Peer-review started: April 8, 2015
First decision: July 6, 2015
Revised: October 19, 2015
Accepted: November 3, 2015
Article in press: November 4, 2015
Published online: January 18, 2016
The most difficult aspect regarding treatment of the pediatric flatfoot is understanding who needs surgery, when it is necessary, and what procedure to be done. A thorough history, clinical examination, and imaging should be performed to guide the surgeon through an often complex treatment path. Surgical technique can be divided in three categories: Soft tissue, bony, and arthroereisis. This paper will describe the joint preserving techniques and their application to treat the pediatric flatfoot deformity.
Core tip: This paper discusses the authors’ approach to treating the pediatric flatfoot based on the their extensive clinical and surgical experience.
- Citation: Vulcano E, Maccario C, Myerson MS. How to approach the pediatric flatfoot. World J Orthop 2016; 7(1): 1-7
- URL: https://www.wjgnet.com/2218-5836/full/v7/i1/1.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i1.1
Pes planovalgus is a common condition in children. Despite being typically idiopathic, it may be associated with neuromuscular diseases, tarsal coalitions, and the accessory navicular syndrome. A common mistake that is made by surgeons is to consider the pediatric flatfoot as a small version of the adult flatfoot deformity. Indeed, the etiology and management of the deformity may be quite different. Often children are asymptomatic, and the main concern is the foot shape or the parents’ concerns for future impairment. The most important challenge for the physician is to distinguish a condition that may have a benign natural history from those that may cause disability if left untreated. The treatment to correct the flat foot deformity can be nonsurgical or surgical. We can divide the surgical techniques used to correct this deformity into three categories: Soft tissue, bony (osteotomies and arthrodesis), and arthroereisis[1]. It is unlikely that a soft tissue procedure alone can successfully correct the deformity. For such reason the addition of bony procedures and/or arthroereisis is warranted[2]. Subtalar arthroereisis has been introduced in recent years to treat flatfeet in the pediatric population. Arthroereisis is a joint-sparing technique that allows for correction of the deformity through proprioception and mechanical impingement[3,4].
As crucial as taking a good history is, it may be difficult to obtain information from young patients. They may refuse to cooperate or even minimize their symptoms. In these circumstances feedback from the parents may play an important role. History-taking should include pain, location, intensity, timing, functional problems, and alleviating/aggravating factors. A history of trauma or recurrent ankle sprains should also be specifically questioned[5].
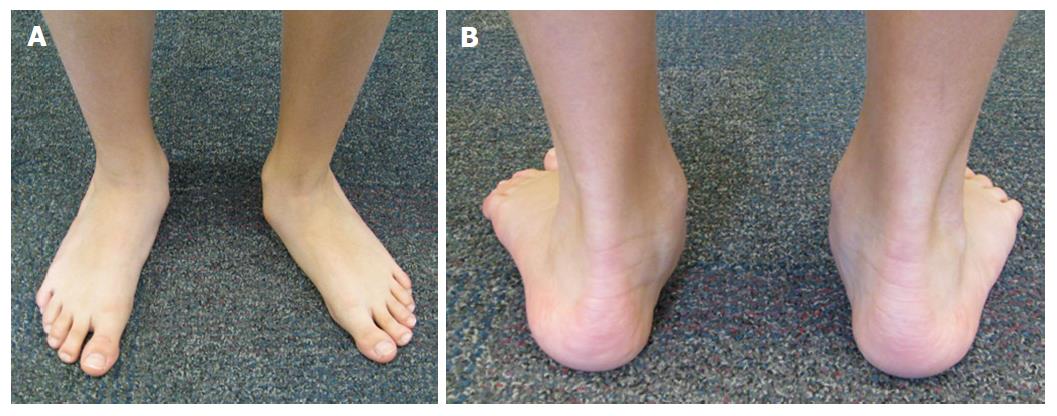
Patients must be examined both sitting and standing. Flatfoot deformity may be a dynamic deformity that requires weight bearing to be unmasked during clinical examination. The patient must be observed walking barefoot to assess instability and gait asymmetry. It is also important look at the young patient’s shoes to identify asymmetric wear of the soles. When the patient is weightbearing the physician should assess the presence (or absence) of the medial longitudinal arch, the prominence of the navicular, midfoot abduction (i.e., ‘‘too-many-toes’’ sign)[6], and heel alignment (Figure 1). Children will often present with a hindfoot valgus. Heel rises and manipulation of the calcaneus can confirm flexibility or rigidity of the deformity. A flexible flatfoot is one whose heel valgus can be corrected into neutral or slight varus. Fixed forefoot supination should also be evaluated with manual reduction of the hindfoot deformity, and be addressed in surgical planning by performing a plantar flexion osteotomy of the medial cuneiform.
