Published online Jan 18, 2019. doi: 10.5312/wjo.v10.i1.33
Peer-review started: September 12, 2018
First decision: October 19, 2018
Revised: November 17, 2018
Accepted: December 17, 2018
Article in press: December 17, 2018
Published online: January 18, 2019
Processing time: 128 Days and 18.2 Hours
No dynamic technique, such as tendon transfer, has been described for scapular winging due to levator scapulae or rhomboid major and minor palsies resulting from an isolated dorsal scapular nerve injury. Thus, we evaluated how the contralateral trapezius compound osteomuscular flap transfer would work in stabilizing lateral scapular winging, and the case is reported here. A literature review was also conducted, and articles relevant to the case are presented.
A 37-year-old male patient who had sustained an isolated dorsal scapular nerve injury underwent reconstructive surgery using the contralateral trapezius compound osteomuscular flap transfer technique to treat scapular winging and the consequent pain, and to restore function from the shoulder impairment. As a result, the involved shoulder showed an improved Constant-Murley score, from 19.5% to 81.88%.
Contralateral trapezius osteomuscular flap transfer succeeded in stabilizing scapular winging in this case, improving shoulder function and affording pain relief.
Core tip: This report describes a case of scapular winging as a result of dorsal scapular nerve injury. Only few cases of winged scapula due to rhomboid paralysis are reported in the literature. Although scapular winging can seriously impair shoulder function, no dynamic techniques have been described to treat this condition. This case reveals that contralateral trapezius compound osteomuscular flap transfer can successfully stabilize lateral scapular winging due to a dorsal scapular nerve injury, while improving shoulder function and affording pain relief.
- Citation: Gil-Álvarez JJ, García-Parra P, Anaya-Rojas M, Martínez-Fuentes MDP. Contralateral trapezius transfer to treat scapular winging: A case report and review of literature. World J Orthop 2019; 10(1): 33-44
- URL: https://www.wjgnet.com/2218-5836/full/v10/i1/33.htm
- DOI: https://dx.doi.org/10.5312/wjo.v10.i1.33
Winging of the scapula was first described over 200 years ago[1]. It remains a cause of serious impairment of upper limb function, decreasing shoulder range of motion and strength; ultimately, it affects activities such as lifting, pushing and pulling heavy objects[2], not to mention the pain associated with doing so[3,4]. In addition to these functional restrictions, it affects the shape of the back and can become an aesthetic and psychological issue[5].
To understand this pathology, the anatomy of the shoulder must be fully known. The minor rhomboid muscle originates from the cervical spinous processes 6-7 and the major rhomboid muscle from the thoracal spinous processes 1-4. The major and minor rhomboid muscles are both innervated by the dorsal scapular nerve which originates from C5 or C5 and C6[6], inserts at the scapula medially, presses the scapula on the thorax and pulls it to the spine. This anatomy preconditions for retroversion and internal rotation in antagonization of the serratus anterior muscle which is innervated by the long thoracic nerve which originates from C5, C6 and C7[7], and inserts at the scapula medially. This anatomy preconditions for anteversion and external rotation. With rhomboid muscle insufficiency, elevation of the arm is still possible but for full movement both preconditions have to be met.
The other involved muscles (function) in scapular girdle motion are: Pectoralis major muscle (anteversion, internal rotation); pectoralis minor muscle (adduction, internal rotation); coracobrachialis muscle (anteversion); deltoid muscle (abduction up to 90°, strongest anteversion with its clavicular part, internal rotation with its clavicular part, retroversion and external rotation with its spinal part); subscapular muscle (strongest internal rotation); supraspinatus muscle (external rotation and additionally abduction); infraspinatus muscle (strongest external rotation); teres major muscle (strongest retroversion, internal rotation); teres minor muscle (external rotation); latissimus dorsi muscle (adduction, retroversion, internal rotation); and, trapezoid muscle (elevation/abduction of more than 90° with its descending part). The trapezoid muscle is innervated by the spinal accessory nerve, a cranial nerve which originates from the first five to six spine segments before entering the cranium through the foramen magnum (Ramus externus or Radices spinales) and is then accompanied by its cranial part that originates from the oblongata medulla (Ramus internus or Radices craniales). Both parts run together with the vagal nerve, through the jugular foramen, before innervating the sternocleidomastoid muscle and the trapezoid muscle. Contributions to trapezius innervation by the cervical plexus have also been described but findings thus far suggest it has limited significance[8].
Many etiologies can cause scapular winging. Most cases, however, are attributed to neurological lesions. These include long thoracic, spinal accessory and dorsal scapular nerve injuries, which are linked to this problem due to paralysis of the serratus anterior, trapezius and/or rhomboid muscles, respectively. Normally, the synchronized actions of these muscles push the medial border of the scapula against the thoracic wall; dysfunction of any of them will consequently lift the medial border of the scapula away from the back. In any case, dorsal scapular nerve lesions are quite rare and the literature contains few case reports of winged scapula due to rhomboid paralysis in particular[9-11].
The direction of displacement of the inferior angle of the scapula determines whether winging will be medial or lateral. The former is due to a lack of function of the serratus anterior muscle, and the latter to a lack of function of the trapezius and/or rhomboid muscles. Winging can be also classified as primary, secondary, or voluntary. Causes of primary winging are neurological injuries, usually involving the long thoracic nerve, the accessory nerve or the dorsal scapular nerve. These occur in association with tumor on the ribs or scapula or malunited fractures of the scapula, as well as following the rupture or absence of periscapular muscles. Secondary winging is due to glenohumeral and subacromial disorders. Voluntary winging of the scapula is very rare and psychological factors play an important role[12].
Scapular winging presents a diagnostic challenge, as evidenced by the many patients that are initially misdiagnosed[13,14]. Electromyography of the serratus anterior, trapezius and rhomboid muscles is useful to inform the diagnosis and reveal which muscles are involved as well as the degree of denervation[15,16]. Electromyographic testing typically shows resting denervation potentials, decreased motor unit recruitment, and polyphasic motor unit potentials during volitional activity[17,18] if any recovery is taking place. Imaging studies are rarely diagnostic but should be performed to ascertain any structural abnormalities and aid in ruling out other diagnoses[10,15,19,20].
