Published online Mar 11, 2024. doi: 10.5313/wja.v13.i1.90514
Peer-review started: December 9, 2023
First decision: December 23, 2023
Revised: January 5, 2024
Accepted: February 25, 2024
Article in press: February 25, 2024
Published online: March 11, 2024
Processing time: 89 Days and 18.1 Hours
Osteonecrosis or avascular necrosis (AVN) of the hip was one of the dreaded complications of coronavirus disease 2019 (COVID-19), which emerged in patients who received steroid therapy. Corticosteroids have been a mainstay in the treatment protocol of COVID-19 patients. Popular corticosteroid drugs used in patients suffering from COVID-19 were intravenous (IV) or oral dexamethasone, methylprednisolone or hydrocortisone. The use of such high doses of corticosteroids has shown very positive results and has been lifesaving in many cases. Still, long-term consequences were drug-induced diabetes, osteoporosis, Cushing syndrome, muscle wasting, peripheral fat mobilization, AVN, hirsutism, sleep disturbances and poor wound healing. A significant number of young patients were admitted for bilateral total hip replacements (THR) secondary to AVN following steroid use for COVID-19 treatment.
To assess the efficacy of bilateral pericapsular end nerve group (PENG) blocks in patients posted for bilateral THR post-steroid therapy after COVID-19 infection and assess the time taken to first ambulate after surgery.
This prospective observational study was conducted between January 2023 and August 2023 at Care Hospitals, Hyderabad, India. Twenty young patients 30-35 years of age who underwent bilateral THR were studied after due consent over 8 months. All the patients received spinal anaesthesia for surgery and bilateral PENG blocks for postoperative analgesia.
The duration of surgery was 2.5 h on average. Seventeen out of twenty patients (85%) had a Visual Analog Score (VAS) of less than 2 and did not require any supplementation. One patient was removed from the study, as he required re-exploration. The remaining two patients had a VAS of more than 8 and received IV morphine post-operatively as a rescue analgesic drug. Fifteen out of seventeen patients (88.2%) could be mobilized 12 h after the procedure.
Osteonecrosis or AVN of the hip was one of the dreaded complications of COVID-19, which surfaced in patients who received steroid therapy requiring surgical intervention. Bilateral PENG block is an effective technique to provide post-operative analgesia resulting in early mobilization and enhanced recovery after surgery.
Core Tip: Avascular necrosis (AVN) of the hip was one of the dreaded complications of coronavirus disease 2019 (COVID-19), which emerged in patients who received steroid therapy. Corticosteroids have been a mainstay in the COVID-19 treatment protocol. High doses of corticosteroids have shown positive results and have been lifesaving in many cases. Still, long-term consequences were AVN of the hip, which unfortunately affected young individuals. These patients were posted for bilateral hip replacement surgeries. Our study aimed to study the dynamics of pericapsular end nerve block to provide adequate analgesia to these patients for enhanced postoperative recovery and discharge. While epidural analgesia is the gold standard technique, it has several complications like hypotension, motor blockade and urinary retention.
- Citation: Christopher S, Dutta S, Gopal TVS. Bilateral pericapsular end nerve blocks for steroid-induced avascular necrosis following COVID-19 infection requiring bilateral total hip replacement. World J Anesthesiol 2024; 13(1): 90514
- URL: https://www.wjgnet.com/2218-6182/full/v13/i1/90514.htm
- DOI: https://dx.doi.org/10.5313/wja.v13.i1.90514
