Published online Jun 18, 2017. doi: 10.5312/wjo.v8.i6.455
Peer-review started: December 16, 2016
First decision: March 27, 2017
Revised: April 1, 2017
Accepted: April 23, 2017
Article in press: April 24, 2017
Published online: June 18, 2017
Processing time: 184 Days and 11.1 Hours
Sternal metastases are not studied extensively in the literature. There is a paucity of information on their role in metastatic disease. The concept of the fourth column was described by Berg in 1993, and has been proven in case report, clinically and biomechanical studies. The role of the sternum as a support to the thoracic spine is well documented in the trauma patients, but not much is known about its role in cancer patients. This review examines what is known on the role of the fourth column. Following this we have identified two likely scenarios that sternal metastases may impact management: (1) sternal pathological fracture increases the mobility of the semi-rigid thorax with the loss of the biomechanical support of the sternum-rib-thoracic spine complex; and (2) a sternal metastasis increases the risk of fracture, and while being medical treated the thoracic spine should be monitored for acute kyphosis and neurological injury secondarily to the insufficiency of the fourth column.
Core tip: The sternal-rib complex provides additional support to the thoracic spine. The role of sternal fracture affecting the stability of the thoracic spine is well established in trauma, to date however its role in metastatic disease is unclear. Biomechanical studies highlight its importance and the presence of sternal metastasis should be considered when assessing the stability of the thoracic spine in metastatic disease.
- Citation: Piggott RP, Curtin M, Munigangaiah S, Jadaan M, McCabe JP, Devitt A. Sternal metastasis - the forgotten column and its effect on thoracic spine stability. World J Orthop 2017; 8(6): 455-460
- URL: https://www.wjgnet.com/2218-5836/full/v8/i6/455.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i6.455
Cancer remains the second leading cause of death in the United States, with 589430 cancer related deaths each year[1]. In Europe, collective data from 40 countries has yielded an annual incidence of 3.45 million new cases per year, with 1.75 million cancer related deaths[2]. With early detection and increased treatment options, prolonged survival in patients with metastatic disease will result with increased incidence of skeletal related events (SREs) that will require orthopaedic intervention. The skeleton is the third most common site for metastatic disease to occur in the body, with only the lungs and liver with a higher incidence. Within the skeletal system, the spine is the most common site of metastases. The thoracic spine is most prone to metastatic disease as it contains the greatest volume of bone marrow per vertebrae[3]. Bone metastases are associated with a considerable degree of morbidity both due to pain and SREs. SREs are defined as a pathological fracture, a requirement for surgical intervention and palliative radiotherapy to a bone lesion, hypercalceamia of malignancy, and spinal cord compression. Metastatic spinal cord compression occurs in 3.4% patients with cancer per year in the United States[4] is a source of considerable morbidity. Breast, prostate, renal, lung, and haematopoietic tumours most commonly metastases to the spine and are discussed elsewhere in more detail. But what of sternal metastases which occur in the setting of spinal metastatic disease. Do they have an effect on the spine and its stability?
Sternal metastases are a rare phenomenon[5,6] and there is a paucity of information published regarding their incidence and also their effect on spine stability. Best medical therapy, such as external beam radiotherapy or chemotherapy, is advocated for the vast majority of cases[7] however when a pathological fracture occurs, then there is potential for delayed union and deformity. When present with concomitant thoracic spinal disease then the role of the sternum-rib-thoracic spine complex in thoracic spine stability, as the fourth column, is an important consideration. Berg[8] first proposed the fourth column in 1993, as an adjunct to the three-column theory of spine stability of Denis[9]. To date no study has looked at the role of the sternum in thoracic spine stability in the presence of a sternal metastasis. Hence the focus of this review is to identify what is known on the topic of sternal metastasis in the setting of spinal metastatic disease, and their potential effect on spine stability.