Finally, Achilles and gastrocnemius contractures must always be identified. As the hindfoot deforms into valgus the Achilles complex is deviated laterally and shortened, leading to contracture that, in turn, aggravates the deformity.
Over time flexible feet in pediatric patients will become more rigid. This may occur in early adolescence or young adulthood. Adaptive changes inevitably take place in the hindfoot that alter its relationship with the forefoot. In order to keep the foot plantigrade, as the hindfoot everts and the calcaneus moves into valgus, the forefoot has to supinate. The Achilles tendon moves laterally with the calcaneus, and the axis of force on the subtalar joint changes, increasing the likelihood of a contracture of the gastrocnemius-soleus. As these structural changes take place, rigidity increases, consequently making the treatment more challenging.
Routine standard radiographs are not essential for diagnosis. However, they should always be ordered to more precisely assess uncharacteristic pain, decreased flexibility, and for surgical planning[7]. Weight-bearing anteroposterior (AP), lateral, and oblique views of the foot and the ankle should be obtained. Ankle radiographs may demonstrate signs of ankle instability or even overload and compromise of the medial physis. Hindfoot alignment may also be evaluated with Saltzman-view X-rays[8].
In case of an accessory navicular syndrome, an internal rotation oblique view is recommended in addition to the abovementioned views. A calcaneo-navicular coalition is best seen on the external rotation 45° oblique view, while a talonavicular coalition best visualized on the axial view[4,9].
The most commonly used radiographic measurement is Meary’s angle (or talar-first metatarsal angle): The angle formed by a line through the long axis of the talus and navicular in relation to the first metatarsal axis. A flatfoot demonstrates a negative Meary’s angle (apex plantar). On the lateral foot view one can measure the lateral talocalcaneal angle, the talometatarsal angle, and calcaneal pitch. On the AP foot view one can assess the talometatarsal angle and the talonavicular coverage angle[6].
Computed tomography (CT) scan and magnetic resonance imaging (MRI) are not necessary unless in patients with uncommon causes of flatfoot deformity[4].
The CT scan (possible weightbearing) represents the gold standard for the assessment of tarsal coalitions. While many patients with a tarsal coalition show some radiographic evidence (i.e., the ‘‘C’’ sign, talar beaking, or osseous bridging), these may sometimes be absent or unclear on standard X-rays[6]. Similarly, MRI provides additional information on fibrous coalitions as well as in cases of accessory navicular syndrome where the posterior tibial tendon could be compromised[5].
Young patients and their parents should be reassured that most flexible flatfeet are normal in childhood, and that the foot arch elevates over the first 10 years of age[10]. Although orthotics are diffusely prescribed to alleviate symptoms, to date there is no evidence supporting the use of orthotics to correct the deformity[11]. As a matter of fact some authors even suggest that insoles could cause more harm, leading to dependency and long-term negative psychological effects[11-13].
Orthotic supports and bracing may be appropriate for children who are symptomatic, although shoe wear modifications and other inexpensive modalities are quite appropriate for initial management. Custom molded orthotics or custom shoe wear should only be reserved for those that fail the aforementioned modalities. Stretching of a contracted Achilles tendon and physical therapy may offer symptomatic relief as well. The judicious use of nonsteroidal anti-inflammatories is a useful adjunct.
Indications to surgery and the type of surgery to be performed for the pediatric flatfoot continue to represent a challenge for surgeons. Surgical management is recommended in patients complaining of pain and dysfunction. While clinical and radiographic measurements can help stage a deformity, there are no guidelines that help orthopedic surgeons navigate through the different types of surgical procedures. Some patients may present with mild pain but severe deformity, while other may show mild deformity with severe pain.
