Published online Apr 18, 2017. doi: 10.5312/wjo.v8.i4.301
Peer-review started: October 1, 2016
First decision: November 10, 2016
Revised: December 22, 2016
Accepted: February 8, 2017
Article in press: February 13, 2017
Published online: April 18, 2017
Processing time: 201 Days and 4.2 Hours
Reconstruction of unstable syndesmotic injuries is not trivial, and there is no generally accepted treatment guidelines. Thus, there still remain considerable controversies regarding diagnosis, classification and treatment of syndesmotic injuries. Syndesmotic malreduction is the most common indication for early re-operation after ankle fracture surgery, and widening of the ankle mortise by only 1 mm decreases the contact area of the tibiotalar joint by 42%. Outcome of ankle fractures with syndesmosis injury is worse than without, even after surgical syndesmotic stabilization. This may be due to a high incidence of syndesmotic malreduction revealed by increasing postoperative computed tomography controls. Therefore, even open visualization of the syndesmosis during the reduction maneuver has been recommended. Thus, the most important clinical predictor of outcome is consistently reported as accuracy of anatomic reduction of the injured syndesmosis. In this context the TightRope® system is reported to have advantages compared to classical syndesmotic screws. However, rotational instability of the distal fibula cannot be safely limited by use of 1 or even 2 TightRopes®. Therefore, we developed a new syndesmotic InternalBraceTM technique for improved anatomic distal tibiofibular ligament augmentation to protect healing of the injured native ligaments. The InternalBraceTM technique was developed by Gordon Mackay from Scotland in 2012 using SwiveLocks® for knotless aperture fixation of a FiberTape® at the anatomic footprints of the augmented ligaments, and augmentation of the anterior talofibular ligament, the deltoid ligament, the spring ligament and the medial collateral ligaments of the knee have been published so far. According to the individual injury pattern, patients can either be treated by the new syndesmotic InternalBraceTM technique alone as a single anterior stabilization, or in combination with one posteriorly directed TightRope® as a double stabilization, or in combination with one TightRope® and a posterolateral malleolar screw fixation as a triple stabilization. Moreover, the syndesmotic InternalBraceTM technique is suitable for anatomic refixation of displaced bony avulsion fragments too small for screw fixation and for indirect reduction of small posterolateral tibial avulsion fragments by anatomic reduction of the anterior syndesmosis with an InternalBraceTM after osteosynthesis of the distal fibula. In this paper, comprehensively illustrated clinical examples show that anatomic reconstruction with rotational stabilization of the syndesmosis can be realized by use of our new syndesmotic InternalBraceTM technique. A clinical trial for evaluation of the functional outcomes has been started at our hospital.
Core tip: Reconstruction of unstable syndesmotic injuries is not trivial, and there are no generally accepted treatment guidelines. The TightRope® system is reported to have advantages compared to classical syndesmotic screws. However, rotational instability of the distal fibula is not safely eliminated by use of 1 or even 2 TightRopes®. Therefore, we developed a new syndesmotic InternalBraceTM technique using SwiveLocks® for knotless aperture fixation of a FiberTape® at the anatomic footprints of the injured ligaments for improved anatomic distal tibiofibular ligament augmentation to protect healing of the injured native ligaments.
- Citation: Regauer M, Mackay G, Lange M, Kammerlander C, Böcker W. Syndesmotic InternalBraceTM for anatomic distal tibiofibular ligament augmentation. World J Orthop 2017; 8(4): 301-309
- URL: https://www.wjgnet.com/2218-5836/full/v8/i4/301.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i4.301
The ligaments stabilizing the syndesmosis prevent excess fibular motion in multiple directions: Anterior-posterior translation, lateral translation, cranio-caudal translation, and internal and external rotation[1]. Appropriate fibular position and limited rotation are necessary for normal syndesmotic function and talar position within the ankle mortise[2]. Reconstruction of unstable syndesmotic injuries is not trivial, and there is no generally accepted treatment guidelines[1,3,4]. Thus, there still remains considerable controversies regarding diagnosis, classification and treatment of syndesmotic injuries[1,5]. Syndesmotic malreduction is the most common indication for early re-operation after ankle fracture surgery, and widening of the ankle mortise by only 1 mm decreases the contact area of the tibiotalar joint by 42%[6-9]. Syndesmotic instability is a strong predictor for less favorable clinical outcomes of ankle fractures, even after surgical syndesmotic stabilization. This may be due to a high incidence of syndesmotic malreduction revealed by increasing postoperative computed tomography (CT) controls[10-14]. Therefore, even open visualization of the syndesmosis during the reduction maneuver has been recommended[13]. Thus, the most important clinical predictor of outcome is consistently reported as accuracy of anatomic reduction of the injured syndesmosis[12,14,15].
