Published online Nov 27, 2016. doi: 10.5313/wja.v5.i3.67
Peer-review started: May 12, 2016
First decision: July 11, 2016
Revised: July 27, 2016
Accepted: September 13, 2016
Article in press: September 18, 2016
Published online: November 27, 2016
Processing time: 192 Days and 5.2 Hours
To compare the efficacy of intrathecal morphine and single shot femoral nerve block for patients undergoing primary total knee arthroplasty.
Data was extracted from electronic medical records and case-paper record files of patients who underwent unilateral primary total knee arthroplasty under spinal anesthesia using bupivacaine 12.5 mg with intrathecal morphine (ITM) 0.2 mg and under general anesthesia (GA) with single shot femoral nerve block (FNB) using 20 mL 0.5% bupivacaine at our hospital in 2013 and 2014. All patients had received peri-articular infiltration as per the hospital protocol. Data for gender, age, weight, American Society of Anesthesiologists status, total surgical time, postoperative pain score using visual analogue scale (VAS) from 1 to 10 at 6 h, 12 h and 24 h postoperatively, 24 h opioid consumption, use of oral multimodal analgesia, postoperative high dependency unit (HDU) admission and the time to discharge from the hospital was collected. The data was analyzed using Mann-Whitney U test for continuous variables and Fischer’s exact-t-test for categorical variables.
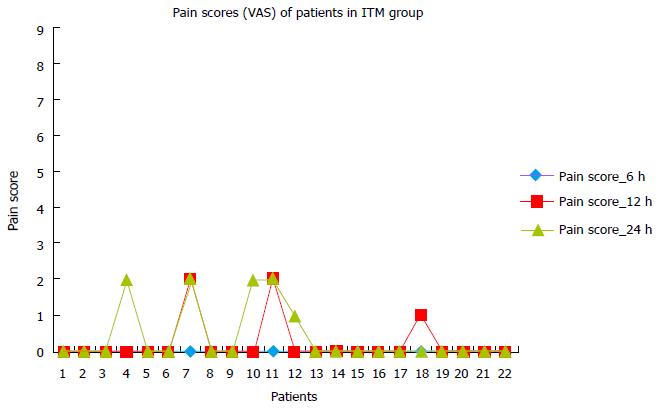
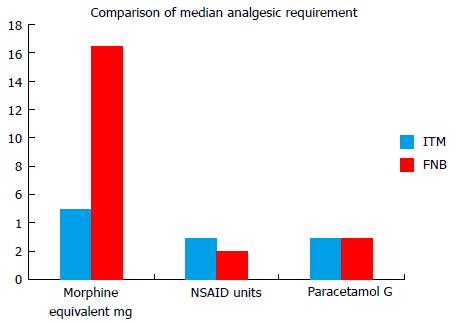
Twenty-two patients in ITM group and 32 patients in FNB group were analyzed. Median pain scores using VAS in ITM group were significantly lower at 6 h (0.0 vs 2.0, P < 0.001), 12 h (0.0 vs 2.0, P < 0.001) and 24 h (0.0 vs 2.0, P < 0.001) postoperatively. Also, postoperative morphine consumption in ITM group was significantly lower (P < 0.001). However, median of non-steroid anti-inflammatory drug unit requirement in 24 h postoperatively was statistically significant higher in ITM compared to FNB group (2.0 vs 1.0, P = 0.025). The difference in postoperative paracetamol consumption in 24 h was not statistically significant (P = 0.147). There was no significant difference in the postoperative HDU admission or time to discharge from the hospital. No respiratory depression in either group was noticed.
The ITM group patients had much lower pain scores and morphine requirement in the first 24 hour postoperatively compared to FNB group.
Core tip: In this retrospective analysis, intrathecal morphine (ITM) with spinal anesthesia and single shot femoral nerve block (FNB) with general anesthesia were compared in 54 patients undergoing primary total knee arthroplasty over two years at our institute. Pain scores and morphine consumption in 1st 24 h after surgery were significantly lower in ITM group compared to FNB group (P < 0.001); while complication rates, high dependency unit admission rates, and time to discharge from the hospital were similar in both groups. Also, patients in ITM group were highly satisfied (P < 0.001).