Transfers of several muscles have been described to treat scapular winging. In this sense, transfer of the rhomboid major and minor has been suggested to treat scapular winging due to spinal accessory nerve injury and trapezius paralysis. Transfer of the pectoralis major is widely used when scapular winging is present following a long thoracic nerve injury and serratus anterior paralysis. To the best of our knowledge, there are no reports of any muscle transfer for primary scapular winging due to an isolated dorsal scapular nerve injury.
With written informed consent, we report herein the unusual case of an adult patient who developed scapular winging on the right side due to a dorsal scapular nerve injury. We chose to treat the case with contralateral trapezius transfer, and obtained approval from the local Ethics Committee (No. JGA-TCEA-2017). The surgical technique provided successful restoration of scapulothoracic joint function and pain relief, and may be a useful means by which to treat scapular winging due to an isolated dorsal scapular nerve injury.
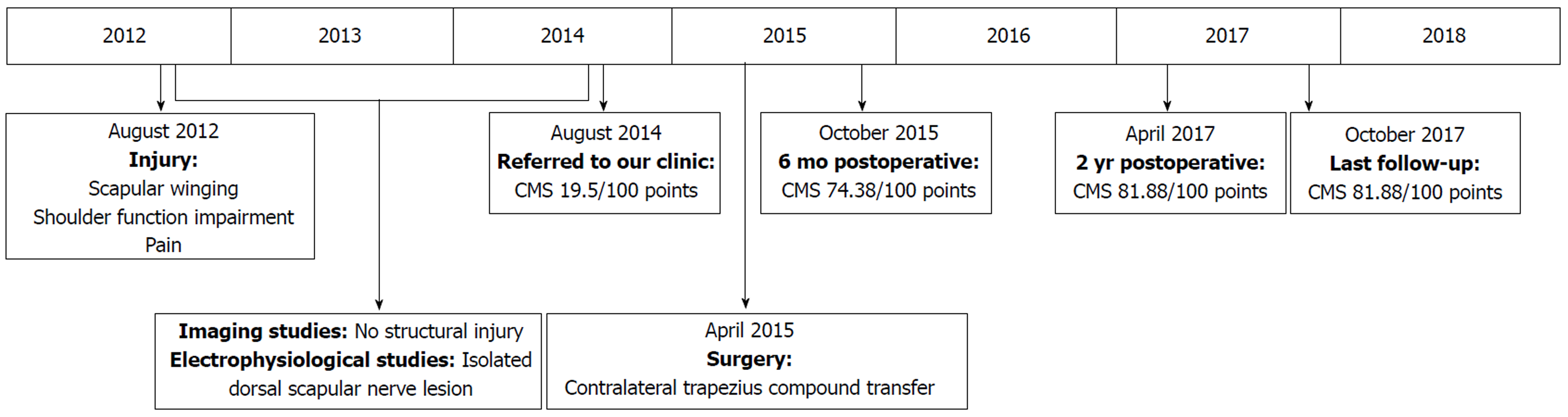
A 37-year-old male patient was referred to our clinic with a history of right shoulder indirect injury sustained 2 years prior (Figure 1). He worked carrying heavy marble stones. The injury had occurred when he was trying to prevent one from falling. He reported having made a sudden arm movement, followed by tremendous effort to hold the stone. Following the incident, the patient experienced right scapular winging, shoulder function impairment, and pain.
Clinical examination revealed scapular winging at rest and during both passive and active shoulder flexion (Figure 2), together with decreased active shoulder movement on the right side, having 60º flexion and 45º abduction (Figure 3). In terms of shoulder rotations, the patient was able to put his hands behind his head with elbows forward but was unable to reach his back. The patient underwent evaluation of overall function of the shoulder using the Constant-Murley score (CMS; a 100-point scale composed of several parameters that define the level of pain, function, range of motion and strength[21]). The patient’s preoperative CMS was 19.5.
Imaging studies (plain X-rays and magnetic resonance imaging) did not reveal any structural injury. Electrophysiological studies showed an isolated dorsal scapular nerve lesion and proper function of other nerves, such as the long thoracic and spinal nerves.
Dorsal scapular nerve injury.
The case was considered to be an irreparable nerve lesion given the time elapsed between nerve injury and the patient’s referral to our clinic. Nerve surgery was obviated and contralateral trapezius compound osteomuscular flap transfer was proposed to correct the scapular winging.