In this context the TightRope® system (Arthrex®, Naples, United States) is repeatedly reported to have advantages compared to classical syndesmotic screws[12,16-18]. However, rotational instability of the distal fibula cannot be safely limited by standard use of 1 or even 2 TightRopes® as shown by Teramoto et al[18] who tried to imitate anatomy by use of different directions of the TightRopes®.
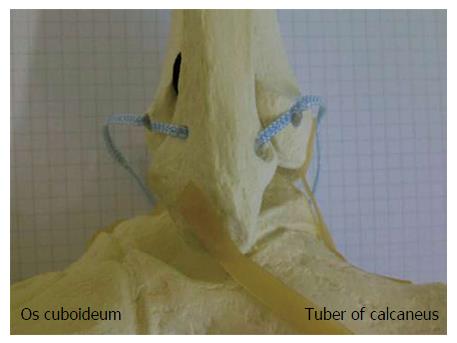
Therefore, we developed a new syndesmotic InternalBraceTM technique using SwiveLocks® (Arthrex®, Naples, United States ) for knotless aperture fixation of a FiberTape® (Arthrex®, Naples, United States ) directly at the anatomic footprints of the injured ligaments for an optimized imitation of the anatomy of the anterior and posterior syndesmosis to protect healing of the injured native ligaments. Figure 1 shows a simulation of an anatomic augmentation of the anterior and posterior tibiofibular ligament by use of a syndesmotic InternalBraceTM technique in a skeletal model of a left ankle joint.
The InternalBraceTM technique was developed by Gordon Mackay from Scotland in 2012 using SwiveLocks® for knotless aperture fixation of a FiberTape® at the anatomic footprints of the augmented ligaments, and augmentation of the anterior talofibular ligament[19-22], the deltoid ligament[3], the spring ligament[23], and the medial collateral and cruciate ligaments of the knee have been published so far[24-28].
The primary aim of an InternalBraceTM is repair of vital tissue rather than reconstruction or replacement with non-vital tendon transplants[3]. Ligament healing should be standard rather than replacement, as the original footprints of ligaments tend to be much larger than tendon grafts could replace. So an important advantage of the the InternalBraceTM technique is preservation of proprioception instead of cutting out the ligament remnants. An InternalBraceTM acts as a check-rein or as a corner stone to stability just like a seat-belt, and thus the InternalBraceTM supports early mobilization of a repaired ligament and allows the natural tissues to progressively strengthen[3,25]. In analogy to fracture repair, an InternalBraceTM applies AO principles to soft tissues.
The FiberTape® is a braided ultra-high-molecular-weight polyethylene/polyester suture tape which has an ultimate tensile strength of about 750 N[3]. Until June 2014, when we started to use this new technique, about 732000 FiberTapes® have been sold, and a total of only 95 complications due to FiberTapes® have been reported so far (internal information by Arthrex). According to Peter Miller FiberTapes® have been recognized to be “incorporated” after 4 mo in revision shoulder surgery. Taken as a whole, FiberTapes® can be considered very safe implants. Alternative applications of FiberTapes®, SwiveLocks® or the InternalBraceTM technique, respectively, are augmentation of the anterolateral ligament of the knee, additional AC-joint stabilization in the horizontal plane, augmentation of the ulnar collateral ligaments for elbow stabilization, or minimally invasive repair of ruptured Achilles tendons[3,29,30].
