Published online Sep 27, 2020. doi: 10.5313/wja.v9.i1.7
Peer-review started: April 29, 2020
First decision: July 5, 2020
Revised: July 12, 2020
Accepted: August 16, 2020
Article in press: August 16, 2020
Published online: September 27, 2020
Processing time: 146 Days and 15.8 Hours
Cement-related embolism is a rare but potentially fatal complication in spinal surgery. Cardiac echocardiography can provide valuable information for the early identification.
A 66-year-old woman who underwent lumbar vertebroplasty and internal fixation under general anesthesia experienced an episode of supraventricular tachycardia and ventricular tachycardia at the end of surgery. Point-of-care echocardiogram revealed a foreign body in the right heart. After conservative treatment in the intensive care unit, her family decided on comfort care and she expired.
Transthoracic echocardiography may provide early valuable information in patients undergoing vertebroplasty, and mild-moderate pericardial effusion may be a significant sign of a poor outcome.
Core Tip: With an aging population and increasing tumor occurrence, there is an ever-growing demand for vertebroplasty surgery. Cement related embolism subsequently increases. We recommend echocardiography in the early identification of cement embolism and foreign body with pericardial perfusion should be paid more attention.
- Citation: Xu ZZ, Li HJ, Li X, Zhang H. Cement-related embolism after lumbar vertebroplasty: A case report. World J Anesthesiol 2020; 9(1): 7-11
- URL: https://www.wjgnet.com/2218-6182/full/v9/i1/7.htm
- DOI: https://dx.doi.org/10.5313/wja.v9.i1.7
Cement augmented pedicle screw instrumentation of the thoracolumbar spine is indicated in spinal metastasis to release pain and stabilize the vertebral body. The incidence of cement leakage in multi-level vertebroplasty is more than 65%, and the incidence in single-level vertebroplasty is even higher[1,2]. Cement-related embolism is a rare but potentially fatal complication, with an incidence of 4.6%-7.9%[2,3]. Those with advanced age, metastatic bone disease, osteoporosis, underlying cardiovascular disease, and patent foramen ovale were reported to be at higher risk[4]. Early screening and detection are crucial for these patients, and point-of-care echocardiography can provide valuable information in the clinical setting. Cardiac effusion revealed in echocardiogram examination may be a significant indicator of a poor outcome. Here, we report a case of cement-related pulmonary embolism following vertebroplasty for spinal metastasis.
A 66-year-old woman, complaining of back pain and lower limb weakness for about 2 mo, was referred from the orthopedics clinic to the inpatient department.
The patient underwent radical mastectomy 8 years ago for breast cancer, followed by chemotherapy and endocrine therapy. Six months ago, she was admitted to the emergency room, presenting with proximal femoral fracture. After surgical femoral head replacement, biopsy of the femur suggested metastatic breast adenocarcinoma. The patient had type 2 diabetes mellitus that was controlled by insulin injections for 10 years.
Lumbar magnetic resonance imaging showed that there were occupying lesions at the level of T12 to S3 vertebrae and vertebral pedicle, suggestive of metastases. The patient was diagnosed with breast cancer and multiple bone metastases according to clinical evidence. Laboratory examination results were within normal limits, including hematological, coagulation, kidney, and liver functions as well as electrolytes. Electrocardiogram revealed tachycardia with a heart rate of 110 bpm. Preoperative transthoracic echocardiography (TTE) showed normal contraction function with an ejection fraction of 71% and normal diastolic function with a septal e’ value of 12 cm/s. Chest X-ray did not show any abnormalities. Physical examination revealed normal cardiorespiratory findings, but low back tenderness and lower extremity weakness.
Invasive blood pressure, SpO2, lead II electrocardiogram, end-tidal concentrations of inhalational anesthetics and carbon dioxide, nasopharyngeal temperature, bispectral index, and urine output were monitored during surgery. Intravenous access was obtained using an 18G cannula before induction and a central venous catheter was inserted after the induction of general anesthesia. General anesthesia was induced with sufentanil (targeted controlled infusion at an effect-site concentration of 0.5 ng/mL), 60 mg propofol, 7 mg etomidate, and 50 mg rocuronium. After successful intubation, anesthesia was maintained with inhalation nitrous oxide, propofol (25-30 mL/h) infusion, and sufentanil (targeted controlled infusion at an effect-site concentration of 0.1-0.3 ng/mL) to achieve appropriate depth of anesthesia and pain control. Cis-atracurium was intermittently administered to ensure muscle relaxation. The patient was placed in the prone position and her eyes and nose were protected to avoid bruising. Hemodynamics management was guided by the stroke volume variation and cardiac index. When the surgery was finished, an episode of supraventricular tachycardia and ventricular tachycardia occurred without unstable hemodynamics. A 4-mL bolus of 2% lidocaine was administered intravenously to alleviate the arrhythmia. Arterial blood gas results were within normal limits (K+ 4.8 mmol/L and lactate 1.0 mmol/L). The patient then recovered and was extubated with sinus tachycardia of 110 bpm, intra-arterial blood pressure of 140/90 mmHg, and SpO2 of 95%.