The techniques available to correct flatfoot deformity can be divided into three procedure categories: Soft tissue, bony (osteotomies and arthrodesis), and arthroereisis.
Soft tissue procedures usually involve the Achilles tendon and/or the gastrocnemius, the posterior tibial tendon, and the peroneal tendons. The aim of these procedures is to balance the deforming forces. A gastrocnemius contracture is almost always present in children with a flatfoot and must be addressed with a gastrocnemius recession. The Silfverskiold test is a useful method to distinguish between a gastrocnemius contracture and an Achilles tendon contracture (the latter requiring a tendo Achilles lengthening, open or percutaneous). In children, the posterior tibial tendon is typically involved in the accessory navicular syndrome and requires an advancement following a modified Kidner procedure. As for the peroneals, we rarely intervene on them in the pediatric population. Only severe cases of flatfoot deformity with significant midfoot/forefoot abduction could require a peroneus brevis to peroneus longus transfer to allow good realignment and to prevent recurrence.
Arthroereisis should only be used to correct hindfoot valgus. Treatment results for children undergoing arthroereisis have been excellent, provided that the talonavicular joint is not significantly uncovered. The procedure seems to work very well in younger children who have predominantly heel valgus, presumably because they have more capacity for remodeling and adaptation of the forefoot. Once the talonavicular joint sags, particularly as seen on the lateral radiographic view, these feet seem to require more correction of the pronation deformity than a medial displacement calcaneal osteotomy can provide. If there is abduction deformity of the foot, with uncovering of the talonavicular joint, then neither the arthroereisis nor the medial displacement osteotomy are likely to be successful. The pediatric patient typically adapts to the arthroereisis very well, and the incidence of implant failure is low in this age-group. By contrast, in our experience with use of arthroereisis as an adjunctive procedure in a group of carefully selected adult patients, sinus tarsi pain warranted implant retrieval in approximately half of the cases. In children, however, implant removal has been necessary in less than 10% of the cases, probably because the foot adapts as it matures.
One cause for failure of the implant regardless of the age of the patient is inadequate correction of the forefoot. When the hindfoot is restored to a neutral position with the implant, some supination of the forefoot occurs. If the forefoot is able to compensate by increased plantar flexion of the first metatarsal, then a plantigrade foot is maintained. If the supination exceeds this adaptive ability, however, then in order to maintain the forefoot in a plantigrade position, the hindfoot has to evert during the foot flat phase of gait. This increased eversion then compresses the subtalar implant, causing pain. For this reason, an opening wedge osteotomy of the medial cuneiform is necessary if supination is excessive.
Intraoperatively, always start with the smallest trial sizers to get a feel for the position, location, and size of the tarsal canal. The range of motion of the subtalar joint should be carefully assessed with each incremental increase in the size of the dilator. The dorsiflexion of the foot now occurs more directly through the ankle joint, rather than in an oblique direction with a combined motion of dorsiflexion and eversion through the subtalar joint. If too large a prosthesis is inserted, motion of the subtalar joint will be limited. An important point here is that the goal of this operation is simply to limit excessive eversion of the hindfoot. If the prosthesis is too small, correction of hindfoot valgus will not be obtained, and dorsiflexion of the foot through the subtalar joint will persist. The appropriate sizer should limit abnormal subtalar joint eversion and allow for a few degrees of remaining eversion only.
Once the ideal size has been determined, the definitive implant is inserted to rest between the middle and the posterior facets. On the anteroposterior view of the foot, the lateral edge of the prosthesis should be 4 mm medial to the lateral edge of the talar neck.
The range of motion of the subtalar joint, especially eversion with the foot in neutral dorsiflexion, must be reassessed. In most young patients treated for a flexible flatfoot deformity, insertion of the implant is enough to provide appropriate correction (Figure 2). The forefoot should be plantigrade, and no excessive supination of the forefoot should be present after hindfoot correction. If fixed forefoot supination is present, an opening wedge osteotomy of the medial cuneiform is an excellent procedure to correct any residual forefoot supination after correction of the hindfoot.