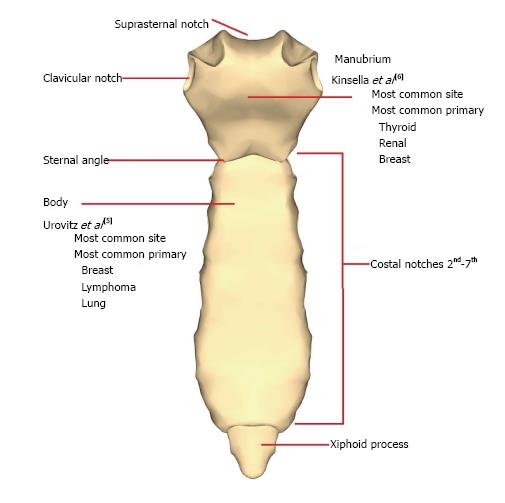
There has been little focus on the incidence and association of sternal metastatic disease in recent years. A necropsy study by Urovitz et al[5] form 1977 remains the largest single study on the topic. In a patient population of 415 patients, the incidence of sternal metastases was found to be 15.1%, of which 30.2% had a sternal fracture[5]. These fractures also demonstrated delayed or nonunion features and were associated with greater deformity than traumatic sternal fractures[5]. Conflicting reports on the commonest location and most prevalent tumours exist. Urovitz et al[5] identified the body of the sternum as the commonest site of metastases with breast, lymphoma and myeloma the most prevalent primary oncological processes. This was contrary to what was previously described by Kinsella et al[6] who concluded that the manubrium was most at risk, and that thyroid, renal and breast carcinoma were the most common. These findings are summarized in Figure 1.
Once sternal metastases have developed, best medical therapy with either radiotherapy, hormonal therapy or chemotherapy is recommended as per the primary diagnosis[7]. This is regardless of location and size of the metastatic disease as the sternum is a non-weight bearing bone and treatment is not altered by whether the lesion is osteoblastic, osteolytic or mixed on imaging[7]. The treating oncologist should closely evaluate the response of treatment, especially pain relief. If pathological fracture occurs, continued medical therapy is advocated and only those patients who fail best medical therapy are to be referred for consideration for surgical intervention[7]. Sternal metastasis in isolation may be treated by a number of mechanisms. Usually in the setting of isolated metastatic disease, the tumour may be excised and the sternum may be reconstructed with titanium mesh[10], locking titanium plate[11] or even an allogenic transplant[12]. In the palliative setting, kyphoplasty of sternal metastasis has been advocated for pain relief[13]. Unfortunately, all recommendations are for sternal metastases in isolation and do not take into account the sternum-rib-thoracic spine complex in combination. Specifically, there are no recommendations for the prophylactic surgery on the sternum to prevent fracture in a patient with concurrent spinal metastatic disease.
Spinal metastases can be treated medically, with radiotherapy and or spinal surgery and treatment must be individualized to accommodate for tumour type, performance status of the patient, life expectancy and neurological status. It is a fundamental realization that any intervention with regards spinal metastases is palliative. There are four primary indications to intervening in metastatic disease of the spine: Neurological compromise, spinal instability, unrelenting pain and in the case which histological diagnosis must be established. Historically radiotherapy became the first-line treatment for most patients[14]. Recent advances in imaging, surgical technique and instrumentation systems have improved outcomes from surgery. Patchell et al[15] in a randomized control trial showed that surgery follow by radiotherapy to be superior to radiotherapy alone. These findings were reproduced in a large multicentre observational study[16]. The is a multitude of evidence on surgery in neurological compromise including spinal cord compression, in which cases the spine needs to be decompressed and stabilized[17-19]. The sternum in this setting does not play a role in the management strategy as the evidence supports intervention regardless of sternal disease. Likewise, management of intractable pain and the need for histological diagnosis is not altered by whether disease is present in the sternum. Spinal stability however is directly affected by the sternum in biomechanical studies of the spine[20] and thus it follows that it has the potential to affect stability in the metastatic spine, but remains to be investigated fully.
Assessing the spine stability in metastatic disease however is more difficult, and especially in the setting of impending instability, the sternum could play a role. Form the literature we know that defining instability in the spine using trauma criteria is not directly applicable to the setting of metastatic disease[21]. This is because the injury does not follow typical patterns seen in trauma, and involves different biological healing potential and patient factors[22]. As we have no evidence on the topic then we must be cautious when applying observations from traumatic sternal and spinal injuries to the oncological setting as we assess the thoracic spine as a whole with the sternum-rib-thoracic spine complex.
The Spine Oncology Study Group (SOSG) defines stability as the “loss of spinal integrity as a result of a neoplastic process that is associated with movement-related pain, symptomatic or progressive stability and/or neurological compromise under physiological loads”[22]. It is the major goal of any spinal surgery in oncology to preserve or restore the spines stability. Regardless of indication, surgery is generally reserved for patients with a life expectancy of greater than 3 mo[23]. To determine a patient’s life expectancy, multiple scoring systems have been developed. Tokuhashi et al[24] developed one example of a scoring system to evaluate prognosis of metastatic spine tumour patients. This was further assessed by Enkaoua et al[25] regarding its reliability, and demonstrates a median survival of 5.7 mo with a score ≤ 7 mo vs 23.6 mo for a score of ≥ 8. Regardless of scoring systems however, establishing survival of patients is subjective and must take into account multiple patient and disease factors before a decision on suitability for surgery is made.
Surgeons rely on their clinical experience as well as internationally accepted scoring systems to determine a spines stability and appropriate treatment. The SOSG have provided a classification n system for spinal instability - The Spinal Instability Neoplastic Score (SINS) - which was developed from existing evidence based medicine and expert consensus opinion[22]. Factors included in the score include location, pain, alignment, vertebral body collapse, posterior element involvement and type of bone lesion (Table 1). The SINS has been shown to have good inter- and intraobserver reliability in determining stability. Stability is derived from overall score out of a max score of 18. Neoplastic disease is deemed unstable with a score of 13-18, stable with a score of 0-6 and indeterminate instability or possibly impending with a score of 7-12. The specificity and sensitivity of the SINS for unstable or potentially unstable spines is 95.7% and 79.5% respectively. The SINS provides a useful tool for assessing spinal disease and aids in the decision making for surgical intervention but is not binding. Unfortunately the sternum is not considered in the SINS in its current format, and thus the fourth column becomes the forgotten column when considering spine stability in metastatic disease.
| Score | |
| Spine location | |
| Junctional (occiput-C2, C7-T2, T11-L1, L5-S1) | 3 |
| Mobile (C3-C6, L2-L4) | 2 |
| Semi-rigid (T3-T10) | 1 |
| Rigid (S2-S5) | 0 |
| Mechanical or postural pain | |
| Yes | 3 |
| No (occasional pain but not mechanical) | 1 |
| Pain-free lesion | 0 |
| Bone lesion quality | |
| Lytic | 2 |
| Mixed lytic/blastic | 1 |
| Blastic | 1 |
| Radiographic spinal alignment | |
| Subluxation/translation | 4 |
| De novo deformity (kyphosis/scoliosis) | 1 |
| Normal | 0 |
| Vertebral body involvement | |
| > 50% collapse | 3 |
| < 50% collapse | 2 |
| No collapse with > 50% involvement | 1 |
| None of the above | 0 |
| Posterior involvement | |
| Bilateral | 3 |
| Unilateral | 1 |
| None | 0 |
Further scoring systems exist which can also aid in the decision making process. As survivorship improves with neoplastic conditions so does the incidence of metastatic disease in the axial skeleton. Predicting the survivorship of patients with metastatic disease is important in the planning of surgical intervention. The Oswestry Spinal Risk Index (OSRI) is a simple, reproducible measure of survivorship looking at primary tumor pathology and the patient’s general condition[26]. It has been externally validated twice and provides accurate prediction of a patients survivorship which can be used in the decision making process[27,28].
Biomechanically, the inherent stability of the thoracic spine is augmented by the sternum and rib cage, which increases the moment of inertia and stiffens the spine against rotary forces[29]. There is a multitude of evidence from case reports, retrospective reviews and biomechanical studies on the importance of the sternum and ribs in the presence of thoracic spine injury in acute trauma but none on metastatic disease. The association between sternal fractures and spine injuries is well documented in the literature[8,30-32]. In clinical practice a spinal injury must be suspected to exist in the presence of a sternum fracture, even at discordant levels.
A 50-year literature review by Fowler[30] concluded that 43% of sternum fractures had associated spinal fractures. Berg postulated that the sternum and ribs represents a fourth column of structural support for the thoracic spine in addition to the three described by Denis[8]. The three column model divides the osteoligamentous structures of the spinal column into an anterior, middle and posterior column[9]. Involvement of 2 of the 3 columns resulted in potentially unstable spinal injury at risk of progressive deformity and neurological compromise[9]. The additional fourth column theory was based on two cases of displaced sternal fractures with minimally displaced thoracic spine injuries leading to progressive kyphosis[8].
This pattern of injury is often associated with neurological compromise, with increasing degrees of kyphosis being observed. Golpalakrish and Masri reported 83% of patients with sternum and spine fracture combinations had complete neurologic injury and were paraplegic[32]. Vioreanu et al[31] in 2005 reported an incidence of 1.4% of sternal fracture with vertebral fracture, which rises to 9.2% when the subset of thoracic fractures is examined in isolation. There is a clear association of neurological compromise in these patients with all six patients suffering neurological injury of which four patients had complete injuries[31].
However, neither Berg nor Vioreanu et al[31] described the behavior of a three-column injury with an intact sternum or “fourth column”. A case report by Shen describes how the sternum provided sufficient stability for the conservative management of a three-column unstable injury pattern in an ankylosing spondylitis patient without neurological compromise[33]. The authors concluded that the case confirmed the existence and clinical relevance of the fourth column proposed by Berg. An in vitro cadaveric study estimated that the sternum-rib complex accounts for up to 78% of thoracic stability[34]. Watkins et al[20] examined the biomechanics of the fourth column in 10 human cadaveric thoracic spines using multidirectional flexibility tests. They found that an indirect flexion-compression fracture of the sternum decreased the stability of the thoracic spine by 42% in flexion-extension, 22% in lateral bending and 15% in axial rotation[20]. This is evidence of the importance of the sternum in stability of the thoracic spine, and why the thoracic spine is considered a semi-rigid structure[22]. Following from this we can conclude that sternal and thoracic spine injury is a potentially unstable combination.
Metastasis of the sternum and their role on stability is not addressed in the Spinal Instability Neoplastic Score (Table 1). There are two areas where they have a potential role, which needs to be further explored. The thorax (T3-T10) is termed semi-rigid in the location score secondary to the biomechanical benefit of the sternum and rib cage, and is only scored 1 out of a possible 3. Concomitant sternal metastasis with pathological fracture would affect the semi rigid nature of the thorax with loss of the stability provided by the fourth column. The flexion-extension stability of the spine is reduced by 42%[20] in this setting regardless of thoracic disease, with rotational and lateral bending also affected. We must ask the question - with the loss of the biomechanical benefit of the sternum, should the thoracic now be considered “mobile” and the location score increased to 2 to reflect this? Secondarily, in the presence of metastases without pathological fracture, a lytic lesion of the sternum would be at risk for impeding fracture and should be observed closely. If the spine is deemed stable, close follow up of both the sternal and thoracic metastatic disease is required as early de novo kyphosis deformity would add an additional 2 points to a patients score and may change management. The association between kyphosis and loss of sternal integrity is well established in case reports and carries a significant risk of neurological injury[8,30,32].
In addition, sternal metastasis may be painful but this would not impact on the SINS pain score. Local pain may be related to the sternal metastases themselves but back pain in the setting of concurrent sternum and spine disease which worsens with movement and loading of the spine and is relieved by recumbence would suggest that it is mechanical in nature and thus increase the patients score, as set out by the SOSG[22].
In conclusion, the thoracic spine should not be examined in isolation. The sternum is a pivotal support in thoracic spine stability and should not be overlooked when assessing a patient’s thoracic spine. Assess spinal stability in the metastatic diseased spine is a complex and multifactorial process. The sternum provides essential support to the thorax spine and pathological fracture or impending fracture in the sternum has the potential for acute deformity of the thoracic spine that could lead to neurological injury. No evidence exists on the sternum role in metastatic spinal stability to date and thus hard conclusions cannot be made. We recommend that sternal metastatic disease be assessed in conjunction with spinal metastatic disease, and that treatment be tailored to individual cases. Further study is needed to fully evaluate the role of the sternum in spine stability with metastatic disease. A biomechanical study looking at the location and involvement of the sternum and the subsequent risk of fracture and deformity is needed to quantify the risk to the spine. Following this there may be a role for modification of the SINS once their role has been fully investigated. For now, clinical judgment is recommended until further evidence is provided in the literature.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: Ireland
Peer-review report classification
Grade A (Excellent): A, A, A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Erkan S, Kahveci R, Teli MGA S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | American Cancer Society. Cancer Facts & Figures 2015. Available from: http://www.cancer.org/acs/groups/content/@editorial/documents/document/acspc-044552.pdf. |
| 2. | Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JW, Comber H, Forman D, Bray F. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer. 2013;49:1374-1403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3526] [Cited by in RCA: 3651] [Article Influence: 304.3] [Reference Citation Analysis (2)] |
| 3. | Taneichi H, Kaneda K, Takeda N, Abumi K, Satoh S. Risk factors and probability of vertebral body collapse in metastases of the thoracic and lumbar spine. Spine (Phila Pa 1976). 1997;22:239-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 156] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 4. | Mak KS, Lee LK, Mak RH, Wang S, Pile-Spellman J, Abrahm JL, Prigerson HG, Balboni TA. Incidence and treatment patterns in hospitalizations for malignant spinal cord compression in the United States, 1998-2006. Int J Radiat Oncol Biol Phys. 2011;80:824-831. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 66] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 5. | Urovitz EP, Fornasier VL, Czitrom AA. Sternal metastases and associated pathological fractures. Thorax. 1977;32:444-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Kinsella TJ, White SM, Koucky RW. Two unusual tumors of the sternum. J Thorac Surg. 1947;16:640-667. [PubMed] |
| 7. | Capanna R, Campanacci DA. The treatment of metastases in the appendicular skeleton. J Bone Joint Surg Br. 2001;83:471-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 82] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 8. | Berg EE. The sternal-rib complex. A possible fourth column in thoracic spine fractures. Spine (Phila Pa 1976). 1993;18:1916-1919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 68] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976). 1983;8:817-831. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1792] [Cited by in RCA: 1414] [Article Influence: 33.7] [Reference Citation Analysis (0)] |
| 10. | Zhang Y, Li JZ, Hao YJ, Lu XC, Shi HL, Liu Y, Zhang PF. Sternal tumor resection and reconstruction with titanium mesh: a preliminary study. Orthop Surg. 2015;7:155-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | Demondion P, Mercier O, Kolb F, Fadel E. Sternal replacement with a custom-made titanium plate after resection of a solitary breast cancer metastasis. Interact Cardiovasc Thorac Surg. 2014;18:145-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Stella F, Dell’Amore A, Dolci G, Cassanelli N, Caroli G, Zamagni C, Bini A. Allogenic sternal transplant after sternectomy for metastasis of ovarian carcinoma. Ann Thorac Surg. 2012;93:e71-e72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Shah RV. Sternal kyphoplasty for metastatic lung cancer: image-guided palliative care, utilizing fluoroscopy and sonography. Pain Med. 2012;13:198-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Gilbert RW, Kim JH, Posner JB. Epidural spinal cord compression from metastatic tumor: diagnosis and treatment. Ann Neurol. 1978;3:40-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 746] [Cited by in RCA: 570] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 15. | Patchell RA, Tibbs PA, Regine WF, Payne R, Saris S, Kryscio RJ, Mohiuddin M, Young B. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet. 2005;366:643-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1662] [Cited by in RCA: 1501] [Article Influence: 75.1] [Reference Citation Analysis (0)] |
| 16. | Ibrahim A, Crockard A, Antonietti P, Boriani S, Bünger C, Gasbarrini A, Grejs A, Harms J, Kawahara N, Mazel C. Does spinal surgery improve the quality of life for those with extradural (spinal) osseous metastases? An international multicenter prospective observational study of 223 patients. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2007. J Neurosurg Spine. 2008;8:271-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 218] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 17. | Choi D, Crockard A, Bunger C, Harms J, Kawahara N, Mazel C, Melcher R, Tomita K. Review of metastatic spine tumour classification and indications for surgery: the consensus statement of the Global Spine Tumour Study Group. Eur Spine J. 2010;19:215-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 200] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 18. | Klimo P, Thompson CJ, Kestle JR, Schmidt MH. A meta-analysis of surgery versus conventional radiotherapy for the treatment of metastatic spinal epidural disease. Neuro Oncol. 2005;7:64-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 250] [Cited by in RCA: 232] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 19. | George R, Jeba J, Ramkumar G, Chacko AG, Leng M, Tharyan P. Interventions for the treatment of metastatic extradural spinal cord compression in adults. Cochrane Database Syst Rev. 2008;CD006716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 42] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 20. | Watkins R, Watkins R, Williams L, Ahlbrand S, Garcia R, Karamanian A, Sharp L, Vo C, Hedman T. Stability provided by the sternum and rib cage in the thoracic spine. Spine (Phila Pa 1976). 2005;30:1283-1286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 130] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 21. | Fourney DR, Gokaslan ZL. Spinal instability and deformity due to neoplastic conditions. Neurosurg Focus. 2003;14:e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 59] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 22. | Fisher CG, DiPaola CP, Ryken TC, Bilsky MH, Shaffrey CI, Berven SH, Harrop JS, Fehlings MG, Boriani S, Chou D. A novel classification system for spinal instability in neoplastic disease: an evidence-based approach and expert consensus from the Spine Oncology Study Group. Spine (Phila Pa 1976). 2010;35:E1221-E1229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 996] [Cited by in RCA: 768] [Article Influence: 51.2] [Reference Citation Analysis (0)] |
| 23. | White AP, Kwon BK, Lindskog DM, Friedlaender GE, Grauer JN. Metastatic disease of the spine. J Am Acad Orthop Surg. 2006;14:587-598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 57] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 24. | Tokuhashi Y, Matsuzaki H, Toriyama S, Kawano H, Ohsaka S. Scoring system for the preoperative evaluation of metastatic spine tumor prognosis. Spine (Phila Pa 1976). 1990;15:1110-1113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 531] [Cited by in RCA: 444] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 25. | Enkaoua EA, Doursounian L, Chatellier G, Mabesoone F, Aimard T, Saillant G. Vertebral metastases: a critical appreciation of the preoperative prognostic tokuhashi score in a series of 71 cases. Spine (Phila Pa 1976). 1997;22:2293-2298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 114] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 26. | Balain B, Jaiswal A, Trivedi JM, Eisenstein SM, Kuiper JH, Jaffray DC. The Oswestry Risk Index: an aid in the treatment of metastatic disease of the spine. Bone Joint J. 2013;95-B:210-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 63] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 27. | Whitehouse S, Stephenson J, Sinclair V, Gregory J, Tambe A, Verma R, Siddique I, Saeed M. A validation of the Oswestry Spinal Risk Index. Eur Spine J. 2016;25:247-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 28. | Fleming C, Baker JF, O’Neill SC, Rowan FE, Byrne DP, Synnott K. The Oswestry Spinal Risk Index (OSRI): an external validation study. Eur Spine J. 2016;25:252-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 29. | White AA, Panjabi MM. Clincal Biomechanics of the Spine. Philadelphia: Lippincott 1978; 191-192. |
| 30. | Fowler AW. Flexion-compression injury of the sternum. J Bone Joint Surg Br. 1957;39-B:487-497. [PubMed] |
| 31. | Vioreanu MH, Quinlan JF, Robertson I, O’Byrne JM. Vertebral fractures and concomitant fractures of the sternum. Int Orthop. 2005;29:339-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 26] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 32. | Gopalakrishnan KC, el Masri WS. Fractures of the sternum associated with spinal injury. J Bone Joint Surg Br. 1986;68:178-181. [PubMed] |
| 33. | Shen FH, Samartzis D. Successful nonoperative treatment of a three-column thoracic fracture in a patient with ankylosing spondylitis: existence and clinical significance of the fourth column of the spine. Spine (Phila Pa 1976). 2007;32:E423-E427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 34. | Brasiliense LB, Lazaro BC, Reyes PM, Dogan S, Theodore N, Crawford NR. Biomechanical contribution of the rib cage to thoracic stability. Spine (Phila Pa 1976). 2011;36:E1686-E1693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 59] [Article Influence: 4.2] [Reference Citation Analysis (0)] |