Published online Jul 2, 2025. doi: 10.5319/wjo.v12.i1.109355
Revised: May 14, 2025
Accepted: June 11, 2025
Published online: July 2, 2025
Processing time: 55 Days and 11.6 Hours
Otitis media with effusion (OME), glue ear, serous otitis media, or secretory otitis media is a common paediatric condition. Two widely used surgical interventions for OME are myringotomy alone and myringotomy with tympanostomy tube. While both procedures aim to improve hearing outcomes, the efficacy of these approaches has been a subject of ongoing research and debate.
To compare the efficacy of myringotomy alone and myringotomy with tympa
In this comparative study, 66 patients diagnosed as OME meeting the inclusion criteria were selected via ear, nose and throat department. They were divided into two groups randomly, each of 33 patients. In the first group (Group A) myrin
The mean age of the patients in Group A was 10.96 ± 2.76 SD but the mean age of the patients in Group B was 10.22 ± 2.73 SD (P = 0.1056). In Group A, males were 63.6% and females were 36.3%. Also in Group B, males were 63.6% and females were 36.3% (P = 1.0). In group A, post operative hearing gain using pure tone audiometry at one month was 20.45 ± 3.78 SD while in group B, post operative hearing gain using pure tone audiometry at one month was 23.84 ± 3.69 SD (P = 0.00005). However, ear discharge was noted in 3.03% cases in group A and 15.15% cases in group B (P = 0.035). By applying independent t-test, the P < 0.05 indicated that there is a significant association between Group B and hearing improvement at 4th week.
Our study concluded that myringotomy with tympanostomy tube seems to have better hearing results than myringotomy alone in treatment of OME.
Core Tip: This comparative study shows that myringotomy with tympanostomy tube offers significantly better short-term hearing improvement in otitis media with effusion patients than myringotomy alone. However, it may carry a higher risk of postoperative ear discharge.
- Citation: Basit A, Noor S, Ahmad SA, Noor N, Maryam R, Basil AM. Otitis media with effusion and hearing outcomes - Myringotomy vs myringotomy and tympanostomy: A comparative study. World J Otorhinolaryngol 2025; 12(1): 109355
- URL: https://www.wjgnet.com/2218-6247/full/v12/i1/109355.htm
- DOI: https://dx.doi.org/10.5319/wjo.v12.i1.109355
Otitis media with effusion (OME) also called as glue ear or serous or secretory otitis media is defined as the appearance of non purulent fluid in the middle ear in the absence of any associated signs or symptoms of acute ear infection usually for more than 90 days with an intact tympanic membrane[1]. It is a common disease of childhood and is the leading cause for conductive hearing loss in this population[2]. At 10 years, one out of eight children suffers from OME or 1.9% of total hearing impairment children have OME[3]. The prevalence of OME has spikes at two age groups, first at 2 years and second at 5 years which usually coincides with kindergarten and primary school time[4]. According to one study, almost 5.6% of school going children has hearing difficulty due to OME[3]. Chronic OME without treatment may lead to complications such as hearing loss and damage to the tympanic membrane like atrophy, retraction pockets and cholesteatoma. It can also cause speech learning delay which may lead to behavioral disorders and poor academic results[5]. The reason children are at higher risk of OME are due to the narrow, shorter and more horizontal position of eustachian tube along with adenoid hypertrophy besides infection, impaired eustachian tube function, immature immune status and allergy[6]. A study conducted in Rawalpindi among children aged 1–5 years reported a prevalence of 27%, with higher rates observed in males and in the 2–3 years age group. In Southern Punjab, a study found that 30.9% of patients aged 14 to 50 years had OME, with the highest infection rates among individuals aged 14 to 22 years. Another study focusing on children with recurrent upper respiratory tract infections found a frequency of 29.2% for OME.
