Published online Mar 27, 2014. doi: 10.5313/wja.v3.i1.124
Revised: September 4, 2013
Accepted: January 6, 2014
Published online: March 27, 2014
Processing time: 270 Days and 13.6 Hours
AIM: To investigate extravascular lung water indexed to predicted body weight (EVLWIp) and actual body weight (EVLWIa) on outcome of patients with severe sepsis.
METHODS: Transpulmonary thermodilution was prospectively used to measure cardiovascular hemodynamics, EVLWIp and EVLWIa via an arterial catheter placed in each patient within 48 h of meeting the criteria for severe sepsis from a medical intensive care unit (ICU) at a university affiliated hospital. Survival was the single dependent variable. In order to examine and compare the predictive power of EVLWIp, EVLWIa and other clinically significant factors in predicting the in-hospital survival status of severe sepsis patients in the medical ICU, a receiver operating characteristic (ROC) curve method to analyze the significant variables and the area under the ROC curve (AUC) of the variables, P value and 95%CI were calculated.
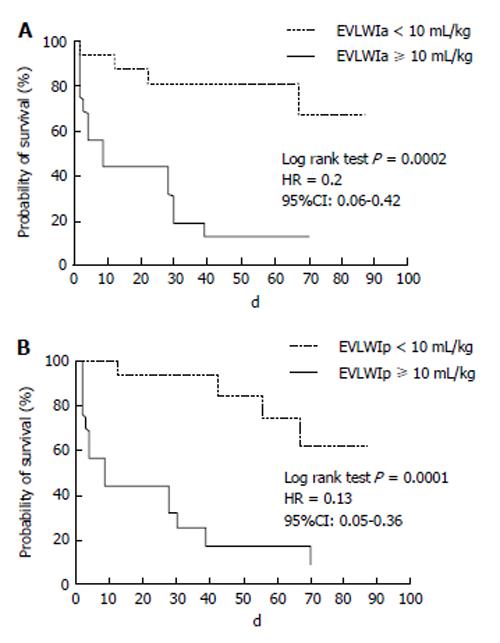
RESULTS: In total, 33 patients were studied. In the ROC curve method analyses, EVLWIp (the AUC: 0.849; P = 0.001, 95%CI: 0.72-0.98) was as predictive for in-hospital survival rate as variables with EVLWIa (AUC, 0.829; P = 0.001, 95%CI: 0.68-0.98). The proportion of patients surviving with a low EVLW (EVLWI < 10 mL/kg) was better than that of patients with a higher EVLW, whether indexed by actual (HR = 0.2; P = 0.0002, 95%CI: 0.06-0.42) or predicted body weight (HR = 0.13; P < 0.0001, 95%CI: 0.05-0.35) during their hospital stay with the Kaplan-Meier method (76% vs 12.5%, respectively).
CONCLUSION: This investigation proposed that EVLWIp is as good a predictor as EVLWIa to predict in-hospital survival rate among severe sepsis patients in the medical ICU.
Core tip: Our study provides the important finding that extravascular lung water index (EVLWI) indexed by predicted body weight is as good as it indexed by actual body weight for for in-hospital survival in patients with severe sepsis. Clinicians could monitor EVLWI indexed by predicted or actual body weight in patients with severe sepsis.
- Citation: Chung FT, Lin SM, Lin HC, Yu CT, Hsieh MH, Fang YF, Liu CY, Kuo CH, Wang TY. Predictive value of extravascular lung water indexed to predicted body weight. World J Anesthesiol 2014; 3(1): 124-128
- URL: https://www.wjgnet.com/2218-6182/full/v3/i1/124.htm
- DOI: https://dx.doi.org/10.5313/wja.v3.i1.124
Transpulmonary thermodilution to assess extravascular lung water (EVLW) at the bedside by a pulse-induced contour cardiac output (PiCCO) system, a comparatively less invasive method than the traditionally used pulmonary arterial catheter, has been popular to monitor the hemodynamic status of patients in critical care units[1]. Measuring EVLW is useful to predict outcome, to diagnose pulmonary edema, to better characterize patients with acute respiratory distress syndrome (ARDS), to guide fluid therapy and to assess the value of new treatments or ventilator setting strategies in septic patients with ARDS[2].
Previously, one study reported the prognostic value of EVLW indexed to actual body weight (EVLWIa) in critically ill patients[3]. However, another study reported that EVLW indexed to predicted body weight (EVLWIp) may improve correlation with severity and survival in sepsis with ARDS. This is because lung size correlates better with height and gender than that of actual body weight[4]. On the other hand, Drs. Meyer and Hall thought that the transpulmonary thermodilution technique used to calculate EVLWIp in theory may be inaccurate in cases of high dead space fraction, which may impair equilibration of cold saline across a portion of the extravascular space[5].
We have reported that EVLW indexed to actual body weight is an independent predictor for in-hospital survival in medical intensive care unit (ICU) patients with severe sepsis[6]. We conducted this study to compare the predicted value of EVLWIp and EVLWIa on in-hospital survival rates of medical ICU patients with severe sepsis.
The population being investigated was recruited from patients admitted to a medical ICU of a university affiliated medical center from 2005 to 2006. The institutional review board approved this study and informed consent was obtained from all of the patients or their surrogates. All enrolled patients were recruited consecutively. Patients were followed-up until death or discharge post enrollment. Patients younger than 18 years old, pregnant or with a terminal malignancy were excluded.
All eligible patients were enrolled within 48 h of meeting the criteria for severe sepsis. Severe sepsis was defined by the consensus committee of the American College of Chest Physicians and Society of Critical Care Medicine[7]. Patient-specific data were obtained upon enrollment, including demographic data, past medical history, source of sepsis and Acute Physiology and Chronic Health Evaluation (APACHE) II score. The physiological parameters, including the presence of shock status, and the hemodynamic parameters were assessed on patient enrollment. Shock was defined as systolic blood pressure < 90 mmHg or mean arterial pressure < 60 mmHg. Patient management decisions, including the type and amount of volume resuscitation, were based on the discretion of the primary intensive care physician[8].
The laboratory serological data (albumin, white blood cell counts and platelets) and oxygenation parameters [PaO2/FiO2 ratio, lung injury score (LIS) and chest X-ray (CXR) score (the number of quadrants with > 50% involvement in the alveolar filling process)] were recorded simultaneously as EVLW was made available by the PiCCO system. Additional patient records, such as ventilator settings and shock management during ICU admission, were also available.
The EVLW measurement was based on the transpulmonary thermodilution method. This method was recently introduced as part of the PiCCO plus system (Pulsion Medical System, Munich, Germany). This method only used a single indicator (cold saline solution). Following central venous injection of 10 mL iced 0.9% saline solution, continuous cardiac output (CO) and EVLW measurements were obtained. CO and EVLW determinations were performed immediately following catheter insertion and were employed as the hemodynamic parameters for managing the patients in the medical ICU with severe sepsis.
To facilitate comparing the EVLWIp and actual body weight, these indices are described by the following terms: EVLIp refers to EVLW indexed to predicted body weight and EVLIa refers to EVLW indexed to actual body weight. ARDS was considered to be present when the American-European Consensus Conference (AECC) criteria[9] were met during medical intensive care unit hospitalization after monitoring with the PiCCO system.
Survival was the single dependent variable. In order to examine and compare the predictive power of EVLWIp, EVLWIa and other clinically significant factors in predicting the in-hospital survival status of severe sepsis patients in the medical ICU, a receiver operating characteristic (ROC) curve method to analyze the significant variables and the area under the ROC curve (AUC) of the variables, P value and 95%CI were calculated. Patients were also divided into 2 subgroups according to their optimal cutoff values of EVLW obtained by the ROC curve method. Survival days and rate were compared with these subgroups with different EVLW. Kaplan-Meier curves for cumulative survival during the hospitalization observation period were constructed and compared with the use of the log-rank test. All analyses were conducted using SPSS software (version 10.0, SPSS, Chicago, IL, United States) and Prism 4 for Windows (version 4.03, Graphpad Software Inc., San Diego, CA, United States).
This study enrolled thirty-three patients with severe sepsis. Table 1 lists the demographic and underlying diseases. The sources of sepsis included pneumonia (n = 24), empyema (n = 1), primary blood stream infection (n = 3), pressure sore infection (n = 2) and urosepsis (n = 3). The incidence of ARDS was 33.3% (11/33), according to the AECC definition. The overall 28 d mortality was 51.5% (17/33). Upon enrollment, Table 1 lists physiological characteristics, EVLWI, global end-diastolic volume index, systemic vascular resistance index, PaO2/FiO2 ratio, LIS and the mean CXR score. Fluid balance (net intake/output) was consistently positive, with a cumulative mean of 2286 ± 1165 mL at 24 h before the EVLW measurement.
| Characteristics | Value |
| Patients (n) | 33 |
| Baseline characteristics | |
| Age (yr) | 65.67 ± 15.49 |
| Male | 69.7% |
| APACHE II score | 24.39 ± 7.921 |
| BMI (kg/m²) | 22.30 ± 5.679 |
| Pneumonia | 72.73% |
| Empyema | 3.03% |
| Primary bloodstream infection | 9.09% |
| Pressure sore infection | 6.06% |
| Urosepsis | 9.09% |
| ARDS | 33.30% |
| Physiology at enrollment | |
| Prior 24 h I/O balance (mL) | 2286 ± 1165 |
| Shock (vasopressor requirement) | 84.85% |
| EVLWI (mL/kg) | 16.64 ± 11.93 |
| Oxygenation | |
| PaO2/FiO2 ratio | 173.4 ± 87.09 |
| CXR score | 2.24 ± 1.30 |
| Lung injury score | 2.04 ± 0.86 |
| Laboratory data | |
| Albumin (g/L) | 0.021 ± 0.007 |
| Platelet (109/L) | 170.03 ± 135.47 |
| WBC (109/L) | 15.91 ± 9.24 |
In the ROC curve method analysis, the AUC of EVLWIp (0.849) was similar to the AUC of EVLWIa (0.829), but larger than that of the APACH II score (0.721), LIS (0.706) and CXR score (0.708) in Table 2.