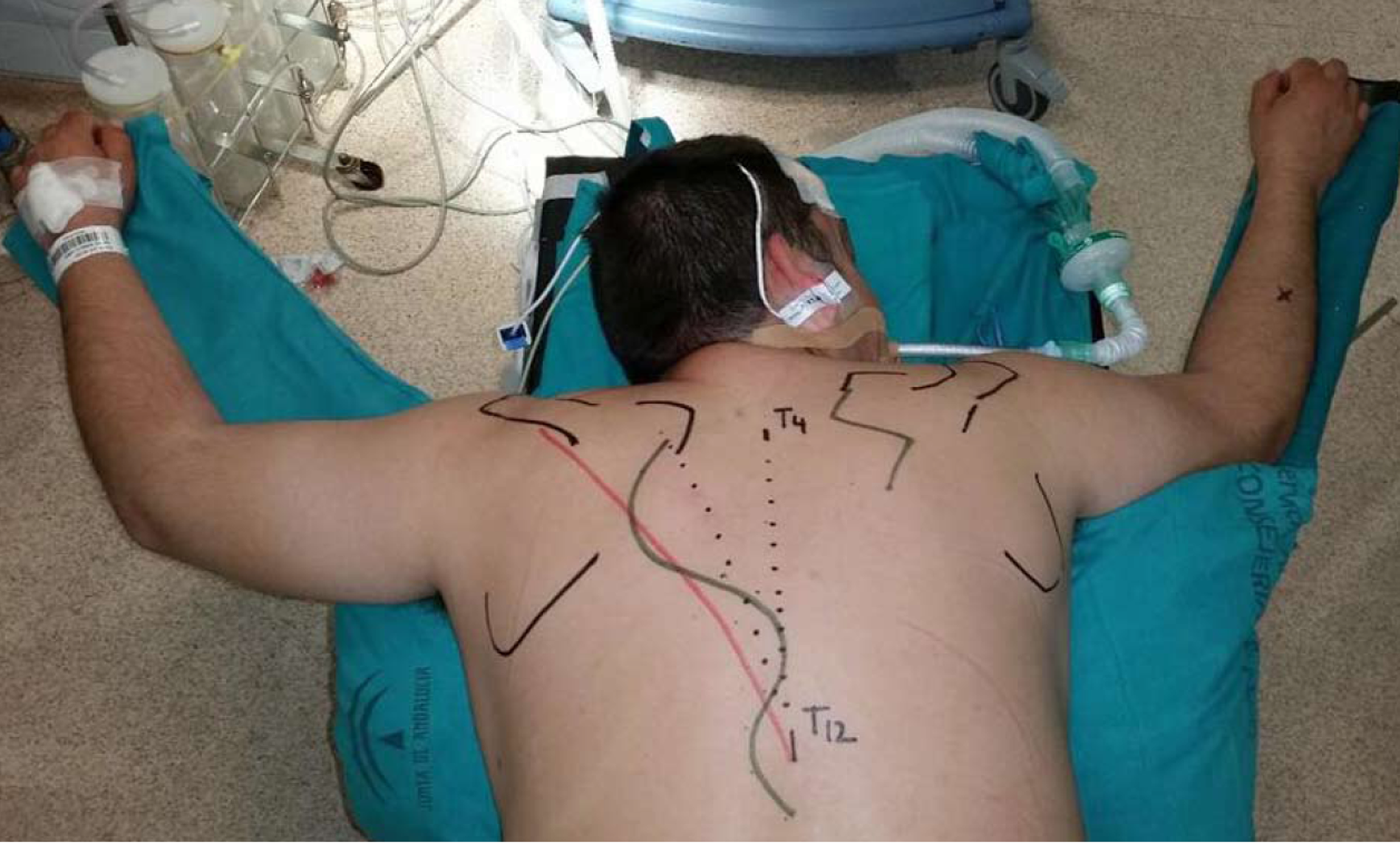
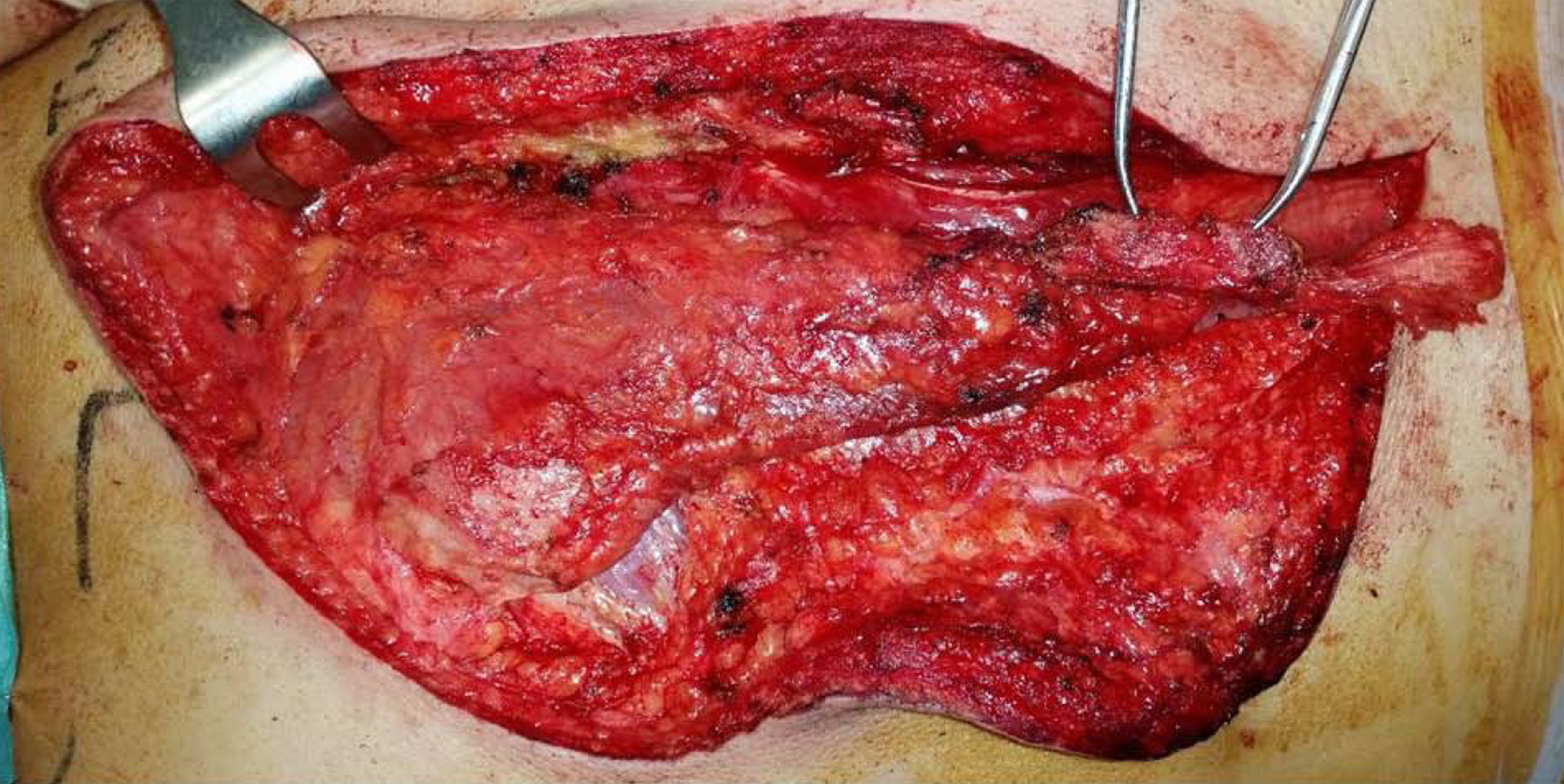
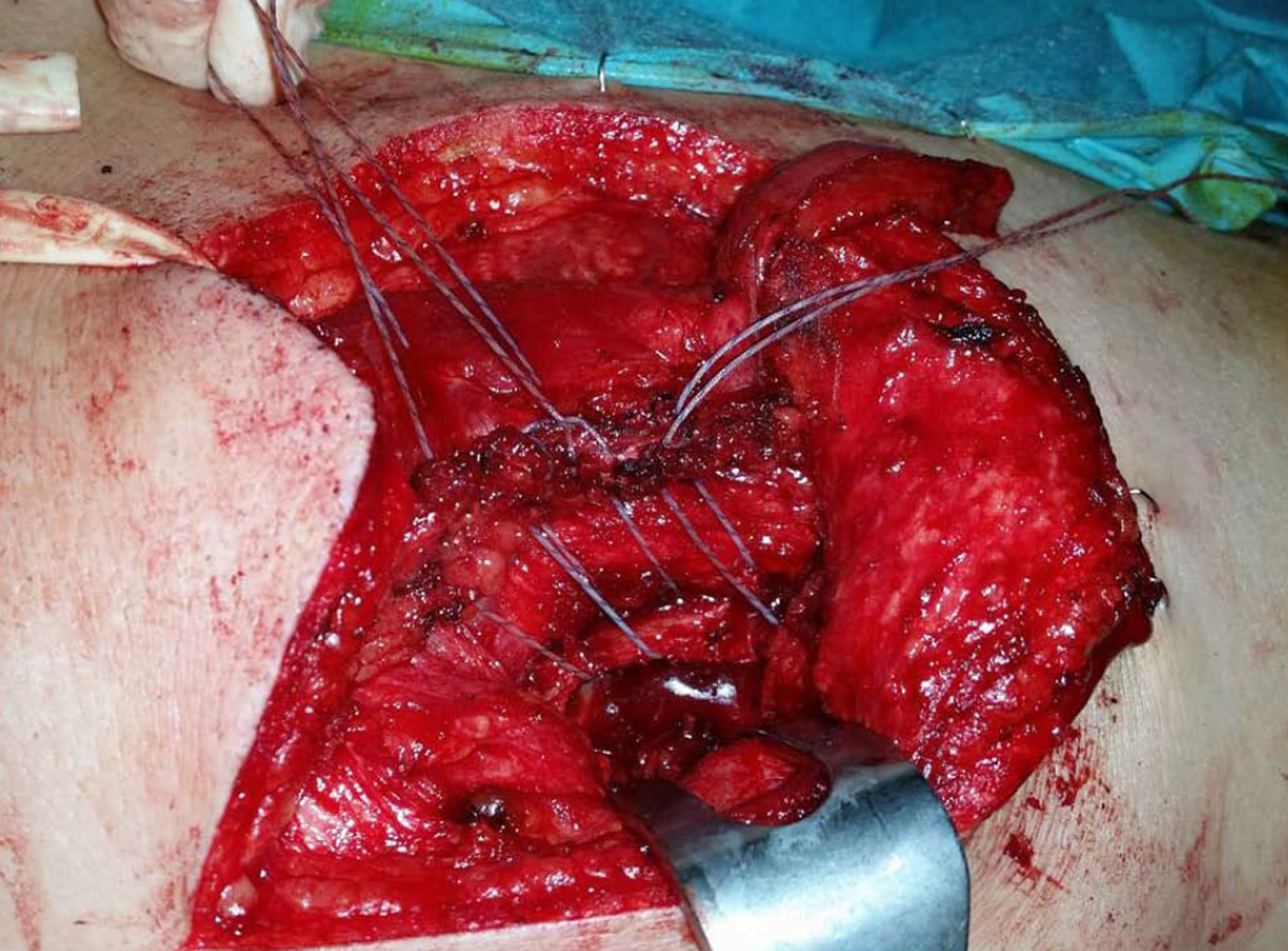
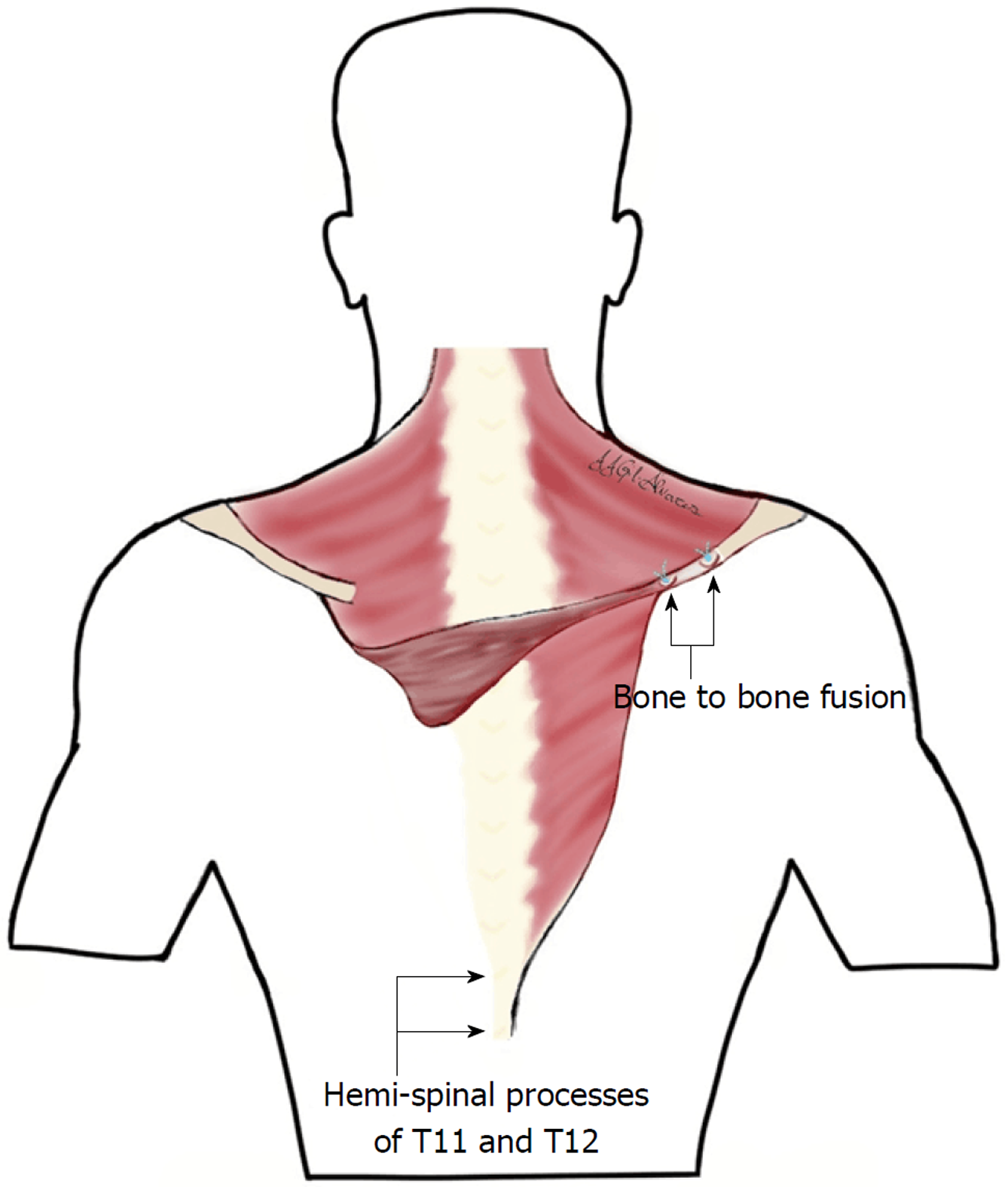
Surgery was performed under general anesthesia. The patient was placed in the prone position. Superficial anatomical landmarks were drawn, including scapular silhouette on both the recipient and donor sites, lateral edge of the trapezius muscle, and spinal processes from T4 to T12. Centered on a line bisecting the angle formed between midline and the lateral edge of trapezius, an “s” shaped incision was made with the caudal flap designed to expose the lowest thoracic spinal processes. A second incision was made along the medial border of the scapula at the site of injury, at the level of the scapular spine (Figure 4). At the donor site, the trapezius flap was raised and freed from its bed, from lateral to medial, and detached from the spinal processes except from the last two (T11 and T12), which were osteotomized to include two hemispinal processes in the compound flap. Bone bleeding in the flap indicated bone viability (Figure 5). The trapezius flap was detached from its insertion at the spinal processes, from T4 to T10. Continuity of the posterior elements of the spine was not interrupted and posterior interspinous ligament was spared. The compound osteomuscular trapezius flap was raised and passed through a subcutaneous tunnel towards the second incision (Figure 6). Prior to attaching the flap to the recipient site, the shoulder of the injured site was pushed backward to bring the medial border of the scapula closer to the midline. In this position, we marked the sites where the two hemispinal processes of the compound flap were to be placed on the scapular spine with the flap under maximal tension. At these sites, we created two beds in the spine of the scapula so that bone-to-bone fusion could take place between them, providing a footprint for bone-to-tendon fusion. The flap was then attached using anchors in the beds and transosseous sutures through the scapular spine (Figure 7). Nonabsorbable sutures were used. Layered closure was performed and drainage was placed in the donor site. A diagram of the surgery is provided in Figure 8.
The scapulothoracic joint was controlled postoperatively with a brace (Actimove® Clavicula; BSN Medical Inc., Rutherford College, North Carolina, United States), with both shoulders positioned “at attention” to avoid flap elongation for 6 wk. Five days later, the patient was discharged from in-patient care. Skin sutures were removed after 2 wk. Subsequently, the patient first underwent daily check-up by the therapist for a period of 2 mo, then twice weekly for another 2 mo.
CMS was measured monthly using an automated dynamometer (microFET®2; Hoggan Scientific LLC, Salt Lake City, Utah, United States). The patient then learned to dissociate donor from recipient movement by performing recipient movement without consciously thinking about donor movement (Video 1).
The patient improved his CMS from day 1 preoperative (19.5%) to 74.38% at 6 mo postoperative and 81.88% at 2 year postoperative. No additional improvement or impairment has been reported up to the last follow-up revision (30 mo postoperatively).
The patient was asked to record his preoperative and postoperative pain using a 10-cm visual analogue scale (commonly known as VAS). The preoperative level of pain of the injured shoulder was 5 on a 0-10 VAS. Following surgery, this score fell to 3 at 6-mo follow-up, and it was 0 at 2-year follow-up. Soreness was reported at the donor site for 6-mo postoperative.
Shoulder motion was measured preoperatively and in the follow-ups. Preoperative shoulder flexion and abduction were 60º and 45º, respectively; external rotation allowed the patient to reach the occipital area with elbows forward but internal rotation was severely impaired, since the patient was unable to reach his back. Postoperatively, all active ranges of motion were measured, and at 6 mo the patient achieved maximum postoperative mobility of the shoulder. This was maintained through to the last follow-up, with the patient having 155º flexion, 95º abduction, full elevation and ability to reach T12 on his back (Figure 9).
With respect to strength, the patient was able to lift up to 9.1 kg with no pain and shoulder flexed at 90º with the arm positioned in the axis of the scapula at the most recent measurement. No preoperative strength measurements were performed, since the patient was not able to achieve 90º of active flexion.
No impairment of the contralateral shoulder or scapular girdle was detected postoperatively. Scapulothoracic rhythm was not altered in the donor site, while it was improved in the recipient site.
We searched PubMed from January 1990 up to October 2018 using the search terms “dorsal scapular nerve”, “dorsoscapular nerve”, “nervus dorsalis scapulae”. Sixty-nine articles were retrieved, of which thirteen were deemed relevant and were used in this report. In addition, other topically relevant articles are discussed in order to support the treatment approach used on our patient; the treatment decision was based on the fact that, to the best of our knowledge, no dynamic technique (i.e., tendon transfer) had yet been described for scapular winging due to rhomboid major and minor palsy resulting from an isolated dorsal scapular nerve injury.