OME is diagnosed mostly by otoscopy, pneumatic otoscopy, audiometry and tympanometry. Although tympanocentesis is the gold standard but otoscopy, pneumatic otoscopy, tympanometry and audiometry are preferred because they are economical to the patient and hospital, easy to perform, non-invasive and almost accurate means for detecting OME[2]. The hearing loss on pure tone audiometry of OME is approximately a conductive hearing loss of approximately 25 dB associated with fluid in the middle ear[7]. There are few options for the treatment of OME but which treatment option is better is a matter of debate. Neither the indications for surgical therapy nor the types and numbers of procedures are uniform[8]. Surgery involves alone or various combinations of myringotomy, tympanostomy tube placement, and adenoidectomy[9]. Myringotomy with aspiration of fluid has the direct aim of improving hearing and preventing atrophy of the drum, organization of the secretion and adhesive changes. Insertion of a tympanostomy tube (grommet) abolishes the negative pressure in the middle ear for a long period of time, and sustains ventilation of the middle ear[10].
Myringotomy with tympanostomy tube (grommet) showed favorable results of hearing improvement according to studies published by Rawalpindi Medical University in 2018 and Pakistan Airforce Hospital Jacobabad and CMH Lahore in 2020[6,10]. However another study conducted in Southern Oman and Egypt in 2020 did not showed any significant difference between both modalities but myringotomy alone showed fewer complications as compared to myringotomy with grommet[11].
In Pakistan, very limited studies are available comparing these two treatment options. So the rationale of this study is to compare treatment regarding improvement of hearing outcome of these two treatment modalities due to scarcity of available research on this topic in this country[12].
Taking reference of the previous study, a sample size of 66 patients (33 patients in each group) is estimated by using 5% level of significance, 95% power of test with expected percentage of hearing improvement by voice test after one month with Group A (Myringotomy alone) as 36% and Group B (Myringotomy with tympanostomy tube) as 75%[6].
n = {(Z(1-α/√2) × √[2P(1-P)] + Z(1-β) × √[P1(1-P1) + P2(1-P2)]) ^2}/(P1 - P2) ^2.
Where: n = Number of patients = 66.
Z1-α = 95%CI = 1.96 Z1-β = Power of test = 95%; P1 (Population proportion I) = 36% P2 (Populationproportion II) = 75%.
Non-probability convenient sampling.
Inclusion criteria: Between the ages of 5 and 15years old. Either gender. Otoscopy reveals a dull appearance of the tympanic membrane (there is no cone of light). Pneumatic otoscopy reveals that the tympanic membrane has less mobility than normal. Hearing loss detected during voice examinations. Tympanogram of type B, which might be dome-shaped or flat or negative. Agap between the air and bone conduction on the pure-tone audiogram.
Exclusion criteria: Adenoidectomy or tonsillectomy. Patients having acute otitis media. Discharging ear (Perforated tympanic membrane). Bleeding disorders. History of prior Myringotomy with or without tympanostomy tube. Cleft palate repair. Unilateral OME. Sensorineural hearing loss.
After approval from Advance Studies and Research Board, patients meeting the inclusion criteria were selected through the ENT department of the Mayo hospital Lahore. Informed written consent was taken from every patient’s attendant. Patient was randomized using lottery method and single blinded and divided into two groups as group A and group B. Patients having no co-morbidities and family history of OME were selected. All patients in group A were managed with Myringotomy alone while all patients in group B were managed with Myringotomy with tympanostomy tube. We assessed hearing outcome by Pure Tone Audiogram (PTA) pre operatively. Patients were followed up and re-assessed in outdoor patient department at 4th week postoperatively again by PTA.
Any related complications were mentioned in follow up proforma as secondary outcome and were managed as per standard protocols.
