Published online Jan 18, 2020. doi: 10.5312/wjo.v11.i1.10
Peer-review started: March 20, 2019
First decision: June 11, 2019
Revised: August 30, 2019
Accepted: November 6, 2019
Article in press: November 6, 2019
Published online: January 18, 2020
Processing time: 304 Days and 13.3 Hours
In rotator cuff repair surgery, the double-row technique is widely performed. Studies have shown that with increased contact area and pressure between tendon and bone interface, better healing is promoted.
To assess the different suture configurations with the double-row technique and how this influences the contact area of the rotator cuff tendon to bone.
This was a controlled laboratory study where identical tears were created in 24 fresh porcine shoulders over a 1.5 cm × 2.5 cm infraspinatus insertion footprint. Double-row repair techniques, with 3 to 4-suture anchors in different configurations (2 medial, 2 lateral vs 2 medial, 1 lateral vs 1 medial, 2 lateral), were employed for three control groups. Each group consisted of eight shoulders with identical repair configurations. Footprint contact areas of the repaired tendon against the tuberosity were determined using pressure sensitive Fujifilm placed between the tendon and tuberosity.
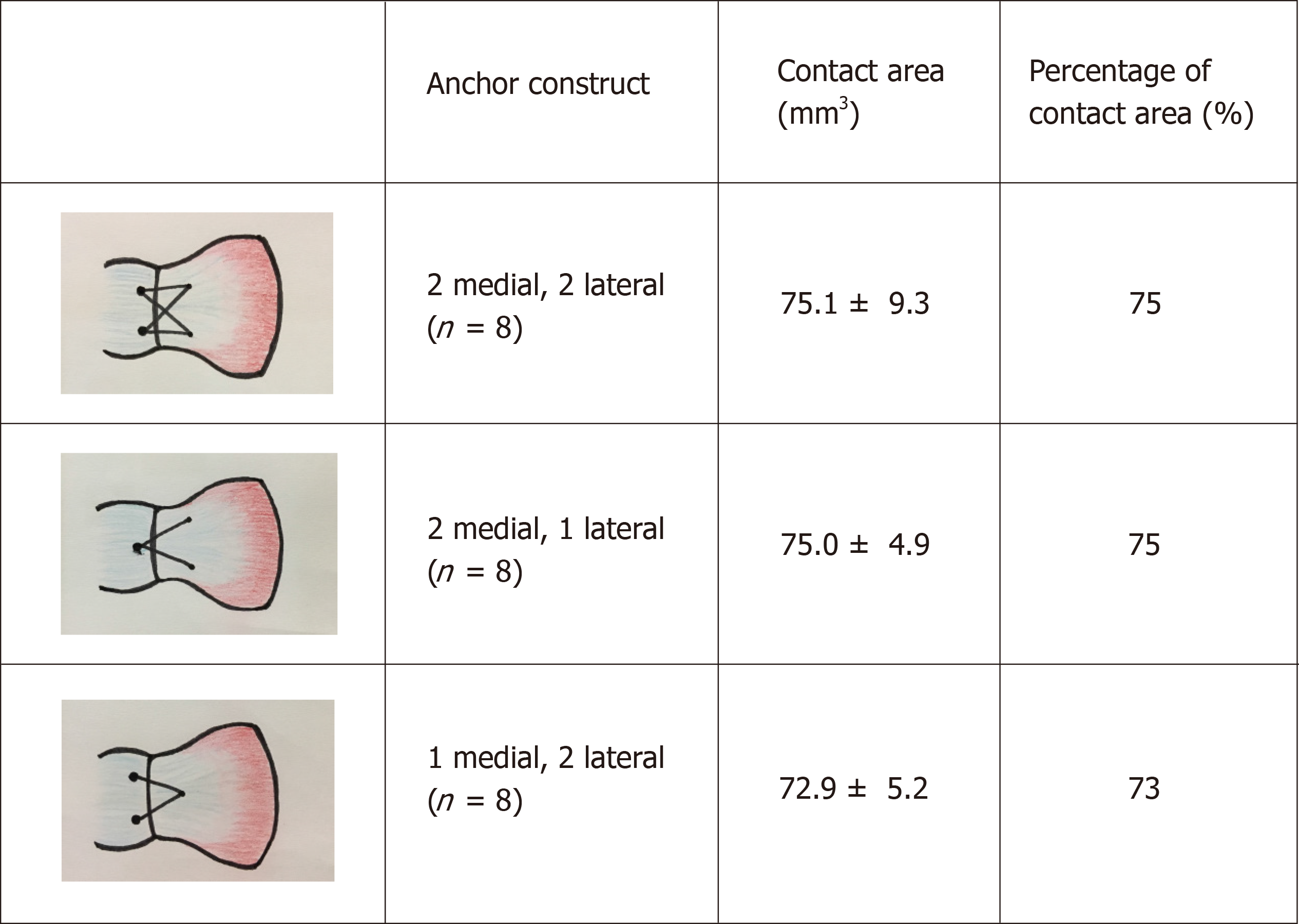
The mean contact area between tendon and insertion footprint from the imprinted Fujifilm was obtained using computer software. The contact area measured from a standard 4-suture anchor double row repair was 75.1 ± 9.3 mm2, whereas areas obtained for the 2 lateral - 1 medial and 2 medial - 1 lateral anchor configurations were 72.9 ± 5.2 mm2 and 75.0 ± 4.9 mm2 respectively. No statistical significance was noted between the three groups.
In the technique of double-row repair, using a 3-suture anchor configuration may offer a non-inferior alternative to the standard 4-anchor construct in terms of efficacy. This may also result in overall cost reduction and shorter surgical time.
Core tip: We report our first results derived from a porcine model investigating different suture configurations in the double-row technique, and how this influences the contact area of the rotator cuff tendon to bone. This study demonstrates for the first time that there is no statistical difference in tendon to bone contact area when using a 3 or 4-suture anchor construct, suggesting that the 3-anchor construct may be a comparable alternative to the standard 4-anchor construct in terms of efficacy.
- Citation: Ng SHA, Tan CHJ. Double-row repair of rotator cuff tears: Comparing tendon contact area between techniques. World J Orthop 2020; 11(1): 10-17
- URL: https://www.wjgnet.com/2218-5836/full/v11/i1/10.htm
- DOI: https://dx.doi.org/10.5312/wjo.v11.i1.10
Rotator cuff tendon tears are one of the commonest sources of pain in the shoulder. Studies have shown that the incidence can range from 5% to 40%[1-3] of the population. Patients with symptoms often present with chronic pain and limitation in range of motion of the shoulder. Such tears are usually detected via ultrasonography or magnetic resonance imaging. Surgery is often recommended if the tear causes persistent pain or if there is profound loss of joint function. There are several repair techniques that the surgeon may opt for, depending on the size of the tear and the degree of tendon retraction. One commonly performed technique is the double-row repair.
Post-surgical healing of the repaired tendon is strongly correlated to the patient’s functional outcome[4]. Therefore, much research has involved identifying strategies to help enhance tendon healing and to maintain integrity of the repair during the post-operative period. If the tendon is completely or partially detached from the tuberosity, the surgeon will face the challenge of ensuring adequate healing between the rotator cuff tendon and the tuberosity of the humerus. One strategy to counter this would be to maximise the contact area between tendon and bone[4,5]. The underlying principle is that a greater area of contact of tendon-to-bone will result in a greater chance of tendon healing[4-8]. This, in turn, leads to improved mechanical strength and function of the repaired tendon[5-7,9].
Differences between the double and single-row repair for rotator cuff tears have been widely discussed. In a review by Roth et al[10], the double-row repair was shown to have superior characteristics in terms of footprint contact area, tendon-to-bone compression and eventual load-to-failure rate. Similarly, tendon gap formation and re-tear rates are lower in double-row repairs compared to single-row repairs. It is interesting to note that no difference in clinical outcomes was observed between both groups; however, this could possibly be attributed to the relatively short follow up of 2 years[10-12]. The double-row repair still appears to be the favoured technique amongst surgeons.
The double-row repair is traditionally performed using four suture anchors – two are placed in the most medial aspect of the exposed humeral tuberosity footprint, forming the medial row; the other two anchors are placed at the superior or lateral aspect of the greater tuberosity, depending on the extent of exposed tuberosity. Whilst many studies have looked into the biomechanical properties and outcomes of single and double-row repair, few have actually compared the different types of double-row repair techniques, particularly in the area of tendon-to-bone contact.
A distinction should be made between coverage vs compression of the rotator cuff tendon to the footprint insertion. Coverage refers to the area of tendon-to-bone contact, while compression refers to the pressure of the tendon against the bone. While both coverage and compression are possible contributory factors in tendon healing, our study has a preliminary focus on coverage, with planned future studies focusing on compression to support our findings.
Our study aims to investigate the relationship between different double-row suture anchor configurations and the tendon-to-bone contact area in the repair of medium-sized rotator cuff tendon tears in a porcine cadaver model. We hypothesis that employing different double-row suture anchor configurations in rotator cuff repairs will not influence tendon to bone contact area.
Twenty-four fresh porcine shoulders (mean age, 24 wk; range, 22-25 wk) without gross evidence of rotator cuff pathology were used for this study. We chose to use the infraspinatus tendon in a porcine model for a few reasons. Fukuhara et al[13] concluded that the geometric and biomechanical properties of the porcine infraspinatus tendon were similar to those of the human supraspinatus tendon, mainly in terms of thickness, footprint area, ultimate load-to-failure and linear stiffness. The porcine infraspinatus tendon is also easily identified. In addition, the bone surface where the infraspinatus tendon inserts into is relatively flat, making it ideal for secure placement of the pressure-sensitive film. In our city, fresh porcine shoulders are also easily available.
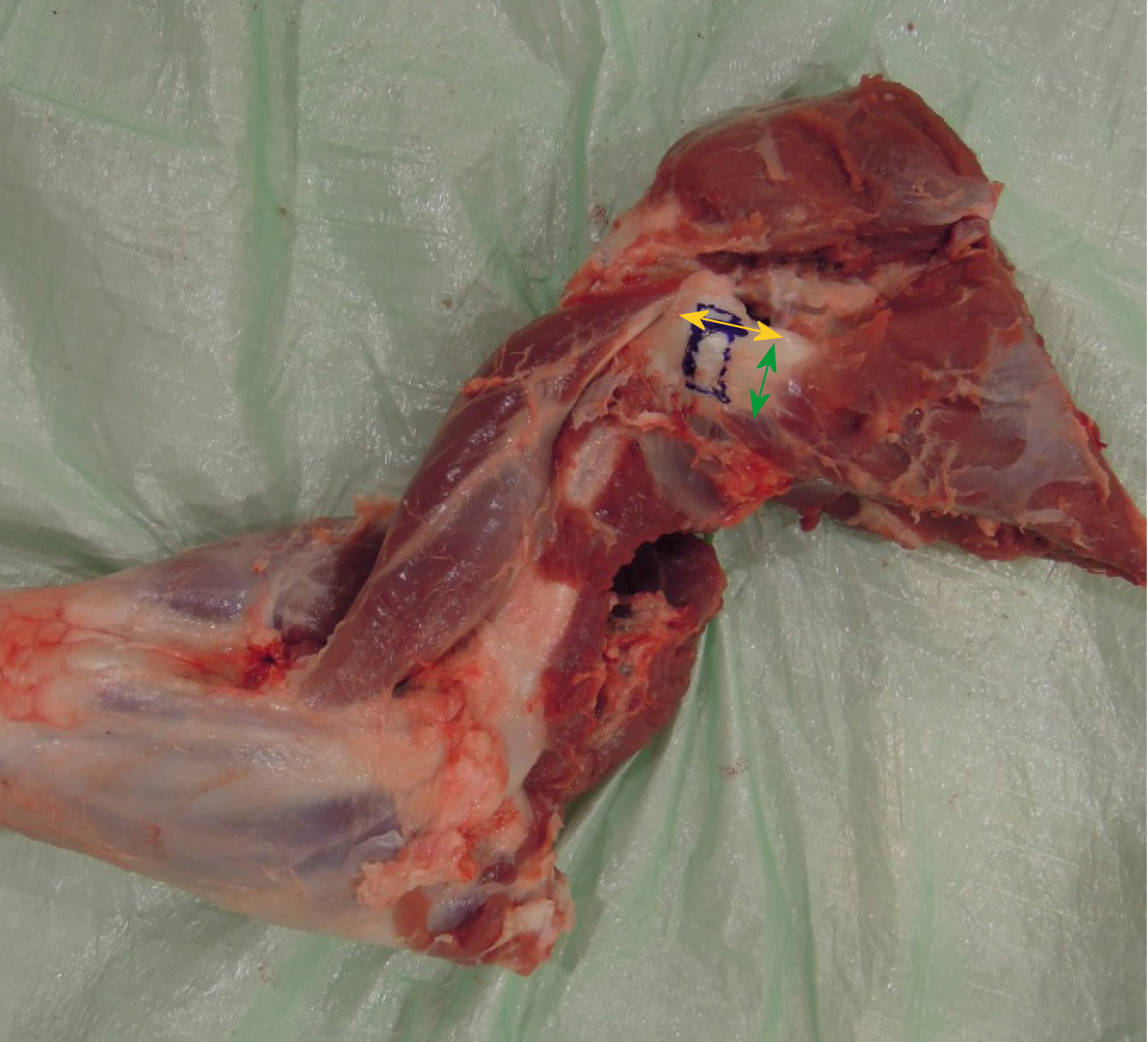
Soft tissue was carefully dissected from the scapula and the proximal humerus, preserving the infraspinatus muscle and tendon (Figure 1). To create a tear in the infraspinatus tendon, a 1.5 cm × 2.5 cm rectangular full thickness segment of the infraspinatus tendon was sharply detached from its distal footprint. This was repeated in all specimens to create identical tears. The underlying bone surface was then prepared using a fine rasp to ensure an even surface for placement of subsequent pressure sensitive films.
We used identical pressure-sensitive films (Prescale Ultra Super Low Pressure type, Fujifilm, Tokyo, Japan) to determine the contact areas between the repaired infraspinatus tendons and the tuberosities. The pressure sensitivity range for this film was 0.2 to 0.6 MPa. Identical 10 mm × 10 mm pressure-sensitive films were cut to conform to the exposed bone on the tuberosities. Each film was fully sealed with adhesive tape prior to placement to prevent contamination.