- Citation: DeSousa K, Chandran R. Intrathecal morphine vs femoral nerve block for postoperative-analgesia after total knee arthroplasty: A two-year retrospective analysis. World J Anesthesiol 2016; 5(3): 67-72
- URL: https://www.wjgnet.com/2218-6182/full/v5/i3/67.htm
- DOI: https://dx.doi.org/10.5313/wja.v5.i3.67
Total knee arthroplasty (TKA) leads to considerable post-operative pain, which requires optimal control for early mobilization as per the current trend. Femoral nerve block (FNB) and intrathecal morphine (ITM) are commonly used techniques for postoperative analgesia since the recommendation by PROSPECT group[1] as a part of multimodal technique with non-steroid anti-inflammatory drugs and centrally acting drugs like paracetamol and systemic opioids. To compare the efficacy of these methods, we performed a retrospective analysis of patients who underwent unilateral primary TKA with single shot FNB with general anesthesia (GA) and ITM with spinal anesthesia (SA) in the year 2013 and 2014 at our hospital. Earlier, low dose ITM and ultrasound guided FNB have been compared albeit both groups had received SA[2]. In this study, Frassanito et al[2] 0.1 mg ITM was found to be safe and more efficient compared to single shot FNB using 25 mL 0.75% ropivacaine though the lower pain scores and morphine consumption in ITM group compared to FNB group were not statistically significant.
After permission from the hospital ethics committee, and approval by SingHealth centralized institutional review board, data was extracted from electronic medical records for all patients who underwent unilateral primary TKA in the year 2013 and 2014. Only those patients who underwent primary TKA under SA using bupivacaine 12.5 mg with ITM 0.2 mg and those who underwent primary TKA under GA with FNB using 20 mL 0.5% bupivacaine at our hospital in 2013 and 2014 were included in this analysis. The case-paper record files were also obtained at this stage and looked into.
In the ITM group, 0.2 mg morphine was mixed with bupivacaine while performing SA. Preservative free morphine is supplied in ampoules of 10 mg in 1 mL. The person performing SA diluted preservative free 10 mg morphine with 9 mL of normal saline to obtain 1 mg/mL under aseptic precautions. From this diluted morphine, 0.2 mL was taken using insulin syringe and mixed with 2.5 mL of isobaric 0.5% bupivacaine. Lumber puncture was performed under asepsis using either Quincke or Whitacare spinal needle of 25 G and the mixture of bupivacaine and morphine was injected slowly. Only patients who received this dose of morphine and bupivacaine were included in this analysis for uniformity.
In the FNB group, FNB was performed before the induction of GA and its effectiveness was confirmed by checking loss of sensation on the medial aspect of leg just below the knee before the start of GA. All FNBs were performed using ultrasound guidance and 22 G Stimuplex needle A50 (by B. Braun Medical Inc. - a stimulating non-echogenic single shot 50 mm needle). GA was induced with appropriate dose of propofol, fentanyl and atracurium and airway maintenance was with laryngeal mask airway. GA was maintained with oxygen, sevoflurane and intermittent doses of morphine. Only patients who received 20 mL of 0.5% bupivacaine for FNB were included in this study for uniformity. Patients who received a different dose of bupivacaine or ropivacine were not included. Patients who received continuous FNB, FNB plus sciatic block, SA with FNB or any other combination were not included in this analysis.
All patients in both groups had received intra-operative peri-articular infiltration as per the hospital protocol; a mixture of 20 mL of 0.5% bupivacaine with 30 mg ketorolac, and 5 mg morphine plus 20 mL normal saline. In FNB group, the surgeon carried this out at least 120 min after FNB was performed to avoid local anesthetic toxicity.
Data for gender, age, weight, total surgical time, ASA status, postoperative pain scores using visual analogue scale (VAS) from 1 to 10 on flexion of the operated knee at 6, 12 and 24 h postoperatively, 24 h opioid consumption, use of oral multimodal analgesia, postoperative high dependency unit (HDU) admission and the time to discharge from the hospital was collected.
All patients had received O2 2 lit/min through nasal prongs for the first 12-h after the surgery. Also, we looked for complications such as postoperative nausea and vomiting (PONV), respiratory depression, urinary retention and itching. We defined respiratory depression for this study as respiratory rate < 8/min or SaO2% < 94%.
Postoperatively, all FNB group patients were prescribed patient controlled analgesia (PCA) with morphine while ITM patients were prescribed intravenous tramadol on as required (PRN) basis. For calculations, tramadol 100 mg was considered equivalent to 10 mg morphine[3]. Diclofenac, eterocoxib and celecoxib were used orally on PRN basis in both groups. One unit of non-steroidal anti-inflammatory drugs (NSAIDs) was considered as 50 mg diclofenac or 90 mg eterocoxib or 200 mg celecoxib. Patients in both groups were given paracetamol 1 g on PRN basis.
A backward sample size calculation was done for this retrospective study: With a standard deviation (SD) of 10 mg and clinical relevant difference of 10 mg between ITM and FNB (in a ratio of 1:1.5) for the amount of post-operative morphine consumption, the minimum sample size of 20 patients for ITM and 30 patients for FNB were required for a significance level of 5% and power of 90%.
The data was analyzed using Mann-Whitney U test for continuous variables and Fisher’s Exact test for categorical variables. Patient satisfaction was evaluated from the discharge feedback form.
Ms Carmen Kam Jia Wen, research officer at “Clinical and Trial and Research Unit” (CTRU) at Changi General Hospital, Singapore helped and reviewed this statistical analysis.
There was no statistically significant difference between two groups as far as the gender, weight, ASA status and total surgery time was concerned (P > 0.05). However, median age was significantly older in ITM group than FNB group (69 years vs 61 years, P = 0.002) (Table 1). Patients who received additional blocks or continuous femoral block or combined technique were excluded from the analysis. Twenty two patients in ITM group and 32 patients in FNB group were analyzed.
| ITM (n = 22) | FNB (n = 32) | Statistical significance | |
| Median (IQR) age: Years | 69.0 (62.8-74.3) | 61.0 (57.0-67) | P = 0.002 |
| Sex: Numbers | |||
| Male | 9 (37.5%) | 15 (62.5%) | P = 0.665 |
| Female | 13 (43.3%) | 17 (56.7%) | |
| Median (IQR) weight: Kg | 64.3 (53.2-77.2) | 67.3 (61.2-80.2) | P = 0.275 |
| Median (IQR) ASA status | 3.0 (2.0-3.0) | 2.0 (2.0-3.0) | P = 0.161 |
| Median (IQR) total surgery time in minutes | 117.5 (108.8-135.0) | 107.5 (86.3-128.8) | P = 0.163 |
Median pain scores in ITM group were significantly lower at 6 h (0.0 vs 2.0, P < 0.001), 12 h (0.0 vs 2.0, P < 0.001) and 24 h (0.0 vs 2.0, P < 0.001) postoperatively. Also, median of postoperative morphine consumption in ITM group was significantly lower (P < 0.001). However, median of NSAID (unit) requirement in 24 h postoperatively was statistically significant higher in ITM compared to FNB group (2.0 vs 1.0, P = 0.025). The difference in postoperative paracetamol consumption in 24 h was not statistically significant (P = 0.147).
There was no statistically significant difference in the postoperative HDU admission or time to discharge from the hospital.
All patients in ITM group were prescribed antiemetic at regular time interval and hence did not have any incidence of PONV. While the patients in FNB group were prescribed antiemetic on PRN basis; for this reason the incidence of PONV cannot be compared. There were a number of patients who reported PONV in FNB group: 16 patients at 6 h, 11 patients at 12 h and 9 patients at 24 h. Use of sevoflurane and morphine can also cause PONV. Also, a urinary catheter was electively placed for 24 h for all patients in ITM group and hence urinary retention could not be assessed. The results are presented in the Table 2 and Figures 1-3.
| ITM (n = 22) | FNB (n = 32) | |
| Ease of performance | Very easy, no special training | Expertise and training required, special equipment required |
| Added cost | Only morphine | Ultrasound machine, special needle and local anesthetic |
| Median (IQR) pain score at: | Low | High |
| 6 h | 0.0 (0.0-0.0) | 2.0 (2.0-4.8) |
| 12 h | 0.0 (0.0-0.0) | 2.0 (2.0-3.8) |
| 24 h | 0.0 (0.0-0.3) | 2.0 (2.0-4.0) |
| Median (IQR) of morphine requirement (in mg) in 24 h | Low 5.0 (3.8-10.0) | High 16.5 (8.0-21.5) |
| Median (IQR) of NSAID unit in 24 h | 2.0 (1.0-2.0) | 1.0 (0.0-1.3) |
| Median (IQR) of Paracetamol (G) in 24 h | 3.0 (2.0-3.0) | 3.0 (2.0-4.0) |
| Complications | Low | Low |
| No PONV since antiemetic prescribed in anticipation | Incidence of PONV was higher since no regular antiemetic given (16 at 6 h, 11 at 12 h and 9 at 24 h) | |
| No urinary retention since all patients were catheterized | No urine retention | |
| No respiratory depression | No respiratory depression | |
| No itching recorded | No itching recorded | |
| Number of elective HDU admission status | 3 (15%) | 2 (6.5%) |
| Median (IQR) days to discharge | 4.5 (3.0-5.0) | 4.0 (3.0-6.0) |
| Patient satisfaction | 18/20 (90.0%) rated good | 4/31 (12.9%) rated good |
In this two-year retrospective analysis, patients who received 0.2 mg ITM had much lower pain scores and lower morphine requirement in the first 24 hour postoperatively compared to patients who received FNB using 20 mL of 0.5% bupivacaine.
The pain scores using VAS are recorded by our acute pain service nurses every 6 h for the first 24 hour postoperatively when ITM is given or single shot peripheral or neuraxial blocks are given. Only when the catheters are placed for peripheral or neuraxial blocks or PCA pumps are attached, the acute pain service nurses would evaluate these patients for pain beyond 24 h till the catheters or PCA pumps are removed. For this reason we could not analyze the data for pain beyond 24 h postoperatively.
TKA causes a lot of pain postoperatively. Current trend amongst most surgeons is to mobilize the patients early and discharge from the hospital as early as possible. Hence good pain control in immediate postoperative period is imperative for early mobilization and full flexion recovery.
ITM provides excellent post-operative analgesia and with low dosage it gives segmental analgesia, resulting in localized nociception without motor, sensory or autonomic side effects[4]. Late last century very large dose up to 4 mg ITM was used while today the dose ranges from 0.1-0.5 mg, depending on the type of surgery[5]. In one meta-analysis, it was shown that the use of ITM at dose < 0.3 mg, the rate of episodes of respiratory depression was not higher compared to the placebo group who received systemic opioids[6]. In our analysis where 0.2 mg ITM was used, no respiratory depression was recorded. Other undesirable side effects of ITM are itching, urinary retention and PONV. All patients who had received ITM in our analyses had indwelling urinary catheter for the first 24 h. Also they received round the clock prophylactic antiemetic and hence no patient suffered from PONV.
Regional and peripheral nerve blocks are promising inclusions in multimodal analgesia techniques. According to one study, femoral nerve block is still the gold standard for an effective analgesia approach in knee arthroplasty and should be supplemented (if needed) by oral opioids[7]. Femoral nerve block is frequently used as a part of multimodal technique for postoperative analgesia after TKA all over the world. In a meta-analysis by Paul et al[8], single shot FNB or continuous FNB plus patient controlled analgesia (PCA) was found to be superior to PCA alone for postoperative analgesia for patients having TKA. The impact of adding a continuous FNB to a single shot FNB was not found to be superior and further investigations were suggested by the authors. The use of single shot FNB was frequent at our hospital in 2013 and 2014. Also, single shot FNB can have analgesic effect from 12 to 24 h[9,10] and may extend up to 48 h[11]. Similarly analgesic effect of ITM also lasts for around 24 h and hence it is only fair to compare ITM and single shot FNB for their efficacy for postoperative analgesia.
In a meta-analysis by PROSPECT working group[1], for joint replacement surgery GA combined with an FNB for surgery and postoperative analgesia, or SA with local anesthetic plus ITM is recommended. The group also recommends cooling and compression techniques, paracetamol and conventional NSAIDs or COX-2-selective inhibitors, plus intravenous strong opioids (high-intensity pain) or weak opioids (moderate- to low-intensity pain) for postoperative analgesia. At our institute we follow these recommendations. In addition, the surgical team also prefers to use local infiltration technique as described earlier.
FNB requires the use of ultrasound machine and a special needle, which add to the cost. Also, an expertise in performing the FNB is necessary for good outcome. Additional time to perform and to evaluate the block is also required. In addition, there is a possibility of motor weakness which can increase the risk of postoperative fall. ITM is very cost effective, time saving and a relatively simple technique. Having these considerations on our mind we decided to analyze the outcome for these two techniques and found that ITM group had lower pain scores in the first 24 hour after surgery though the number of patients that we could include was small.
We found three more clinical trials in the literature comparing ITM and FNB for primary unilateral TKA but in all three trials both groups had received SA. In the study published by Frassanito et al[2], where SA was used for both ITM and FNB group, the 24 h and 48 h morphine consumption was lower in ITM group though not statistically significant. In this prospective study, a very low dose of ITM of 0.1 mg was used. In another trial by Sites et al[12] there was no statistically significant difference in the morphine consumption or pain scores between ITM and FNB group where SA was used for both groups. This trial reports more adverse effects in ITM group compared to FNB group but a slightly higher dose of ITM 0.25 mg was used. Tarkkila et al[13] compared ITM with continuous 3 in 1 femoral block in primary unilateral TKA patients and reported lower pain scores in ITM group. Our study involved use of 0.2 mg ITM with statistically significant lower pain scores and morphine consumption without any respiratory depression. Perhaps a large prospective trial with standardized drug regime and multivariate analysis may be needed to prove superiority of ITM over FNB in this particular group of surgical patients.
From our analysis we conclude that 0.2 mg ITM with SA is more effective for first 24 hour postoperatively compared to single shot FNB with GA for primary unilateral TKA. Also, 0.2 mg ITM is safe, time saving and cost effective with better patient satisfaction compared to FNB.
We thank Ms Carmen Kam Jia Wen, research officer at “Clinical and Trial and Research Unit” (CTRU) at Changi General Hospital, Singapore for her statistical help.
Total knee arthroplasty (TKA) leads to considerable post-operative pain, which requires optimal control for early mobilization. Till date, varieties of techniques and drugs have been used to achieve this optimal pain control. Use of intrathecal morphine (ITM) with spinal anesthesia (SA) is extremely easy and can be time saving and cost effective. Also, femoral nerve block (FNB) is one of the easiest peripheral nerve blocks. In this study the authors have compared these two easy techniques for postoperative pain management after TKA.
Regional blocks are commonly used for pain management after TKA. Most recent studies are comparing femoral nerve blocks with adductor canal block and local infiltration techniques. This study compares use of ITM with SA and FNB with GA. In the past only three other studies have compared ITM and FNB, albeit both groups had undergone surgery under SA.
In this study, 0.2 mg ITM with SA was more effective for first 24 hour postoperatively compared to single shot FNB with GA for primary unilateral TKA. In one previous study, which compared 0.1 mg ITM with SA and FNB with SA, pain scores and postoperative opioid consumption were lower in ITM group though statistically not significant. In another similar study, ITM group had more complications when a higher dose of 0.25 mg ITM was used. In their study using 0.2 mg ITM, lower pain scores and opioid consumption were statistically significant. This study also illustrates that use of adequate prophylaxis can prevent known complications of ITM.
This retrospective analysis shows that 0.2 mg ITM with SA is more effective for first 24 h postoperatively compared to single shot FNB with GA for primary unilateral TKA. Perhaps a prospective trial with standardized drug regime and multivariate analysis in a large group of patients is required to prove their findings.