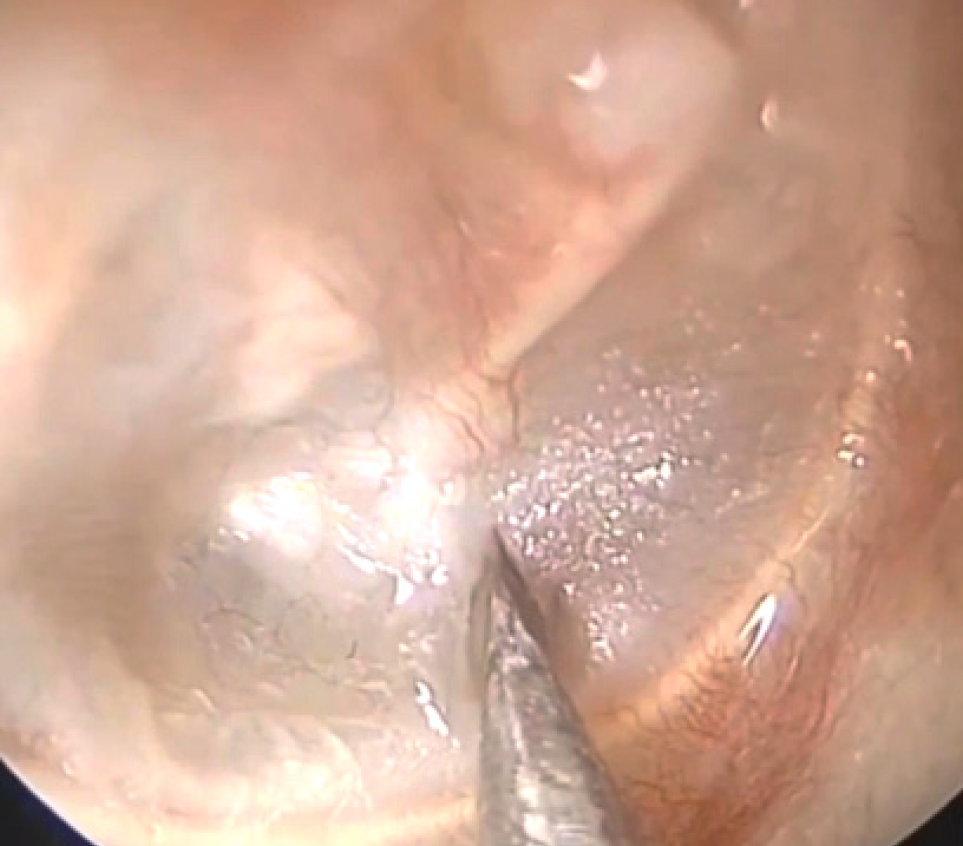
Myringotomy: All patients in group A were managed by myringotomy alone.
Patients were prepared. Informed consent were taken from patients or their attendants and put on OT table in supine position. An incision was given in the anterior inferior quadrant of tympanic membrane to drain fluid from middle ear and to relieve pressure caused by excessive build up of fluid (Figure 1).
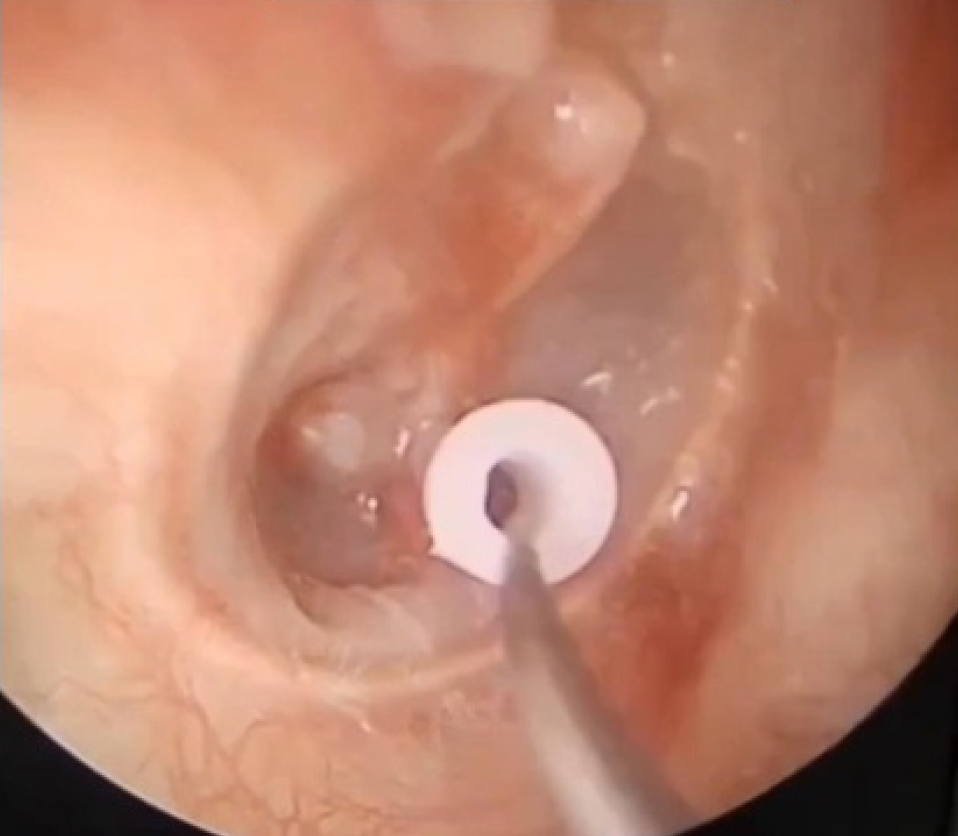
Myringotomy with tympanostomy tube (Grommet): All patients in group B were managed using Myringotomy with Tympanostomy tube (Grommet).
Patients were prepared. Informed consent was taken from patients or their attendants. After myringotomy, a grommet of appropriate size was put in the incision site to keep the middle ear cavity persistently aerated and continuously drain fluid from it (Figure 2).
Data was organized, entered and analyzed using SPSS version 26.0. Quantitative variables like age and hearing assessment by PTA were presented as mean ± SD. Qualitative variables like gender, hearing assessment by voice test and ear discharge were presented as numbers and percentages. Comparison of both groups, Group A (Myringotomy alone) and Group B (Myringotomy with grommets insertion) was done by applying independent t-test. P-value less than 0.05 was taken significant.
The average age in group A was 10.96 ± 2.76 years old while the average age in group B was 10.226 ± 2.73 with no statistically significant difference (P = 0.1056). In group A, there were males and females and in group B, there were males and females with no statistically significant difference (P = 1.0) between the two groups (Table 1).
| Group A | Group B | P value | |
| Age | 10.96 ± 2.76 | 10.226 ± 2.73 | 0.1056 |
| Gender | Male: 21 (63.6) | Male: 21 (63.6) | 1.0 |