Avascular necrosis (AVN) is known by various synonyms such as aseptic necrosis of bone, ischemic bone necrosis, osteonecrosis, and osteochondritis desiccans[1]. It is defined as the cellular death of bone components due to the interruption of blood supply to the bone[1]. Compromised blood supply results in collapse, pain, loss of joint function, long-term joint damage, and alteration in bone architecture[2-4]. AVN usually involves the epiphysis (end part of a long bone), such as the femoral and humeral heads and the femoral condyles, but small bones can also be affected. Clinically, most AVN cases are encountered in the hip. AVN can be most commonly due to trauma, which directly disrupts the blood supply. Non-traumatic causes include the use of glucocorticoids, alcohol intake, haematological diseases, metabolic diseases, pregnancy, chronic renal failure, and the use of intravenous (IV) bisphosphonates[5]. AVN of the hip was one of the dreaded complications of coronavirus disease 2019 (COVID-19), which emerged in patients who received steroid therapy. The use of high doses of corticosteroids had shown very positive results and had been lifesaving in many cases, but long-term consequences were drug-induced diabetes, osteoporosis, Cushing syndrome, muscle wasting, peripheral fat mobilization, AVN, hirsutism, sleep disturbances and poor wound healing[6]. Popular corticosteroid drugs used in COVID-19 patients were dexamethasone, methylprednisolone and hydrocortisone with IV or oral administration[7,8]. Management of AVN varies depending upon the patient's age, occupation, stage of AVN and previous treatment received. Surgical treatment during the early stages of AVN includes core decompression, bone grafting, valgus osteotomy, and tantalum rod. Total hip arthroplasty (THR) can be considered in later stages of surgical correction. THR is performed under spinal anaesthesia with numerous regional anaesthesia techniques to alleviate pre-operative and post-operative pain[9]. Femoral nerve block, fascia iliaca plane block, and femoral 3 in 1 block are the options for reducing post-operative pain. However, these blocks also cause motor blockades that can delay mobilization postoperatively[10]. Recent anatomical studies have shown that the anterior hip capsule is supplied by articular branches of both the femoral and obturator nerves, which these techniques may not optimally block. Pericapsular end nerve group (PENG) block is a novel regional anaesthesia technique, which helps to reduce post-operative pain as well as its motor-sparing block[11]. PENG block was first described by Girón-Arango et al[12] in 2018, as a plane block, which involves a single injection of a high volume of local anaesthetic, injected into the musculofascial plane between the psoas tendon anteriorly and the pubic ramus posteriorly. It provides perioperative analgesia in hip fracture patients by blocking the articular branches of the hip: the accessory obturator nerve, obturator nerve, and femoral nerve[12,13].
This prospective observational study was conducted in Department of Anaesthesiology at Care Hospital, Hyderabad. American Society of Anaesthesiology (ASA) grade I & II patients with a history of steroid use secondary to COVID-19 infection resulting in avascular necrosis requiring bilateral hip replacement were studied over 8 months. Inclusion criteria: (1) Either sex; (2) Patients between the ages of 30-35 years; (3) ASA grade I or II; (4) Bilateral total hip replacement (THR); and (5) Patients who are hemodynamically stable with all routine investigations within normal limit. Exclusion criteria: (1) Patients below 30 years and over 35 years of age; (2) Unilateral THR; (3) Patients with a pre-existing nerve deficit; (4) Patients with pre-existing peripheral neuropathy; (5) Patients with contraindication to peripheral nerve block (e.g., local anaesthetic allergy, coagulopathy, or infection at the block site); and (6) ASA III or IV patients.
After Institutional Ethics and Scientific Committee approval, 20 patients of either sex undergoing bilateral THR under spinal anaesthesia were enrolled on our study. Patients aged 30-35 and the ASA physical status I or II were randomly selected. After admission, a thorough pre-anaesthetic check-up was done, including a detailed history, physical and systemic examination, and relevant investigations. Patients were explained about the plan of anaesthesia and analgesia. Written and informed consent was taken from all the patients. The pre-operative Visual Analog Score (VAS) was assessed and noted.
On the day of surgery, after shifting the patient to the operation theatre, standard ASA monitors like pulse oximeter, electrocardiogram and non-invasive blood pressure were connected. Intravenous access was secured, and IV fluids were started. The patient was then seated, and spinal anaesthesia was performed at L3-L4 intervertebral space with a 27-gauge Whitacre needle using 0.5% Bupivacaine (heavy).