The initial concept of mechanically altering the axis or position of the calcaneus to better normalize deformity was first described by Gleich[14] in 1893. However, it was Koutsogiannis who first recognized that sliding the calcaneus medially improves outcomes in flexible pes planus[15].
The medial displacement calcaneal osteotomy (MDCO) is a powerful procedure to correct hindfoot valgus. The procedure not only restores the mechanical tripod of the heel with respect to the forefoot, but also medializes the insertion of the Achilles tendon relative to the axis of the subtalar joint[16,17].
The MDCO requires approximately 10 to 12 mm of translation (about 50% of the calcaneal width). While a dorsal translation must always be avoided, a mild plantar translation of the posterior tuberosity is often desirable to increase the calcaneal pitch angle. Once the displacement has been completed, the choice of fixation is dependent on skeletal maturity. If the physis is closed or reaching skeletal maturity, the construct can be stabilized with one 6.5-mm cannulated screw. If skeletally immature with significant growth remaining, the osteotomy can be stabilized with smooth pin fixation. Once the hindfoot is corrected, attention is turned to the forefoot. Depending on the amount of deformity, additional procedures may be added.
A painful accessory navicular is almost always associated with a flatfoot of variable degree. The symptoms associated with this condition result from the disruption of the synchondrosis between the navicular and the accessory bone. As the synchondrosis is stressed, disruption of the attachment of the accessory navicular and thus of the posterior tibial tendon occurs. Another source of pain comes from pressure in the shoe secondary to an uncorrected pronated flatfoot.
Various degrees of deformity and flexibility of the hindfoot are associated with the accessory navicular. A painful accessory bone almost always requires surgical treatment. In addition to addressing the abovementioned condition, additional procedures are often required to correct the foot alignment. Such procedures may include a MDCO, lateral column lengthening, subtalar arthroereisis, medial cuneiform osteotomy, or Achilles tendon lengthening/gastrocnemius recession.
We prefer treating the painful os naviculare with a modified Kidner procedure and advancement of the posterior tibial tendon on the navicular using a suture anchor. However, large accessory bones can be treated with resection of the synchondrosis and fixation with a screw. This has the advantage of preserving the insertion of the posterior tibial tendon on the bone, thus providing quicker recovery and stronger repair (Figure 3). Nonetheless, the disadvantage is the potential for continued swelling on the medial aspect of the foot as well as nonunion. These complications can be decreased by generously shaving both the os naviculare and the medial pole of the navicular, to decrease the bulk of the bone on its medial aspect and expose bleeding subchondral bone.
Intraoperatively, the accessory navicular must be completely excised, taking care not to injure the posterior tibial tendon and the underlying spring ligament. Next, the medial border of the navicular must be resected until flush with the anterior edge of medial cuneiform to decrease the medial bulk. Once the bones have been modeled, the posterior tibial tendon is advanced with the foot in mild overcorrection (plantarflexion and inversion). In young children the tendon can be anchored into the bone using a sharp needle inserted directly into the navicular bone, the cuneiform, or both. In the older children and adolescents, the use of a suture anchor is preferable. In our experience most patients require additional procedures to correct the foot. These include a gastrocnemius recession, an arthroereisis or a MDCO. These procedures should be done prior to the modified Kidner, as they will affect the tension on the posterior tibial tendon. Conversely, a cotton osteotomy to correct the fixed forefoot supination (often required in our experience) can be performed before or after the modified Kidner.
Sangeorzan et al[18] presented a cadaveric study in 1993 using the Evans procedure and found significant improvements in talonavicular coverage, talometatarsal angle, and calcaneal pitch angle.
The indications for lengthening of the lateral column (LCL) are quite specific and include a flexible foot that is amenable to correction. In this context, correction implies that the talonavicular joint can be covered with the procedure. The lateral column lengthening procedure does not work well if the foot is stiff.
The hindfoot alignment can be corrected with either a MDCO (to correct the heel valgus) or a lateral column lengthening calcaneus osteotomy. The latter will not only correct the midfoot abduction, but also push the heel medially. A LCL through a calcaneocuboid fusion is not recommended in children.
We make a short incision over the sinus tarsi. The osteotomy is made 1 cm posterior to the calcaneocuboid joint. The position of the osteotomy is marked with a guide pin and checked fluoroscopically. Osteotomy cuts are then made on either side of the guide pin and completed through the neck of the calcaneus. A common mistake is to make the osteotomy too far posterior, causing subtalar impingement. With the osteotomy distracted, the position of the talus relative to the navicular is checked clinically and radiographically, and once positioning is corrected, the appropriate-size auto/allograft is prepared. The size of the graft in children is about 8 to 10 mm on the lateral aspect of the graft, and should be trapezoid shaped as opposed to triangular (Figure 4). Fixation of the graft is not necessary, unless grossly unstable. Potential complications of LCL include lateral foot pain, nonunion, sinus tarsi impingement (typically when the osteotomy is too posterior), and a slight dorsal subluxation of the distal calcaneus (creating prominence of the anterior process of the calcaneus subcutaneously).
The opening wedge medial cuneiform osteotomy is an excellent adjunct to many hindfoot correction procedures, including lateral column lengthening, MDCO, excision of an accessory navicular, and placement of an arthroereisis implant. Determining the exact indications for this procedure is not easy, because the capacity of the forefoot for plantar flexion subsequent to the calcaneus osteotomy cannot be predicted. As a general rule, if the forefoot is supinated more than 15 degrees, we add a cotton osteotomy.
The incision is made along the dorsal margin of the medial cuneiform A K-wire is inserted from dorsal to plantar in the middle of the cuneiform, directed slightly proximally. There is a tendency to make the saw cut too vertically and not along the axis of the cuneiform. If this placement is exaggerated, the osteotomy may enter the metatarsocuneiform joint. The osteotomy should be completed up to the base of the cuneiform without violating the plantar cortex that will act as a hinge. Once the cut is completed, a laminar spreader is inserted into the osteotomy, and as it is distracted, the first metatarsal is plantarflexed, correcting the metatarsal declination angle. A structural bone graft (allograft or autograft) is then carefully tamped into the osteotomy. Contrarily to the LCL graft which should be trapezoid shaped, the cotton osteotomy graft should be triangular. Most times the graft measures between 5 and 7 mm across at the dorsal base of the graft. The osteotomy is very stable once the graft is wedged into place, and fixation is not necessary.
Tarsal coalitions can determine a rigid flatfoot deformity. Historically, coalition resection was indicated for coalitions inferior to 50% of the middle facet, whereas fusion was indicated for coalitions greater than 50%. We disagree with this philosophy and always try to perform a complete resection of any coalition. The decision is guided by the age of the patient, the severity of the deformity, the degree of stiffness, and the presence of arthritis. A CT scan (possibly weightbearing) is always indicated not only to assess the coalition, but also to identify other coalitions which are present in almost 50% of patients. The most common cause of a rigid flatfoot in a child is a talocalcaneal coalition of the middle facet. The senior author recently presented a new technique to precisely excise the coalition[19]. A 5-cm incision is created inferior to the posterior tibial tendon, over the coalition. The coalition is identified in the interval between the flexor digitorum longus and flexor hallucis longus. The soft tissue and periosteal flap over the coalition must be elevated away from the coalition to ensure adequate visualization. Next, a 1-cm incision is made over the sinus tarsi soft spot. A guide pin (part of a system for subtalar arthroereisis) is inserted through the tarsal canal and pushed between the coalition and the posterior facet. Then, the coalition is exposed by inserting the arthroereisis sizing device over the guide wire in a lateral to medial direction through the sinus tarsi. The arthroereisis sizer will open up the coalition as it is inserted. In cases of a solid, complete coalition, a fracture occurs along the margins of the coalition. Resection can then be carried out using osteotomes and rongeurs. As the coalition is resected, the sizing guide can be advanced, further opening the subtalar joint and the coalition. With the arthroereisis guide in place, the coalition can be fully resected, allowing visualization of articular cartilage around the resected coalition.
Pediatric flat foot deformity should be classified as rigid vs flexible. A combination of soft tissue and bony procedures is almost always necessary to correctly realign the foot and prevent recurrence. Too often surgeons ignore the power of a gastrocnemius recession and a cotton osteotomy when performing reconstructive surgery. A thorough examination of the foot both preoperatively and intraoperatively will help unmask a gastrocnemius contracture and/or a fixed forefoot supination.
P- Reviewer: Graham ME, Kelesidis T
S- Editor: Song XX L- Editor: A E- Editor: Li D
| 1. | Mosca VS. Flexible flatfoot in children and adolescents. J Child Orthop. 2010;4:107-121. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 178] [Cited by in F6Publishing: 159] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 2. | Roth S, Sestan B, Tudor A, Ostojic Z, Sasso A, Durbesic A. Minimally invasive calcaneo-stop method for idiopathic, flexible pes planovalgus in children. Foot Ankle Int. 2007;28:991-995. [PubMed] [Cited in This Article: ] |
| 3. | Fernández de Retana P, Alvarez F, Viladot R. Subtalar arthroereisis in pediatric flatfoot reconstruction. Foot Ankle Clin. 2010;15:323-335. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 4. | Usuelli FG, Montrasio UA. The calcaneo-stop procedure. Foot Ankle Clin. 2012;17:183-194. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 5. | Dare DM, Dodwell ER. Pediatric flatfoot: cause, epidemiology, assessment, and treatment. Curr Opin Pediatr. 2014;26:93-100. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 44] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 6. | Kwon JY, Myerson MS. Management of the flexible flat foot in the child: a focus on the use of osteotomies for correction. Foot Ankle Clin. 2010;15:309-322. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | De Pellegrin M, Moharamzadeh D, Strobl WM, Biedermann R, Tschauner C, Wirth T. Subtalar extra-articular screw arthroereisis (SESA) for the treatment of flexible flatfoot in children. J Child Orthop. 2014;8:479-487. [Cited in This Article: ] |
| 8. | Saltzman CL, el-Khoury GY. The hindfoot alignment view. Foot Ankle Int. 1995;16:572-576. [PubMed] [Cited in This Article: ] |
| 9. | Nogarin L. Retrograde endorthesis. Ital J Pediatr Othop. 1997;13:34-39. [Cited in This Article: ] |
| 10. | Wenger DR, Mauldin D, Speck G, Morgan D, Lieber RL. Corrective shoes and inserts as treatment for flexible flatfoot in infants and children. J Bone Joint Surg Am. 1989;71:800-810. [PubMed] [Cited in This Article: ] |
| 11. | Helfet AJ. A new way of treating flat feet in children. Lancet. 1956;270:262-264. [PubMed] [Cited in This Article: ] |
| 12. | Rao UB, Joseph B. The influence of footwear on the prevalence of flat foot. A survey of 2300 children. J Bone Joint Surg Br. 1992;74:525-527. [PubMed] [Cited in This Article: ] |
| 13. | Driano AN, Staheli L, Staheli LT. Psychosocial development and corrective shoewear use in childhood. J Pediatr Orthop. 1998;18:346-349. [PubMed] [Cited in This Article: ] |
| 14. | Gleich A. Beitrag zur operative Plattfussbehandlung. Arch Klin Chir. 1893;46:58-62. [Cited in This Article: ] |
| 15. | Koutsogiannis E. Treatment of mobile flat foot by displacement osteotomy of the calcaneus. J Bone Joint Surg Br. 1971;53:96-100. [PubMed] [Cited in This Article: ] |
| 16. | Nyska M, Parks BG, Chu IT, Myerson MS. The contribution of the medial calcaneal osteot-omy to the correction of flatfoot deformities. Foot Ankle Int. 2001;22:278-282. [PubMed] [Cited in This Article: ] |
| 17. | Sung IH, Lee S, Otis JC, Deland JT. Posterior tibial tendon force requirement in early heel rise after calcaneal osteotomies. Foot Ankle Int. 2002;23:842-849. [PubMed] [Cited in This Article: ] |
| 18. | Sangeorzan B, Mosca V, Hansen S. Effect of calcaneal lengthening on relation-ships among the hindfoot, midfoot, and forefoot. Foot Ankle. 1993;14:136-141. [PubMed] [Cited in This Article: ] |
| 19. | Humbyrd CJ, Myerson MS. Use of a cannulated guide in talocalcaneal coalition resection: technique tip. Foot Ankle Int. 2015;36:225-228. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |