nerve schwannomas have been reported but are still rare[9,27]. They are Schwann cell derived tumours which arise intracranially and then extend inferiorly along the jugular foramen[27]. Pressure erosion is common in patients with jugular foramen schwannomas but rare in glomus jugulare tumours where bony erosion is common[9].
Post-surgical traumatic neuromas of Jacobson’s nerve have been reported, usually occurring in the context of previous middle ear surgery where the tympanic nerve is damaged or severed (intentionally or otherwise) leading to formation of neuromas from nerve growth around the amputated stump, leading to recurrent otalgia[28].
Lempert first described tympanic plexus ablation for the relief of tinnitus in 1946, referring to it as tympanosympathectomy[29]. Clinical use of the procedure faltered owing to unsatisfactory results. Hemenway later suggested interruption of the efferent neuronal pathway at the level of the middle ear by sectioning the tympanic nerve as a theoretical approach to the management of Frey’s syndrome[30]. However, the procedure was later popularised by Golding-Wood who used it for the successful treatment of Frey’s syndrome coining the term tympanic neurectomy to describe it[31]. In addition to the management of Frey’s syndrome, Golding-Wood postulated other indications for the procedure notably, paradoxical gustatory lacrimal reflex “crocodile tearing” and chronic secretory otitis media although these have no indication in modern clinical practise[21]. Tympanic neurectomy has been considered useful in the management of otalgia with the proviso that other important causes of otalgia have been excluded[22].
Later Friedman added other important indications for tympanic neurectomy including parotid duct stenosis, salivary duct dilation (sialectasis) and parotid salivary fistula[21].
Owing to the potential serious complications of parotidectomy, duct ligation or radiotherapy as alternative forms of treatment for these conditions, tympanic neurectomy can be undertaken with little morbidity or operative discomfort[17]. A case series of ten patients for parotid sialectasis managed with tympanic neurectomy in the United Kingdom by Daud et al[17] demonstrated symptom alleviation in seven patients and as such is advocated by the authors as a first-line surgical procedure for such symptoms with parotidectomy in reserve.
To perform the procedure a tympanomeatal flap is raised to expose the promontory and hypotympanum[32]. Success of tympanic neurectomy lies in complete division of the tympanic nerve below its lowest intratympanic branch with the corollary that promontory branches are less significant to the success of the procedure[33]. As such adequate exposure may require drilling of the bony annulus inferiorly until the floor is flush with the hypotympanium[33]. Drilling is required medially below the basal turn of the cochlea to sever all nerve filaments[19]. A comprehensive understanding of the different anatomical segments, variations and most importantly the potential of the tympanic nerve being partially covered in bone as highlighted above is therefore crucial in the success of this procedure.
In more recent years the tympanic nerve has gained favour as a useful anatomical landmark in cochlear implantation where the classical approach to the scala tympani through the round window niche by way of facial recess is impossible[8,14]. Successful intubation of the scala tympani in such instances utilises the anatomical proximity of the tympanic nerve to the round window and the cochlea as has already been highlighted[8,14].
The tympanic nerve remains an anatomical area of complexity that is easy to overlook yet functionally its relevance to the modern clinician is ever more pertinent. It is increasingly regarded as an important operative marker in cochlear implantation due to its anatomical relations and continues to retain an important role in the management of salivary disorders. In appreciating its anatomical path, we gain an improved understanding of the arrangement of the middle ear and its dual relevance to both anatomists and surgeons.