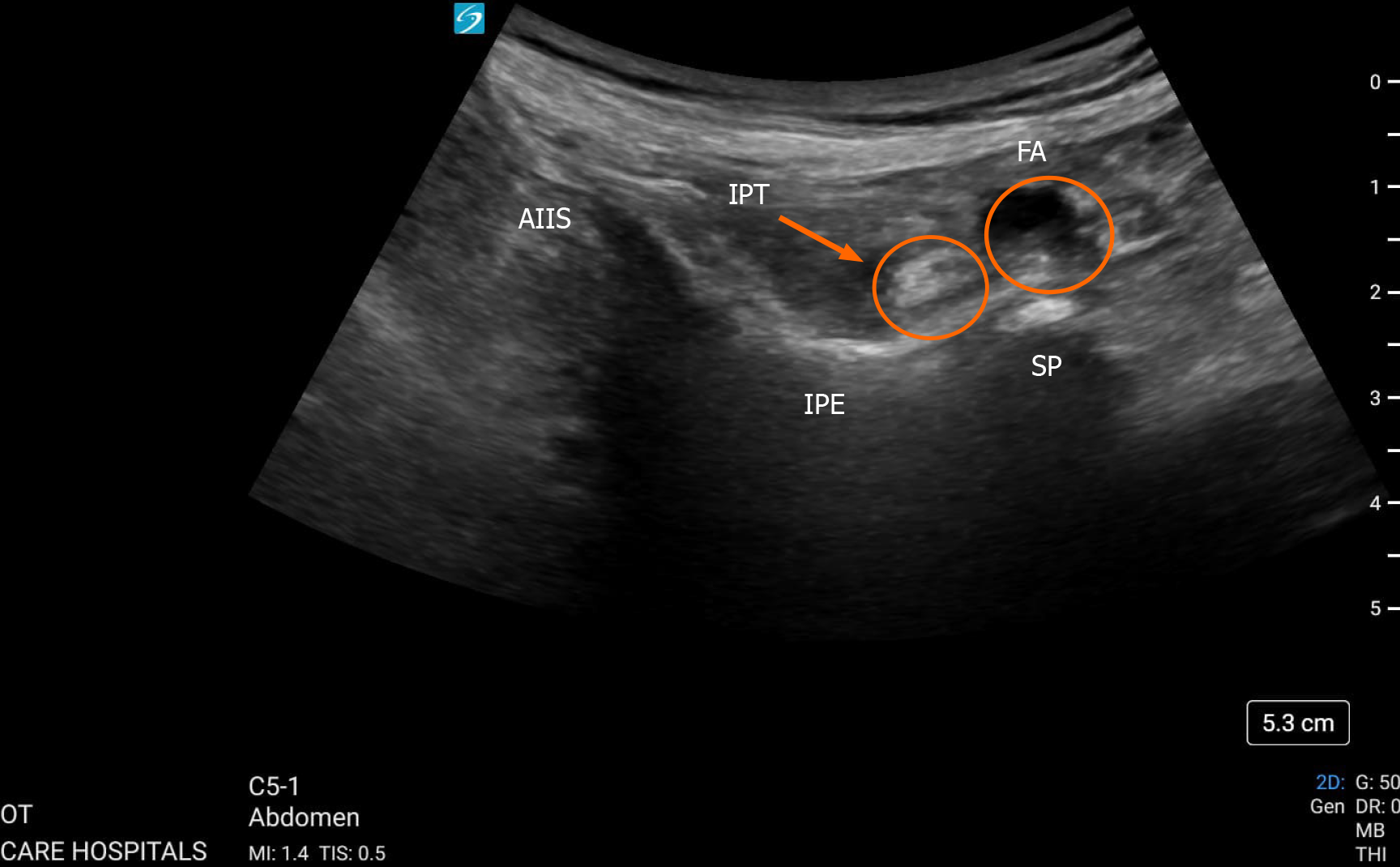
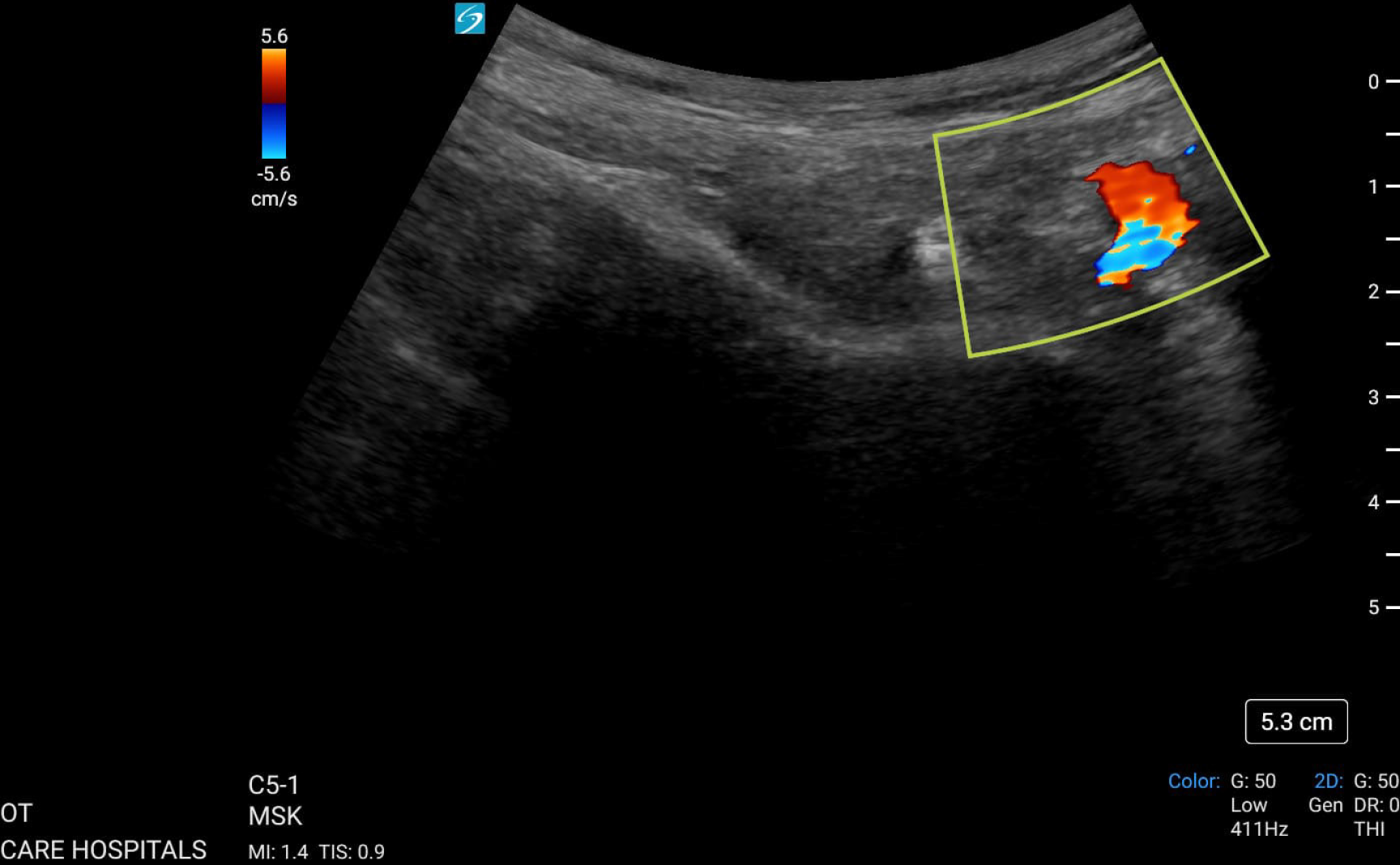
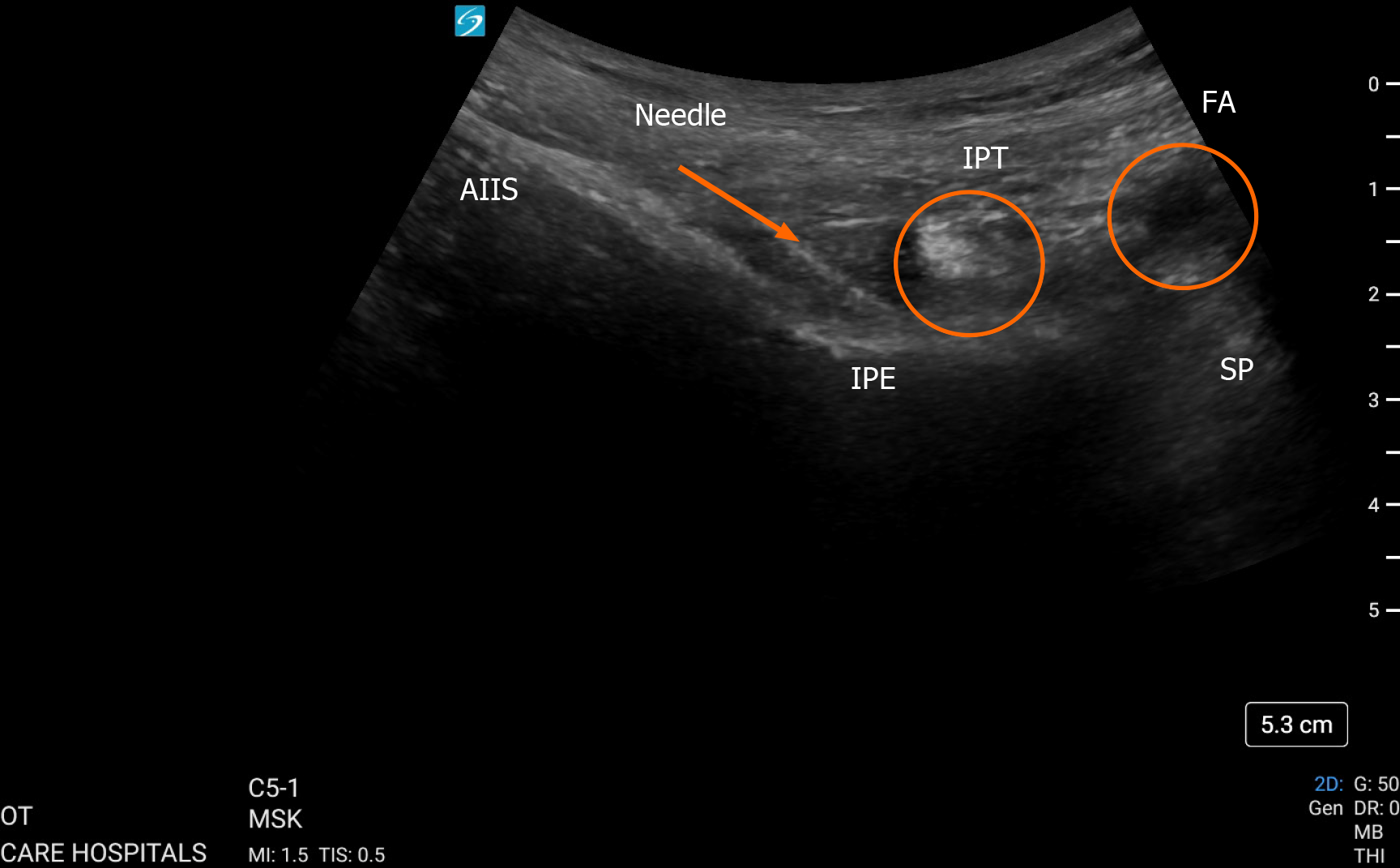
After checking the adequate anaesthesia level, B/L PENG blocks were given. A curvilinear low-frequency (2-5 MHz) ultrasound probe was used to identify the landmarks. The probe was placed caudal and medial to ASIS in a transverse orientation. The anteroinferior iliac spine, the iliopubic eminence, the psoas tendon and the femoral artery were identified (Figures 1 and 2). A 21-gauge 100-mm stimuplex needle was inserted using an in-plane lateral-to-medial approach. The needle was advanced between the psoas tendon and iliopubic eminence, and 20 mL of 0.2% ropivacaine was deposited after negative aspiration for blood (Figure 3). The local anaesthetic spread was observed. The block was repeated on the other side. The average duration of surgery was two and a half hours using a mini-posterior approach for THR (Figure 4).
