Peer-review started: April 18, 2023
First decision: May 9, 2023
Revised: May 10, 2023
Accepted: May 19, 2023
Article in press: May 19, 2023
Published online: May 31, 2023
Processing time: 43 Days and 1.1 Hours
Steroid-induced psychosis is a common adverse effect of steroid exposure. Reported cases were mostly related to rheumatologic disease. Despite its high incidence, there is only one case reported related to perioperative steroid replacement for pituitary adenoma surgery. This manuscript presents the second case of such and compared the two with the latest literature review of steroid-induced psychosis.
This is a case of an adult male with a chief complaint of auditory hallucinations and was referred by Neurosurgery to Psychiatry Out-patient department. He was diagnosed with pituitary adenoma who underwent trans-sphenoid excision of the mass from which steroid exposure led to steroid-induced psychosis. Also, patient had a history of psychiatric illness of severe depressive episode. At the out-patient department, patient was started on antipsychotic, Risperidone, which led to eventual improvement of his symptoms.
The two cases of pituitary adenoma surgery with steroid-induced psychosis had almost similar clinical profile with the latest literature review of steroid-induced psychosis. However, the present case highlights the association of psychiatric illness in predisposing an individual in developing it. Also, this manuscript emphasizes that early recognition of steroid-induced psychosis leads to better prognosis. Multispecialty treatment is vital in the holistic management of the patient with timely referral and close coordination.
Core Tip: This case report supports the association between a history of psychiatric illness with higher incidence in developing steroid-induced psychosis. Also, the higher dosage of steroid exposure can cause earlier manifestation of psychotic symptoms. Steroid dosage was observed to be directly proportional to the severity of psychosis. Later improvement may be due to the delayed initiation of antipsychotics. Multispecialty treatment is vital in the holistic management of the patient with timely referral and close coordination. Lastly, proper determination of indication and minimum dose of steroids in patients undergoing pituitary surgery must be done so as to avoid any perturbing complications.
- Citation: Aranas DR, Tangalin JA. Steroid-induced psychosis related to pituitary adenoma status post trans-sphenoid excision and a history of psychiatric illness: A case report. World J Neurol 2023; 9(3): 28-36
- URL: https://www.wjgnet.com/2218-6212/full/v9/i3/28.htm
- DOI: https://dx.doi.org/10.5316/wjn.v9.i3.28
Steroid-induced psychosis is categorized by the Diagnostic and Statistical Manual of Mental disorders, fifth edition, as a form of substance/medication-induced psychotic disorder with the following criteria: psychosis occurred after exposure to psychedelic substances/medications, which cannot be better explained by another condition or substance and does not occur during the course of a delirium[1]. Lastly, it must cause significant distress and functional impairment. With those requirements, this condition is a diagnosis of exclusion, hence other potential differential diagnoses must be ruled out such as infectious, other substance-use related condition, metabolic, neurologic, vascular and other medical causes. The frequency of steroid-induced psychosis is estimated at under 5% from review of cases and clinical study literature, much of this focused on rheumatologic conditions[2]. Despite the high incidence of steroid-induced psychosis, there is only one case report about the occurrence of it after perioperative steroid replacement for pituitary adenoma surgery published by Mizutani et al[3] in 2015. Currently, there are no clear guidelines regarding the dose and period of steroid replacement for pituitary adenoma surgery hence, it varies in every institution. This report supports the highlighted risk of steroid psychosis associated with it.
This manuscript has the following objectives: (1) To present a rare case of an adult male with Pituitary adenoma status post transphenoid excision with steroid-induced psychotic disorder and history of severe depressive episode; (2) To discuss the biological, psychological, and social factors in the development of his disorder, as well as treatment and management; and (3) To compare the findings of the latest literature review of steroid-induced psychosis with the two cases related with pituitary adenoma and discuss the currently suggested guidelines for the perioperative assessment and management of pituitary surgery.
Referred by his attending neurosurgeon for evaluation and management of auditory hallucinations status post Trans-sphenoid excision of Pituitary Adenoma.
18 years prior to consultation, the patient was apparently well until his wife left their family to work abroad as a factory worker and then cut off communications with them. Patient had a severe depressive episode in reaction to this event. He had a depressed mood and lost interest in his daily activities with associated poor sleep and poor appetite however denied thoughts of death and suicidal ideations. Patient had feelings of betrayal and worthlessness. Patient had a constant feeling of fatigue that slowed him down. He preferred staying in his room ruminating about what he did wrong to deserve the abandonment. Patient had diminished concentration at work and would often forget his tasks. The depressive episode lasted for 2 wk with no noted psychosis. No excessive alcohol drinking and no use of illicit drugs. No noted manic or hypomanic episodes. No medical condition noted. The patient coped by focusing on his furniture shop business and in taking good care of his two young children.