P- Reviewer: Hortobagyi T, Mazzocchi M S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Lekakis GK. Philipp Friedrich Arnold, Ludvig Levin Jacobson and their contribution to head and neck anatomy. J Laryngol Otol. 2003;117:28-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Jacobson L, Trotier D, Døving KB. Anatomical description of a new organ in the nose of domesticated animals by Ludvig Jacobson (1813). Chem Senses. 1998;23:743-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Porto AF, Whicker J, Proud GO. An anatomic study of the hypotympanic branch of Jacobson’s nerve. Laryngoscope. 1978;88:56-60. [PubMed] |
| 4. | Goodwin WJ, Arnold D, Wachholz J. Surgical anatomy of the glossopharyngeal nerve. Laryngoscope. 1993;103:1302-1304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Van Loveren HR, Sing Liu S, Pensak ML, Keller JT. Anatomy of the jugular foramen: The neurosurgical perspective. Op Tech Otolaryngol Head and Neck Surg. 1996;7:95-98. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Donaldson I. Surgical anatomy of the tympanic nerve. J Laryngol Otol. 1980;94:163-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Tekdemir I, Aslan A, Tüccar E, Cubuk HE, Elhan A, Deda H. An anatomical study of the tympanic branch of the glossopharyngeal nerve (nerve of Jacobson). Ann Anat. 1998;180:349-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Goravalingappa R. Cochlear implant electrode insertion: Jacobson’s nerve, a useful anatomical landmark. Indian J Otolaryngol Head Neck Surg. 2002;54:70-73. [PubMed] |
| 9. | Ozveren MF, Türe U. The microsurgical anatomy of the glossopharyngeal nerve with respect to the jugular foramen lesions. Neurosurg Focus. 2004;17:E3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Ozveren MF, Türe U, Ozek MM, Pamir MN. Anatomic landmarks of the glossopharyngeal nerve: a microsurgical anatomic study. Neurosurgery. 2003;52:1400-1410; discussion 1410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 49] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 11. | Townsend GL, Morimoto AM, Kralemann H. Management of sialorrhea in mentally retarded patients by transtympanic neurectomy. Mayo Clin Proc. 1973;48:776-779. [PubMed] |
| 12. | Sinha P. Successful treatment of parotid fistula with tympanic neurectomy. Indian J Otolaryngol Head Neck Surg. 2008;60:227-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Frenckner P. Observations on anatomy of the tympanic plexus and technique of tympanosympathectomy. AMA Arch Otolaryngol. 1951;54:347-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Todd NW. Jacobson’s nerve clues to the round window niche. Cochlear Implants Int. 2009;10:63-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Allam AF. Transtympanic neurectomy in chronic recurrent parotid sialoadenitis. J Laryngol Otol. 1975;89:405-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 16. | Rosen S. The tympanic plexus: An anatomical study. Arch Otolaryng. 1950;53:15-18. [RCA] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Daud AS, Pahor AL. Tympanic neurectomy in the management of parotid sialectasis. J Laryngol Otol. 1995;109:1155-1158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Rosen S. Tic douloureux of the chorda tympani. AMA Arch Neurol Psychiatry. 1953;69:375-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 19. | Bailey BJ, Calhoun KH. Head and neck surgery-Otolaryngology. 2nd Edition. Philadelphia: Lippincott, Williams and Wilkins 2001; 342-343. |
| 20. | Schuknecht HF. Pathology of the Ear, 2nd Edition. Philadelphia: Lea and Febiger 1993; 40-41. |
| 21. | Friedman WH, Swerdlow RS, Pomarico JM. Tympanic neurectomy: a review and an additional indication for this procedure. Laryngoscope. 1974;84:568-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 22. | Cook JA, Irving RM. Role of tympanic neurectomy in otalgia. J Laryngol Otol. 1990;104:114-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 23. | Eden AR, Gannon PJ. Neural control of middle ear aeration. Arch Otolaryngol Head Neck Surg. 1987;113:133-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 36] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 24. | Eden AR, Laitman JT, Gannon PJ. Mechanisms of middle ear aeration: anatomic and physiologic evidence in primates. Laryngoscope. 1990;100:67-75. [PubMed] |
| 25. | Songu M, Aslan A, Unlu HH, Celik O. Neural control of eustachian tube function. Laryngoscope. 2009;119:1198-1202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Miyazaki C, Katsume M, Yamazaki T, Aoki K, Kuroki T, Takasu N. Unusual occipital condyle fracture with multiple nerve palsies and Wallenberg syndrome. Clin Neurol Neurosurg. 2000;102:255-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 27. | Sözen E, Uçal YO, Kabukçuoğlu F, Celebi I, Dadaş B. An incidental middle-ear mass: Jacobson's nerve schwannoma. Otol Neurotol. 2012;33:e37-e38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 28. | Naraev BG, Linthicum FH. Traumatic neuroma of the tympanic (Jacobson’s) nerve as a possible cause of otalgia. Otolaryngol Head Neck Surg. 2008;138:735-737. [PubMed] |
| 29. | Lempert J. Tympanosympathectomy; a surgical tèchnic for the relief of tinnitus aurium. Arch Otolaryngol. 1946;43:199-212. [PubMed] |
| 30. | Hemenway WG. Gustatory sweating and flushing. The auriculo-temporal syndrome--Frey’s syndrome. Laryngoscope. 1960;70:84-90. [PubMed] |
| 31. | Golding-Wood P. Tympanic neurectomy. J Laryngol Otol. 1962;76:688-693. [RCA] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 72] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 32. | Goycoolea MV, De Souza C. 2012. Atlas of otologic surgery and magic otology. New Delhi: Jaypee Brothers Medical Publishers New Delhi 2012; 443-451. [DOI] [Full Text] |
| 33. | Harrison K, Donaldson I. Frey’s syndrome. J R Soc Med. 1979;72:503-508. [PubMed] |