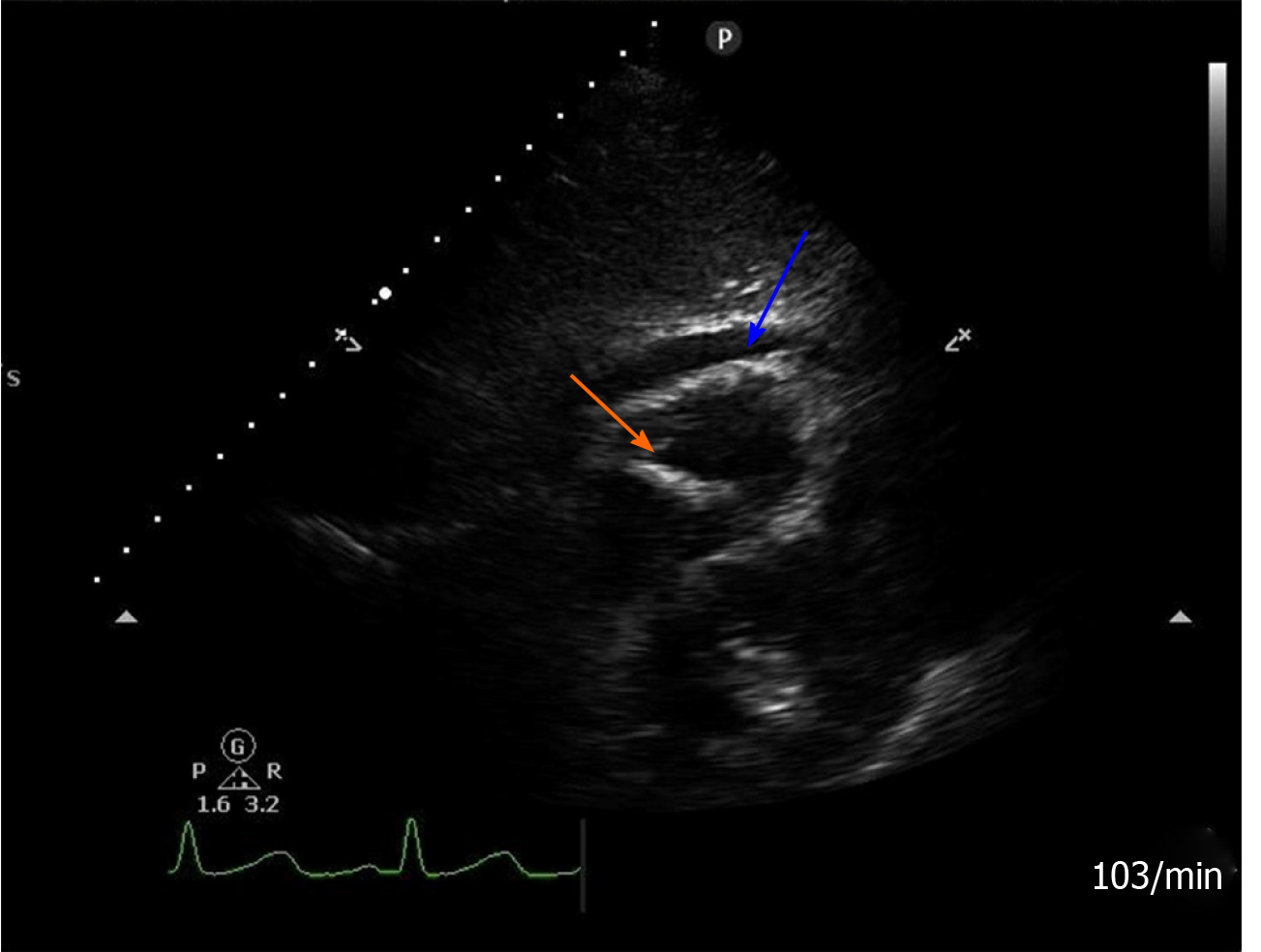
After transferred to the post-anesthesia care unit, TTE was performed by a skillful anesthesiologist. A hyper-echogenic material signal was observed in the right heart, across the tricuspid valve area extending to the right ventricular apex. This sign might indicate a foreign body. Both foreign body and pericardial effusion could be detected on the apical four chamber view, parasternal long axis view, and subxiphoid four chamber view under TTE (Figure 1). With the exception of sinus tachycardia which already existed preoperatively, her general vital signs were within the normal range. We made a preliminary diagnosis of cement-related embolism. Subsequently, coronary angiography confirmed the presence of cement within the right heart and right pulmonary (Figure 2). She was finally diagnosed with cement-related embolism, and received non-invasive ventilation support afterwards.