Interim revealed that the patient was apparently well until four years prior to consultation when the patient had an onset of intermittent flickering of vision. This was disregarded by the patient until two years prior to consultation, the patient started to have visual field loss on the temporal side of the left eye. He thought of this as the result of his frequent exposure to direct heat of the sun as he works in his shop and felt that he was neglecting his health due to over working. Patient then decided to seek consultation with an optometrist to acquire eye glasses which he claimed to have provided temporary relief of his condition. However, one year prior to consultation, his right eye then started to have loss of vision on the temporal side also, however now with associated intermittent headaches. Patient noted that it affects his performance in making furniture however disregarded it. No noted depressive or manic episodes. No substance use or medications taken. No psychosis noted.
One year prior to consultation, due to the persistence of the problem with vision, the patient decided to seek consultation with an ophthalmologist and was diagnosed with bitemporal hemianopsia. The ophthalmologist explained that the problem with his vision were not primarily age-related eye diseases and that a mass in his brain was causing it. Upon hearing this, the patient asked about the etiology of this mass as he was shocked and anxious of it. Further testing was suggested and he was assured by the ophthalmologist that there was treatment of his condition. Patient complied with the advised and there were no depressive episodes noted as he confided all his worries to his partner. And so, MRI was immediately done showing heterogeneously enhancing sellar/suprasellar mass measuring 2.4 cm × 2.73 cm × 3.0 cm with considerations of pituitary macroadenoma or craniopharyngioma. The ophthalmologist referred the patient to a neurosurgeon in their local institution where consult was done. It was explained that surgical intervention was needed to address his problem in his vision however the nature of his disease and etiology was not understood by the patient. Patient felt anxious at first about the said procedure and the expenses for it. Patient decided to close his furniture shop and allocate his savings for his procedure. His partner assured him that she and other relatives will help him financially. Patient remained hopeful that he will be cured with the help of his doctors however, he was hold on queue for surgery in the government hospital during the pandemic. Hence, patient was repeatedly told to wait for schedule as elective surgeries were not the priority at the height of the pandemic. Patient understood the situation and that being safe from coronavirus disease 2019 (COVID-19) was his first priority. No noted depressive or manic episode. The patient then received a recommendation to seek consultation in our institution.
Upon consultation in our institution, preoperative endocrine studies were done to assess the hypothalamic-pituitary-adrenal axis: Serum growth hormone, 0.04 ng/mL; free thyroxine, 12.68 pmol/L; cortisol, 274.20 nmol/L; and ACTH, 23.70 pg/mL. Hence, the patient was diagnosed with a non-functioning pituitary adenoma. Patient was then scheduled for admission the next month for trans sphenoidal excision of sellar-suprasellar mass. Patient thought that the fast catering of service in the institution helped him feel relieved and that securing a schedule immediately made him feel hopeful once again. Even though, he still did not understand very well the nature and course of his disease, he chose to trust his doctors as he had great confidence with their competency as endorsed by a relative to him.
Upon admission, the patient had routine laboratory tests done including pre-operative Head computed tomography (CT) scan – plain. Patient was started on Dexamethasone 4 mg/tab 1 tablet twice a day among other drugs for perioperative preparation. The patient was referred to Internal Medicine for cardiopulmonary clearance and to Anesthesiology for pre-operative orders. There was no noted anxiety in the patient. Pt. had good sleep and appetite. No depressive episode noted. On his first hospital day, patient claimed that he was emotionally prepared for the day of his operation with the help of his faith and he had no anxiety or fear related to it as he prayed for guidance and strength. He was grateful for receiving the chance to be operated on even though there was still the pandemic. No depressive or manic episode noted. On his second hospital day, the patient underwent cardiopulmonary clearance and was classified as having 3.9% risk in developing cardiac complications with low to intermediate risk in developing pulmonary complications. These risks and possible complications like excessive bleeding and other possible morbidity were explained and understood by the patient. No noted depressive or manic episode noted. Oral Dexamethasone was shifted and increased to 4 mg/mL intravenous every 6 h. Patient received a total of 12 mg of Dexamethasone before the operation.
On his third hospital day, patient was primed for operation and oriented about the procedure to be done. Patient thought that everything would work out well and he will soon regain his normal vision. No anxiety or fear was noted at the operating room. The patient then underwent surgery under general endotracheal anesthesia via endoscopic endonasal approach. There were no surgical complications during and after the procedure. Patient continued to receive Dexamethasone 4 mg intravenously every six hours. No complications of anesthesia immediately post operation. However, at the post-anesthesia care unit, patient experienced a transient elevated blood pressure ranging from (140-150/100-110) for which patient was started on Nicardipine drip 10 mg in 90 cc Plain Normal Saline Solution titrated at 5 mL/h to maintain blood pressure of ≤ 140/90.
On the fourth hospital day and post-operative day (POD) 1, the patient has recovered from immediate effects of anesthesia with stable vital signs, fully awake, conversant and able to follow commands. Patient was for Head CT scan prior to transfer to the ward however was uncooperative due to persecutory delusion that the nurses and doctors are planning to harm him. Patient had an anxious mood and withdrawn behavior. At this time, there were no noted fever, headache, disorientation and problem with attention in the patient. After verbal pacification and assurance by his live-in partner, the patient agreed to do the imaging test. Even after the procedure, the patient claimed that his vision improved however now characterized as blurry with white hazy smoke for both eyes. Patient thought that this will just be temporary and hoped that it will soon fade. No depressive or manic episodes noted.
On the fifth hospital day and POD 2, the patient continued to receive Dexamethasone 4 mg/mL intravenously every six hours. The patient was now at the surgery ward and was observed by his lived-in partner to have persistence of his anxious mood however now associated with poor sleep. Patient claimed to be having an auditory hallucination that he heard the nurses planning to put poison in his medications. Patient also had a delusion of thought broadcasting that people around him could read his mind. Also, patient had a command hallucination of telling him to run away from the hospital. The patient acted on his persecutory delusion and became agitated. He began pulling out all of his intravenous lines and demanded to go home. He then refused to take all of his medications. Patient and live-in partner then opted for discharge against medical advice despite the explanation of the patient’s condition, risks and consequences of their decision including disability, infection and death. Patient was given home medications including Dexamethasone to be tapered over 11 days (PODs 3, 4, and 5 - 4 mg/tab 1 tablet every 6 h for 3 d, PODs 6, 7, and 8 - 1 tablet thrice a day for 3 d, PODs 9, 10, and 11 - 1 tablet twice a day for 3 d, PODs 12 and 13 – ½ tablet twice a day for 2 d).
For PODs 3, 4, and 5, patient went back to his house together with his live-in partner still with persistence of his psychosis however the episodes were intermittent. The patient only wanted to stay inside their house, closed and covered all the windows, due to fear of the outside light. Patient falsely believes that he was implanted with magnets and that if he were to go out he would be dragged away. Patient claimed that a voice told him to run away and so he did. His eldest son tried to calm him down however was not verbally pacified. Patient was apprehended and brought back to their house. No consultations were done despite the persistence of psychotic episodes. His family did not want to seek psychiatric consultation as they fear that the patient will be institutionalized which they deemed unnecessary. Patient continued his home medications as supervised by his live-in partner.
For PODs 6, 7, and 8, the patient was already able to go out of their house however falsely believed that the people around him could read his mind. No agitation or aggression noted. Patient was able to care for himself and had good interaction with family.
For the last of the days of dexamethasone tapering doses, the only psychosis that persisted was the auditory hallucination of a voice telling him to run away. However, the patient had better impulse control and did not act on it.
In the interim, patient was able to function again by being able to do self-care, relate well at home, and socialize with other people but this was lower level unlike his baseline functioning due to the persistence of blurred vision. As he could no longer work in his furniture shop, drive his motorbike, and had difficulties doing house hold chores. Hence, patient had lowered self-esteem. However, the patient did not experience any depressive or manic episodes. No feelings of worthlessness and hopelessness. As the patient was supported by his partner financially and emotionally and was able to confide his worries to her most of the time. Due to the persistence of his auditory hallucination and blurring of vision, the patient decided to have a follow-up consultation with his Neurosurgeon and was then referred to the Psychiatry department for evaluation and management regarding his hallucinations; hence, consult.
Patient was diagnosed with Pituitary adenoma in August 2022 for which he underwent trans-sphenoidal excision of sellar-suprasellar mass last September 15, 2022. Patient had a history of severe depressive episode without psychotic symptoms last 2005, however, no consult was done and no medications taken. Patient had no history of seizures, head trauma, and loss of consciousness. No comorbidities like hypertension, cardiac disease, diabetes, or thyroid disease. The patient also denies any substance use.
There is no psychiatric or neurologic condition present in the family. No one in the family had substance abuse or attempted suicide. There is no history of diabetes, hypertension, cancer, neurologic diseases, cardiac diseases, and stroke in the family.
Patient had an unremarkable physical and neurologic exam except for the remarkable visual acuity of the patient: 20/400, right eye and no light perception, left eye.
Laboratory tests requested were all unremarkable except for the lipid profile indicating hyperlipidemia. Patient had low high-density lipoprotein and elevated low density lipoprotein, triglycerides, and total cholesterol. At the psychiatry out-patient department, postoperative hormone status was rechecked and revealed unremarkable results with normal morning cortisol level of 20.38 μg/dL.
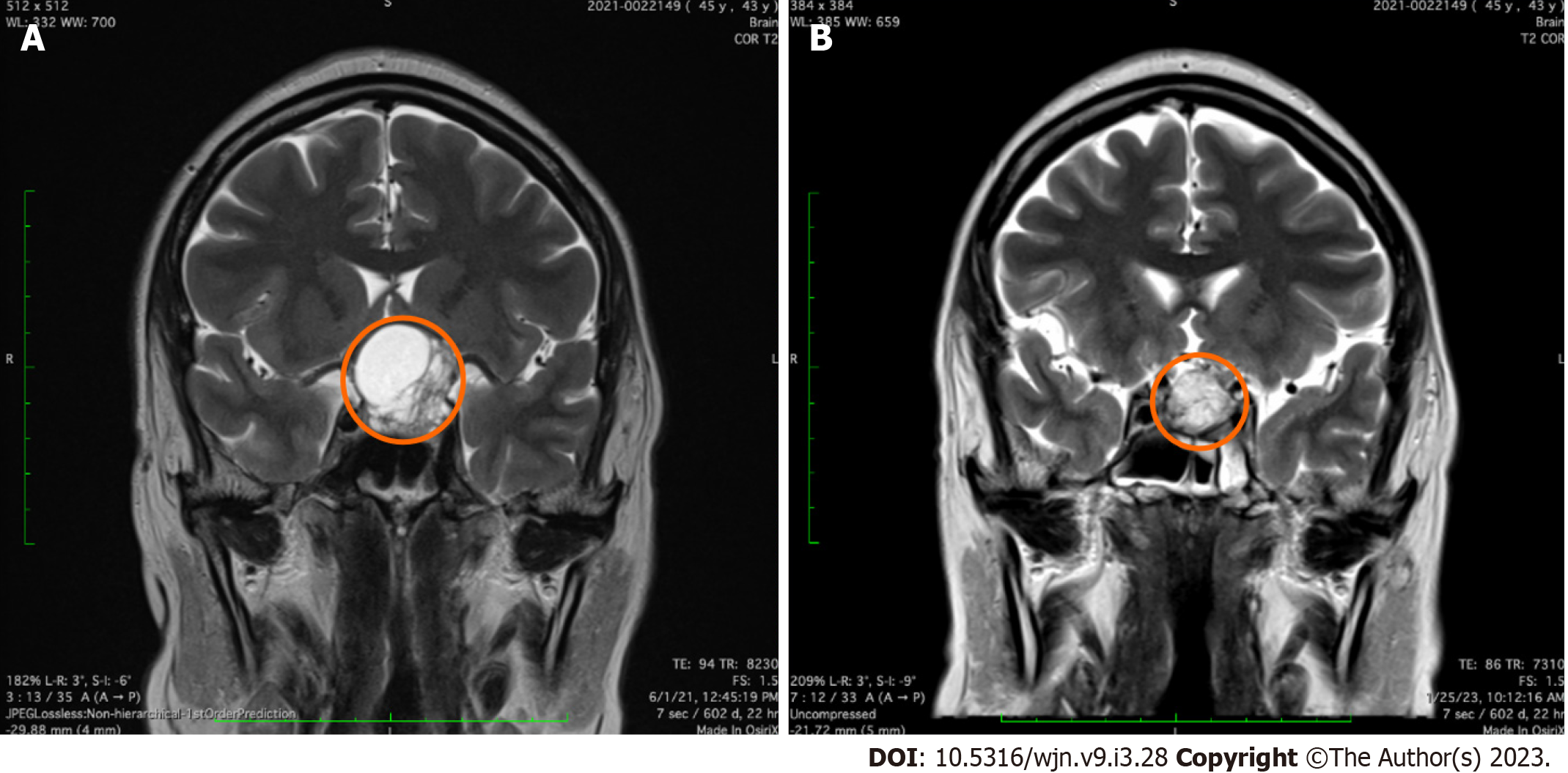
Magnetic Resonance Image - T2 Weighted Image of the Brain Coronal view with the location of the mass presented in Figure 1: (1) Preoperative image - heterogeneously enhancing sellar/suprasellar mass measuring 2.4 cm × 2.73 cm × 3.0 cm with considerations of pituitary macroadenoma or craniopharyngioma; and (2) Postoperative image – interval decrease in size of the sellar-suprasellar mass that appears as a T1W/T2W isointense signal surrounding a fat intensity signal, now measuring 1.5 cm × 1.9 cm × 1.8 cm which still abuts the bilateral carotid arteries and obliterates the suprasellar cistern. The residual intrasellar tumor noted may have caused the minimal improvement of the patient’s visual acuity as its mass effect, however this does not contribute to the psychosis experienced by the patient.
Patient had a final diagnosis of International Classification of Disease-10: Psychoactive substance-induced (steroid) psychotic disorder with delusions and hallucinations; Severe depressive episode without psychotic symptoms; Pituitary adenoma status post trans-sphenoid excision, Hyperlipidemia and Diagnostic Statistical Manual 5: Substance/medication induced (steroid) psychotic disorder; Major depressive disorder, single episode, without psychotic features.
For the management, ideally the patient should have tapering or if possible discontinuation of steroid therapy at the onset of his psychosis during admission. Referral to Psychiatry department should have been done at the ward level and atypical antipsychotic should have been started by that time as well. The biological treatment of choice given for the patient was Risperidone. According to the recent review of efficacy and safety of medications used in the management of steroid-induced psychosis, atypical antipsychotics had established effectiveness in treating steroid psychosis. Among other atypical antipsychotics, Risperidone and Olanzapine were more effective for the positive symptoms such as hallucinations and delusions present in steroid psychosis[4]. Olanzapine was noted to be related to more adverse metabolic effects[5]. In the patient, his body mass index is within normal however his lipid profile revealed hyperlipidemia. Hence, Risperidone 2 mg/tab 1 tablet once a day at bed time, was started for the patient at the Out-patient department upon referral by Neurosurgery. This was the minimum dose to check efficacy and be able to go low and slow in the dosaging of his medication. The increase in his dosage, Risperidone 2 mg/tab 1 tablet twice a day, was done after 4 wk of administration with minimal response.
Ideally, the psychological treatment should also have been started for the patient in his admission. Standard nonpharmacological methods such as nursing by familiar faces, adequate ambient lighting, regular assurance and reorientation, de-escalation and gentle distraction when necessary should have been done at the ward[2]. As well as, psychoeducation and supportive psychotherapy however these were catered at the out-patient department.
Intermediate treatment plans were to continue his medication, supportive psychotherapy, and continue referral and coordination with the multispecialty team for the holistic care of the patient.
Long term treatment plans include tapering and subsequent discontinuation of antipsychotic medication and still with regular follow up consultation for observation of his overall condition. Socially, the minimum goals were to maintain his good interpersonal relationship and ensure good family support.
Patient had recovered from the effects of steroid. Patient continued consultation for long-term treatment plans.
Steroid psychosis is a common complication of steroid therapy. This case report presents the second patient who underwent perioperative steroid replacement for pituitary adenoma surgery and then experienced an adverse effect of steroid-induced psychosis. However, an important predisposing factor noted in this case was the history of psychiatric illness which was severe depressive episode. In the latest literature review of steroid-induced psychosis by Huynh et al[4] in 2021, majority of the cases were without history of psychiatric illness however history of anxiety and depressive disorders were identified in a few cases. This case report supports the association observed in various studies that a history of psychiatric illness and/or history of previous steroid-psychosis are associated with higher incidence in developing it[6-8].
In order to understand the history of mental illness in this case, the theoretical model of self-psychology developed by Heinz Kohut needs to be applied[9]. This theory focuses on external relationships and their impact on the development of self-esteem and self-cohesion[9]. Examining the patient’s anamnesis, he did not experience developmental stunting as related to empathic failures in his mother. At an early stage he was not arrested in the evolution of the structure of the self. However, according to Kohut the needs of mirroring and idealization continues throughout life[9]. In the patient’s adulthood when his wife was his self-object not satisfying his needs for idealizing and mirroring for the maintenance of the self that was the time he experienced disintegration of the self-object. When his wife left him and cut-off their relationship abruptly after all that he has done to help her he was not reciprocated leading to feelings of abandonment and betrayal which lead to the manifestation of severe depressive episode. The patient was able to cope by employing mature defense mechanism of altruism in committing himself to the needs of his children. Another important factor in his eventual recovery from depression was when he found a loving and supportive partner who accepted him and his children. These secured his sense of self once again.
However, the maintenance of his self-esteem was again challenged when he experienced blurring of his vision and eventually diagnosed with pituitary adenoma. He had poor understanding of the nature and course of his disease and had anxiety about the uncertainties of his condition. On top of that, patient experienced delays in treatment brought by the COVID-19 pandemic. The need for trans-sphenoid excision of the pituitary adenoma precipitated the development of steroid-induced psychosis from receiving a high dose ranging from 26.7-106.7 mg of prednisone or its equivalent per day. Exposure to high dosage of steroids caused stress on the hypothalamus-pituitary adrenal axis leading to deleterious effects on cognitive function caused by a change of metabolic needs that can shrink the hippocampus[4]. The psychosis manifested brought about by the increase of dopamine that may be attributed to the induction of tyrosine hydroxylase by the steroid[4].
Several factors perpetuating the complication were identified including continuing exposure to steroid and late initiation of antipsychotic medications. Hence, the persistence of steroid-induced psychosis lowering the level of functioning of the patient at home and at work. Aside from that, there was also persistence of blurring of vision even after his operation. All of this led to him having a low self-esteem. However, no noted depressive episodes in response to these events.
As there are various protective factors identified as well, patient was eventually referred to Psychiatry and he was noted to have good adherence with treatment regimen which can be attributed to his trust and confidence to the medical team covering multispecialty treatment for his condition. Hence, the patient has sustained a positive outlook or optimism in his future. With good support system from partner and family, strong spirituality, and financial stability the patient had been able to recover from his complication.
In this manuscript, a summarized clinical profile of Steroid-induced Psychosis from the study of Huynh et al[4] was compared with the clinical profile of the 2 cases of Steroid-induced Psychosis associated with excision of pituitary adenoma presented in Table 1.
| Parameters | Latest literature review of steroid-induced psychosis (Huynh et al[4], 2021) | Mizutani et al[3], 2015 | Aranas & Tangalin, 2023 |
| Age | Mean age of 42.54 yr old | 35 yr old | 47 yr old |
| Sex | Cases were mostly male; Female sex – proven risk factor | Male | Male |
| Indication for steroids | Suppression of inflammatory processes and the immune system | Perioperative steroid replacement | Perioperative steroid replacement |
| Steroids (prednisone equivalent in average (mg/d) | Prednisone, Prednisolone, Methylprednisolone, Dexamethasone, Hydrocortisone, Triamcinolone, Betamethasone; (15-1250 mg of prednisone/d) | Hydrocortisone 10-300 mg/d; (2.5-75 mg of prednisone/d) | Dexamethasone 2–16 mg/d; (26.7-106.7 mg of prednisone or its equivalent per day) |
| Duration of steroid therapy | Shortest: < 2 d; Longest: 2 yr; Mostly within 3 d up to 6 mo | 8 d | 11 d |
| Onset of psychosis from 1st dose of steroids | Earliest: < 24 h; Latest: After 2 yr of chronic use; Mostly within 2 da to up to 2 wk | 4 d | 1 d |
| Symptomatology | Most common: Delusions & hallucinations; Others: Insomnia, agitation, irritability, combativeness, confusion, cognitive impairment, mania, depression, and suicidal ideation | Elated and irritable mood, grandiose and persecutory delusions, anxiety, and agitation | Anxious mood, persecutory delusions, thought broadcasting, auditory hallucination, agitation |
| History of Psychiatric illness | Majority without psychiatric illness; Anxiety disorder; Depressive disorder | None | Severe depressive episode without psychotic symptoms |
| Steroid management following diagnosis of psychosis | Discontinued – quicker resolution; Tapered | Tapered (7 d) | Tapered (11 d) |
| Pharmacologic intervention | Typical antipsychotics: Haloperidol, Levomepromazine, perphenazine, & zuclopenthixol; Atypical antipsychotics: Risperidone, Olanzapine & Quetiapine; Mood stabilizers: Lithium & Valproic acid; Benzodiazepines: Clonazepam, diazepam, lorazepam, & Flunitrazepam | Atypical antipsychotic: Risperidone | Atypical antipsychotic: Risperidone |
| Recovery/Improvement | Earliest: 1 mo; Longest: 8 wk | 4 d | 3 wk |
The mean age of patients in the latest review was 42.54 years old with more male cases identified in the study. This is close to the mean age of the 2 cases which is 41 years old with both being of male sex. However, according to studies female sex was a proven risk factor in developing the condition[2,10,11]. As for the common indication for steroid use in the review, it was generally for suppression of inflammatory processes and the immune system however for pituitary adenoma surgery the perioperative steroid replacement was for the prevention of associated complications related with hypoadrenalism[4]. The steroid dosage given for the cases included in the review ranges from 15-1250 mg of prednisone or its equivalent per day. The case of Mizutani et al[3] received a lesser steroid dosage range from 2.5-75 mg of prednisone/d while the present patient higher ranging from 26.7-106.7 mg of prednisone/d. The steroid utilized in this case report was Dexamethasone 2-16 mg/d, with 0.75 mg of it being equivalent to 5 mg of Prednisone. The higher the dose of steroid used has been implicated to be associated with higher incidence of steroid-induced psychosis[2]. For patients who received ≥ 40 mg/d of prednisone, the risk sharply increases to 4.6% and even more drastic increase for ≥ 80 mg/d rising to 18.4%[12,13].
In the latest review, the shortest duration of treatment was less than 2 d while the longest was 2 years. Mostly were within 3 d up to 6 mo. The case of Mizutani et al[3] had shorter duration of treatment and the present patient had longer exposure of steroid therapy, 8 and 11 d, respectively. The earliest onset of psychosis from the 1st dose of steroid exposure in the latest review was < 24 h. And the latest was after 2 years of chronic use. Mostly were within 2 d up to 2 wk. On the other hand, Mizutani et al[3] noted the presentation of psychosis in his case was at postoperative day 4 while in the present patient it was earlier at postoperative day 1. According to several studies, presentation of psychosis for most cases was < 2 wk of its induction, however, the more typical onset is at 3 or 4 d after initiation of steroid[14,15]. Although, it was also noted that symptoms can occur anytime even after discontinuation of steroid therapy[16]. This case report highlights that the higher dosage of steroid exposure can cause earlier manifestation of psychotic symptoms as observed from the 2 cases related to pituitary adenoma surgery. Also, the dosage was observed to be directly proportional to the severity of psychosis wherein the present patient had florid episodes of agitation when he was maintained on 106.7 mg/d of Prednisone.
In an older study of Lewis and Smith in 1983, most of the cases back then were most commonly presenting with delusions and a few had psychotic disorder without evidence of significant mood changes or features of delirium[10]. On the other hand, most common symptoms for all of the cases in the latest review were delusions and hallucinations however other psychiatric symptoms were also noted such as insomnia, agitation, irritability, combativeness, confusion, cognitive impairment, mania, depression, and even suicidal ideation. Both cases related to pituitary adenoma had similar presentation with that of any typical steroid-induced psychosis in the latest review however there were no noted combativeness, mania, depression, and suicidal ideation among them.
In the latest review, discontinuation and/or tapering of the steroid use were the management utilized following the diagnosis of psychosis. It was observed that discontinuation provided quicker resolution of symptoms. However, discontinuation may not be feasible for all medical indications, the benefit should always outweigh the risk in considering to withdraw steroids. As for the two cases of pituitary adenoma surgery, tapering was employed. The case of Mizutani et al[3] had a 7-d period of tapering while in the present patient, he had longer period for 11 d. There are no studies yet about recommended standard period of tapering and no established association if a shorter or longer period of tapering would lead to earlier recovery or improvement.
For the pharmacologic interventions, typical antipsychotics, atypical antipsychotics, mood stabilizers and benzodiazepines were utilized in the latest review. While for both cases of pituitary adenoma surgery, Risperidone, an atypical antipsychotic was utilized. The latest review of cases supports the high effectiveness of Haloperidol and Risperidone in managing adult patients exhibiting delusions or hallucinations after exposure to steroids[4]. However, it has been shown that there is greater preference in using atypical antipsychotics over the typical antipsychotics because of it lower adverse risk profile[15,17].
In the latest review, recovery or improvement was noted earliest by 1 mo and longest by 8 wk. And a great majority of patient completely recover within an average span of 2 wk after treatment initiation[4]. The case of Mizutani et al[3] had earlier recovery while the present patient had later improvement, at 4 d and 3 wk, respectively. This maybe due to the delayed initiation of antipsychotics which did not start at the onset of psychosis and did not overlap with the tapering period of steroid. Aside from that, the steroids given to the present patient was notably excessive when compared to the current suggested guidelines for the perioperative assessment and management of pituitary surgery by Inder et al[12] in 2002.
In the guidelines, no perioperative glucocorticoid cover should be given in patients with a normal hypothalamic-pituitary-adrenal (HPA) axis function and/or those in whom selective adenectomy can be performed. While for patients with abnormal HPA axis function, the preoperative steroid supplementation regimen recommends that a usual daily dose of prednisone is 5 mg/d (equivalent values: methylprednisolone 4 mg/d, dexamethasone 0.5 mg/d, hydrocortisone 20 mg/d) or 10 mg of prednisone every other day should be given followed by the regimen used for extensive pituitary surgery. The recommended hydrocortisone perioperative steroid regimen for extensive pituitary surgery is 50 mg IV every 8 h. On day 0 then taper dose by half per day, 25 mg IV every 8 h. On day 1 and so on until usual daily dose is reached. The present case received Dexamethasone 12 mg as its perioperative steroid dose which is equivalent to Hydrocortisone 320 mg. Hence, the present patient received more than 6 times greater than the recommended perioperative steroid dose by Inder et al[12] predisposing the patient to steroid psychosis. This highlights the importance of proper determination of indication and providing the appropriate minimum dose of steroids in patients undergoing pituitary surgery so as to avoid any perturbing complications.
For patients undergoing pituitary adenoma surgery, the indication for perioperative steroid replacement must be evaluated properly and the minimum dose should be utilized. Early recognition of steroid-induced psychosis would lead to better prognosis. Multispecialty treatment is vital in the holistic management of the patient with timely referral and close coordination.
I would like to express my gratitude to my Supervising Consultant, Dr. Jovy Anne J. Tangalin for guiding me in writing this case report and in handling the case appropriately. I am also grateful for all the staff of the Department of Psychiatry – Baguio General Hospital Medical Center for helping me develop my skills as a psychiatrist and researcher.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Clinical neurology
Country/Territory of origin: Philippines
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Odabasi O, Turkey; Lei T, China S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th Ed. Washington, DC: American Psychiatric Publishing; 2013. [RCA] [DOI] [Full Text] [Cited by in Crossref: 66101] [Cited by in RCA: 58044] [Article Influence: 3627.8] [Reference Citation Analysis (4)] |
| 2. | Sadock BJ, Sadock VA, Ruiz P. Kaplan and Sadock’s Comprehensive Textbook of Psychiatry. 10th ed. Wolters Kluwer, 2017. |
| 3. | Mizutani K, Toda M, Kikuchi R, Uchida H, Yoshida K. Steroid psychosis caused by perioperative steroid replacement for pituitary adenoma: a case report. Keio J Med. 2015;64:11-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Huynh G, Reinert JP. Pharmacological Management of Steroid-Induced Psychosis: A Review of Patient Cases. J Pharm Technol. 2021;37:120-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 5. | Leucht S, Komossa K, Rummel-Kluge C, Corves C, Hunger H, Schmid F, Asenjo Lobos C, Schwarz S, Davis JM. A meta-analysis of head-to-head comparisons of second-generation antipsychotics in the treatment of schizophrenia. Am J Psychiatry. 2009;166:152-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 340] [Cited by in RCA: 326] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 6. | Wada K, Yamada N, Suzuki H, Lee Y, Kuroda S. Recurrent cases of corticosteroid-induced mood disorder: clinical characteristics and treatment. J Clin Psychiatry. 2000;61:261-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Evans RR, Rackemann FM. Allergy; corticotropin and cortisone: a review of the literature from September, 1950, to January, 1952. AMA Arch Intern Med. 1952;90:96-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Goggans FC, Weisberg LJ, Koran LM. Lithium prophylaxis of prednisone psychosis: a case report. J Clin Psychiatry. 1983;44:111-112. [PubMed] |
| 9. | Gabbard GO. Psychodynamic psychiatry in the "decade of the brain". Am J Psychiatry. 1992;149:991-998. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 49] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Lewis DA, Smith RE. Steroid-induced psychiatric syndromes. A report of 14 cases and a review of the literature. J Affect Disord. 1983;5:319-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 369] [Cited by in RCA: 340] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 11. | Boye Nielsen J, Drivsholm A, Fischer F, Brochner-mortensen K. Long-term treatment with corticosteroids in rheumatoid arthritis (over a period of 9 to 12 years). Acta Med Scand. 1963;173:177-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Inder WJ, Hunt PJ. Glucocorticoid replacement in pituitary surgery: guidelines for perioperative assessment and management. J Clin Endocrinol Metab. 2002;87:2745-2750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 92] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 13. | Acute adverse reactions to prednisone in relation to dosage. Clin Pharmacol Ther. 1972;13:694-698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 227] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 14. | Kenna HA, Poon AW, de los Angeles CP, Koran LM. Psychiatric complications of treatment with corticosteroids: review with case report. Psychiatry Clin Neurosci. 2011;65:549-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 177] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 15. | Warrington TP, Bostwick JM. Psychiatric adverse effects of corticosteroids. Mayo Clin Proc. 2006;81:1361-1367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 306] [Cited by in RCA: 332] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 16. | Janes M, Kuster S, Goldson TM, Forjuoh SN. Steroid-induced psychosis. Proc (Bayl Univ Med Cent). 2019;32:614-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 17. | Meltzer HY. Update on typical and atypical antipsychotic drugs. Annu Rev Med. 2013;64:393-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 269] [Cited by in RCA: 298] [Article Influence: 22.9] [Reference Citation Analysis (0)] |