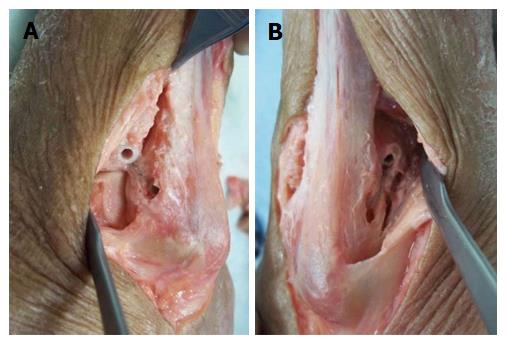
Primary feasibility studies in human cadaver models showed that the syndesmotic InternalBraceTM technique can be performed easily in a minimally invasive fashion (Figures 2 and 3). A longitudinal incision about 15 mm long was performed at the level of the ankle joint line just a few millimeters anterior and posterior of the distal fibula. An aiming drill guide was used to insert a k-wire into the distal fibula from the anterior to the posterior footprint of the syndesmotic ligaments for creating a bone tunnel using a 2.7 mm cannulated drill (Figure 2A). A FiberTape® was inserted through the bone tunnel until the middle of the tape was inside the tunnel. The FiberTape® was then locked securely inside the bone tunnel of the distal fibula by use of an interference screw (SwiveLock® 3.5 mm) to avoid movements of the tape inside the tunnel with potential sawing effects (Figure 2B). Using the existing approaches, 3.4 mm bone tunnels were drilled at the tibial footprints of the anterior and posterior syndesmotic ligaments identified by fluoroscopy, and after adequate tapping of the bone tunnels and correct positioning of the distal fibula, both free ends of the FiberTape® were fixed into the bone tunnels with a 4.75 mm SwiveLock® (Figure 2C-F). Control of the minimally invasively performed positioning of the implants was possible by extensive opening of the cadaver situs. The view from anterolateral (Figure 3A) and from posterolateral (Figure 3B) on the left ankle joint reveals correct placement of the four anchors for anatomic reduction and augmentation of the anterior and posterior tibiofibular ligaments. Based on these positive results of the feasibility studies we started to use this technique in patients.
According to the individual injury pattern, patients were either treated by the new syndesmotic InternalBraceTM technique alone as a single anterior stabilization (Figure 4), or in combination with one posteriorly directed TightRope® as a double stabilization (Figures 5 and 6), or in combination with one TightRope® and a posterolateral malleolar screw fixation as a triple stabilization (Figure 7).
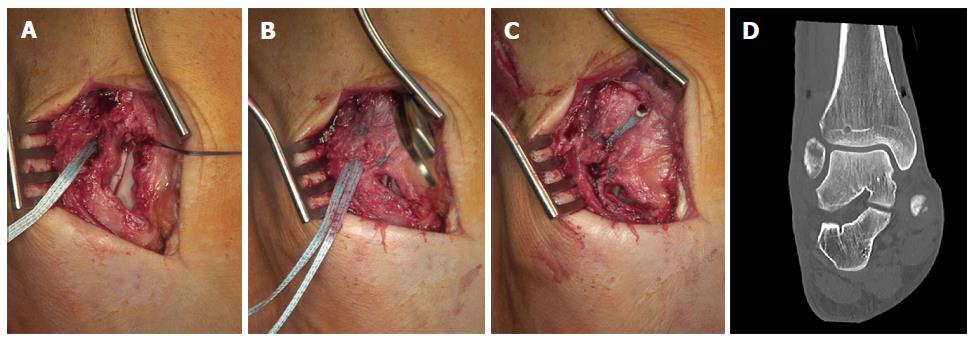
Figure 4 shows the clinical example of a 32-year-old female soccer player with acute injury of the anterior syndesmosis after supination-inversion sprain of the right ankle (Figure 4A). We sutured the torn ligament (Figure 4B) and performed a single stabilization of the anterior syndesmosis with a 3.5 mm SwiveLock® at the fibular and a 4.75 mm SwiveLock® at the tibial footprint, respectively (Figure 4C). In case of open surgery, the fibular and tibial footprints can be identified by direct visualization just following the fibers of the injured ligament. Here it is important to avoid distal malpositioning of the SwiveLocks to prevent impinging of the FiberTape® on the anterolateral aspect of the talus. To avoid over-constraining of the anterior syndesmosis a hemostat clamp can be put under the FiberTape® during tensioning. After surgery we performed a CT scan to verify anatomic positioning of the ankle mortise and correct screw placement (Figure 4D).