Due to advanced stage of the tumor and lung embolism and high risk of treatment, her family refused surgical embolectomy and percutaneous emboli removal and decided on comfort care.
The patient experienced dyspnea and progressive heart failure due to cement-related embolism. She eventually expired.
The incidence of vertebroplasty related symptomatic pulmonary cement embolism is reported to be approximately 3% to 23%, according to different imaging methods[5]. Common complications in vertebroplasty include rib fracture, cement leakage, and anaphylactic reaction, with or without hemodynamic turbulence[6]. Although this procedure was strictly monitored using good-quality fluoroscopy for vascular leakage, in our case, cement embolism caused by perivertebral venous migration was not identified early in the operating room. What’s more, real-time detection of lateral-vertebral leakage was difficult due to overlap of the cement filling the vertebral body.
Lack of robust detection of the embolism was due to atypical vital signs in the early stage. The best management of cardiac and pulmonary cement-related embolism in this situation is worthy of debate[7]. Surgical approaches, such as cardiovascular intervention or open cardiac surgery, the best timing for removal of the cement emboli, and patient preference need to be discussed on a multidiscipline basis.
The diagnosis of cardiac cement in our case was determined in the post-anesthesia care unit, and the patient was quickly transferred to the intensive care unit for further treatment. A review of the literatures revealed that conservative treatment may be recommended rather than surgical removal except for extensive obstruction[8]. Moreover, quite a few patients were diagnosed ranging from 10 d to 6 years after surgery due to clinical symptoms[9-12]. As shown in our case, mild-moderate pericardial effusion shortly after surgery may be a significant indicator of a poor outcome. Table 1 summarizes several reported cases with early detection of cement embolism by echocardiography during or shortly after surgery. Most cases requiring surgical treatment were associated with pericardial effusion.
| Ref. | Age/gender | Echocardiography finding/whether pericardial effusion present | Clinical features and occurrence time | Treatment | Outcome |
| Cohen[13],2012 | 65 yr/ female | Foreign body in the right ventricle/with little pericardial effusion | Ventricular tachycardia intraoperatively | Progression to right ventricle failure and surgical removal | Uneventful recovery |
| Tran et al[14], 2013 | 68 yr/ female | Tamponade | Cardiac shock during coronary angiography after lumbar surgery | Percutaneous catheterization removal | Recovery |
| Elapavaluru et al[15], 2015 | 61 yr/ female | Hyper-echo foreign body in the apex of the left ventricle/pericardial effusion not clearly mentioned | Acute hypoxic respiratory failure within 24 h postoperatively | Mitral valve replacement under cardiopulmonary bypass | Discharged home |
| Puri[16], 2016 | 75 yr/ female | Foreign body in right heart/large pericardial effusion | Chest pain, tachycardia, and hypotension the following day | Surgical removal | Discharge with a normal sinus rhythm |
| Andrä et al[7], 2017 | 62 yr/ female | Hyper-echo foreign body in the right atrium/8-mm wide pericardial effusion | Severe tachycardia and hypotonia intraoperatively | Surgical removal | Stable cardiorespiratory condition |
| Adu-Gyamfi et al[17], 2019 | 86 yr/ female | Cement traversing the tricuspid valve into the right ventricle/without pericardial effusion | Shortness of breath immediately after surgery | Medicine treatment | Discharged home |
Transthoracic echocardiogram is an inexpensive and non-invasive examination, and could probably provide valuable information in such patients. This case emphasizes the importance of early detection of cardiac and pulmonary embolism using polymethylmethacrylate during vertebroplasty, especially the identification of pericardial effusion. However, prospective clinical trials on this issue are still limited.