| Female: 12 (36.4) | Female: 12 (36.4) | 1.0 |
Comparing the pre operative average hearing loss using pure tone audiometry revealed that there was no statistically significant difference in the average air bone gap between the two groups (Table 2).
| Group A | Group B | |
| Right ear hearing gap | 30.35 ± 4 | 30.15 ± 3 |
| Left ear hearing gap | 30.05 ± 3.6 | 30.79 ± 3.1 |
| Mean | 30.02 ± 3.8 | 30.47 ± 3.07 |
| P value | 0.751 | |
Hearing improvement after 4 weeks of the procedures was compared between the two groups using pure tone audiometry. There was statically significant difference between the two groups in regard of hearing improvement as Group B showed more favorable results compared to Group A (Table 3).
| Group A | Group B | |
| Right ear hearing gain | 21 ± 4.1 | 24.73 ± 4.2 |
| Left ear hearing gain | 19.9 ± 3.44 | 22.95 ± 3.12 |
| Mean | 20.45 ± 3.78 | 23.84 ± 3.69 |
| P value | 0.00005 | |
Hearing improvement after 4 weeks of the procedures was compared between the two groups using voice test. There was statically significant difference between the two groups in regard of hearing improvement as Group B showed more favorable results compared to Group A (Table 4).
| Group A | Group B | |
| Hearing gain | 14 (42.4) | 27 (81.8) |
| P value | 0.00026 | |
Post op otorrhea after 4 weeks of the procedures was compared between the two groups. There was statically significant difference between the two groups in regard of post operative otorrhea as Group A showed more favorable results compared to Group B (Table 5).
| Group A | Group B | |
| Post op otorrhea | 1 (3.03) | 5 (15.15) |
| P value | 0.035 | |
The value of P < 0.05 indicates that there is a significant association between myringotomy with tympanostomy tube and hearing improvement at 4th week.
Our study aimed to compare the outcomes of myringotomy with and without tympanostomy tube in patients with OME. In our study the mean age of the patients in myringotomy alone is 10.96 ± 2.76 SD but the mean age of the patient in myringotomy with tympanostomy is 10.226 ± 2.73 SD. In myringotomy alone, males were 63.7% and females were 36.3%. Also in myringotomy with tympanostomy, males were 63.7% and females were 36.3%.
An operation considered as futile till the last century has come a long way to be now performed as one of the most common procedures in the United States with almost 700000 children undergoing myringotomy +/- grommets insertion for OME. No clear cut treatment has been devised for treatment for OME yet, that is why it’s treatment expands from observation and waitful watching to medical to different surgical approaches each having its own pros and cons with none having superiority over others which makes it a colossal topic needed to be explored. Previously, the studies have evaluated the effectiveness of myringotomy with tube insertion, myringotomy alone, adenoidectomy and no surgical intervention. This study revolves around myringotomy +/- grommets insertion excluding the other parameters. A study conducted in Egypt in which two groups A (Myringotomy with tympanostomy tube) and B (Myringotomy alone) was formed each having 37 children. There was no significant hearing difference achieved between both groups. Infact Group B showed more complications like otorrhea and myringosclerosis[11]. In another study conducted in Rawalpindi Pakistan, there were two groups A (Myringotomy alone) and group B (Myrinogtomy with grommets insertion) in which 30 children were taken in each group. Hearing improvement was noted in only 36% in group A while 75% in group B after one month which proved better outcomes in group B[6]. In another study in Jacobabad Pakistan, 28 patients were divided into group A (Myringotomy alone) and Group B (Myringotomy with grommets insertion) with group B having better hearing outcomes at one month interval[10]. Yet in another study 78 patients were subjected to myringotomy +/- tympanostomy tubes but no significant statistical difference was noted in hearing improvement after one month. Even in another study, 52 children were divided into two groups for myrinogotomy alone and myringotomy with grommets insertion, but no difference was seen between hearing outcome[13,14]. But another study showed considerable hearing improvement in children with myringotomy with tympanostomy tube than myringotomy alone. Even another study in Turkey showed better results in hearing with myringotomy with tympanostomy as compared to myringotomy alone[12]. In these studies, adenoidectomy was kept as a constant factor without affecting the hearing outcome. According to one study myringotomy alone did not resulted in better hearing outcomes as compared to myringotomy with tympanostomy tubes.
Our study found out that in myringotomy alone, post operative hearing gain using pure tone audiometry at 4 weeks was 20.45 ± 3.78 SD while in myringotomy with tympanostomy tubes, post operative hearing gain using pure tone audiometry at 4 weeks was 23.84 ± 3.69 SD (P = 0.00005). Also on voice test, hearing improvement in myringotomy alone at 4 weeks was noted in 14/33 (42.4%) cases while hearing improvement in myringotomy with tympanostomy tubes at 4 weeks was noted in 27/33 (81.8%) cases (P = 0.00026)[13]. However ear discharge was noted in 3.03% cases in myringotomy alone and 15.15% cases in myringotomy with tympanostomy tubes (P = 0.035). By applying independent t-test, the P < 0.05 indicated that there is a significant association between myringotomy with tympanostomy tube insertion and hearing improvement at 4th week. So according to our study, although hearing improvement is seen more in myringotomy with tympanostomy tube insertion, but complications like ear discharge were also noted to be more in this group which warrant further studies to assess benefit vs risk for this procedure[15,16].
This study will help us to use better treatment options in OME for good outcomes in terms of hearing outcome in our setup. It may also decrease surgical procedure failure rates, patient’s morbidity also decrease expense burden on patients and on hospitals. It may also help us in decreasing readmission rates and controlling hearing loss.
Our study concluded that myringotomy with tympanostomy tube seems to have better treatment results than myringotomy alone in treatment of OME.
| 1. | Zernotti ME, Pawankar R, Ansotegui I, Badellino H, Croce JS, Hossny E, Ebisawa M, Rosario N, Sanchez Borges M, Zhang Y, Zhang L. Otitis media with effusion and atopy: is there a causal relationship? World Allergy Organ J. 2017;10:37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 2. | Minovi A, Dazert S. Diseases of the middle ear in childhood. Head Neck Surg. 2014;13:Doc11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 25] [Reference Citation Analysis (0)] |
| 3. | Vanneste P, Page C. Otitis media with effusion in children: Pathophysiology, diagnosis, and treatment. A review. J Otol. 2019;14:33-39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 71] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 4. | Khan MA, Alamgir A, Musharaf M. Comparison of outcome of myringotomy alone with myringotomy and tympanostomy tube (Grommet) in otitis media with effusion (OME). J Rawalpindi Med Coll. 2018;22:140-3. |
| 5. | Zada B, Muhammad T, Habib M, Iqbal Z, Saleem R, Rasheed MT. Efficacy of Grommet Insertion for Improvement in Hearing among Patients of Secretory Otitis Media. PJMHS. 2021;15:1857-1859. [DOI] [Full Text] |
| 6. | Browning GG, Rovers MM, Williamson I, Lous J, Burton MJ. Grommets (ventilation tubes) for hearing loss associated with otitis media with effusion in children. Cochrane Database Syst Rev. 2010;CD001801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 90] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 7. | Wallace IF, Berkman ND, Lohr KN, Harrison MF, Kimple AJ, Steiner MJ. Surgical treatments for otitis media with effusion: a systematic review. Pediatrics. 2014;133:296-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 50] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 8. | Akhtar S, Gul U, Jawaid A, Azam K, Niazi MSB, Najam A. Myringotomy for the treatment of otitis media with effusion; a comparison of the outcome with and without grommet insertion. PAFMJ. 2021;71:S521-25. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Abdel Tawab H. Myringotomy with versus without grommet tube insertion in chronic serous otitis media with effusion: Southern Oman experience. Egyptian J Ear, Nose, Throat Allied Sci. 2020;21:82-87. [DOI] [Full Text] |
| 10. | Moffa A, Giorgi L, Fiore V, Baptista P, Cassano M, Casale M. Water protection in paediatric patients with ventilation tubes: Myth or reality? A systematic review. Acta Otorrinolaringol Esp (Engl Ed). 2022;73:246-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | d'Eon B, Hackmann T, Wright AS. The Addition of Intravenous Propofol and Ketorolac to a Sevoflurane Anesthetic Lessens Emergence Agitation in Children Having Bilateral Myringotomy with Tympanostomy Tube Insertion: A Prospective Observational Study. Children (Basel). 2020;7:96. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Popova D, Varbanova S, Popov TM. Comparison between myringotomy and tympanostomy tubes in combination with adenoidectomy in 3-7-year-old children with otitis media with effusion. Int J Pediatr Otorhinolaryngol. 2010;74:777-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Vlastos IM, Houlakis M, Kandiloros D, Manolopoulos L, Ferekidis E, Yiotakis I. Adenoidectomy plus tympanostomy tube insertion versus adenoidectomy plus myringotomy in children with obstructive sleep apnoea syndrome. J Laryngol Otol. 2011;125:274-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Rasheed AM. Adenoidectomy with myringotomy and tympanostomy tube versus adenoidectomy with myringotomy in treatment of otitis media with effusion in 5-7 years old children. Al-Kindy Coll Med J. 2016;12:83-6. |
| 15. | Yegin Y, Çelik M, Olgun B, Koçak HE, Kayhan FT. Is ventilation tube insertion necessary in children with otitis media with effusion? Otolaryngol Pol. 2015;69:39-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Raza M, Jalil J, Shafique M, Ghafoor T. Frequency of Otitis Media with Effusion in recurrent upper respiratory tract infection in children. J Coll Physicians Surg Pak. 2008;18:226-229. |