From an etiological point of view, dorsal scapular nerve injury usually occurs in the context of compressive neuropathy. The compression of the nerve has been described in situations related to sports medicine. Ravindran et al[22] presented the cases of 2 brothers who practiced volleyball at a high level, with both having developed a winged scapula as a consequence of neuropathies of the suprascapular nerve in association with neuropathy of the dorsal scapular nerve. The association of dorsal scapular nerve injury with suprascapular nerve injury has also been described by Lee et al[23]. Also in sports medicine, Jerosch et al[24] described the case of a judoka who, after suffering a dislocation of the glenohumeral joint, had a winged scapula due to injury to the long thoracic nerve and the dorsal scapular nerve.
There have also been reports of cases unrelated to sports medicine. Debeer et al[25] reported a case of compression exerted by a poorly adjusted orthosis in a patient with scoliosis. In our case, the patient suffered a dorsal scapular nerve injury in the workplace, after making an effort to lift a heavy weight. On this same topic are the case reports from Argyriou et al[26] (describing a patient with a winged scapula and work history of carrying about 8 kg of weight repetitively) and of Akgun et al[9] (describing a patient who developed an acute winged scapula after lifting heavy objects above the head). For these two patients, the cause was a compressive neuropathy of the dorsal scapular nerve.
Iatrogenic lesions of the scapular dorsal nerve also occupy an important niche in this research field. A case reported by Lee et al[27] developed as a consequence of a trigger point puncture in the rhomboid major muscle. Saporito[28] concluded that there is potential risk of damaging the dorsal scapular nerve and long thoracic nerve in the anesthetic blocks of the brachial plexus in the interscalene region. This researcher then recommended ultrasonographic localization of both nerves to avoid injuring them; this idea was based on the possible ultrasound localization in most cases as published by Hanson et al[29].
Regarding clinical manifestations, according to Muir et al[30] neuropathy of the dorsal scapular nerve can cause winged scapula to varying degrees, depending on the weakness of the major and minor rhomboid muscles. Sultan et al[31] defined, in addition to the winged scapula, other symptoms related to entrapment of the dorsal scapular nerve, such as interscapular pain. These authors attributed such symptoms to sensitization of nociceptors of the nerve sheath; although, interscapular pain may also be a consequence of the tension affecting the cutaneous medial branches of the dorsal primary rami of thoracic spinal nerves, that develops when the winged scapula occurs. We believe that the latter reasoning fits the cause of pain in our patient best, given that in our case the pain presented by the patient before the operation had a value of 5 in the VAS and that after the surgery the pain decreased in intensity without the need of perform any type of intervention on the nerve, only treating the winged scapula.
Another symptom reported by Sultan et al[31] is the loss of range of motion of the shoulder. In our case, the patient lost mobility in every arc of movement of the shoulder, which was recovered after the surgery. These features suggested to us that the loss of mobility was due to an alteration of the dynamics of the scapulothoracic joint and the unfavorable position by which the winged scapula affects all muscle groups of the scapular girdle. Although, in our patient, we did not observe the profile of symptomatology described by Sultan et al[31], such as cervicogenic dorsalgia, notalgia paresthetica and posterolateral arm pain, possibly related to dorsal scapular nerve neuropathy. Chen et al[32] have also reported discomfort and soreness of the neck, shoulder and back region too as part of the symptomology.
Argyriou et al[26] considered conservative treatment of dorsal scapular nerve neuropathy suitable for mild or moderate cases, as did Benedetti et al[33] who obtained satisfactory results through a multidisciplinary rehabilitation approach. However, for those cases in which conservative treatment is not effective, Argyriou et al[26] recommended surgical treatment. In this sense, Chen et al[32] considered that the symptoms derived from the compression of the scapular dorsal nerve can be improved if the middle scalene muscle and its tendinous tissue are sectioned in relation to the compressed nerve.
Nevertheless, nerve acute injuries are difficult to treat, given that such lesions are often diagnosed late. Motor endplate atrophy leads to suboptimal results when reconstruction is performed more than 3-6 mo after the nerve damage occurs. However, even immediate restoration of original function does not always result in satisfactory outcomes[34]. In these cases, tendinous transfers are widely used for the treatment of peripheral nerve injuries that are in the sequelae phase and otherwise not repairable. These dynamic procedures are currently the standard of care for restoration of shoulder function after chronic scapular winging from nerve palsy in younger, active people[35].
To the best of our knowledge, no dynamic technique, such as tendon transfer, has been described for scapular winging due to rhomboid major and minor palsy resulting from an isolated dorsal scapular nerve injury. Medial static stabilization of the scapulothoracic joint has been performed using strips of fascia lata. This technique was described by Ketenjian in 1978[36] and posteriorly modified by Atasoy and Majd[37], who obtained good results. Scapulothoracic fusion has also been suggested, although disparate results have been reported after fusion with complications such as pneumothorax, pleural effusion, atelectasis, fracture of the scapula, and pseudarthrosis[38].
Terzis et al[39] found that contralateral low trapezius transfer was a useful technique to treat scapular winging in patients with brachial plexus birth palsy (known as BPBP). Scapular winging in children with sequelae of BPBP is due not only to weakness of periscapular musculature but also to glenohumeral dysplasia, which results from an imbalance in the internal and external rotators of the shoulder. This dysplasia also leads to abnormal scapulothoracic movement during shoulder motion, due to both the anatomical and structural alterations of the glenohumeral joint. Moreover, most patients who suffer from BPBP sustain postganglionic root lesions where dorsal scapular, long thoracic and spinal nerves are usually spared. In these cases, scapular winging also develops, revealing that this condition is caused mainly by shoulder rotator imbalance instead of weakness of the periscapular muscles.
As described by Elhassan et al[40], contralateral trapezius transfer to the infraspinatus insertion appears feasible and has been used to restore external rotation of the shoulder by transferring to the infraspinatus insertion[41]. Given that suture is performed to join two tendons, weakness at the junction should not be a main concern in these cases, as it is when tendons are transferred to bone. The best healing interface is obtained when repair is performed between homogeneous tissues (i.e., bone-to-bone and tendon-to-tendon) and shows better healing quality with respect to mechanical and histological assessments, as compared to the healing between heterogeneous tissues (i.e., bone-to-tendon)[42]. Consequently, and given that at the recipient site muscle and bone are the only tissues available, we decided to take bone from the donor site to perform bone-to-bone fusion. Bone tissue was obtained without interrupting the continuity of the posterior elements of the spine, taking only the ipsilateral hemispinal processes and sparing the posterior interspinous ligament, not only in adjacent spinal processes (T10 and L1) but also in the affected ones (T11 and T12).
For our patient, scapulothoracic rhythm was preserved in the donor site and it was improved in the recipient site. Measurements were performed with visual inspection systems. Digital inclinometers have been recommended for quantifying shoulder and scapular kinematics[43], and it is possible that these devices would have reported subtle changes in the donor site.
We have found that contralateral trapezius compound osteomuscular flap transfer was able to successfully stabilize lateral scapular winging due to an isolated dorsal scapular nerve injury in the case reported, while improving shoulder function and affording pain relief. Further studies are needed with a larger sample size to determine whether the contralateral trapezius compound osteomuscular flap transfer technique is the best choice for patients with scapular winging due to an isolated dorsal scapular nerve injury.
Whole shoulder girdle exploration is needed when the shoulder function is impaired, since dorsal scapular nerve injury may go unnoticed without a high degree of suspicion. The contralateral trapezius compound osteomuscular flap is a technique that we consider to be not especially complex if performed by surgeons with experience in shoulder and periscapular surgery. Given the good result obtained with this dynamic technique for scapular stabilization when the scapular winging was due to dorsal scapular nerve injury, we have abandoned the static techniques that were carried out previously and that yielded worse results with higher associated morbidity.
In our patient, no complications were observed at the donor site, except for soreness reported at the 6-mo postoperative follow up. The conclusion we have come to from our experience and literature review is that contralateral trapezius transfer is a safe technique, even when the two lowest hemispinal processes are included in the flap.
A 37-year-old male presented at 2 years after a right shoulder indirect injury, with right scapular winging, shoulder function impairment, and pain.
Physical examination of the patient suggested a lateral scapular winging. Definitive diagnosis was obtained after neurophysiological studies revealed an isolated dorsal scapular nerve injury.
Lateral scapular winging is due to lack of function of the trapezius and/or rhomboid muscles, so these two entities should be considered. Given that in obese patients it is difficult to differentiate medial from lateral scapular winging, medial scapular winging due to lack of function of serratus anterior muscle should also be taken into account.
Electrophysiological studies showed an isolated dorsal scapular nerve lesion and proper function of other nerves, such as the long thoracic and spinal nerves.
Imaging studies (plain X-rays and magnetic resonance imaging) did not reveal any structural injury.
Not applicable in this case.
Scapular stabilization was performed by attaching, to the spine of the scapula, a compound osteomuscular flap obtained from the contralateral trapezius and T11 and T12 hemispinal processes.
Scapular winging: Scapular malposition with its inferior angle prominent, which leads to impairment of shoulder function and pain.
Contralateral trapezius compound osteomuscular flap is a technique that we consider not especially complex if performed by surgeons with experience in shoulder and periscapular surgery. Given the good result obtained with this dynamic technique for scapular stabilization when the scapular winging was due to dorsal scapular nerve injury, we have abandoned the static techniques that were carried out previously and that yielded worse results with higher associated morbidity.
Manuscript source: Unsolicited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: Spain
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Ciuman RR S- Editor: Dou Y L- Editor: A E- Editor: Tan WW
| 1. | Winslow M. Observations anatomiques sur quelques mouvements extraordinaires des omoplates et des bras, et sur une nouvelle espèce de muscles. In: Panckoucke CJ. Mémories de l’académie royale des sciences de Paris. Paris: Panckoucke, 1777: 98-112. . [Cited in This Article: ] |
| 2. | Kauppila LI, Vastamäki M. Iatrogenic serratus anterior paralysis. Long-term outcome in 26 patients. Chest. 1996;109:31-34. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 66] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 3. | Wiater JM, Bigliani LU. Spinal accessory nerve injury. Clin Orthop Relat Res. 1999;. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 33] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Wiater JM, Flatow EL. Long thoracic nerve injury. Clin Orthop Relat Res. 1999;. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 64] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 5. | Johnson JT, Kendall HO. Isolated paralysis of the serratus anterior muscle. J Bone Joint Surg Am. 1955;37-A:567-574. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 65] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 6. | Tubbs RS, Tyler-Kabara EC, Aikens AC, Martin JP, Weed LL, Salter EG, Oakes WJ. Surgical anatomy of the dorsal scapular nerve. J Neurosurg. 2005;102:910-911. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 38] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Bertelli JA, Ghizoni MF. Long thoracic nerve: anatomy and functional assessment. J Bone Joint Surg Am. 2005;87:993-998. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Gavid M, Mayaud A, Timochenko A, Asanau A, Prades JM. Topographical and functional anatomy of trapezius muscle innervation by spinal accessory nerve and C2 to C4 nerves of cervical plexus. Surg Radiol Anat. 2016;38:917-922. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 9. | Akgun K, Aktas I, Terzi Y. Winged scapula caused by a dorsal scapular nerve lesion: a case report. Arch Phys Med Rehabil. 2008;89:2017-2020. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Lee SG, Kim JH, Lee SY, Choi IS, Moon ES. Winged scapula caused by rhomboideus and trapezius muscles rupture associated with repetitive minor trauma: a case report. J Korean Med Sci. 2006;21:581-584. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Tsivgoulis G, Vadikolias K, Courcoutsakis N, Heliopoulos I, Stamboulis E, Piperidou C. Teaching neuroimages: differential diagnosis of scapular winging. Neurology. 2012;78:e109. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Kuhn JE, Plancher KD, Hawkins RJ. Scapular Winging. J Am Acad Orthop Surg. 1995;3:319-325. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 119] [Cited by in F6Publishing: 80] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 13. | Bigliani LU, Compito CA, Duralde XA, Wolfe IN. Transfer of the levator scapulae, rhomboid major, and rhomboid minor for paralysis of the trapezius. J Bone Joint Surg Am. 1996;78:1534-1540. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 43] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Bigliani LU, Perez-Sanz JR, Wolfe IN. Treatment of trapezius paralysis. J Bone Joint Surg Am. 1985;67:871-877. [PubMed] [DOI] [Cited in This Article: ] |
