Copyright
©The Author(s) 2017.
World J Orthop. Feb 18, 2017; 8(2): 115-129
Published online Feb 18, 2017. doi: 10.5312/wjo.v8.i2.115
Published online Feb 18, 2017. doi: 10.5312/wjo.v8.i2.115
Figure 1 With the patient under anesthesia, we verify that the patella can be dislocated laterally.
Figure 2 Lateral patellar instability in flexion.
The patella dislocates laterally beyond 40º of knee flexion.
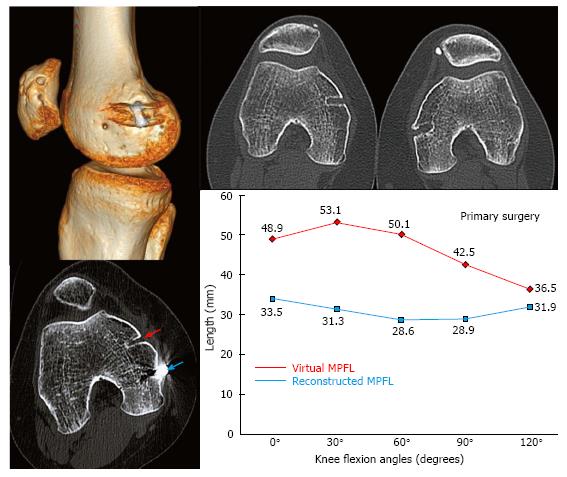
Figure 3 The femoral tunnel is non-anatomic.
A very serious mistake when performing patellar tunnels. We can see that the patellar tunnels are drilled through the medial facet articular surface and exit through the central dorsal aspect of the patella.
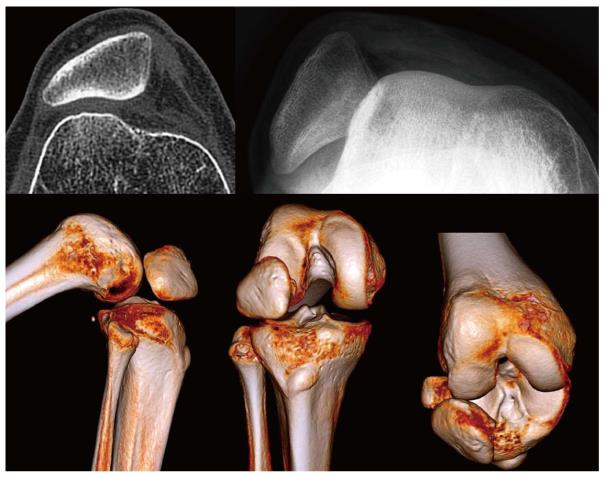
Figure 4 Patient of 19 years of age with severe anterior knee pain and lateral patellar instability.
Three years ago, he had a MPFL reconstruction with a single bundle semitendinosus tendon graft. During the physical examination, there was no disorder in patellofemoral tracking. With the patient under general anesthesia, the patella could not be dislocated beyond 40º of knee flexion. We note that the femoral tunnel of the MPFL reconstruction is too anterior, which is a serious mistake. There is also severe chondropathy of the articular surface of the patella. We can see that the distance between the patellar fixation point and the femoral fixation point increases with knee flexion. Clinically, this causes an increase in patellofemoral pressure during knee flexion that could justify the severe patellar chondropathy the patient has. The anatomic MPFL reconstruction, using the contralateral semitendinosus tendon with a double bundle technique, led to the resolution of all the patient’s symptoms. MPFL: Medial patellofemoral ligament.
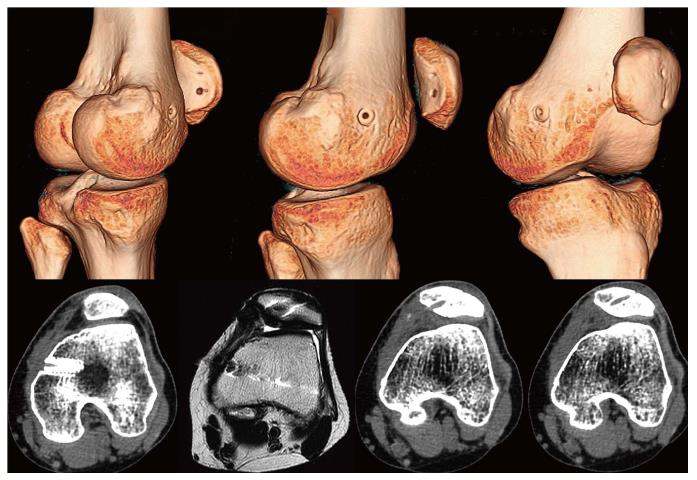
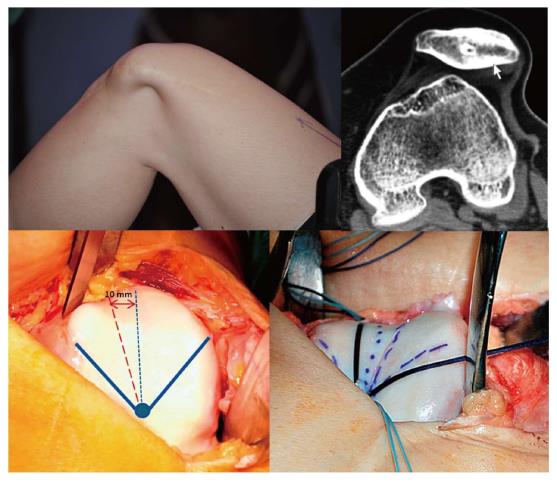
Figure 5 Patient 28-year-old, with very severe anterior knee pain and lateral patellar instability.
During the physical examination, we saw a clear patellofemoral mal-tracking and we were able to dislocate the patella laterally beyond 60º of knee flexion. She has been operated on several times over the last 8 years: A lateral retinacular release, proximal realignment, an ostetotomy for medialization of the tibial tubercle and MPFL reconstruction. We note that the femoral tunnel is too proximal and anterior. The distance between the patellar fixation point and the femoral fixation point increases significantly with knee flexion. Clinically, this increases patellofemoral pressure significantly during knee flexion, which could explain the severe patellofemoral osteoarthritis the patient has. In this specific case the pain disappeared after a sulcus deepening trochleoplasty. We performed an anatomic double bundle MPFL reconstruction with a semitendinosus tendon graft and the lateral patellar instability also disappeared completely. MPFL: Medial patellofemoral ligament.
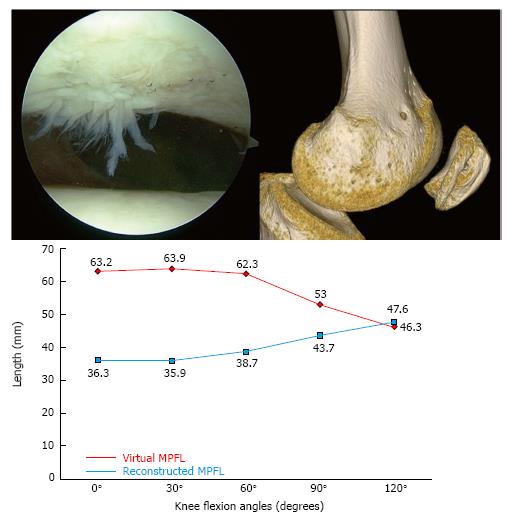
Figure 6 Very severe left anterior knee pain in a female patient of 30 years of age who had a medial patellofemoral ligament reconstruction using partial thickness quadriceps tendon.
Clinically, no patellofemoral tracking disorders were found. With the patient under general anesthesia, the patella could be dislocated laterally despite an intact MPFL. In this specific case, the instability is due to an inadequate graft length change pattern during knee flexion and extension. After an anatomic double bundle MPFL reconstruction, using a semitendinosus tendon graft, the lateral patellar instability as well as the pain were completely resolved. MPFL: Medial patellofemoral ligament.
Figure 7 The anatomic variability of the adductor tubercle may explain the anatomic variability of the medial patellofemoral ligament femoral fixation point.
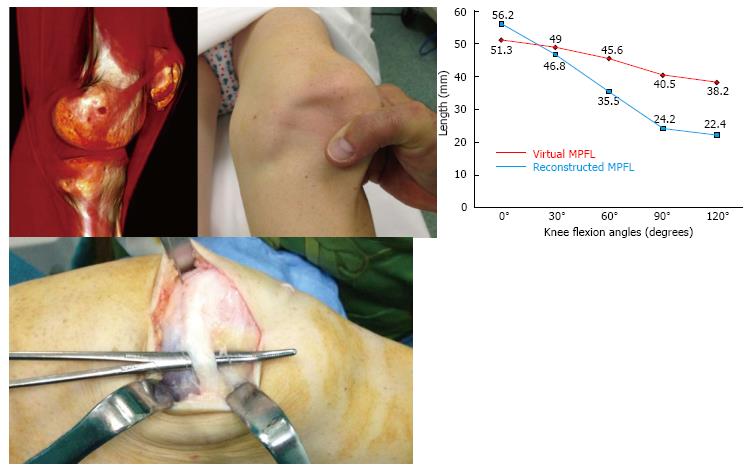
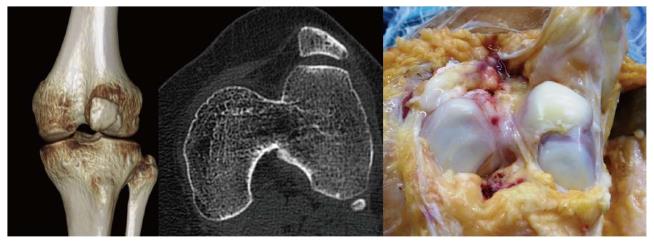
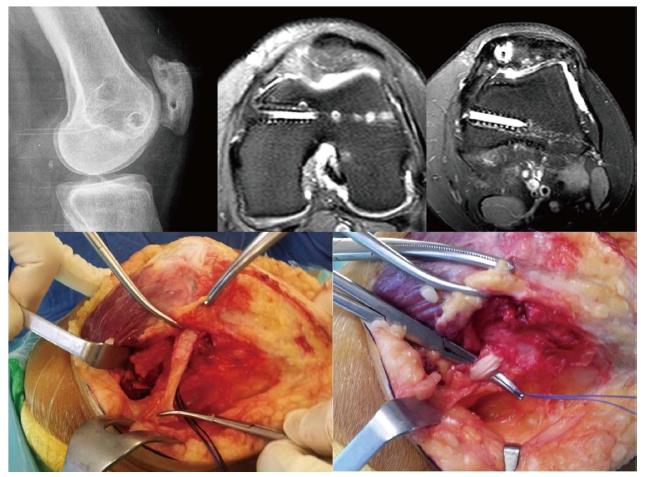
Figure 8 This patient had a bilateral medial patellofemoral ligament reconstruction for lateral patellar instability with no anatomical predisposing factors.
The left knee has an anatomic femoral tunnel with an excellent clinical result. However, the right knee has a femoral tunnel that is too anterior and this fact is responsible for the non-physiological behavior of the graft. It is isometric from 0º to 120º of knee flexion. After anatomic MPFL reconstruction, the symptoms disappeared completely (Reproduced with permission from Springer). MPFL: Medial patellofemoral ligament.
Figure 9 Chronic lateral patellar instability in a patient with grade D trochlear dysplasia.
We note that the patella dislocates beyond 40º of knee flexion. Lateral patellar instability resolved after a MPFL reconstruction associated with a sulcus deepening trochleoplasty. MPFL: Medial patellofemoral ligament.
Figure 10 Notice how the medial patellofemoral ligament tightens with the patella’s passive medial displacement.
In this case, the MPFL can be visualized very well because the patient is slender and has subcutaneous tissue atrophy due to multiple cortisone injections. This finding confirms the fact that the MPFL is not only a stabilizer for patellar lateral displacement but also for medial displacement. MPFL: Medial patellofemoral ligament.
Figure 11 The TT-TG distance is not measurable in this particular case because of the severe and peculiar trochlear dysplasia.
On the 3D model, the TT looks quite lateralized in comparison with the TT-TG distance calculated by the radiologist: 15 mm. We suggest a TT-PCL measurement when the TT-TG is not measurable.
Figure 12 When we consider a surgical procedure to correct patellofemoral maltracking, we have to take not only the TT-TG distance (abnormal if > 20 mm) into consideration but also the existence of chondral lesions and their location in the patella.
In this case, a possible candidate for a Fulkerson osteotomy, the location of the chondral lesion would worsen the prognosis.
Figure 13 This patient has had two operations on his medial patellofemoral ligament.
We can observe the different tunnels in the patella and distal femur. In this case, a MPFL reconstruction was performed without bone tunnels using the adductor magnus tendon as a post and a partial thickness medial quadriceps tendon as a graft (reproduced with permission from AOTT Journal, The Turkish Society of Orthopaedics and Traumatology). MPFL: Medial patellofemoral ligament.
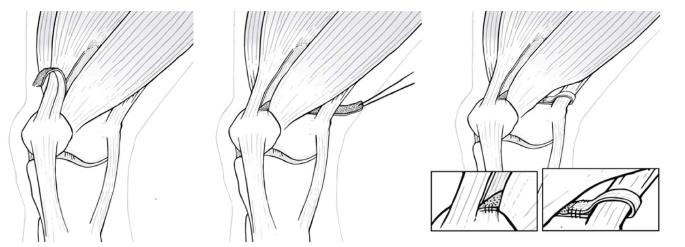
Figure 14 Diagram of a medial patellofemoral ligament reconstruction without bone tunnels using a partial thickness graft of the medial area of the quadriceps tendon (reproduced with permission from AOTT Journal, The Turkish Society of Orthopaedics and Traumatology).
- Citation: Sanchis-Alfonso V, Montesinos-Berry E, Ramirez-Fuentes C, Leal-Blanquet J, Gelber PE, Monllau JC. Failed medial patellofemoral ligament reconstruction: Causes and surgical strategies. World J Orthop 2017; 8(2): 115-129
- URL: https://www.wjgnet.com/2218-5836/full/v8/i2/115.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i2.115