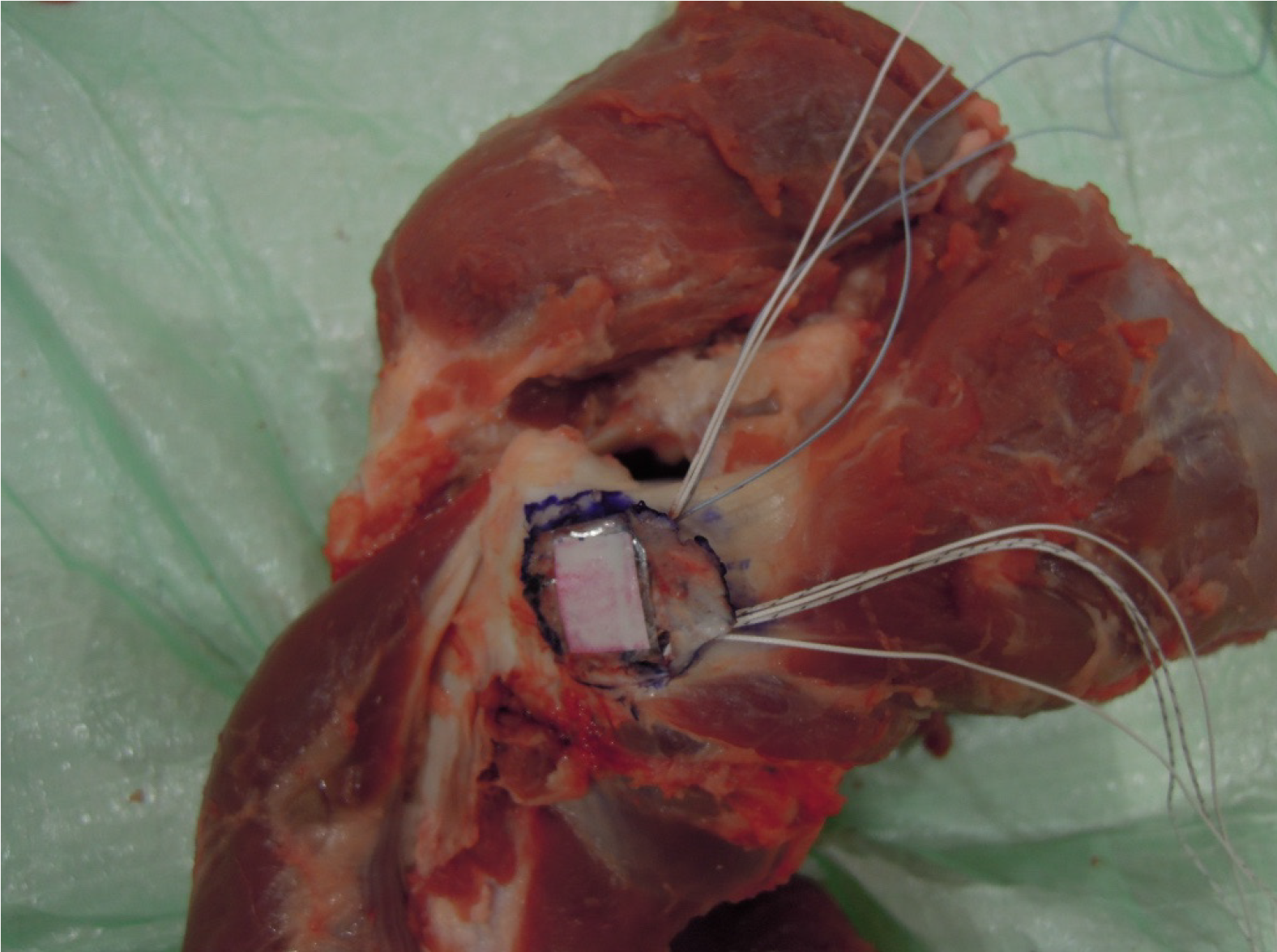
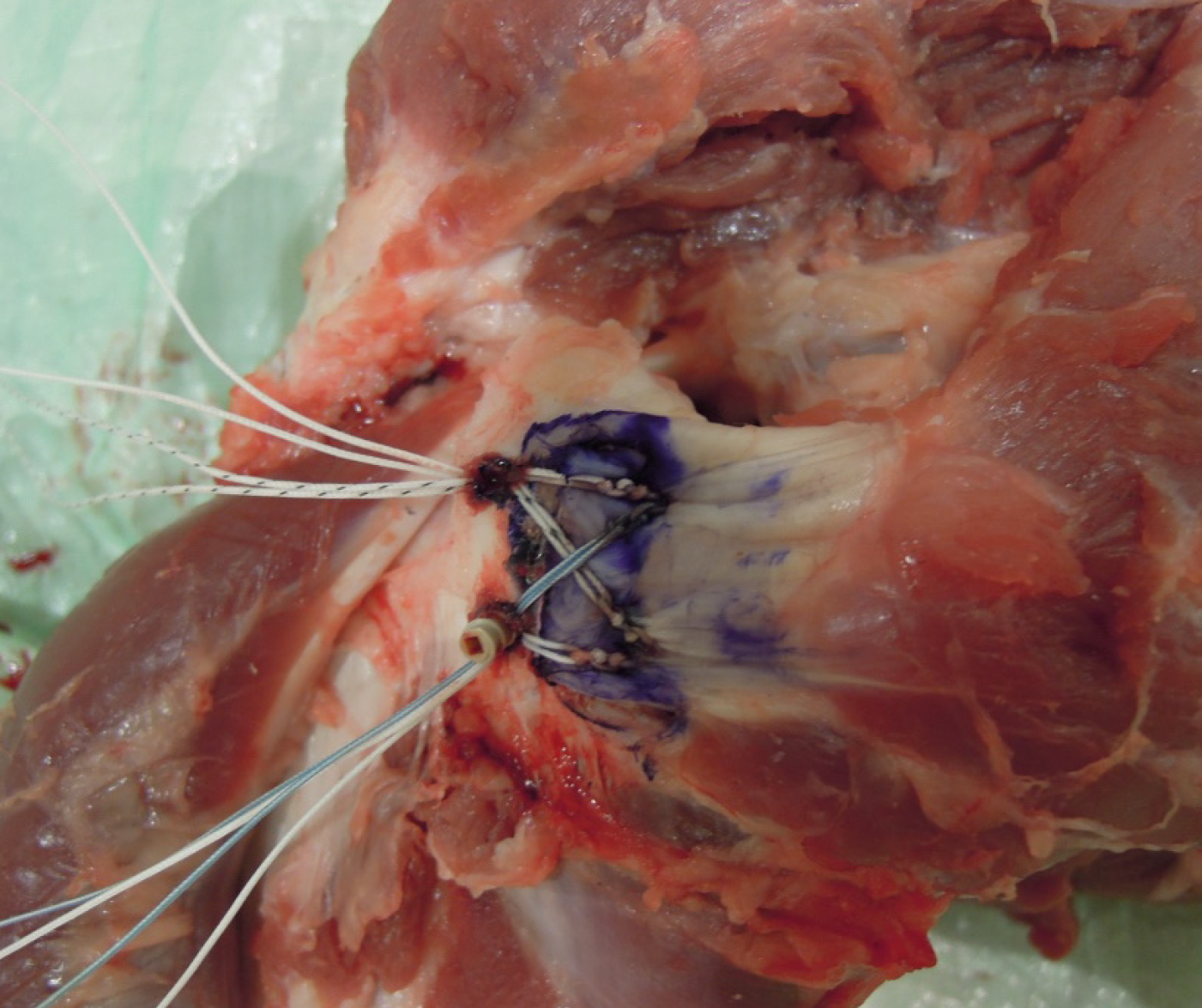
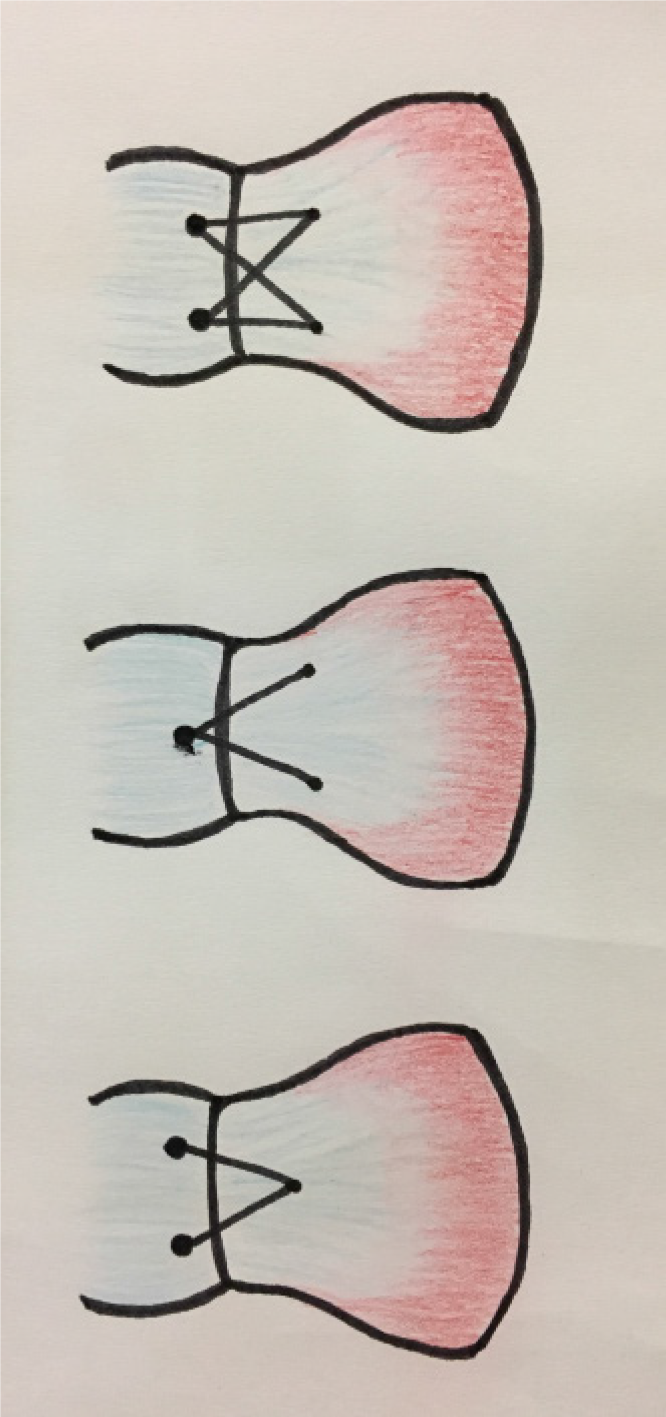
The 24 porcine shoulders were divided into three groups of eight specimens. Double-row repair was performed for all three groups. The technique for Group 1 (G1) consisted of the standard two medial suture anchors - two lateral knotless anchors configuration, forming a suture bridge. The detached infraspinatus tendon was reflected off bone, and two symmetrically placed holes measuring 2 mm in diameter were created 1.5 cm apart from each other using a surgical awl at the medial edge of the reflected tendon. Similarly, two holes were placed over the lateral edge of bone where the tendon was detached, forming the lateral row. A 5.5 mm Bio-Corkscrew (Arthrex, Inc., Naples, FL, United States) with two #2 fibrewire sutures (four strands) attached was then inserted at a 45° angle in both medial holes to a depth marked on the suture anchor device. The sutures were then passed through the edge of the tendon in a knotless fashion. The sealed pressure sensitive film was placed over the centre of the footprint and secured in place with adhesive glue (Figure 2). One pair of sutures from each medial row suture anchor was crossed with the corresponding pair in the other medial anchor and, together with the uncrossed pair of sutures, secured to one lateral row knotless anchor each (5.5 mm Bio-Swivelock, Arthrex, Inc.) (Figure 3). Upon completion of the repair, a 60-s interval was maintained before the sutures were cut sharply with a scalpel. Careful measures were taken to avoid placing additional pressure on the soft tissue. The pressure sensitive film was then carefully removed from the footprint for further analysis. All dissections and repairs were carried out by a single surgeon under the supervision of the senior author to minimise inter-specimen technique variability.
For Group 2 (G2), two medial suture anchors and one lateral knotless anchor were inserted. The medial and lateral anchors were similarly connected by a suture bridge. The technique and instruments used were identical to G1, apart from the placement of only one lateral knotless anchor, which was inserted at equidistance from each lateral row knotless anchor.
Group 3 (G3) consisted of one medial suture anchor - two lateral knotless anchors repair connected by a suture bridge. The technique and instruments used were once again identical to G1, except that only a single medial anchor was used. Placement of this anchor was inserted at equidistance from each medial row suture anchor (Figure 4).
After the film was retrieved from the footprint, the adhesive tapes were carefully removed. The digital image of each pressure sensitive film imprint was obtained at a resolution of 600 pixels/inch using a digital scanner. The area marked out in dark pink represented good contact from the overlying repaired tendon, while areas in light pink or white indicated little or no contact. Image J, an imaging software, was used to analyse the digital images in grey scale (Figure 5A and B). The imprinted contact area on the pressure sensitive film was digitized and subsequently computed using the imaging software.
Statistical analyses were performed using the Kruskal-Wallis test, with the repair construct as the factor and contact area as the measured variable. Results from the three groups of double-row rotator cuff repair techniques were analysed. Significant differences were noted where P < 0.05.
Our results showed that the mean contact area (± SD) between the infraspinatus tendon and the underlying tuberosity for G1 (2 medial - 2 lateral) was 75.1 ± 9.3 mm2. The mean contact area for G2 (2 medial - 1 lateral) was 75.0 ± 4.9 mm2, while the mean contact area for G3 (1 medial - 2 lateral) was 72.9 ± 5.2 mm2.
Our results showed that there was no statistically significant difference between the mean contact areas of the treatment groups (P = 0.82) (Figure 6). This was an interesting finding as we were expecting to see a greater tendon contact area in the 2 medial - 2 lateral group (G1).
The double-row repair has been described in the literature to be superior in restoring footprint dimensions as compared to the single-row repair[6,9,14]. In maximising the contact area between the rotator cuff tendon and bone with a double-row repair, the healing potential is optimized[4-6,8,15]. Apreleva et al[5] described a possible improved biological healing process with a larger area of contact between the rotator cuff tendon and bone by increasing the size of the newly formed insertion site, to allow more fibres to participate in the healing process. Fealy et al[6] believes that vigorous tendon mobilization, combined with a broad surface area to allow for bone-tendon healing, provides a suitable environment for repair of rotator cuff tears, including large ones. The hypothesis is that with a larger footprint contact area, more tendon fibres are exposed to bone, which in turn results in improved healing potential[16]. A study by Park et al[4] has further supported this, concluding that by maximising the contact area between the tendon and tuberosity at the rotator cuff footprint, the biological healing process is enhanced, which leads to improvement of mechanical strength and function of the repaired tendon. A number of ongoing and recent studies are describing new techniques in an effort to achieve stronger fixation strength and to increase the rotator cuff footprint contact area. There is paucity of literature to show that contact area is not important in terms of rotator cuff repair and healing.
We acknowledge that both coverage and compression are contributory factors in tendon healing[8,17-19]. While the role of contact area is supported by literature, the effects of compression – which is the pressure experienced between the tendon and bone – may not be that clear. Multiple studies have shown that optimizing pressure between the tendon and bone can be beneficial for healing[8,17-19]. Weiler et al[19] showed that a high pressure environment created with the use of interference fit fixation was beneficial for direct osseous bridging between the tendon and bone using autologous Achilles tendon. However, microscopically, the effects of high tendon to bone pressure at the footprint may be at the expanse of vascularity. Further studies in this area, together with a follow-up study focusing on compression, could potentially further validate the use of the 3-anchor construct.
While many studies have looked at the contact area between single vs double-row repairs, few or no studies to our knowledge have analysed the contact area characteristics between double-row repairs performed using 3 and 4-suture anchors. Our study has shown that the double-row technique not only results in good footprint contact area (> 70% compression at a defined area of footprint), but also that the use of either a 3 or 4-suture anchor construct yields similar tendon-to-bone contact area in the repair of a medium-sized tear, no larger than 1.5 cm × 2.5 cm. This potentially favours the use of just three anchors. With the use of less hardware, the chance of creating a high-pressure environment at the expense of vascularity between tendon to bone may hypothetically be reduced. Further in-vivo studies will be needed to substantiate this.
In our institution, the cost of a suture anchor ranges between S$600 to S$900. By using one less anchor per patient (25% savings in terms of cost), it appears that the same result may be achieved while promising a potential reduction in healthcare costs in the long run. Additionally, by employing one less anchor, there is a significant reduction in the surgical time required to complete the double-row repair, which translates to the benefit of decrease in anaesthetic time. In our local context, patients’ bone sizes are generally smaller, which may further support the use of fewer suture anchors; the greater tuberosity in Asians may not be large enough for four anchors[20]. In a study conducted by Franceschi et al[21], they reported a statistically significant difference in operative time between the single-row and double-row repair (42 ± 18.9 min vs 65 ± 23.4 min, respectively). The increase in surgical time together with the higher cost of placing more anchors appear to make the use of the double-row repair less ideal than the single-row repair, especially for smaller (< 3 cm) tears. The use of a 3-anchor double-row construct is a potential solution to minimize these disadvantages, yet reaping its own benefits of maximizing footprint contact area and healing.
Our study has a few limitations. The first would be the small sample size, which is inherent to cadaveric studies. Secondly, the use of a porcine cadaveric model – while geometrically and biomechanically similar to humans – is still disadvantageous as compared to using a human cadaveric model due to the difference in anatomy. However, the effect of this limitation is reduced as contact area, instead of the healing process, was being measured. Additionally, our study did not make use of a tensiometer to gauge the tension of the repairs. The effect of this was minimised as much as possible by maintaining equal depths of all the suture anchors, to ensure uniform tension in all the repairs. Lastly, fresh tendons tears were used, which may not replicate the quality of the tendons in chronic tears. Perhaps further studies can be performed in human cadaveric specimens to quantify contact pressure and pull-out strength, to validate further the use of the 3-anchor construct.
In conclusion, the double-row repair technique is commonly employed for the surgical treatment of rotator cuff tears. Our study showed that there is no statistical difference in tendon-to-bone contact area when using a 3 or 4-suture anchor construct. This may potentially translate to shorter surgical times and lower healthcare costs with the use of fewer anchors without compromising tendon-to-bone healing of rotator cuff tears.
In rotator cuff repair surgery, the double-row technique is widely performed and remains one of the most commonly performed techniques. The double-row repair is traditionally performed using four suture anchors.
This study proves that the use of a 3-suture anchor construct is non-inferior to that of a 4-suture anchor construct in terms of footprint contact area. The use of a 3-suture anchor construct may potentially translate to significant reductions in surgical and anaesthetic times, as well as a reduction in healthcare costs in the long run. Future research studying the contact pressure and pull-out strength can be undertaken to validate further the use of a 3-suture anchor construct as a non-inferior alternative to the 4-suture anchor construct while achieving the abovementioned benefits.
The objective of our study was to demonstrate for the first time that there is no statistical difference in tendon to bone contact area when using a 3 or 4-suture anchor construct. By demonstrating so, it has introduced the possibility that the 3-anchor construct may be a comparable alternative to the standard 4-anchor construct in terms of efficacy. This study can be used in conjunction with future research comparing contact pressure and pull-out strength to further validate the use of 3-anchor construct over the traditional 4-anchor construct.
Twenty-four fresh porcine shoulders without gross evidence of rotator cuff pathology were used. The use of a porcine model was chosen due to a previous study reporting the geometric and biomechanical similarities between the porcine infraspinatus tendon and the human supraspinatus tendon. Identical tears were created in these porcine shoulders over a 1.5 cm × 2.5 cm infraspinatus insertion footprint. Double-row repair techniques, with 3 to 4-suture anchors in different configurations, were employed for three control groups. Each group consisted of eight shoulders with identical repair configurations. Footprint contact areas of the repaired tendon against the tuberosity were determined using pressure sensitive Fujifilm placed between the tendon and tuberosity.
The study demonstrated for the first time that there is no statistical difference in tendon-to-bone contact area when using a 3 or 4-suture anchor construct. This study can be used in conjunction with future research comparing contact pressure and pull-out strength to further validate the use of 3-anchor construct over the traditional 4-anchor construct.
The study found for the first time that there is no statistical difference in tendon-to-bone contact area when using a 3 or 4-suture anchor construct. It has hence introduced the possibility that the 3-anchor construct may be a comparable alternative to the traditional 4-anchor construct in terms of efficacy. This may potentially translate to shorter surgical times and lower healthcare costs with the use of fewer anchors without compromising tendon-to-bone healing of rotator cuff tears.