| 15. | van Tuijl JH, Schmid A, van Kranen-Mastenbroek VH, Faber CG, Vles JS. Isolated spinal accessory neuropathy in an adolescent: a case study. Eur J Paediatr Neurol. 2006;10:83-85. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Friedenberg SM, Zimprich T, Harper CM. The natural history of long thoracic and spinal accessory neuropathies. Muscle Nerve. 2002;25:535-539. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 82] [Cited by in F6Publishing: 56] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 17. | Oakes MJ, Sherwood DL. An isolated long thoracic nerve injury in a Navy Airman. Mil Med. 2004;169:713-715. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Murphy MT, Journeaux SF. Case reports: long thoracic nerve palsy after using a single axillary crutch. Clin Orthop Relat Res. 2006;447:267-269. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Bowen TR, Miller F. Greenstick fracture of the scapula: a cause of scapular winging. J Orthop Trauma. 2006;20:147-149. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 20. | Martin RM, Fish DE. Scapular winging: anatomical review, diagnosis, and treatments. Curr Rev Musculoskelet Med. 2008;1:1-11. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 138] [Cited by in F6Publishing: 102] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 21. | Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1732] [Cited by in F6Publishing: 1750] [Article Influence: 47.3] [Reference Citation Analysis (0)] |
| 22. | Ravindran M. Two cases of suprascapular neuropathy in a family. Br J Sports Med. 2003;37:539-541. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Lee SY, Lee HD, Cho YS, Han SH. Winged scapula caused by dorsal scapular neuropathy combined with suprascapular neuropathy: A case report. Medicine (Baltimore). 2018;97:e12515. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 24. | Jerosch J, Castro WH, Geske B. Damage of the long thoracic and dorsal scapular nerve after traumatic shoulder dislocation: case report and review of the literature. Acta Orthop Belg. 1990;56:625-627. [PubMed] [Cited in This Article: ] |
| 25. | Debeer P, Van Den Eede E, Moens P. Scapular winging: an unusual complication of bracing in idiopathic scoliosis. Clin Orthop Relat Res. 2007;461:258-261. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 26. | Argyriou AA, Karanasios P, Makridou A, Makris N. Dorsal scapular neuropathy causing rhomboids palsy and scapular winging. J Back Musculoskelet Rehabil. 2015;28:883-885. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 27. | Lee DG, Chang MC. Dorsal scapular nerve injury after trigger point injection into the rhomboid major muscle: A case report. J Back Musculoskelet Rehabil. 2018;31:211-214. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 28. | Saporito A. Dorsal scapular nerve injury: a complication of ultrasound-guided interscalene block. Br J Anaesth. 2013;111:840-841. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 29. | Hanson NA, Auyong DB. Systematic ultrasound identification of the dorsal scapular and long thoracic nerves during interscalene block. Reg Anesth Pain Med. 2013;38:54-57. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 34] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 30. | Muir B. Dorsal scapular nerve neuropathy: a narrative review of the literature. J Can Chiropr Assoc. 2017;61:128-144. [PubMed] [Cited in This Article: ] |
| 31. | Sultan HE, Younis El-Tantawi GA. Role of dorsal scapular nerve entrapment in unilateral interscapular pain. Arch Phys Med Rehabil. 2013;94:1118-1125. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 32. | Chen D, Gu Y, Lao J, Chen L. Dorsal scapular nerve compression. Atypical thoracic outlet syndrome. Chin Med J (Engl). 1995;108:582-585. [PubMed] [Cited in This Article: ] |
| 33. | Benedetti MG, Zati A, Stagni SB, Fusaro I, Monesi R, Rotini R. Winged scapula caused by rhomboid paralysis: a case report. Joints. 2017;4:247-249. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 34. | Kömürcü F, Zwolak P, Benditte-Klepetko H, Deutinger M. Management strategies for peripheral iatrogenic nerve lesions. Ann Plast Surg. 2005;54:135-139; discussion 140-142. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 35. | Galano GJ, Bigliani LU, Ahmad CS, Levine WN. Surgical treatment of winged scapula. Clin Orthop Relat Res. 2008;466:652-660. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 76] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 36. | Ketenjian AY. Scapulocostal stabilization for scapular winging in facioscapulohumeral muscular dystrophy. J Bone Joint Surg Am. 1978;60:476-480. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 65] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 37. | Atasoy E, Majd M. Scapulothoracic stabilisation for winging of the scapula using strips of autogenous fascia lata. J Bone Joint Surg Br. 2000;82:813-817. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 38. | Letournel E, Fardeau M, Lytle JO, Serrault M, Gosselin RA. Scapulothoracic arthrodesis for patients who have fascioscapulohumeral muscular dystrophy. J Bone Joint Surg Am. 1990;72:78-84. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 42] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 39. | Terzis JK, Papakonstantinou KC. Outcomes of scapula stabilization in obstetrical brachial plexus palsy: a novel dynamic procedure for correction of the winged scapula. Plast Reconstr Surg. 2002;109:548-561. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 40. | Elhassan BT, Wagner ER, Bishop AT. Feasibility of contralateral trapezius transfer to restore shoulder external rotation: part I. J Shoulder Elbow Surg. 2012;21:1363-1369. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 41. | Elhassan BT, Wagner ER, Spinner RJ, Bishop AT, Shin AY. Contralateral Trapezius Transfer to Restore Shoulder External Rotation Following Adult Brachial Plexus Injury. J Hand Surg Am. 2016;41:e45-e51. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 14] [Article Influence: 1.8] [Reference Citation Analysis (1)] |
| 42. | Leung KS, Chong WS, Chow DH, Zhang P, Cheung WH, Wong MW, Qin L. A Comparative Study on the Biomechanical and Histological Properties of Bone-to-Bone, Bone-to-Tendon, and Tendon-to-Tendon Healing: An Achilles Tendon-Calcaneus Model in Goats. Am J Sports Med. 2015;43:1413-1421. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 43. | Scibek JS, Carcia CR. Assessment of scapulohumeral rhythm for scapular plane shoulder elevation using a modified digital inclinometer. World J Orthop. 2012;3:87-94. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 35] [Cited by in F6Publishing: 31] [Article Influence: 2.6] [Reference Citation Analysis (1)] |