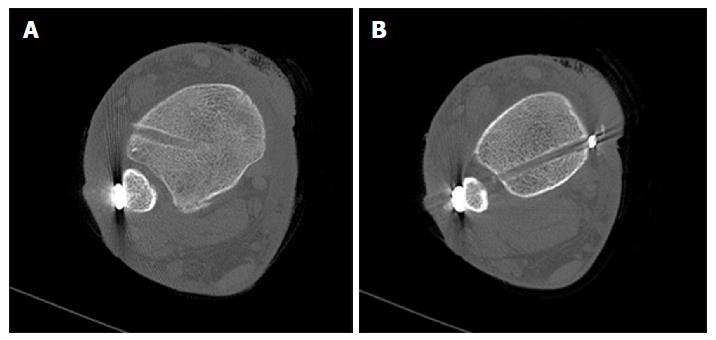
Figure 5 shows a double stabilization with an anterior InternalBraceTM and one posteriorly directed TightRope® resulting in a perfect indirect reduction of the small posterolateral avulsion fragment. The 45-year-old male patient sustained a type B ankle fracture with posterolateral subluxation of the talus due to an avulsion of the posterolateral malleolus (Figures 6A, C, E and G). After standard plate osteosynthesis of the distal fibula the syndesmosis remained unstable, especially when performing external rotation or posterior translation of the distal fibula. Due to the multidirectional instability of the syndesmosis a double stabilization was performed. Here the sequence of stabilization is important: First the anterior stabilization should be performed ensuring anatomic positioning of the distal fibula under direct visualization so that the posteriorly directed second stabilization using the TightRope® will not lead to malreduction. In contrast, not directing the TightRope® posteriorly could lead to malreduction in kind of anterior displacement or malrotation of the distal fibula. To protect the neurovascular bundle the surgeon has to check under fluoroscopy if the aiming k-wire enters the tibia on the lateral side and comes out of the tibia at the medial side, and before overdrilling the k-wire the surgeon has to ensure that the k-wire comes out of the tibia at the medial side anterior to the tendon of the posterior tibial muscle. Figure 6 shows the comparison of preoperative (left) and postoperative (right) CT scans revealing anatomic positioning (Figure 6F, H) and rotation (Figure 6J) of the distal fibula and indirect anatomic reduction of the fracture of the posterior malleolus (Figure 6D, F and H).
Figure 7 shows a syndesmotic InternalBraceTM for triple stabilization with an additional posterolateral screw. The 27-year-old male patient sustained a type C Maisonneuve ankle fracture during a mountain bike accident. The anterior syndesmosis was disrupted and the posterolateral malleolus was fractured. The high fibular fracture did not need osteosynthesis. In a first step, the posterior malleolus was directly refixed with a lag screw via a posterolateral approach (Figure 7A). Then the anterior syndesmosis was augmented with an InternalBraceTM after anatomic reduction of the distal fibula under direct view via an anterolateral approach (Figure 7B and C). And finally, the posterolateral screw fixation was augmented by a slightly posteriorly directed TightRope® inserted at a level just above the tibial incisura, resulting in a perfect anatomical positioning of the distal fibula, which initially had been highly unstable due to the Maisonneuve fracture (Figure 7D).