This study introduces a new, alternative technique to the traditional 4-anchor construct that has been performed for years. This study can be used in conjunction with future research comparing contact pressure and pull-out strength to validate further the use of 3-anchor construct over the traditional 4-anchor construct.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: Singapore
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Anand A, Francesco SM, Papachristou G S-Editor: Wang JL L-Editor: Filipodia E-Editor: Liu MY
| 1. | Minagawa H, Yamamoto N, Abe H, Fukuda M, Seki N, Kikuchi K, Kijima H, Itoi E. Prevalence of symptomatic and asymptomatic rotator cuff tears in the general population: From mass-screening in one village. J Orthop. 2013;10:8-12. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 255] [Cited by in F6Publishing: 320] [Article Influence: 29.1] [Reference Citation Analysis (0)] |
| 2. | Oliva F, Osti L, Padulo J, Maffulli N. Epidemiology of the rotator cuff tears: a new incidence related to thyroid disease. Muscles Ligaments Tendons J. 2014;4:309-314. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Sambandam SN, Khanna V, Gul A, Mounasamy V. Rotator cuff tears: An evidence based approach. World J Orthop. 2015;6:902-918. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 102] [Cited by in F6Publishing: 97] [Article Influence: 10.8] [Reference Citation Analysis (5)] |
| 4. | Park MC, Cadet ER, Levine WN, Bigliani LU, Ahmad CS. Tendon-to-bone pressure distributions at a repaired rotator cuff footprint using transosseous suture and suture anchor fixation techniques. Am J Sports Med. 2005;33:1154-1159. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 187] [Cited by in F6Publishing: 192] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 5. | Apreleva M, Ozbaydar M, Fitzgibbons PG, Warner JJ. Rotator cuff tears: the effect of the reconstruction method on three-dimensional repair site area. Arthroscopy. 2002;18:519-526. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 260] [Cited by in F6Publishing: 218] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 6. | Fealy S, Kingham TP, Altchek DW. Mini-open rotator cuff repair using a two-row fixation technique: outcomes analysis in patients with small, moderate, and large rotator cuff tears. Arthroscopy. 2002;18:665-670. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 106] [Cited by in F6Publishing: 77] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 7. | Lee KW, Yang DS, Lee GS, Ma CH, Choy WS. Clinical outcomes and repair integrity after arthroscopic full-thickness rotator cuff repair: suture-bridge versus double-row modified Mason-Allen technique. J Shoulder Elbow Surg. 2018;27:1953-1959. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 8. | Park JY, Lhee SH, Choi JH, Park HK, Yu JW, Seo JB. Comparison of the clinical outcomes of single- and double-row repairs in rotator cuff tears. Am J Sports Med. 2008;36:1310-1316. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 175] [Cited by in F6Publishing: 178] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 9. | Lo IK, Burkhart SS. Double-row arthroscopic rotator cuff repair: re-establishing the footprint of the rotator cuff. Arthroscopy. 2003;19:1035-1042. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 306] [Cited by in F6Publishing: 249] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 10. | Roth KM, Warth RJ, Lee JT, Millett PJ, ElAttrache NS. Arthroscopic Single-Row Versus Double-Row Repair for Full-Thickness Posterosuperior Rotator Cuff Tears: A Critical Analysis Review. JBJS Rev. 2014;2:01874474-201402070-00007. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Millett PJ, Warth RJ, Dornan GJ, Lee JT, Spiegl UJ. Clinical and structural outcomes after arthroscopic single-row versus double-row rotator cuff repair: a systematic review and meta-analysis of level I randomized clinical trials. J Shoulder Elbow Surg. 2014;23:586-597. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 196] [Cited by in F6Publishing: 188] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 12. | Nicholas SJ, Lee SJ, Mullaney MJ, Tyler TF, Fukunaga T, Johnson CD, McHugh MP. Functional Outcomes After Double-Row Versus Single-Row Rotator Cuff Repair: A Prospective Randomized Trial. Orthop J Sports Med. 2016;4:2325967116667398. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 13. | Fukuhara T, Mihata T, Horinouchi T, Yasui K, Asai S, Watanabe C, Kinoshita M. Biomechanical Propaties of Porcine Infraspinatus Tendon. Katakansetsu. 2008;32:361-363. [DOI] [Cited in This Article: ] |
| 14. | Gazielly DF, Gleyze P, Montagnon C. Functional and anatomical results after rotator cuff repair. Clin Orthop Relat Res. 1994;43-53. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 137] [Cited by in F6Publishing: 111] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 15. | Deprés-Tremblay G, Chevrier A, Snow M, Hurtig MB, Rodeo S, Buschmann MD. Rotator cuff repair: a review of surgical techniques, animal models, and new technologies under development. J Shoulder Elbow Surg. 2016;25:2078-2085. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 108] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 16. | Ostrander RV, Smith J, Saper M. Triple-Row Modification of the Suture-Bridge Technique for Arthroscopic Rotator Cuff Repair. Arthrosc Tech. 2016;5:e1007-e1013. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Park MC, ElAttrache NS, Tibone JE, Ahmad CS, Jun BJ, Lee TQ. Part I: Footprint contact characteristics for a transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elbow Surg. 2007;16:461-468. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 313] [Cited by in F6Publishing: 287] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 18. | Park MC, Tibone JE, ElAttrache NS, Ahmad CS, Jun BJ, Lee TQ. Part II: Biomechanical assessment for a footprint-restoring transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elbow Surg. 2007;16:469-476. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 315] [Cited by in F6Publishing: 281] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 19. | Weiler A, Hoffmann RF, Bail HJ, Rehm O, Südkamp NP. Tendon healing in a bone tunnel. Part II: Histologic analysis after biodegradable interference fit fixation in a model of anterior cruciate ligament reconstruction in sheep. Arthroscopy. 2002;18:124-135. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 20. | Cong E, Walker MD. The Chinese skeleton: insights into microstructure that help to explain the epidemiology of fracture. Bone Res. 2014;2:14009. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 21. | Franceschi F, Ruzzini L, Longo UG, Martina FM, Zobel BB, Maffulli N, Denaro V. Equivalent clinical results of arthroscopic single-row and double-row suture anchor repair for rotator cuff tears: a randomized controlled trial. Am J Sports Med. 2007;35:1254-1260. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 351] [Cited by in F6Publishing: 305] [Article Influence: 17.9] [Reference Citation Analysis (0)] |