After the surgery, patients were shifted to the post-surgical care unit. VAS score was assessed after 6 h, 12 h and 24 h. IV morphine 3 mg was administered as rescue analgesia if the patient complained of pain.
The statistics described were used to assess the efficacy of bilateral PENG block in patients posted for bilateral THR post-steroid therapy after COVID-19 infection. Quantitative variables are represented in terms of mean and standard deviation; qualitative variables are presented using count and percentages. The statistical analysis was performed in R software version 4.3.1. A paired t-test was used to compare the mean VAS scores.
This study enrolled 20 patients of either sex who were posted for bilateral THR. A total of 11 male and 9 female patients participated in the study over 8 months. Three patients (two males and one female) were excluded (Table 1).
| Number of patients | Female, n (%) | Male, n (%) | Age in yr, mean ± SD |
| 17 | 8 (47.1) | 9 (52.9) | 32.647 ± 1.618 |
Pre-operative mean VAS score of these patients was 6.412. After completion of surgery at 30 min, the mean VAS score was 0.471. This low pain score and significant motor block may be attributed to residual effect of the subarachnoid block. VAS score was assessed again 6 h after surgery. Among 20 patients, 17 had no/minimal pain with a mean VAS score of 0.824. Two patients complained of pain 2 h after surgery under spinal anaesthesia with PENG block and required rescue analgesia; they were excluded from the study. The VAS score was 1.765 12 h after surgery and all 17 patients were comfortable. The VAS score of 3.353 suggested significant pain 24 h after surgery (Table 2). All 15 patients were comfortable and could be mobilized after 12 h.
A paired t-test was employed to compare the mean VAS scores preoperatively and postoperatively at 12 h and 24 h. The results revealed a significant difference between the mean VAS scores at these time points, with a P value less than 0.001.
The above suggests that there was a significant pain reduction in patients administered PENG block at 6 h and 12 h after bilateral THR. While comparing 12 h and 24 h timepoints, the mean VAS score suggests significant pain after 24 h as the drug given during PENG block gets metabolized.
Sub-arachnoid block is preferred for THR as it shortens the length of hospital stay and reduces post-operative nausea and vomiting (PONV), blood loss and pulmonary complications compared to general anaesthesia[14]. Determining the ideal nerve or fascial plane block for post-operative pain relief is difficult in patients with THR, given its complex innervation. Although the placement of an epidural catheter for bilateral THR is the gold standard, it is associated with side effects like urinary retention and motor block, which may outweigh the beneficial effects[15].
Femoral nerve block, fascia iliaca plane block and femoral 3 1 block are the other blocks that can reduce post-operative pain after bilateral THR.
A femoral nerve block is a simple, superficial, easy-to-perform block that can be given bilaterally. Despite the above advantages, it may result in inadequate pain relief[10] and quadriceps weakness, which can interfere with patient mobilization, predisposing them to deep vein thrombosis. The fascia iliaca compartment block also provides good post-operative analgesia for THR[16]. In a study by Kamal Bansal and team, the suprainguinal fascia iliaca compartment block is superior to the infrainguinal fascia iliaca compartment block[17]. Significant motor blockage was observed with both these blocks, which can delay mobilization and ineffective/partially adequate analgesia[18,19]. Thybo et al[20] reported no additional analgesia when lateral femoral cutaneous nerve block was given along with a basic analgesic regimen. Huda et al[21] stated in their meta-analysis that quadratus lumborum block (QLB) provides good pain control post-THR surgery and reduces PONV. Limitations in their study were the use of different drugs, dose of local anaesthetics and approaches of QLB[21]. A study by Tayfun et al[22] suggested that the PENG block and QLB were equally effective in reducing post-operative pain after THR surgery, but the PENG block was more motor-protective. Only the articular branches of femoral and obturator nerves are blocked in the PENG block without significantly reducing muscle strength. This motor sparing is consistent with the previous study by Lin et al[24]. Preserving muscle strength makes early ambulation possible, leading to enhanced patient recovery[24-27]. PENG block also provides adequate analgesia for pre-operative analgesia in the emergency room, patient positioning during spinal block and post-operative analgesia for hip surgeries[28,29]. Kukreja et al[30] suggested that the PENG block and multimodal analgesia improve the recovery score. In this study, we chose PENG to block post-operative analgesia for THR in case of AVN. In contrast to the survey done by Aygun et al[29], who performed PENG block before the neuraxial blockade, we performed PENG post-neuraxial block. We observed that VAS scores were significantly lower 30 min post-surgery. This can be attributed to the spinal effect. Pain scores continued to be lower at 6 h and 12 h post-surgery. Two patients had a VAS score of 8 at 30 min, so they have been excluded from the study. One patient was re-explored for surgical reasons and was excluded from our study. A total of 17 patients were studied, among which 15 could mobilize with a VAS score less than 2 at an average of the 13th hour. The remaining two patients were uncooperative. Therefore, we conclude that pericapsular end nerve block is promising for adequate pain relief without major side effects. Comparative and extensive trial studies are required for further validation.
Osteonecrosis or AVN of the hip was one of the dreaded complications of COVID-19, which surfaced in patients who received steroid therapy requiring surgical intervention. Bilateral PENG Block is an effective technique to provide post-operative analgesia resulting in early mobilization and enhanced recovery after surgery.
Avascular necrosis of the hip emerged as a significant complication of steroid use during coronavirus disease 2019 (COVID-19) treatment requiring surgical intervention in the form of bilateral total hip replacements (THR). Pericapsular end nerve block (PENG) has been reported to provide good analgesia after THR. The study aimed to study the efficacy of the block and also add to the present limited knowledge.
The main motivation behind the study was to find an efficient and safe technique to provide analgesia to patients who have undergone bilateral THR surgery. Adequate analgesia will aid in early mobilization, prevent bed sores and deep vein thrombosis, which are important aspects of enhanced recovery after surgery.
The main objective was to evaluate the efficacy of PENG block in patients who underwent bilateral THR. We were able to conclude that the pain scores in patients were significantly low in patients who received PENG block. However, larger comparative studies are required to validate the use of this block.
Statistical analysis was performed in R software version 4.3.1. A paired t-test was employed to compare the mean Visual Analog Score (VAS).
A total of 17 patients were eligible for the study. The mean VAS score was 6.4 pre-operatively and 1.7 12 h after the procedure (P < 0.001). Two patients complained of pain after the PENG block and were therefore excluded from the study. All 15 patients were comfortable and could be mobilized 12 h after surgery.
This study proposes the use of PENG block for effective analgesia after total hip replacement.
This is a small study done on patients requiring total hip replacement following steroid use for COVID-19 treatment. We recommend further large comparative studies to test the efficacy of this block.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Anesthesiology
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Naderi D, Iran; Zhang L, China S-Editor: Zhang H L-Editor: Filipodia P-Editor: Zhao YQ
| 1. | Lespasio MJ, Sodhi N, Mont MA. Osteonecrosis of the Hip: A Primer. Perm J. 2019;23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 67] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 2. | Weinstein RS. Glucocorticoid-induced osteonecrosis. Endocrine. 2012;41:183-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 224] [Cited by in RCA: 282] [Article Influence: 21.7] [Reference Citation Analysis (0)] |
| 3. | Matthews AH, Davis DD, Fish MJ, Stitson D. Avascular Necrosis. 2023 Aug 28. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan- . [PubMed] |
| 4. | Chan KL, Mok CC. Glucocorticoid-induced avascular bone necrosis: diagnosis and management. Open Orthop J. 2012;6:449-457. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 85] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 5. | Wang Y, Li Y, Mao K, Li J, Cui Q, Wang GJ. Alcohol-induced adipogenesis in bone and marrow: a possible mechanism for osteonecrosis. Clin Orthop Relat Res. 2003;213-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 135] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 6. | Banerjee I, Robinson J, Sathian B. Corticosteroid induced avascular necrosis and COVID-19: The drug dilemma. Nepal J Epidemiol. 2021;11:1049-1052. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 7. | Fadel R, Morrison AR, Vahia A, Smith ZR, Chaudhry Z, Bhargava P, Miller J, Kenney RM, Alangaden G, Ramesh MS; Henry Ford COVID-19 Management Task Force. Early Short-Course Corticosteroids in Hospitalized Patients With COVID-19. Clin Infect Dis. 2020;71:2114-2120. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 249] [Cited by in RCA: 282] [Article Influence: 56.4] [Reference Citation Analysis (0)] |
| 8. | Mulchandani R, Lyngdoh T, Kakkar AK. Deciphering the COVID-19 cytokine storm: Systematic review and meta-analysis. Eur J Clin Invest. 2021;51:e13429. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 117] [Cited by in RCA: 172] [Article Influence: 43.0] [Reference Citation Analysis (0)] |
| 9. | Patel SB, Rheumatologist MD, Rheumatology DFW, Scott B, Health W. Avascular Necrosis Treatment & Management. Medscape. 2022 Aug 19 [cited 9 December 2023]. Available from: https://emedicine.medscape.com/article/333364-treatment?form=fpf. |
| 10. | Rowlands M, Walt GV, Bradley J, Mannings A, Armstrong S, Bedforth N, Moppett IK, Sahota O. Femoral Nerve Block Intervention in Neck of Femur Fracture (FINOF): a randomised controlled trial. BMJ Open. 2018;8:e019650. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 11. | Ben Aziz M, Mukhdomi J. Pericapsular Nerve Group Block. 2023 Feb 28. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan- . [PubMed] |
| 12. | Girón-Arango L, Peng PWH, Chin KJ, Brull R, Perlas A. Pericapsular Nerve Group (PENG) Block for Hip Fracture. Reg Anesth Pain Med. 2018;43:859-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 134] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 13. | Morrison C, Brown B, Lin DY, Jaarsma R, Kroon H. Analgesia and anesthesia using the pericapsular nerve group block in hip surgery and hip fracture: a scoping review. Reg Anesth Pain Med. 2021;46:169-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 76] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 14. | Basques BA, Toy JO, Bohl DD, Golinvaux NS, Grauer JN. General compared with spinal anesthesia for total hip arthroplasty. J Bone Joint Surg Am. 2015;97:455-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 168] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 15. | Min BW, Kim Y, Cho HM, Park KS, Yoon PW, Nho JH, Kim SM, Lee KJ, Moon KH. Perioperative Pain Management in Total Hip Arthroplasty: Korean Hip Society Guidelines. Hip Pelvis. 2016;28:15-23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 16. | Zhang XY, Ma JB. The efficacy of fascia iliaca compartment block for pain control after total hip arthroplasty: a meta-analysis. J Orthop Surg Res. 2019;14:33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 17. | Bansal K, Sharma N, Singh MR, Sharma A, Roy R, Sethi S. Comparison of suprainguinal approach with infrainguinal approach of fascia iliaca compartment block for postoperative analgesia. Indian J Anaesth. 2022;66:S294-S299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 18. | Ilfeld BM, Duke KB, Donohue MC. The association between lower extremity continuous peripheral nerve blocks and patient falls after knee and hip arthroplasty. Anesth Analg. 2010;111:1552-1554. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 304] [Cited by in RCA: 262] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 19. | Gasanova I, Alexander JC, Estrera K, Wells J, Sunna M, Minhajuddin A, Joshi GP. Ultrasound-guided suprainguinal fascia iliaca compartment block versus periarticular infiltration for pain management after total hip arthroplasty: a randomized controlled trial. Reg Anesth Pain Med. 2019;44:206-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 49] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 20. | Thybo KH, Schmidt H, Hägi-Pedersen D. Effect of lateral femoral cutaneous nerve-block on pain after total hip arthroplasty: a randomised, blinded, placebo-controlled trial. BMC Anesthesiol. 2016;16:21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 21. | Huda AU, Minhas R. Quadratus Lumborum Block Reduces Postoperative Pain Scores and Opioids Consumption in Total Hip Arthroplasty: A Meta-Analysis. Cureus. 2022;14:e22287. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 22. | Et T, Korkusuz M. Comparison of the pericapsular nerve group block with the intra-articular and quadratus lumborum blocks in primary total hip arthroplasty: a randomized controlled trial. Korean J Anesthesiol. 2023;76:575-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 16] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 23. | Gaffney CJ, Pelt CE, Gililland JM, Peters CL. Perioperative Pain Management in Hip and Knee Arthroplasty. Orthop Clin North Am. 2017;48:407-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 132] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 24. | Lin DY, Brown B, Morrison C, Fraser NS, Chooi CSL, Cehic MG, McLeod DH, Henningsen MD, Sladojevic N, Kroon HM, Jaarsma RL. The Pericapsular Nerve Group (PENG) block combined with Local Infiltration Analgesia (LIA) compared to placebo and LIA in hip arthroplasty surgery: a multi-center double-blinded randomized-controlled trial. BMC Anesthesiol. 2022;22:252. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 32] [Reference Citation Analysis (0)] |
| 25. | Kenyon-Smith T, Nguyen E, Oberai T, Jarsma R. Early Mobilization Post-Hip Fracture Surgery. Geriatr Orthop Surg Rehabil. 2019;10:2151459319826431. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 64] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 26. | Baer M, Neuhaus V, Pape HC, Ciritsis B. Influence of mobilization and weight bearing on in-hospital outcome in geriatric patients with hip fractures. SICOT J. 2019;5:4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 61] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 27. | Kuru T, Olçar HA. Effects of early mobilization and weight bearing on postoperative walking ability and pain in geriatric patients operated due to hip fracture: a retrospective analysis. Turk J Med Sci. 2020;50:117-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 28. | Del Buono R, Padua E, Pascarella G, Costa F, Tognù A, Terranova G, Greco F, Fajardo Perez M, Barbara E. Pericapsular nerve group block: an overview. Minerva Anestesiol. 2021;87:458-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 29. | Aygun H, Tulgar S, Yigit Y, Tasdemir A, Kurt C, Genc C, Bilgin S, Senoğlu N, Koksal E. Effect of ultrasound-guided pericapsular nerve group (PENG) block on pain during patient positioning for central nervous blockade in hip surgery: a randomized controlled trial. BMC Anesthesiol. 2023;23:316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 30. | Kukreja P, Uppal V, Kofskey AM, Feinstein J, Northern T, Davis C, Morgan CJ, Kalagara H. Quality of recovery after pericapsular nerve group (PENG) block for primary total hip arthroplasty under spinal anaesthesia: a randomised controlled observer-blinded trial. Br J Anaesth. 2023;130:773-779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 32] [Article Influence: 16.0] [Reference Citation Analysis (0)] |