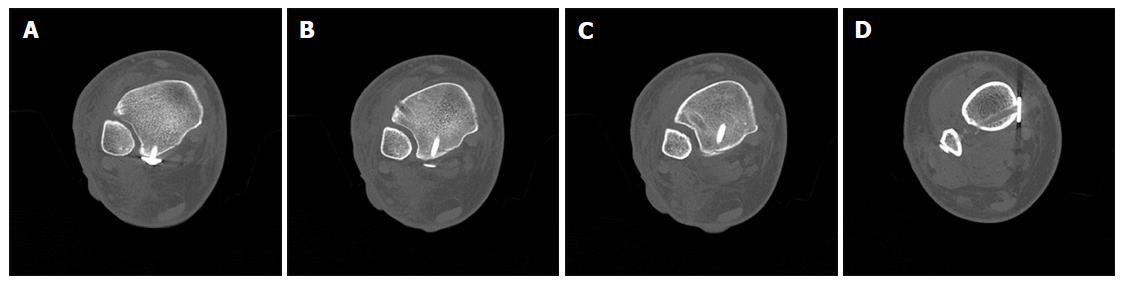
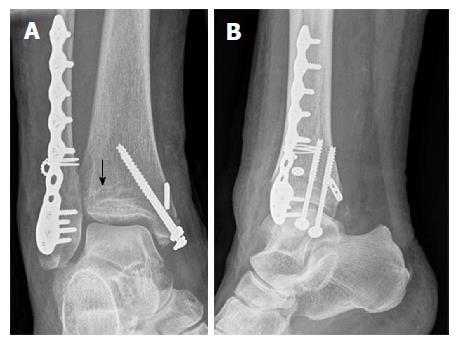
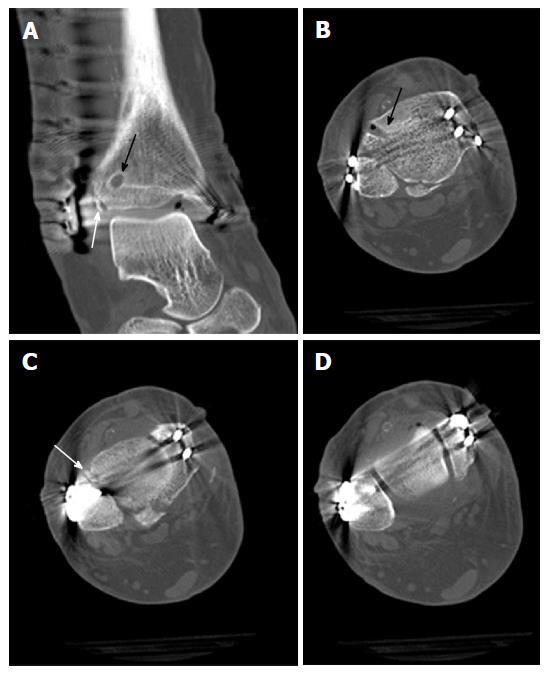
Moreover, we found that the syndesmotic InternalBraceTM technique is quite suitable for anatomic refixation and stabilization of displaced bony avulsion fragments too small for screw fixation. For example, Figure 8 shows X-rays of a 43-year-old male patient who sustained a trimalleolar dislocation fracture of the right ankle joint during a motor bike accident. After immediate closed reduction and cast immobilization, CT scans of the ankle showed tibial avulsion of the anterior tibiofibular ligament with dislocation of a bone fragment (black arrow) too small for screw fixation (Figure 9A). Furthermore, complete closed reduction was not possible due to a small bone fragment (white arrow) interposed between distal tibia and fibula (Figure 9B). Figure 9C and d reveal a displaced avulsion of a small fragment of the posterolateral malleolus. Due to the fracture pattern the patient was treated by open surgery (Figure 10).
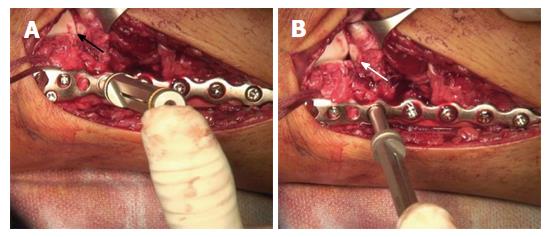
The distal fibula and the anterolateral ankle joint were exposed by a lateral approach. Note the small bony tibial avulsion fragment of the anterior tibiofibular ligament (black arrow) and the corresponding avulsion site (white arrow) at the tubercule de Chaput (Figure 10A). After reduction of the avulsion fragment the whole ligament proved to be intact (Figure 10B). After insertion of a FiberTape® about 4 mm proximal and medial of the avulsion site (Figure 10C) with a 4.75 mm SwiveLock®, standard osteosynthesis of the distal fibula was performed using an anatomic preformed locking plate (Arthrex®, Naples, United States). The reduced tibial avulsion fragment was then stabilized with a FiberTape® fixed by the tibial 4.75 mm SwiveLock® and by knots under the osteosynthesis plate.