| Variable (s) | Area under curve | P value | 95%CI |
| EVLWIp | 0.849 | 0.001 | 0.72-0.98 |
| EVLWIa | 0.829 | 0.001 | 0.68-0.98 |
| APACHE II score | 0.721 | 0.03 | 0.54-0.90 |
| LIS | 0.706 | 0.04 | 0.52-0.89 |
| CXR score | 0.708 | 0.04 | 0.53-0.89 |
The proportion of patients surviving with a low (< 10 mL/kg, 17 patients) and a high (≥ 10 mL/kg) EVLWIa were traced during their hospital stay with the Kaplan-Meier method (76% vs 12.5%, respectively; log-rank test, HR = 0.2; P = 0.0002, 95%CI: 0.06-0.42) (Figure 1A). The Kaplan-Meier overall survival estimate was also significantly higher for patients with a low EVLWIp (< 10 mL/kg, 17 patients) than for patients with a low EVLWIp (≥ 10 mL/kg) (76% vs 12.5%, respectively; log-rank test, hazard ratio, 0.13; P < 0.0001, 95%CI: 0.05-0.35) (Figure 1B).
As previous studies have reported, EVLWIp may predict mortality in sepsis with ARDS[4]. Our study revealed similar results in that EVLW indexed to actual body weight was a predictor factor of ICU mortality in patients with septic shock; meanwhile, indexing EVLW to predicted body weight did not enhance its discriminatory power as a predictor indicator of mortality.
Although Drs. Meyer et al[5] thought that the transpulmonary thermodilution technique used to calculate EVLWIp in theory may be inaccurate in cases of high dead space fraction, which may impair equilibration of cold saline across a portion of the extravascular space, they agreed with the Dr. Phillips study that an average EVLWIp 16 mL/kg predicted death in sepsis patients with ARDS who had been intubated for 3.5 d.
Our data support the results previously described by Mallat et al[10] who studied 55 patients with septic shock. In that study, EVLW indexing to actual body weight or predicted body weight is an independent predictor of ICU mortality. In our study, ROC curves showed that both EVLWIa and EVLWIp were good discriminators to distinguish between survivors and nonsurvivors. Sakka et al[3] have shown that EVLW indexed to actual body weight predicted mortality in septic shock patients admitted to the ICU and the measurement of EVLW was done using a thermal-dye dilution method. Nevertheless, since this period, the management of septic shock has changed considerably and the results may be influenced by that study. By demonstrating that EVLWa is an independent prognostic factor, we proposed that EVLWa measurements should be performed in patients with septic shock and poor outcome should be considered when EVLWa values are elevated to more than 10 mL/kg. A similar result was seen in EVLWp to predict the outcome of these septic patients. However, further studies are required to assess the effects of EVLW indexed by actual or predicted body weight and the outcome among these patients.
Usually, EVLW measurement has been indexed to actual body weight. However, lung volume was usually determined by height and sex[11]. Someone reported that EVLW when indexed to predicted body weight was a better prognostic factor of mortality than EVLW indexed to actual body weight in patients with ALI/ARDS[4,12]. In contrast with these findings, we found that indexing EVLW to predicted or actual body weight was not more precise to differentiate between survivors and nonsurvivors. Therefore, in that study, the outcome between EVLWa and EVLWp might probably have been linked to the baseline characteristics between the survivors and nonsurvivors.
In fact, our study supports that both EVLWIa and EVLWIp are better predictors than other independent variables, including APACHE II score, LIS and CXR score, to predict in-hospital survival rate in medical ICU patients with severe sepsis. However, further studies are warranted to investigate the effects of correcting EVLWIp and EVLWIa and the clinical outcome among these patients. Also, validation of the EVLWIp to gravimetric lung water may be conducted in animal models to compare it to EVLWIa.
There are some limitations in the current study. Firstly, Frederic Michard reported that the limitations of dilution methods may lead to an underestimation of EVLW in large pulmonary vascular obstruction, focal lung injury and lung resection, but dilution methods remain an easy and clinically acceptable estimation of EVLW in most critically ill patients, including those with ARDS[2]. Secondly, our study is limited by a modest sample size. Nevertheless, we have demonstrated the ability of EVLW indexes to predict ICU outcome in septic shock patients. In addition, there has been previous discussion regarding the potential limitations associated with the single indicator transpulmonary thermodilution technique[13].
In conclusion, this study demonstrated that severe sepsis patients with elevated EVLW were more vulnerable to mortality, whether indexed to predicted or actual body weight. EVLWIp may provide predictive value to in-hospital survival in patients with severe sepsis as good as EVLWIa. However, further studies are needed to determine whether correcting elevated EVLWIp or EVLWIa would affect clinical outcomes in patients with severe sepsis.
We thank Dr. Shinn-Yn Lin, a statistician who studied in the Institute of Preventive Medicine, College of Public Health, National Taiwan University, for providing the recommendations of statistical analyses and manuscript revision.
Transpulmonary thermodilution to asses extravascular lung water (EVLW) at the bedside by pulse-induced contour cardiac output system, which is comparatively a less invasive method than the traditionally used pulmonary arterial catheter has been popular to monitor the hemodynamic status of patients in the critical care units.
Their study revealed similar result that EVLW indexed to actual body weight was a predictor factor of intensive care unit (ICU) mortality in patients with septic shock, meanwhile, indexing EVLW to predicted body weight did not enhance its discriminatory power as a predictor indicator of mortality.
This investigation proposed that EVLW indexed to predicted body weight (EVLWIp) is a good predictor as EVLW indexed to actual body weight to predict in-hospital survival rate among severe sepsis patients in the medical ICU.
This study assesses the prognostic value of EVLW in medical ICU patients with severe sepsis. The authors conclude that EVLWIp is a better predictor of survival than other indices.
P- Reviewers: Boros M, Ikuta S, Juneja D, Mitaka C S- Editor: Gou SX L- Editor: Roemmele A E- Editor: Liu SQ
| 1. | Cottis R, Magee N, Higgins DJ. Haemodynamic monitoring with pulse-induced contour cardiac output (PiCCO) in critical care. Intensive Crit Care Nurs. 2003;19:301-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 35] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 2. | Michard F. Bedside assessment of extravascular lung water by dilution methods: temptations and pitfalls. Crit Care Med. 2007;35:1186-1192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 103] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 3. | Sakka SG, Klein M, Reinhart K, Meier-Hellmann A. Prognostic value of extravascular lung water in critically ill patients. Chest. 2002;122:2080-2086. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 294] [Cited by in RCA: 262] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 4. | Phillips CR, Chesnutt MS, Smith SM. Extravascular lung water in sepsis-associated acute respiratory distress syndrome: indexing with predicted body weight improves correlation with severity of illness and survival. Crit Care Med. 2008;36:69-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 125] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 5. | Meyer NJ, Hall JB. Sizing up (or down) extravascular lung water as a predictor of outcome in acute lung injury/acute respiratory distress syndrome. Crit Care Med. 2008;36:337-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Chung FT, Lin SM, Lin SY, Lin HC. Impact of extravascular lung water index on outcomes of severe sepsis patients in a medical intensive care unit. Respir Med. 2008;102:956-961. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 39] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Bone RC, Sibbald WJ, Sprung CL. The ACCP-SCCM consensus conference on sepsis and organ failure. Chest. 1992;101:1481-1483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 498] [Cited by in RCA: 509] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 8. | Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J, Gea-Banacloche J, Keh D, Marshall JC, Parker MM. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. 2004;32:858-873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2171] [Cited by in RCA: 2051] [Article Influence: 97.7] [Reference Citation Analysis (0)] |
| 9. | Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994;149:818-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4145] [Cited by in RCA: 4153] [Article Influence: 134.0] [Reference Citation Analysis (0)] |
| 10. | Mallat J, Pepy F, Lemyze M, Barrailler S, Gasan G, Tronchon L, Thevenin D. Extravascular lung water indexed or not to predicted body weight is a predictor of mortality in septic shock patients. J Crit Care. 2012;27:376-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 11. | Crapo RO, Morris AH, Gardner RM. Reference spirometric values using techniques and equipment that meet ATS recommendations. Am Rev Respir Dis. 1981;123:659-664. [PubMed] |
| 12. | Craig TR, Duffy MJ, Shyamsundar M, McDowell C, McLaughlin B, Elborn JS, McAuley DF. Extravascular lung water indexed to predicted body weight is a novel predictor of intensive care unit mortality in patients with acute lung injury. Crit Care Med. 2010;38:114-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 104] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 13. | Kuzkov VV, Kirov MY, Sovershaev MA, Kuklin VN, Suborov EV, Waerhaug K, Bjertnaes LJ. Extravascular lung water determined with single transpulmonary thermodilution correlates with the severity of sepsis-induced acute lung injury. Crit Care Med. 2006;34:1647-1653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 106] [Article Influence: 5.6] [Reference Citation Analysis (0)] |