ITM: Intrathecal morphine; FNB: Femoral nerve block; SA: Spinal anesthesia; GA: General anesthesia; PONV: Postoperative nausea and vomiting; PCA: Patient controlled analgesia; NSAIDs: Non-steroidal anti-inflammatory drugs; VAS: Visual analogue scale.
This retrospective analysis is worthy of publishing as it provides value clinical information for how pre-emptive analgesia could effectively prevent or mitigate postoperative pain.
Manuscript source: Invited manuscript
Specialty type: Anesthesiology
Country of origin: Singapore
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Chen CC, Ma SXL, Rikalainen-Salmi R S- Editor: Qiu S L- Editor: A E- Editor: Wu HL
| 1. | Fischer HB, Simanski CJ, Sharp C, Bonnet F, Camu F, Neugebauer EA, Rawal N, Joshi GP, Schug SA, Kehlet H. A procedure-specific systematic review and consensus recommendations for postoperative analgesia following total knee arthroplasty. Anaesthesia. 2008;63:1105-1123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 204] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 2. | Frassanito L, Vergari A, Zanghi F, Messina A, Bitondo M, Antonelli M. Post-operative analgesia following total knee arthroplasty: comparison of low-dose intrathecal morphine and single-shot ultrasound-guided femoral nerve block: a randomized, single blinded, controlled study. Eur Rev Med Pharmacol Sci. 2010;14:589-596. [PubMed] |
| 3. | Vergnion M, Degesves S, Garcet L, Magotteaux V. Tramadol, an alternative to morphine for treating posttraumatic pain in the prehospital situation. Anesth Analg. 2001;92:1543-1546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 39] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | DeSousa K, Chandran R. Intrathecal Morphine for postoperative analgesia: Current trends. World J Anesthesiol. 2014;27:191-202. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 27] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (13)] |
| 5. | Mugabure Bujedo B. A clinical approach to neuraxial morphine for the treatment of postoperative pain. Pain Res Treat. 2012;2012:612145. [PubMed] |
| 6. | Gehling M, Tryba M. Risks and side-effects of intrathecal morphine combined with spinal anaesthesia: a meta-analysis. Anaesthesia. 2009;64:643-651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 185] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 7. | Bauer MC, Pogatzki-Zahn EM, Zahn PK. Regional analgesia techniques for total knee replacement. Curr Opin Anaesthesiol. 2014;27:501-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 67] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 8. | Paul JE, Arya A, Hurlburt L, Cheng J, Thabane L, Tidy A, Murthy Y. Femoral nerve block improves analgesia outcomes after total knee arthroplasty: a meta-analysis of randomized controlled trials. Anesthesiology. 2010;113:1144-1162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 356] [Cited by in RCA: 302] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 9. | Allen HW, Liu SS, Ware PD, Nairn CS, Owens BD. Peripheral nerve blocks improve analgesia after total knee replacement surgery. Anesth Analg. 1998;87:93-97. [PubMed] |
| 10. | Szczukowski MJ, Hines JA, Snell JA, Sisca TS. Femoral nerve block for total knee arthroplasty patients: a method to control postoperative pain. J Arthroplasty. 2004;19:720-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 54] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 11. | Ng HP, Cheong KF, Lim A, Lim J, Puhaindran ME. Intraoperative single-shot “3-in-1” femoral nerve block with ropivacaine 0.25%, ropivacaine 0.5% or bupivacaine 0.25% provides comparable 48-hr analgesia after unilateral total knee replacement. Can J Anaesth. 2001;48:1102-1108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 47] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Sites BD, Beach M, Gallagher JD, Jarrett RA, Sparks MB, Lundberg CJ. A single injection ultrasound-assisted femoral nerve block provides side effect-sparing analgesia when compared with intrathecal morphine in patients undergoing total knee arthroplasty. Anesth Analg. 2004;99:1539-1543; table of contents. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 46] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 13. | Tarkkila P, Tuominen M, Huhtala J, Lindgren L. Comparison of intrathecal morphine and continuous femoral 3-in-1 block for pain after major knee surgery under spinal anaesthesia. Eur J Anaesthesiol. 1998;15:6-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 19] [Article Influence: 0.7] [Reference Citation Analysis (0)] |