Postoperative X-rays of the ankle showed anatomic reduction of the syndesmotic injury (Figure 11). The tibial bone tunnel for the InternalBraceTM is clearly visible (black arrow). Postoperative CT scans in Figure 12 revealed anatomic reduction of the tibial avulsion (white arrows) of the anterior tibiofibular ligament (Figure 12A and C) as well as anatomic reduction of the ankle mortise (Figure 12D). The tibial bone tunnel (black arrows) for the InternalBraceTM is clearly visible (Figure 12A and B).
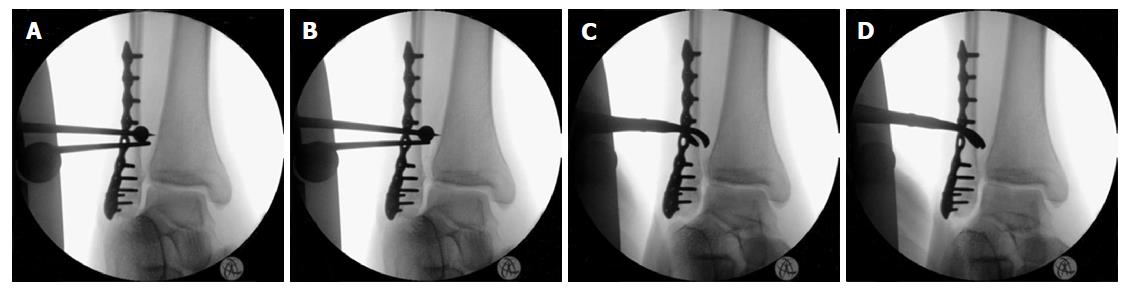
In the field of surgical treatment for unstable syndesmotic injuries, intraoperative testing of the stability of the syndesmosis still remains a major problem, and a normal classical hook test is not sufficient to exclude a clinically relevant syndesmotic instability[31]. Figure 13 shows an example of an intraoperative testing of syndesmotic stability after distal fibula plating of a type B ankle fracture: The classical hook test (Figure 13A and B) shows no lateral translation of the distal fibula while pulling the distal fibula laterally and pushing the distal tibia medially, indicating a normal result without syndesmotic instability. However, the same ankle joint shows relevant rotational instability of the anterior tibiofibular ligament (Figure 13C and D) indicating the need for surgical stabilization. Intraoperative testing of syndesmotic rotational stability under direct visualization after distal fibula plating using a mounted drill bit for locking screws is shown in Figure 14. The ankle joint shows relevant external rotational instability of the anterior tibiofibular ligament (Figure 14B) indicating the need for surgical stabilization. Note the clear opening of the star figure (white arrow) normally built by the tibiofibular, tibiotalar and talofibular joint lines (black arrow) by external rotation of the distal fibula (Figure 14B). Due to the well-known problems of fluoroscopic intraoperative stability testing of the syndesmosis reported in the current literature, an open visualization of the syndesmosis during the reduction maneuver and stability testing has recently been recommended[13]. Disadvantages of the described procedures are higher costs of implants and may be an increased surgical time compared to using classical syndesmotic screws.
Our preliminary clinical results indicate that anatomic reconstruction with rotational stabilization of the syndesmosis can be realized regularly by use of the reported new syndesmotic InternalBraceTM technique. A clinical trial for prospective evaluation of the functional outcomes has just been started at our hospital.
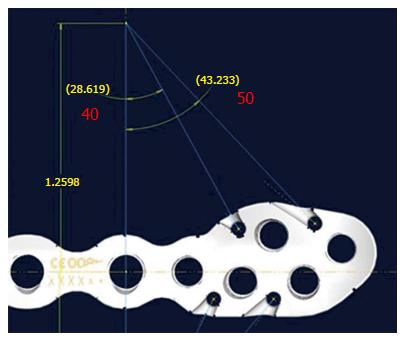
And - based on our positive results - a new syndesmosis plate is currently developed with added suture holes for easier mounting of the FiberTapes® for performing a syndesmotic InternalBraceTM.
Figure 15 shows the current prototype of the new syndesmosis plate (Arthrex®, Naples, United States) with suture holes at the distal part especially designed for augmentation of the anterior and posterior syndesmosis. The four suture holes are combined with a specially designed notch at the inside surface (Figure 16) exactly in line with the potential course of the inserted and tensioned FiberTape® to avoid impaired fitting of the plate to the distal fibula. As expected, this new syndesmosis plate will provide another step for improving anatomical stabilization of syndesmotic injuries.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: Germany
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Fanter NJ, Kutscha-Lissberg F, Newman SDS S- Editor: Song XX L- Editor: A E- Editor: Li D
| 1. | Hunt KJ. Syndesmosis injuries. Curr Rev Musculoskelet Med. 2013;6:304-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 2. | Jelinek JA, Porter DA. Management of unstable ankle fractures and syndesmosis injuries in athletes. Foot Ankle Clin. 2009;14:277-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Mackay GM, Blyth MJ, Anthony I, Hopper GP, Ribbans WJ. A review of ligament augmentation with the InternalBrace™: the surgical principle is described for the lateral ankle ligament and ACL repair in particular, and a comprehensive review of other surgical applications and techniques is presented. Surg Technol Int. 2015;26:239-255. [PubMed] |
| 4. | Bava E, Charlton T, Thordarson D. Ankle fracture syndesmosis fixation and management: the current practice of orthopedic surgeons. Am J Orthop (Belle Mead NJ). 2010;39:242-246. [PubMed] |
| 5. | van den Bekerom MP. Diagnosing syndesmotic instability in ankle fractures. World J Orthop. 2011;2:51-56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 55] [Cited by in RCA: 50] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 6. | Ovaska MT, Mäkinen TJ, Madanat R, Kiljunen V, Lindahl J. A comprehensive analysis of patients with malreduced ankle fractures undergoing re-operation. Int Orthop. 2014;38:83-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 56] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 7. | Hermans JJ, Beumer A, de Jong TA, Kleinrensink GJ. Anatomy of the distal tibiofibular syndesmosis in adults: a pictorial essay with a multimodality approach. J Anat. 2010;217:633-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 172] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 8. | Harris J, Fallat L. Effects of isolated Weber B fibular fractures on the tibiotalar contact area. J Foot Ankle Surg. 2004;43:3-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 63] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Ramsey PL, Hamilton W. Changes in tibiotalar area of contact caused by lateral talar shift. J Bone Joint Surg Am. 1976;58:356-357. [PubMed] |
| 10. | Knops SP, Kohn MA, Hansen EN, Matityahu A, Marmor M. Rotational malreduction of the syndesmosis: reliability and accuracy of computed tomography measurement methods. Foot Ankle Int. 2013;34:1403-1410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 11. | Gardner MJ, Demetrakopoulos D, Briggs SM, Helfet DL, Lorich DG. Malreduction of the tibiofibular syndesmosis in ankle fractures. Foot Ankle Int. 2006;27:788-792. [PubMed] |
| 12. | Naqvi GA, Cunningham P, Lynch B, Galvin R, Awan N. Fixation of ankle syndesmotic injuries: comparison of tightrope fixation and syndesmotic screw fixation for accuracy of syndesmotic reduction. Am J Sports Med. 2012;40:2828-2835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 200] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 13. | Sagi HC, Shah AR, Sanders RW. The functional consequence of syndesmotic joint malreduction at a minimum 2-year follow-up. J Orthop Trauma. 2012;26:439-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 305] [Cited by in RCA: 330] [Article Influence: 25.4] [Reference Citation Analysis (0)] |
| 14. | Egol KA, Pahk B, Walsh M, Tejwani NC, Davidovitch RI, Koval KJ. Outcome after unstable ankle fracture: effect of syndesmotic stabilization. J Orthop Trauma. 2010;24:7-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 177] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 15. | Weening B, Bhandari M. Predictors of functional outcome following transsyndesmotic screw fixation of ankle fractures. J Orthop Trauma. 2005;19:102-108. [PubMed] |
| 16. | Klitzman R, Zhao H, Zhang LQ, Strohmeyer G, Vora A. Suture-button versus screw fixation of the syndesmosis: a biomechanical analysis. Foot Ankle Int. 2010;31:69-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 97] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 17. | Coetzee J, Eberling P. Treatment of syndesmosis disruptions with TightRope fixation. Tech Foot Ankle Surg. 2008;7:196-201. |
| 18. | Teramoto A, Suzuki D, Kamiya T, Chikenji T, Watanabe K, Yamashita T. Comparison of different fixation methods of the suture-button implant for tibiofibular syndesmosis injuries. Am J Sports Med. 2011;39:2226-2232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 78] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 19. | Yoo JS, Yang EA. Clinical results of an arthroscopic modified Brostrom operation with and without an internal brace. J Orthop Traumatol. 2016;17:353-360. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 82] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 20. | Waldrop NE, Wijdicks CA, Jansson KS, LaPrade RF, Clanton TO. Anatomic suture anchor versus the Broström technique for anterior talofibular ligament repair: a biomechanical comparison. Am J Sports Med. 2012;40:2590-2596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 84] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 21. | Viens NA, Wijdicks CA, Campbell KJ, Laprade RF, Clanton TO. Anterior talofibular ligament ruptures, part 1: biomechanical comparison of augmented Broström repair techniques with the intact anterior talofibular ligament. Am J Sports Med. 2014;42:405-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 114] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 22. | Clanton TO, Viens NA, Campbell KJ, Laprade RF, Wijdicks CA. Anterior talofibular ligament ruptures, part 2: biomechanical comparison of anterior talofibular ligament reconstruction using semitendinosus allografts with the intact ligament. Am J Sports Med. 2014;42:412-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 63] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 23. | Acevedo J, Vora A. Anatomical reconstruction of the spring ligament complex: “internal brace” augmentation. Foot Ankle Spec. 2013;6:441-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 62] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 24. | Gilmer BB, Crall T, DeLong J, Kubo T, Mackay G, Jani SS. Biomechanical Analysis of Internal Bracing for Treatment of Medial Knee Injuries. Orthopedics. 2016;39:e532-e537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 58] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 25. | Lubowitz JH, MacKay G, Gilmer B. Knee medial collateral ligament and posteromedial corner anatomic repair with internal bracing. Arthrosc Tech. 2014;3:e505-508. |
| 26. | Heitmann M, Dratzidis A, Jagodzinski M, Wohlmuth P, Hurschler C, Püschel K, Giannakos A, Preiss A, Frosch KH. [Ligament bracing--augmented cruciate ligament sutures: biomechanical studies of a new treatment concept]. Unfallchirurg. 2014;117:650-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 27. | Heitmann M, Gerau M, Hötzel J, Giannakos A, Frosch KH, Preiss A. [Ligament bracing--augmented primary suture repair in multiligamentous knee injuries]. Oper Orthop Traumatol. 2014;26:19-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 28. | Smith JO, Yasen SK, Palmer HC, Lord BR, Britton EM, Wilson AJ. Paediatric ACL repair reinforced with temporary internal bracing. Knee Surg Sports Traumatol Arthrosc. 2016;24:1845-1851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 70] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 29. | McWilliam JR, Mackay G. The Internal Brace for Midsubstance Achilles Ruptures. Foot Ankle Int. 2016;37:794-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 30. | Cisneros LN, Reiriz JS. Management of acute unstable acromioclavicular joint injuries. Eur J Orthop Surg Traumatol. 2016;26:817-830. [PubMed] |
| 31. | Candal-Couto JJ, Burrow D, Bromage S, Briggs PJ. Instability of the tibio-fibular syndesmosis: have we been pulling in the wrong direction? Injury. 2004;35:814-818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 96] [Article Influence: 4.6] [Reference Citation Analysis (0)] |