Anesthesiologists should be aware of spinal metastasis and the anatomy of the vertebral venous system, and master the technique of transthoracic echocardiogram to minimize perioperative cardiovascular risks during vertebroplasty. Attention also should be paid to the early detection of pericardial effusion.
Manuscript source: Unsolicited manuscript
Specialty type: Anesthesiology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Quadros LGD, Surani S S-Editor: Zhang L L-Editor: Wang TQ P-Editor: Ma YJ
| 1. | Bao L, Jia P, Li J, Chen H, Dong Y, Feng F, Yang H, Chen M, Tang H. Percutaneous Vertebroplasty Relieves Pain in Cervical Spine Metastases. Pain Res Manag. 2017;2017:3926318. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 2. | Janssen I, Ryang YM, Gempt J, Bette S, Gerhardt J, Kirschke JS, Meyer B. Risk of cement leakage and pulmonary embolism by bone cement-augmented pedicle screw fixation of the thoracolumbar spine. Spine J. 2017;17:837-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 117] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 3. | Choe DH, Marom EM, Ahrar K, Truong MT, Madewell JE. Pulmonary embolism of polymethyl methacrylate during percutaneous vertebroplasty and kyphoplasty. AJR Am J Roentgenol. 2004;183:1097-1102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 235] [Cited by in RCA: 219] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 4. | Osoba O, Kosko B. Noise-enhanced clustering and competitive learning algorithms. Neural Netw. 2013;37:132-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Krueger A, Bliemel C, Zettl R, Ruchholtz S. Management of pulmonary cement embolism after percutaneous vertebroplasty and kyphoplasty: a systematic review of the literature. Eur Spine J. 2009;18:1257-1265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 221] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 6. | Habib N, Maniatis T, Ahmed S, Kilkenny T, Alkaied H, Elsayegh D, Chalhoub M, Harris K. Cement pulmonary embolism after percutaneous vertebroplasty and kyphoplasty: an overview. Heart Lung. 2012;41:509-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 45] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 7. | Andrä M, Baumer H, Mittergradnegger F, Laschitz M, Petek T, Wandschneider W. Life-Threatening Cardiac Perforation After Posterior Spondylodesis. Ann Thorac Surg. 2017;104:e355-e357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Rahimi B, Boroofeh B, Dinparastisaleh R, Nazifi H. Cement pulmonary embolism after percutaneous vertebroplasty in a patient with cushing's syndrome: A case report. Respir Med Case Rep. 2018;25:78-85. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Bouchez S, Mauermann E, Philipsen T, Wouters P. 3D Echocardiographic Diagnosis of Right Ventricular Perforation With Polymethylmethacrylate Particles After Vertebroplasty. J Cardiothorac Vasc Anesth. 2017;31:2123-2126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Schuerer S, Misfeld M, Schuler G, Mangner N. Intracardiac cement embolization in a 65-year-old man four months after multilevel spine fusion. Eur Heart J. 2015;36:783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Cadeddu C, Nocco S, Secci E, Deidda M, Pirisi R, Mercuro G. Echocardiographic accidental finding of asymptomatic cardiac and pulmonary embolism caused by cement leakage after percutaneous vertebroplasty. Eur J Echocardiogr. 2009;10:590-592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Lee JS, Jeong YS, Ahn SG. Intracardiac bone cement embolism. Heart. 2010;96:387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Cohen JB. Bone cement embolism. Anesthesiology. 2012;117:407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Tran I, Gerckens U, Remig J, Zintl G, Textor J. First report of a life-threatening cardiac complication after percutaneous balloon kyphoplasty. Spine (Phila Pa 1976). 2013;38:E316-E318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Elapavaluru S, Alhassan S, Khan F, Khalil R, Schuett A, Bailey S. Severe Acute Traumatic Mitral Regurgitation, Cardiogenic Shock Secondary to Embolized Polymethylmethracrylate Cement Foreign Body After a Percutaneous Vertebroplasty. Ann Thorac Surg. 2016;101:1169-1171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (1)] |
| 16. | Puri V. Invited Commentary. Ann Thorac Surg. 2016;101:1855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Adu-Gyamfi KO, Patri S. Symptomatic cardiopulmonary cement embolism following vertebroplasty. BMJ Case Rep. 2019;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |