Revised: November 14, 2013
Accepted: December 12, 2013
Published online: February 2, 2014
Actinic lichen planus, a variant of lichen planus usually in people living in the tropics, presents as annular or discoid patches over the sun-exposed regions. We present here a case of actinic lichen planus with papules and plaques over the malar region and dorsum of nose - a rare presentation of this entity.
Core tip: This is an interesting case of a young lady who presented with brown and erythematous papules and plaques. Clinically, no one thought of lichen planus in the differential diagnosis. It exemplifies the fact that a dermatological entity can be so diverse in its presentation and become a mystery for the clinician to diagnose.
- Citation: Ghosh A, Das A, Kumar D, Gharami RC. Actinic lichen planus: a presentation, deviant from the conventional. World J Dermatol 2014; 3(1): 4-5
- URL: https://www.wjgnet.com/2218-6190/full/v3/i1/4.htm
- DOI: https://dx.doi.org/10.5314/wjd.v3.i1.4
Actinic lichen planus is a variant form of lichen planus located on light-exposed areas, occurring in children or young adults (dark skinned individuals) living in tropical countries. The presentation of the entity can be diverse and hereby, we report an interesting presentation.
A middle-aged lady presented to us with asymptomatic multiple red-brown papules and plaques over the face and nose for a duration of 2 years. The course of evolution of the lesion involved a mild burning sensation on sun-exposure 2 years back and 1-2 mo after that, she developed a few papules which gradually increased in number and some of them also coalesced to form small plaques (1.0-2.5 cm) which were erythematous to brownish in color with a history of summer exacerbation (Figure 1). No history of regular drug intake or similar lesions in the past or in the family. Scalp, oral and genital mucosa and nails were absolutely normal. Cosmetic concern prompted her to seek medical treatment. On the basis of the clinical presentation of the patient, we considered syringoma and mucinosis as a differential diagnosis and one of the lesions was subjected to biopsy for confirmation of our diagnosis.
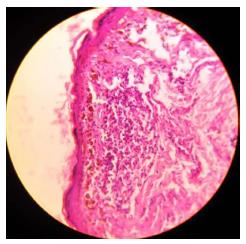
To our utter surprise, on histopathological examination we found epidermal atrophy, basal cell layer degeneration, melanin incontinence and band-like infiltration of lymphocytes at the dermoepidermal junction, which clinched the diagnosis of a variety of actinic lichen planus (Figure 2). Photoprotection and an intramuscular injection of triamcinolone were advised. Marked improvement was seen after a single dose (Figure 3).
Actinic lichen planus, also known as lichen planus subtropicus, lichenoid melanodermatitis and lichen planus atrophicus annularis, mainly affects children and young adults of Middle-East, African or Indian origin. There are 3 clinical types: annular, pigmented and dyschromic[1,2]. There is no sexual predilection and typical lesions are annular or discoid patches on sun exposed regions with a hyperpigmented center and a surrounding hypopigmented zone. Recurrent painful annular erythema on the face and hands in a 52 year old Japanese man have been reported, suggesting varied and atypical presentation of actinic lichen planus[3]. It is treated with acitretin, topical corticosteroids[4] and with cyclosporine[5].
Uncommon morphology is the reason behind our purpose of reporting the case.
A middle-aged lady presented to us with asymptomatic multiple red-brown papules and plaques over the face and nose for a duration of 2 years.
Syringoma and mucinosis.
Syringoma, mucinosis, other deposition disorders, actinic lichen planus.
This is an interesting case that has educative value.
P- Reviewer: Chi CC S- Editor: Wen LL L- Editor: Roemmele A E- Editor: Lu YJ
| 1. | Denguezli M, Nouira R, Jomaa B. [Actinic lichen planus. An anatomoclinical study of 10 Tunisian cases]. Ann Dermatol Venereol. 1994;121:543-546. [PubMed] [Cited in This Article: ] |
| 2. | Bouassida S, Boudaya S, Turki H, Gueriani H, Zahaf A. [Actinic lichen planus: 32 cases]. Ann Dermatol Venereol. 1998;125:408-413. [PubMed] [Cited in This Article: ] |
| 3. | Dekio I, Matsuki S, Furumura M, Morita E, Morita A. Actinic lichen planus in a Japanese man: first case in the East Asian population. Photodermatol Photoimmunol Photomed. 2010;26:333-335. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Jansen T, Gambichler T, von Kobyletzki L, Altmeyer P. Lichen planus actinicus treated with acitretin and topical corticosteroids. J Eur Acad Dermatol Venereol. 2002;16:174-175. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Gallo L, Ayala F, Ayala F. Relapsing lichen actinicus successfully treated with cyclosporin. J Eur Acad Dermatol Venereol. 2008;22:370-371. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |